COVID-19 pandemic is a global public health burden, with progressively growing number of infected subjects, which are often asymptomatic. In this emergency condition, Cardiologists have to improve management of acute coronary syndromes (ACS), in order not only to guarantee the appropriate treatment to ACS patients, but also to protect hospital environment and workers from virus spreading. Accordingly, each patient referred to hospital, or directly sent to Cath lab for invasive coronary angiography, should be regarded as possible COVID-19 carrier, therefore, SARS/CoV2/Nucleic Acid test should be performed before any procedure, standard or total protection personal equipment should be worn by all healthcare workers and patients should be admitted in dedicated COVID Units or similar-wards with the appropriate intensity of care depending on his clinical condition. This document provides a guide for clinicians to manage different cases of STEMI/NSTEMI ACS with potential or known COVID-19 infection, based on recent worldwide evidence and standardization protocols.
The coronavirus disease-2019 (COVID-19) outbreak has become a worldwide healthcare emergency.1,2 The number of severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) cases is rapidly growing, and the majority of them are either asymptomatic or present minor flu-like symptoms.3 In almost 20% of subjects, the disease worsens, leading to clinical complications requiring admission to an intensive care unit (ICU) and ventilatory assistance.3,4 The virus spreads easily from symptomatic patients, through respiratory droplets produced with coughs, sneezes, or sputum, or through close contact with infected people or surfaces.5,6
However, the transmission could occur in the absence of overt symptoms, during the incubation period, from subjects that will never develop symptoms or following an apparent clinical recovery.7–9
In view of this epidemiological scenario, it is necessary to improve the management of patients with acute coronary syndromes (ACS) to prevent the spread of SARS-CoV-2. In our experience, we have considered each ACS patient to be possibly COVID-19 infected. This is of outmost importance for the safety of other hospitalized patients, the hospital environment, and healthcare workers.
Therefore, a cardiologist has to be prepared to manage an emergency situation within a co-existing COVID-19 pandemic, ensuring the appropriate treatment for these patients and, on the other hand, preventing infection of healthcare workers, through the optimization of personal protective equipment (PPE).10–12 The aim of this document is to provide important indications for therapeutic and protective measures to adopt in the case of ACS during the COVID-19 pandemic, based on the newest global evidence and standardization documents.
STEMI and high-risk NSTEMI
Pre-hospital stage
The early admission of patients with suspected ACS, according to the most recent ESC guidelines,14 is implemented by the emergency medical system throughout Europe. In the case of ST-elevation myocardial infarction (STEMI), the ambulance crew should promptly provide to the cardiologist at the hub centre both electrocardiogram (ECG) and clinical information regarding ACS, a detailed history of the patient’s possible contact with COVID-19 illness, and details of the presence of suspected symptoms within the last 14 days.
Likewise, this history screening should be accurately performed in outpatients referred to the emergency department (ED) or transferred from spoke centres.
For NSTEMI with high, intermediate, or low risk, we suggest nasal and/or oropharyngeal swabs if possible before admission to the cardiology department.
A surgical mask must be placed on each patient.
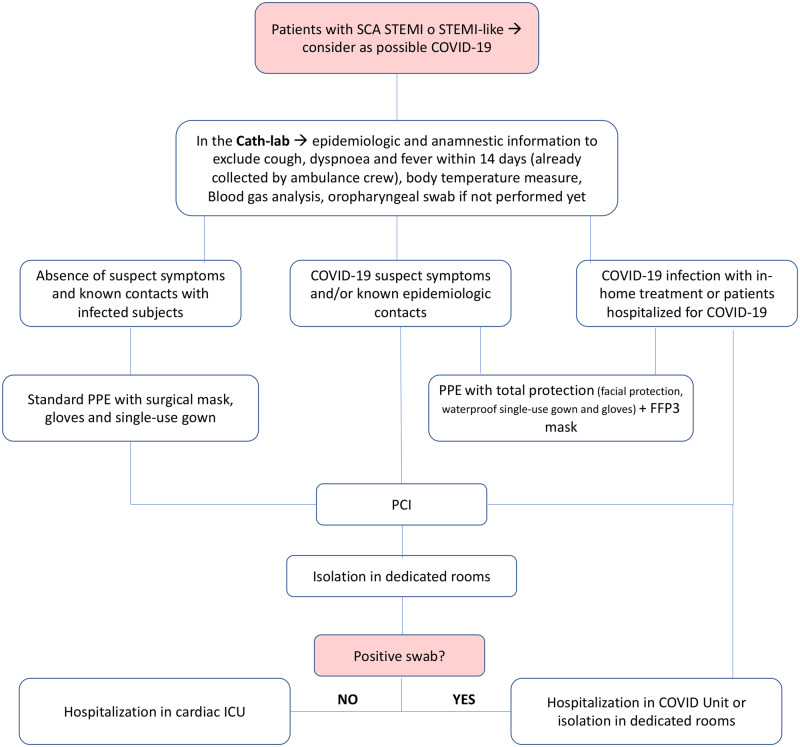
Figure 1.
Algorithm for the management of patients presenting with high-risk acute coronary syndrome (ACS) at the time of COVID-19. ICU, intensive care unit; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary angiography; PPE, personal protective equipment; STEMI, ST-segment elevation myocardial infarction.
In-hospital stage
Following a rapid triage process, ACS patients could be classified into four categories:
STEMI or very-high risk NSTEMI patients (‘STEMI-like’) without COVID-19 and/or known contact with infected subjects healthcare professionals must wear the standard PPE: surgical mask, gloves, cap, goggles, and single-use gown.15,16
STEMI or very-high risk NSTEMI patients with COVID-19 suspected (symptoms and/or known contact with infected subjects) or confirmed infection treated at home healthcare professionals must be equipped with total-protection PPE (i.e. cap, facial protection, waterproof single-use gown, and gloves) and a filtering face piece class 3 (FFP3) mask,15,16 according to current protocols.
STEMI or very-high risk NSTEMI in patients hospitalized for COVID-19 infection healthcare professionals must be equipped with total-protection PPE and an FFP3 mask,15,16, following current protocols.
STEMI or NSTEMI complicated by cardiac arrest healthcare professionals must be equipped with total-protection PPE and an FFP3 mask,15,16 following current protocols, both for intubated and for spontaneously breathing patients (e.g. oxygen therapy with nasal cannula, Venturi mask, non-invasive ventilation (NIV), no oxygen therapy).
On arrival at the Cath lab, vital signs, with particular attention to body temperature and SaO2, should be measured. Furthermore, blood gas analysis and biological specimens (swab) collection for COVID-19 testing should be performed using the necessary PPE according to the severity of respiratory symptoms: (i) low COVID-19 risk, surgical mask; (ii) high COVID-19 risk, PPE with FFP2 or FFP3 mask, depending on the gravity of respiratory impairment. The percutaneous procedure should be performed following the standard protocols of the Centre.
At the end of the invasive coronary angiography, patients with COVID-19 infection should be hospitalized in COVID Units, organized at different levels of care intensity and settings, corresponding to the clinical conditions.
Alternatively, in hospitals without COVID Units, patients should also be hospitalized in COVID-dedicated rooms under the management of specific professionals with the Cardiologist’s support, if not already part of the COVID-Team.
Patients awaiting the COVID-19 test result must be considered as possible COVID-19 carriers, even if asymptomatic; thus, they should be isolated and monitored by dedicated healthcare professionals. If the test is positive, the patients should be admitted to COVID Units or equivalent wards. Asymptomatic patients with negative swabs should be admitted to cardiac ICU.
Patients with negative swab and highly suggestive symptoms for COVID-19 infection should be isolated and undergo a second swab; the destination department for the subsequent admission is to be decided on the basis of the test results.
Finally, in patients hospitalized in a COVID Unit showing signs and symptoms suggestive for STEMI, the risk and benefits of a possible coronary revascularization should be assessed, evaluating the patient’s clinical condition and comorbidities and the risk in transport to the Cath lab.
Thrombolysis could be considered as an alternative to percutaneous coronary intervention;11,12 however, it should be considered that COVID-19 patients, especially those with severe conditions, are at high risk of haemorrhagic and disseminated intravascular coagulation.
In the case of patients with suspected or confirmed SARS-CoV-2, a sanitization of the Cath lab is necessary, according to hospital protocols.
The complete indications for the methods of dressing/undressing of healthcare professionals can be found in specific documents of the Italian Society of Interventional Cardiology (GISE)15 and the National Health Institute (ISS).17
Low- and intermediate-risk NSTEMI
Since patients with low- and intermediate-risk NSTEMI do not need immediate revascularization,18 the stratification to reveal COVID-19 patients should be performed with the same modalities before their transfer to the Cath lab or their admittance to the Cardiology ward, preferably in dedicated areas of the ED. Regarding the protective normative of healthcare professionals, the indications are the same as explained above. While waiting for the SARS-CoV-2 test results, a proper risk assessment should be carried out to identify patients needing expedited angiography and to facilitate earlier discharge.18
Soon after the test results, patients with NSTEMI with a positive COVID-19 test should be admitted to COVID Units within the appropriate care settings, depending on the clinical condition and the thrombotic and arrhythmic risk, evaluating the risk–benefit ratio deriving from a possible revascularization.
Conversely, patients with NSTEMI with a negative COVID-19 test should follow the standard protocol for therapy and will be admitted to the Cardiology department.
Conclusions
In the present global COVID-19 pandemic, a cardiovascular emergency is faced with balancing timeliness of treatment and the safety of other patients and medical personnel. Each patient referred to the ED or directly to the Cath lab requires exclusion of COVID-19 infection, while, in the cases where this is confirmed, specific measures should be undertaken. High protection levels of healthcare workers are required, due to the potential necessity of performing emergency resuscitation measures at any time during the procedure.
This document provides a simple and short guide to assist clinicians in the management of ACS considering COVID-19, based on recent worldwide evidence and protocols of our country.
References
References are available as supplementary material at European Heart Journal online.

Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.