Stress-induced sudden cardiac arrest (SCA) with mitral annulus disjunction (MAD) in a physician amid the COVID-19 pandemic fight. MAD visualized in CMR and TTE. No factors of a high risk of SCA. Could extreme stress be a causative factor?
A 35-year-old female physician with no prior cardiac disease or symptoms of arrhythmia experienced a sudden cardiac arrest (SCA). Ventricular fibrillation occurred during her shift in a designated COVID-19 hospital at the onset of the pandemic. Despite delayed CPR, she was successfully resuscitated. Cardiac magnetic resonance (CMR) and transthoracic echocardiography (TTE) unveiled a typical pattern of mitral annulus disjunction (MAD), and no other abnormalities explaining the SCA were detected in a broad spectrum of diagnostics. After a subcutaneous implantable cardiac device (ICD) was implanted, she was discharged in excellent cardiac and neurological condition.
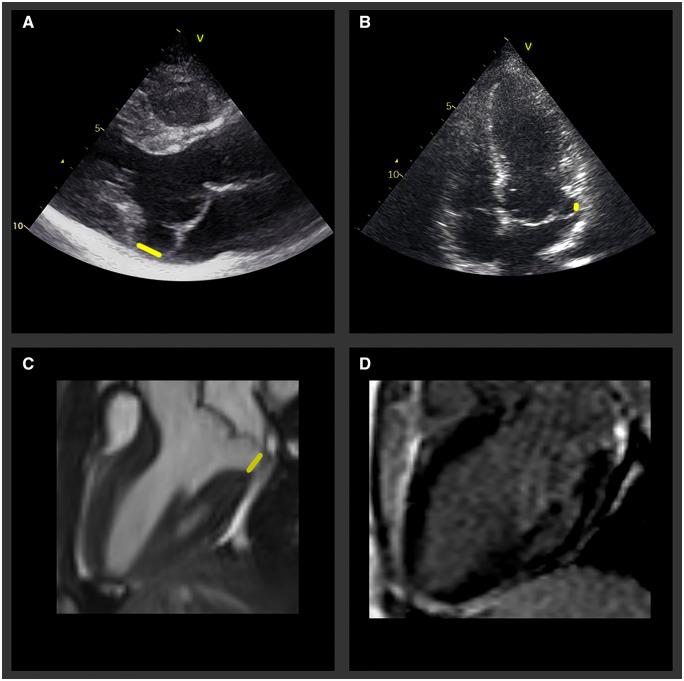
MAD prevails as a novelty, unclear in its prevalence, treatment, and risk stratification. CMR and TTE modalities typically visualize a separation between the left atrial wall–posterior mitral leaflet junction and the top of the posterolateral left ventricular wall in the parasternal long axis or apical view. Additionally, magnetic resonance imaging (MRI) may detect myocardial fibrosis, which, alongside young age and low ejection fraction, is a marked high risk factor. Surprisingly, our patient, except for being relatively young, had none of these. This underscores the incertitude of currently available data. Possible different arrhythmogenic triggers could be the mediators. The majority of observed SCA in mitral valve prolapse patients occurs at rest or during sleep. Contrarily, this patient had ventricular fibrillation in an extremely stressful environment, as a first-line physician treating COVID-19 cases. Although the observed correlation may be random, such relationships of distinct stress factors should be considered and further investigated, particularly among patients with MAD and without apparent clinical variables previously associated with an increased risk.
Panels A–D. Mitral annulus disjunction (MAD) visualized on TTE and MRI; all images captured during end-systole [yellow bar on the parasternal long axis – 11 mm (Panel A) and apical four-chamber view – 4 mm (Panel B) in TTE, three-chamber view in MRI – 9 mm (Panel C)]. No late gadolinium enhancement was seen (Panel D).