Abstract
The coronavirus disease pandemic has affected our practice as healthcare professionals. As burn surgeons, we are obliged to provide the best possible care to our patients. However, due to the risk of viral transmission, the goal should be to provide safe care to our patients as well as ensure the safety of the whole team providing burn care. The burn patients are usually debilitated and require a prolonged hospital stay and multiple operative procedures which put them and everyone involved in their care at increased risk of coronavirus infections and transmission. This warrants special caution to the burn team while managing such patients. In this review, we aim to highlight the key considerations for burn care teams while dealing with burn patients during the COVID-19 pandemic.
The coronavirus disease pandemic has spread to every corner of the world and has affected our practice as healthcare professionals. As burn surgeons, it is our moral obligation to provide the best possible care to our patients. However, in view of the risk of viral transmission, the goal should be to provide safe care to our patients as well as to maintain the safety of our burns team to preserve the capacity of the health system.1
With lockdowns being enforced in various countries due to the pandemic, the risk of minor household burns also poses as much a problem as major burns at this time. These are seen more commonly with children and the elderly who are also predisposed to more severe COVID infections. This fact makes it all the more important for the treating burn team to be aware of the diagnosis and basics of management of coronavirus disease in this age group.2,3
In this review of our clinical experience and published literature, we highlight the key considerations for burn care teams while dealing with burn patients during the COVID-19 pandemic. Individual hospital guidelines may impact how the burn care is delivered, this article provides considerations for practice, which need to be attuned to the local/institutional policies.
-
Team training and preserving the workforce:
It is imperative to train all the healthcare staff about personal safety, screening, and provide refresher training on infection prevention and control (IPC). We must acknowledge the fact that prevalent IPC practices in most burn units are already consistent with the safety measures to be employed during the outbreak. This fact helps burn units to adapt to the new guidelines with ease.
All the team members should be familiarized with the use of personal protective equipment (PPE) using video tutorials as soon as possible.4
Training on managing infected patients, disposal of dressings, and the use of a ventilator may be important in providing quality treatment.
As most critical care specialists will be preoccupied in managing critical COVID patients, the burn team should be trained to manage critically ill burn patients on ventilators. Videoconferences and teleconsultations may be sought from the critical care specialists as and when needed.
The workforce should be restructured to stagger the rota and reduce nonproductive attendance in the hospitals. This will reduce their risk of contracting SARS-CoV-2 infection, while preserving their pool if they need to be redeployed at COVID care.
With limited staffing, it is paramount to protect healthcare workers. Based on the institutional COVID testing capacity, the burn team members may be screened weekly to prevent onward disease transmission in hospitals through asymptomatic infected healthcare staff.5
-
Advice for emergency Burn Clinics:
Minor burns
Minor burns should receive first aid in the form of cooling the burn with water for 20 minutes followed by a clean dressing at home. Professional guidance may be provided to such patients over a remote consultation using video calls.
b. Moderate and major burns
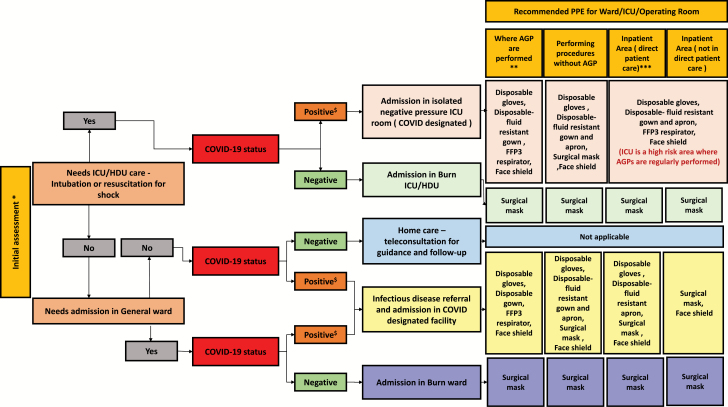
The coronavirus disease has a long mean incubation period and the disease spectrum may range from asymptomatic, mild to severe infections. It is thus prudent to treat every patient in an emergency as a COVID patient.6 All the patients and their caregivers attending the emergency department should be temperature screened at the point of entry. Apart from the history of the burn injury, it is important to obtain a history of travel, close contact with a known case, and symptoms suggestive of COVID in the past 2 weeks. If the history is positive, the infectious disease team should be immediately informed and COVID-19 testing should be performed. The subsequent management decisions and safety measures will depend on the COVID test results (Figure 1).
Figure 1.
An algorithm for decision making for management of burns, admission facility, and recommended safety measures to be worn during the course of hospital stay (adapted from COVID-19: Good Practice for Surgeons and Surgical Teams, Royal College of Surgeons). *At initial assessment in the emergency department, disposable gloves, disposable gown and apron, fluid-resistant mask (type IIR), and face shield should be worn. Every patient presenting for treatment should be treated as a potential infected case and should be tested if screening indicates. Ideally, the surgical mask should be a fluid-resistant (type IIR) facemask.7 The overall filter efficiency of FFP1, FFP2, and FFP3 masks is 80%, 94%, and 99%, respectively.7**The following procedures are currently considered to be AGP (aerosol-generating procedures) for COVID-19: intubation, extubation, and related procedures, eg, manual ventilation and open suctioning of the respiratory tract (including the upper respiratory tract); tracheotomy/tracheostomy procedures (insertion/open suctioning/removal); bronchoscopy and upper ENT airway procedures that involve suctioning; surgical procedures involving high-speed devices; noninvasive ventilation, eg, Bilevel positive airway pressure ventilation and continuous positive airway pressure ventilation, high-frequency oscillatory ventilation, and high-flow nasal oxygen.7 ***Direct patient care: involves working within 2 m of a positive case or direct contact. Note: Hand hygiene should be performed at entry and exit and frequently in between for all categories irrespective of whether PPE is worn. ICU, intensive care unit; HDU, high dependency unit; AGP, aerosol-generating procedure. $A COVID-positive patient should wear a surgical mask, in addition, if the patient undergoes an AGP, a protective hood may be used.
Attending physicians should wear disposable gloves, disposable gown and apron, fluid-resistant mask (type IIR), and face shield and whenever possible, keep a distance of 2 m while examining the patient.
Only one caregiver should be allowed with the patient to avoid overcrowding at the emergency.8 The same caution should be exercised while examining respiratory burns. Securing the airway for such patients is known to generate aerosols. It is recommended to wear an FFP3-N 95 mask along with a full PPE kit for the same.
At the time of admission, consent should be obtained for the risk of COVID-19 infection along with the risks pertaining to surgical procedures.
c. Examination and dressing of burns
The attending physician should wear the recommended protective gear based on the level of risk (Figure 1) and perform hand hygiene before and after the procedure. For regular burn dressings, the frequency of dressing change should be appropriately reduced according to the level of wound exudation and stage of healing.
Newer and advanced foam-based dressings and negative-pressure wound therapy may be employed. To reduce the risk of infection during hospital visits, the patients can get dressings changed at a local facility.
-
3. Advice for in-hospital treatment of burns:
COVID-positive patients
Such patients should be nursed in a COVID designated isolation room for 14 days. After this period, they can be transferred to the relevant ward according to their condition.
Patients with inhalational burns should be nursed in a single isolated negative-pressure room. The intensive care unit (ICU) managing a critical COVID-positive patient should be separate from a burn ICU managing other burn patients as their immunocompromised nature makes them furthermore susceptible.
All the invasive and aerosol-generating procedures should be performed preferably in a negative-pressure room with complete PPE. The nursing personnel should also try to reduce the frequency of invasive procedures such as sputum suction and lavage without compromising the treatment. All the personnel in the ward should wear the recommended protective gear (Figure 1).
The number of caregivers in contact with the patient should be limited to one or two and they should also be screened for the disease at the point of entry. Other visitors should only be allowed to meet through a remote video visiting system.9
b. COVID-negative patients
Fever is not uncommon in severe burns; however, it is important to observe for corresponding indicators such as decreasing consciousness and systemic symptoms such as muscle pain, fatigue, and reduced appetite and to observe whether the patient has chest tightness, dyspnea, and cyanosis, or dry cough, etc. Timely screening of such patients should be performed with a chest CT and SARS-CoV-2 reverse transcriptase-polymerase chain reaction.10,11 Similarly, initially screened negative patients with sudden deterioration should also be reevaluated.
-
4. Advice on burn surgeries:
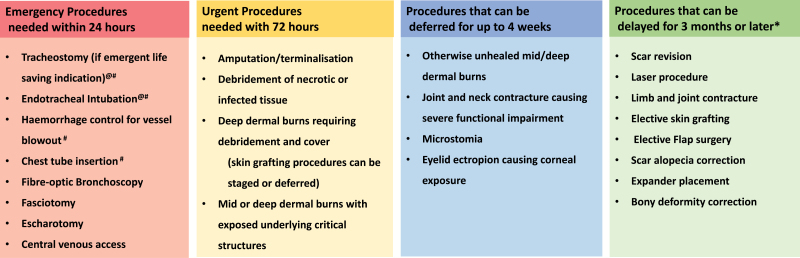
Triaging of procedures
The Royal College of Surgeons and American College of Surgeons provide comprehensive guidance on the triage of nonemergent surgical procedures12,13; however, there are no existing guidelines catering specifically to burns. Figure 2 provides a guide for prioritization of procedures and surgeries on burn patients, although the final decision should be individualized and weighed on risks versus benefits. All burn surgeries that are life- or limb-saving deserve a priority, however, the volume of procedures should be controlled to rationalize the use of precious PPE and safety of healthcare professionals.
Figure 2.
Guide for prioritization of procedures and surgeries on burn patients (adapted from the clinical guide to surgical prioritization during the coronavirus pandemic). #Lifesaving procedures that need to be done within minutes to hours. @Ranked highest among the AGPs (aerosol-generating procedures).7 *Till the pandemic curve flattens or is settled as per definition.
b. Intraoperative prevention and control
All the medical staff inside the operating room (OR) should strictly implement standard protective measures and hand hygiene as per the CDC guidelines for airborne and droplet infections.14
It is recommended that both the anesthesia and surgery teams should wear an FFP3-N95 mask,7 although there is presently no robust evidence to suggest that a powered air-purifying respirator offers better protection compared to N95 mask.15
In an actively infected patient, all measures should be taken to reduce liquid splash and contamination. The time of surgery should be minimized using appropriate devices such as staples. Several studies have found that the viral load remains in essentially all body fluids and surgical smoke from electrocautery. Thus, the generation of smoke should be minimized by reducing the usage of monopolar cautery.16–18
SARS-CoV-2 is found to survive on the surfaces of operating theaters for up to 9 days and also runs the risk of contaminating other ORs.19 Conventionally ORs use a positive pressure flow; however, while operating a COVID-suspected or positive patient, it is recommended to use a negative-pressure operating room. If such a room is unavailable, a COVID-positive patient should be posted as the last case on the list or sufficient time (around 30 minutes) should be allowed between the cases for the complete exchange of room air.20
c. Postoperative management
Patients should be nursed in isolation in the postoperative period and rehabilitation measures should be deferred to limit exposure to the support staff.
5. Advice on discharge and follow-up
For a COVID-19-infected patient in addition to meeting the discharge criteria for burns, they must also fulfill the discharge criteria for coronavirus disease. They must also follow the necessary isolation and observation after discharge.
Post-discharge follow-up can be handled remotely using teleconsultation. The University of Tennessee has developed a mobile application to provide postburn recovery guidance. This helps to relieve the overburdened medical facilities obviating the need for a physical consultation. It provides instructions for rehabilitation and encouragement for self-care.21 Using web-based or smartphone-based video consultations for rehabilitation advice would help to provide customized remote guidance to the patients post-discharge and reduce the need for frequent follow-up. Physiotherapy is a quintessential component of burn care and remotely guided physiotherapy can be a safe and convenient way to implement social distancing. It will supplement face-to-face (supervised) physiotherapy which should only continue when clinically indicated. Strict no-sharing policy for physiotherapy equipment like bands, balls, tubing, and weights until sanitized should be followed.
6. Leveraging technology
Cases being referred from other centers should be discussed via a video/teleconference prior to shifting of the patient and appropriately triaged to decide the setting and time of management. Teleconsultations have been used for triage and clinical decision making for patients with trauma and burns in plastic surgery services and have proven to be convenient, reliable, and cheap.22 In places where such systems do not preexist, it is also an opportunity to set up the facility to provide care using this facility. After the pandemic is over it can help immensely to provide time and cost-effective care for burn patients.
The knowledge about COVID-19 is continually evolving in the global medical community. This review should not be used as official guidelines or recommendations as many of the facts may change in the light of new information available. However, these recommendations may be modified or adapted by individual institutions based on their standard operating procedures.
Funding: No funding was obtained for this study.
Conflict of interest statement. The authors of this study have no conflict of interest.
All authors contributed equally to the preparation of the manuscript. Additionally, M.S. managed the overall writing and concept.
References
- 1. Lancet T. COVID-19: protecting health-care workers. Lancet 2020;395:922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang S-B, Chang W-H, Huang C-H et al. Management of elderly burn patients. Int J Gerontol 2008;2:91–7. [Google Scholar]
- 3. Burns. https://www.who.int/news-room/fact-sheets/detail/burns; accessed 31 Mar. 2020.
- 4. Training | Personal Protective Equipment (PPE) | Public Health Planners | Ebola (Ebola Virus Disease) | CDC. https://www.cdc.gov/vhf/ebola/healthcare-us/ppe/training.html. Published 25 July 2019; accessed 31 Mar. 2020.
- 5. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet 2020;395:1418–20. doi: 10.1016/S0140-6736(20)30917-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lauer SA, Grantz KH, Qifang B et al. The incubation period of coronavirus disease 2019 (covid-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020;172:577–82. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cook TM. Personal protective equipment during the COVID-19 pandemic—a narrative review. Anaesthesia 2020;75:920–7. doi: 10.1111/anae.15071 [DOI] [PubMed] [Google Scholar]
- 8. Ma SY, Yuan ZQ, Peng YZ et al. Recommendations for the regulation of medical practices of burn treatment during the outbreak of the coronavirus disease 2019. Zhonghua Shao Shang Za Zhi 2020;36:E004. [DOI] [PubMed] [Google Scholar]
- 9. Li N, Liu TM, Chen HL, Liao JM. Management strategy of novel coronavirus pneumonia in burn and wound care ward. Zhonghua Shao Shang Za Zhi 2020;36:E002. [DOI] [PubMed] [Google Scholar]
- 10. Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Corman VM, Landt O, Kaiser M et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020;25:2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. COVID-19: Clinical guidance for surgeons [Internet]. cited 29 Apr. 2020; available from https://www.rcsi.com/dublin/coronavirus/surgical-practice/clinical-guidance-for-surgeons; Internet.
- 13. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures [Online 17 Mar. 2020] American College of Surgeons. https://www.facs.org/covid-19/clinical-guidance/triage; accessed 31 Mar. 2020.
- 14. CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. cited 29 Apr. 2020; available from https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html; Internet.
- 15. Qian Y, Willeke K, Grinshpun SA, Donnelly J, Coffey CC. Performance of N95 respirators: filtration efficiency for airborne microbial and inert particles. Am Ind Hyg Assoc J 1998;59:128–32. [DOI] [PubMed] [Google Scholar]
- 16. Simpson AH, Dall G, Haas JG. COVID-19: potential transmission through aerosols in surgical procedures and blood products. Bone Joint Res 2020;9:200–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stephenson DJ, Allcott DA, Koch M. The presence of P22 bacteriophage in electrocautery aerosols. Proceedings of the National Occupational Research Agenda Symposium; Salt Lake City, UT; 2004. http://works.bepress.com/dale_stephenson/9/ [Google Scholar]
- 18. Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med 2016;73:857–63. [DOI] [PubMed] [Google Scholar]
- 19. Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 2020;104(3):246–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Doremalen N, Bushmaker T, Morris DH et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Amid COVID-19 Concerns, App for Patient Support Adopted by Burn Center—News https://news.utk.edu/2020/03/18/amid-covid-19-concerns-app-for-patient-support-adopted-by-burn-center/; accessed 31 Mar. 2020.
- 22. Wallace DL, Jones SM, Milroy C, Pickford MA. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg 2008;61:31–6. [DOI] [PubMed] [Google Scholar]