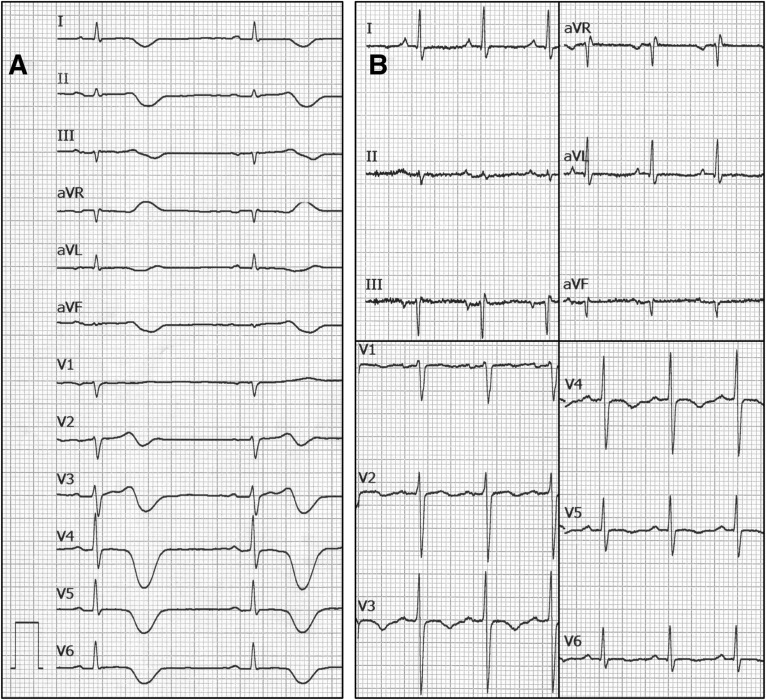
A 70-year-old man with no relevant family or medical history and normal electrocardiogram (ECG) presented at the emergency room with a 6-day history of cough, fever, and dyspnoea suggestive of COVID19 pneumonitis. The polymerase chain reaction for SARS-CoV2 was positive and he received 400 mg of hydroxychloroquine b.i.d. on hospital admission followed by 200 mg b.i.d. for four additional days. This treatment was complemented with 500 mg of azithromycin during these 5 days. On Day 14 from hospital admission, he developed bradycardia, diffuse T-wave inversion and severe QT (620 ms) and QTc (532–560 ms) interval prolongation (Panel A). Isoproterenol infusion quickly restored normal heart rate (70 b.p.m.) and new ECGs showed normal QTc interval with flat and inverted T waves in most ECG leads (Panel B). Electrolyte balance and renal function indicators were within normal values during the whole hospital stay but mild transient elevation of high-sensitive troponin I was demonstrated. A transthoracic echocardiogram showed normal systolic function and no ventricular segmental defects. Diffuse T-wave inversion and transient troponin elevation supports a significant role of myocardial inflammation on QT prolongation in this patient. This case emphasizes that QT prolongation may result from mechanisms other than or concurrent with drug toxicity in COVID patients.
The full-length version of this report can be viewed at: https://www.escardio.org/Education/E-Learning/Clinical-cases/Electrophysiology.