Abstract
We found low prevalence of SARS-CoV-2 (2.7% [5/188]) among pregnant and postpartum patients with universal testing. Prevalence among symptomatic patients was similar under initial targeted screening (22.2% [4/18]) and universal approaches (19.1% [8/42]). Among 170 asymptomatic patients, 2 were positive or inconclusive, respectively; repeat testing at 24 hours was negative.
Keywords: pregnancy, COVID-19, SARS-CoV-2, universal screening, viral shedding
We found a low prevalence of severe acute respiratory syndrome coronavirus 2 among pregnant and postpartum patients after initiation of universal testing at University of Washington–affiliated hospitals using a combination of on-site rapid testing, high-throughput centralized testing, and outpatient drive-through screening prior to admission.
To date, most coronavirus 2019 (COVID-19) reports in pregnancy are case series, with limited insight into population prevalence [1–5]. Reports from New York City described an alarming rate of asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) polymerase chain reaction (PCR)-positive pregnant patients (13.7%–14.5%) [6, 7]. Although Washington State was among the first to confirm community transmission [8], our regional epidemic appears to be slowing with early public health response and widespread testing availability [9]. On 2 March 2020, the University of Washington (UW) Department of Laboratory Medicine obtained emergency use authorization (EUA) for a laboratory-developed SARS-CoV-2 test. Initial testing at UW Medicine focused on symptomatic persons under investigation (PUI), transitioning to universal testing of labor and delivery (L&D) and presurgical patients on 29 March 2020. We present results of L&D SARS-CoV-2 PCR testing from 2 March 2020 through 15 April 2020, encompassing targeted and universal approaches.
METHODS
Study Design and Patients
We performed a retrospective cohort study of SARS-CoV-2 PCR testing of L&D patients at UW Medical Center Montlake and Northwest campuses. The UW Montlake Labor and Delivery unit is a tertiary referral center for high-acuity obstetrical care with approximately 1850 deliveries per year and a cesarean delivery rate of 46%. UW Northwest Birth Center has approximately 1100 deliveries annually of primarily uncomplicated pregnancies, with a cesarean delivery rate of 26%. Patients tested for SARS-CoV-2 from 2 March 2020 through 15 April 2020 were included.
Universal Testing Strategy
UW Montlake initiated universal testing for L&D inpatients on 24 March 2020, followed by full implementation that included outpatient screening of planned admissions on 29 March 2020. UW Northwest implemented universal testing on 2 April 2020. Both campuses had on-site rapid testing available starting on 30 March 2020, preferentially used for L&D. After rapid testing instrument failure on 4 April 2020, UW Northwest reverted to routine testing exclusively. Under universal testing, patients were tested upon hospital admission, or as outpatients, primarily at a drive-through testing center within 48–72 hours of planned admission. Outpatient testing used routine assays located at the off-site centralized UW Virology Laboratory. Patients underwent repeat testing if no result was available within 72 hours of expected delivery or procedure. Known COVID-19 patients underwent repeated testing on admission even if clinically recovered in order to facilitate return to standard precautions and personal protection equipment (PPE) stewardship.
SARS-CoV-2 Testing
Routine centralized UW Virology Laboratory testing used 1 of 3 reverse transcription polymerase chain reaction (RT-PCR) assays depending on instrument availability: Washington state EUA UW Centers for Disease Control and Prevention (CDC)-based laboratory-developed SARS-CoV-2 test or US Food and Drug Administration–authorized Hologic Panther Fusion or Roche cobas SARS-CoV-2 tests. On-site rapid testing used the DiaSorin Simplexa (MDX Liaison) EUA assay with a run time of 75–90 minutes (see Supplementary Materials, SARS-CoV-2 test targets and interpretation).
Data Collection
Eligible patients were identified from outpatient and admission logs of pregnant and postpartum patients. Sociodemographic and clinical characteristics were abstracted from medical records. Test results were queried from the UW Laboratory Medicine data warehouse. Data were entered into Research Electronic Data Capture (REDCap, Vanderbilt University, Nashville, TN) and analyzed with STATA version 15. The UW Institutional Review Board approved the study procedures under a waiver of informed consent.
Statistical Analyses
Patient and testing characteristics were summarized by proportions and medians with interquartile range (IQR) as appropriate. Testing results were characterized as positive, negative, or inconclusive.
RESULTS
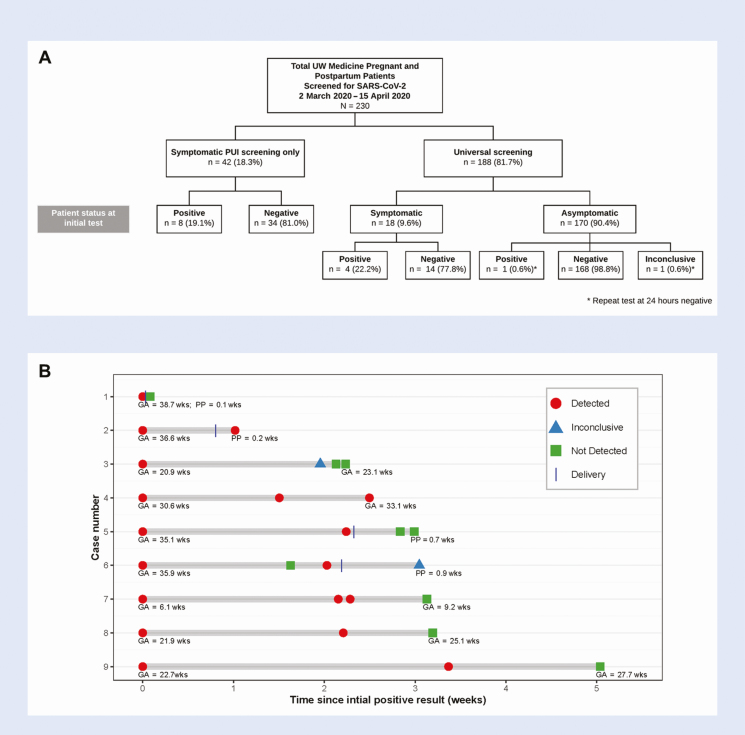
Between 2 March 2020 and 15 April 2020, 230 pregnant and postpartum patients underwent SARS-CoV-2 RT-PCR testing; 42 (18.3%) under the initial targeted symptomatic PUI approach and 188 (81.7%) under universal testing (Figure 1).
Figure 1.
SARS-CoV-2 screening among pregnant and postpartum patients in the UW Medicine system, Seattle, Washington. A, Study flow of pregnant and postpartum patients screened for SARS-CoV-2 prior to and after initiation of universal screening in Seattle. Figure includes results of initial testing only. Among 230 patients, 275 tests were performed. Results of repeat testing are detailed in Supplementary Table 2. B, Results of repeat SARS Co-V-2 RT-PCR testing among initially positive pregnant patients. Timing denotes first and last test performed during the study period by either GA or PP age. Abbreviations: GA, gestational age; PCR, polymerase chain reaction; PP, postpartum; PUI, persons under investigation; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; UW, University of Washington.
Supplementary Table 1 summarizes sociodemographic characteristics, pregnancy status, location, and indication of testing. Among 224 pregnant (median gestational age 37.4 weeks; IQR, 32.9–39.1) and 6 postpartum patients (median postpartum age 1.3 weeks; IQR, 0.0–3.6), the median age was 32 years (IQR, 29–35). Eighty-nine (38.7%) initially tested as outpatients, including 63 (70.8%) with drive-through testing, 16 (7.0%) during emergency room/obstetric triage evaluation that did not require admission, and 125 (54.4%) during admission. More than half of hospitalizations at initial testing were for L&D (66 [52.8%]), followed by antenatal (52 [41.6%]), outpatient/same day procedures (3 [2.4%]), and postpartum admissions (2 [1.6%]).
A total of 184 (80.0%) patients had a pregnancy outcome during the study period; 172 (74.8%) live births, 3 (1.3%) fetal or neonatal demise, 8 (3.5%) termination of pregnancy, and 1 (0.4%) spontaneous abortion; 46 (20.0%) remained pregnant.
Results of SARS-CoV-2 RT-PCR Testing
SARS-CoV-2 prevalence among symptomatic patients during initial targeted PUI screening (19.1% [8/42]) and after universal screening (22.2% [4/18]) was similar (Figure 1). Among 170 asymptomatic patients tested under universal screening, 1 tested positive and 1 inconclusive, with repeat testing at 24 hours negative for both. The asymptomatic positive patient’s initial positive test had a cycle threshold near the detection limit and was negative when retested 24 hours later. Neither patient developed symptoms during the study period.
Thirty patients (13%) underwent repeat testing, with 45 additional tests performed (Supplementary Table 2). Additional testing indications included 6 (13.3%) symptomatic PUI (with negative results), 19 (42.2%) known SARS-CoV-2 positive, 2 (4.3%) previously inconclusive, and 18 (40.0%) for universal screening of asymptomatic patients. Nine patients with initial positive tests underwent retesting; 7 had at least 1 additional positive test, including 6 initially symptomatic patients who remained PCR-positive for ≥2 weeks (Figure 1). No patient with an initial negative or inconclusive test subsequently tested positive.
Among 275 tests performed, 193 (70.2%) patients were tested by routine test and 82 (29.8%) by rapid test. The median turnaround time was 2.5 hours (IQR, 2.0–3.1) for the rapid test and 7.1 hours (IQR, 5.5–9.3) for the routine test (aggregate data reported; disaggregated initial and repeat testing reported in Supplementary Tables 1 and 2).
DISCUSSION
We found low prevalence of SARS-CoV-2 among L&D patients after initiation of universal screening. Universal testing was accomplished using a combination of on-site rapid testing, high-throughput centralized testing, and outpatient drive-through screening prior to admission. This multipronged approach ensured that almost all patients had a known SARS-CoV-2 status prior to delivery or procedure, including patients with precipitous labor and those who required emergent/urgent procedures. Among a small subset of PCR-positive patients who were retested, a high proportion remained positive for ≥2 weeks. While rapid testing aided in short turnaround times, routine testing provided results within 8 hours, further improved to approximately 6 hours by study end as laboratory capacity increased. This approach was feasible and yielded valuable real-time data on SARS-CoV-2 status, enabling judicious PPE use.
Our study has some features that were similar to those in recent reports from New York, including universal screening of all L&D patients [6, 7]; however, prevalence of confirmed SARS-CoV-2 among both symptomatic and asymptomatic patients differed substantially. The positive rate for symptomatic patients in our study was 19.1%–22.2%, in contrast to reported rates of 68.8% (11/16) and 100% (4/4) in New York City [6, 7]. Only 1.2% of asymptomatic women tested positive or inconclusive for SARS-CoV-2 in our study compared with 13.7%–14.5% in New York City reports, and neither patient was positive upon retesting at 24 hours. Our lower SARS-CoV-2 prevalence among pregnant and postpartum patients likely reflects local epidemic dynamics, including potentially earlier community spread, but currently lower prevalence within our region. We estimate that the average population prevalence in greater Seattle and King County between 23 March 2020 and 9 April 2020 was 0.24% (95% confidence interval, .05%–.75%), with evidence of continued decline [9].
PCR-based diagnostics are limited in their ability to differentiate infectious SARS-CoV-2 virus from persistent viral shedding in the setting of clinically recovered COVID-19 patients that likely poses a markedly decreased risk of person-to-person transmission. While we routinely retest known COVID-19 patients on admission and prior to procedures to inform infection prevention practices, the clinical significance of persistently positive PCR in the setting of clinical improvement, including among L&D patients, is unknown [10]. Our institutional practice is to maintain COVID-19 precautions using a test-based strategy and to counsel patients per CDC guidance that the risk of transmission is substantially reduced after 10 days of symptom onset and >72 hours after symptom resolution [11].
Universal SARS-CoV-2 testing of pregnant and postpartum patients occurred in conjunction with testing of all presurgical patients to reduce risk of SARS-CoV-2 transmission from intubation for general anesthesia, an aerosol-generating procedure. The presurgical universal SARS-CoV-2 screening policy was extended to L&D patients with the rationale that many require cesarean delivery or other surgical procedures and may potentially require urgent general anesthesia. Our cesarean delivery rate of 26%–46% illustrates the frequency of surgery during a delivery hospitalization. The American College of Obstetricians and Gynecologists recently strengthened their recommendations regarding testing on L&D units [12]. Our current institution-wide screening approach continues to evolve in response to local epidemiology and testing availability and now includes universal screening of all hospital admissions. Our most recent estimates suggest that <1% of asymptomatic patients have tested positive since initiation of universal screening. Early adoption of universal screening (starting with surgical and L&D patients) allowed data-driven decisions to be made informing PPE use to ensure protection of patients and healthcare workers, including those on L&D-related units (ie, newborn nursery and neonatal intensive care unit). Further, this information aided in counseling regarding risks and benefits of infant separation/co-location and breastfeeding practices, using a shared-decision making approach. Despite low numbers of additional cases identified, universal screening of pregnant patients provides important surveillance information due to the representativeness of this population to the greater community.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author Contributions. S. M. L., A. K., L. S., M. B., A. M., K. A. W., and J. H. drafted the initial manuscript. All authors reviewed, contributed to revision, and approved the final manuscript. S. M. L. had full access to the manuscript and had final responsibility for the decision to submit for publication.
Acknowledgements. The authors acknowledge the following: Nicole Wothe and Brian Reed for administrative support, Jaclyn Escudero for assistance with figures, Grace John-Stewart for editorial advice, Ashleigh Lewis for Research Electronic Data Capture (REDCap) assistance, and Loren Balcom and Melissa Habrat for assistance with data and honest broker review, respectively. We also thank the Washington State COVID-19 in Pregnancy Collaborative, which helped to provide infrastructure for chart abstraction.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases (grants AI133976, AI145890, AI144938, and AI143265 to K. A. W. and AI120793 to S. M. L.). Study data were managed using a REDCap electronic data capture tool hosted by the Institute of Translational Health Sciences at the University of Washington, which was supported by the National Center for Advancing Translational Sciences (UL1TR002319).
Potential conflicts of interest. A. K. has been a consultant for Pfizer and GlaxoSmithKline, outside the submitted work. A. L. G. reports personal fees from Abbott Molecular, outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Li N, Han L, Peng M, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin Infect Dis 2020. DOI: 10.1093/cid/ciaa352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yu N, Li W, Kang Q, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis 2020. DOI: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM 2020: 100118. DOI: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen L, Li Q, Zheng D, et al. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med 2020. DOI: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand 2020. DOI: 10.1111/aogs.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vintzileos WS, Muscat J, Hoffmann E, et al. Screening all pregnant women admitted to labor and delivery for the virus responsible for COVID-19. Am J Obstet Gynecol 2020. DOI: 10.1016/j.ajog.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sutton D, Fuchs K, D’Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med 2020. DOI: 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382(10):929–36 DOI: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Greater Seattle Coronavirus Assessment Network (SCAN) Technical Report, April 17, 2020. Available at: https://publichealthinsider.com/wp-content/uploads/2020/04/SCAN-Technical-Report-v1-17-APR-2020.pdf. Accessed 28 April 2020.
- 10. Wolfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020. DOI: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Symptom-Based Strategy to Discontinue Isolation for Persons with COVID-19. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/strategy-discontinue-isolation.html. Accessed 20 May 2020.
- 12. American College of Obstetricians and Gynecologists. Novel Coronavirus 2019 (COVID-19): Practice Advisory April 2020. (last updated April 23, 2020). Available at: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019. Accessed 24 April 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.