Introduction
Current coronavirus disease (COVID-19) has grown into a pandemic crisis of major health and economic importance. An infection with severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) is known to cause severe respiratory symptoms up to an acute respiratory distress syndrome (ARDS), but also often involves the cardiovascular system,1,2 which is associated with increased mortality.3 The highest mortality rates were observed in patients with underlying cardiovascular disease and co-existing elevated cardiac troponin levels.4 In particular, elevated serum levels of cardiac troponin and inflammatory biomarkers (i.e. interleukin-6 and serum ferritin) were characteristic for cases with severe illness and non-survivors.4–8 This high inflammatory burden in COVID-19, described as a hyperinflammatory response, is considered to be co-responsible for development of ARDS, vascular inflammation, myocarditis, and myocarditis-related cardiac events, e.g. arrhythmias.6,7 However, many individuals have only mild or no symptoms despite being infected.
Are athletes at risk for COVID-19?
Despite the fact that athletes do not belong to the risk group for severe COVID-19, numerous individuals and occasionally entire sports teams have been affected by COVID-19 infections.9,10 In this context, the question arises of to what extent a SARS-CoV-2 infection with or without symptoms can affect eligibility for sport, particularly the point of return to training or competition.
Still, due to their, on average, young age and good general health, it can be assumed that the frequency of mild or asymptomatic persons will be significantly higher in this subgroup when compared with the general public. Nevertheless, a potential risk of a myocardial involvement cannot be excluded even in asymptomatic athletes.
Keep in mind that myocarditis is one of the leading causes of sport-associated sudden cardiac death in the group of athletes under 35 years of age.11 The clinical presentation of myocarditis in general shows a wide and heterogenic spectrum of symptoms. Athletes frequently present with non-specific symptoms such as fatigue, malaise, reduced performance, muscle soreness, or increased resting heart rate, which can often be misinterpreted in the context of other differential diagnoses (e.g. training-related exhaustion/overtraining, depression, or psychosomatic disorders). Thus, athletes are often not subjected to a COVID-19 test (e.g. nasopharyngeal swab), so that the diagnosis of a COVID-19 infection and a potential COVID-19-associated myocardial involvement or myocarditis cannot be made. In this case, further diagnostic or therapeutic measures can be delayed or even completely neglected.
Myocarditis associated with COVID-19 in athletes
In the reports of severe COVID-19 cases, data on cardiac examinations are often missing. However, a report by Inciardi et al.,12 describing the case of an otherwise healthy 53-year-old white woman with cardiac involvement, lists numerous diagnostic anomalies. Remarkably, cardiac pathology developed 1 week after recovering from influenza-like symptoms. Moreover, there are reported cases of sudden cardiac death in non-hospitalized COVID-19-positive individuals with only mild symptoms.13
Descriptions of mild COVID-19-associated myocarditis are very rare or even non-existent. Nevertheless, in the assessment of eligibility for participation in sport for athletes in recovery from COVID-19, these might be very helpful for further risk stratification and for guiding reintegration to training and competition.
Highlighting the diagnostic dilemma in athletes
COVID-19-associated cardiac injury and its long-term consequences in athletes could be significantly underestimated if the assessment of cardiac injury is defined merely by the presence of elevated troponins.14,15
The assessment of suspected myocarditis in athletes, especially those with mild or no symptoms, can be difficult. Even in cases of a variety of abnormal diagnostic results, myocarditis cannot always be diagnosed with certainty. For example, alterations in the ECG can also be explained by long-term training adaptation.16 Similarly, elevated cardiac biomarkers such as troponin or creatine kinase may also be explained by acute exercise.20
Typical presentation of athletes with suspected myocarditis in the outpatient setting differs from that commonly observed in a hospital setting, specifically regarding the significantly greater frequency of milder disease severity. Athletes are usually highly sensitive to subtle changes in their physical condition or performance. This includes symptoms such as prolonged time to recover, fatigue, or peripheral muscle soreness. The symptoms of COVID-19 are often non-specific, too.17
The difficulty in interpretation of such non-specific symptoms in combination with an unclear diagnosis results from the variety of possible differential diagnoses such as mild myocarditis, COVID-19 without cardiac involvement, or sport-associated symptoms such as fatigue and muscle pain.
In summary there is currently insufficient data available to describe the presentation of clinically mild COVID-associated myocarditis or even to predict its long-term outcome. With regard to consultations with non-specific symptoms in sports medicine outpatient clinics, the differential diagnosis of a past COVID-19 infection and/or a COVID-19-associated myocarditis should be taken into consideration, perhaps even retrospectively, where appropriate. The COVID-19 outbreak and its cardiovascular involvement support the need for further research to fill the currently large gaps of knowledge, particularly with regard to immediate and long-term cardiovascular implications of viral infections in athletes.
What do we know from previous outbreaks of respiratory virus infections?
Data from previous epidemics of corona species [SARS-CoV 2002 or Middle Eastern respiratory syndrome (MERS)-CoV 2012] revealed a significant association between underlying cardiovascular disease, myocardial injury, and worse outcomes.13,18
SARS-CoV might manifest as hypotension, cardiac arrhythmias, and sudden cardiac death.19,20 Data obtained in a rabbit model suggest that coronavirus can induce cardiomyopathy, resulting in dilated cardiac chambers and systolic impairment.21 Reversible cardiomegaly with no clinical evidence of heart failure was also reported in a small group of humans.22 Some of the clinical manifestations, such as sinus tachycardia22 or persistent abnormalities of lipid (68%) and glucose metabolism (60%), as well as cardiovascular abnormalities (40%) at 12-year follow-up, appear to persist beyond the acute phase of infection.23
Currently, we do not know whether COVID-19 has the potential to cause myocarditis and myocarditis-associated long-term consequences even in mild cases. Above all, it is unclear how to rate COVID-19-associated risks in comparison with previous influenza or (other) corona epidemics.
Eligibility for sport in situations of possible myocardial involvement
The question of how to deal with athletes following COVID-19 and how to reintegrate them safely into sports is difficult to answer at the moment.
A helpful orientation for guiding clinical processes are the recommendations proposed by the European Society of Cardiology, the American Heart Association/American College of Cardiology, or the 36th Bethesda Conference (2005).24–27 Whether this approach is also applicable in COVID-19-associated myocarditis is presently unclear. In any case, a careful follow-up of athletes recovering from the current COVID-19 should be performed. As patients with COVID-19 have been reported to develop cardiovascular complications even in the absence of underlying cardiovascular disease, prospective data collection via registries such as CAPACITY-COVID28 appears to be an important approach.
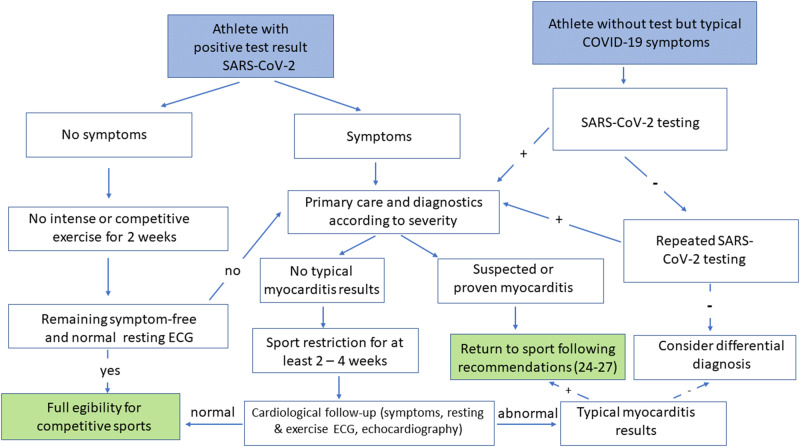
An initial strategy might be to adapt the above-mentioned general recommendations for a return to sport in athletes with (suspected) myocarditis.24–27 We suggest the following approach shown in Figure 1.
Figure 1.
Proposed algorithm for a return to sport for an athlete with positive test result of SARS-CoV-2 or with typical COVID-19 symptoms. Abbreviations: ECG, electrocardiogram; COVID-19, coronavirus disease.
From other virus infections, it is known that viral replication can be enhanced during vigorous activity, resulting in greater structural damage of the heart tissue.29,30 Thus, in the case of an athlete diagnosed with COVID-19, but without any symptoms, we would also recommend refraining from intensive or competitive-like exercise for at least 2 weeks. In the absence of symptoms and abnormalities in the resting ECG at the end of this time period, return to sport can be recommended without restriction.
In any case of myocarditis, a strict ban on sport for a period of at least 3–6 months is recommended based on animal data suggesting a virulence-promoting effect of exercise.29,30 Following the above-mentioned recommendations,24–27 return to training and competition appears to be reasonable if left ventricular function and cardiac dimensions have returned to normal, if clinically relevant arrhythmias are absent in Holter ECG monitoring and exercise test, and if serum markers of inflammation and heart failure have normalized.
In symptomatic COVID-19-positive athletes with no diagnostic evidence of myocarditis, following sport restriction for at least 2–4 weeks, a thorough medical examination (physical examination, resting and exercise ECG, and echocardiography) should be performed before resuming sports activities. Return to sport will be possible in the absence of abnormal results.
It is known that the prognosis of athletes with uncomplicated acute myocarditis and with a complete recovery, including normalized left ventricular function and absence of late gadolinium enhancement, is highly favourable.31,32 Still, in athletes recovering from COVID-19, even without pre-existing diseases, the development of cardiovascular complications and long-term consequences, e.g. arrhythmias, must be taken into consideration and should be ruled out by means of a careful follow-up. In the near future, data about treatment and monitoring of athletes recovering from COVID-19 will be of major importance. Above all, specifically against the background of the wide spectrum of COVID-19 disease manifestations, the questions of eligibility for sport and long-term consequences of COVID-19 for athletes should be addressed.
Summary
The cardiovascular effects and long-term consequences of COVID-19 are currently unclear. The question of eligibility for sport and the point of return to sport following both asymptomatic and symptomatic COVID-19 with or without suspected involvement of the myocardium is currently becoming more and more important in leisure as well as in competitive sports. Fortunately, from previous studies and registries of acute myocarditis, it has been known that athletes with a complete recovery have a very good prognosis. Nevertheless, to optimize counselling and treatment of athletes in the future, prospective data collection on the current corona pandemic is urgently needed. To this end, the non-evidence-based recommendations for a return to sports presented herein might serve as a first guideline.
References
References are available as Supplementary material at European HeartJournal online.


Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.