Abstract
Expression of angiotensin-converting enzyme 2, receptor of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is high in the testes, therefore SARS-CoV-2 infection and its association with male reproductive health should be investigated in male coronavirus disease 2019 patients.
Keywords: ACE2, SARS-CoV-2, testis, Leydig cells, cytokines and infertility
Outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first appeared in Wuhan province, China, in December 2019. Since then, the outbreak has spread worldwide and precipitated into a global pandemic. The mortality rate of SARS-CoV-2 disease (coronavirus disease 2019 [COVID-19]) in different countries has been reported to be between 1 and 4%, with increased risk of severe disease among the elderly and those with preexisting health conditions [1]. The demographic profile of COVID-19 reveals disproportionately higher number of males with severe disease and deaths [1].
SARS-CoV-2 infection is robust in cells expressing angiotensin-converting enzyme 2 (ACE2) receptor, a type I integral membrane protein that controls cardiac and kidney functions by negatively regulating renin-angiotensin systems [2]. During virus entry, the coronavirus spike protein (S protein) requires priming and cleavage at the S1/S2 site of the protein by transmembrane protease serine 2 (TMPRSS2). The S1 site contains a receptor-binding domain, which then binds to the ACE2 and facilitates virus entry into the cell [2]. Expression of ACE2 is cell-type specific and the cells with high ACE2 expression include type II alveolar epithelial cells, renal tubular and intestinal epithelial cells, vascular smooth muscle cells, and cardiomyocytes [3]. High ACE2 expression may augment virus infection in the lung, heart, and small intestine that might explain the pathophysiology of acute lung and myocardial injury, and gastrointestinal symptoms reported in COVID-19 patients [1].
The testis is also one of the organs with high levels of constitutive expression of ACE2 [2, 4]. Physiological functions of ACE2 in Leydig cells (LC) include regulating testosterone (T) production and local vascular regulatory system to balance interstitial fluid volume via modulating conversion of Angiotensin II to Angiotensin I [5]. Our microarray transcriptome analysis also confirms the presence of extremely high levels of ACE2 transcripts in the normal adult testes (Figure 1A). A recent study used previous single-cell RNA-sequencing profiling data of human testes to show predominant expression of ACE2 in spermatogonia (Spg), LC, and Sertoli cells (SC). Downregulation of ACE2 expression in LC is correlated with severe spermatogenesis impairment in men [5]. Wang et al. [4] further suggested that not all LC and SC were ACE-positive; however, ACE2-positive cells expressed a higher number of genes associated with viral replication and transmission. In addition to ACE2, TMPRSS2 is also expressed in spermatogonia, LC, and SC indicating the potential for coronavirus entry into these cells [4].
Figure 1.
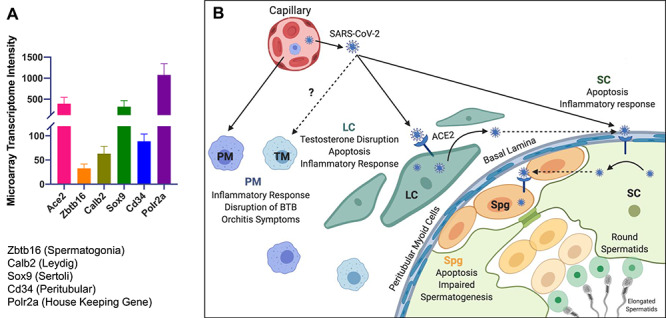
(A) Comparison of ACE2 and cells-specific gene expression in normal adult human testes (n = 3) using microarray profiling assay. It shows the average (standard error of mean) of intensity values of target genes, including ACE2 (Angiotensin I converting enzyme 2), Zbtb16 (Zinc finger and BTB domain containing 16; Plzf), Calb2 (calbindin 2; Calretinin), Sox9 (SRY-box transcription factor 9), Cd34, and house-keeping Polr2a (RNA polymerase II subunit A). (B) Hypothetical model of SARS-CoV-2 testicular infection based on data from other coronaviruses. ACE2 expressing LC in the interstitium are one of the targets of cell free SARS-CoV-2 infection that leads to LC dysfunction including impaired steroidogenesis, inflammatory response and/or apoptosis. SARS-CoV-2 also infects ACE expressing cells of seminiferous tubules including Sertoli cells (SC) and spermatogonia cells (Spg) that may cause production of inflammatory cytokines, transient blood–testis barrier disruption, and germ cell depletion thus leading to impaired spermatogenesis. SARS-CoV-2 infection-associated inflammatory response in the testes may result in increased recruitment of the peripheral immune cells including peripheral macrophages (PM) and virus-specific T cells (not shown here) that may facilitate virus clearance. Virus may not directly infect testicular macrophages (TM) but they play a role in suppressing the inflammatory response and limiting the testicular damage.
The outbreak of SARS-CoV-2 is still ongoing, therefore the data on testicular infection of SARS-CoV-2 are limited. So far, there are only two studies that have assessed viral RNA in the semen. The first study from China by Pan et al. [6] reported that SARS-CoV-2 was not detected in the semen collected between 8 and 75 days (median 31 days) after COVID-19 diagnosis from any of 34 patients with mild–moderate symptoms. Interestingly, 19% of these patients reported scrotal discomfort as one of their symptoms around the time of COVID-19 diagnosis. In the second study, 12 patients with asymptomatic to mild COVID-19 disease in Wuhan were tested for SARS-CoV-2 RNA in their semen 14 to 42 days after COVID-19 diagnosis [7]. None of them were positive for COVID-19 in the semen. Neither study measured any other semen parameters including sperm concentration, motility, or serum hormone levels. However, a recent report from 81 moderate-to-severe COVID-19 adult male patients and 100 age-matched healthy men documented that serum luteinizing hormone (LH) was significantly increased, whereas the ratio of T to LH (T/LH) and ratio of follicle-stimulating hormone (FSH) to LH (FSH/LH) were dramatically decreased in males with COVID-19 [8]. It was also found that serum testosterone levels did not differ between the COVID-19 and control groups. Elevated serum LH and decreased T/LH ratio are often clinical indicators of primary hypogonadism, suggesting testicular failure with LC involvement. This was the first study that provides strong evidence that acute SARS-CoV-2 infection can lead to dysregulation of male sex hormones, however it is important to repeat these measurements at least 3–6 months post recovery.
Although SARS-CoV-2 is not detected in the semen of recovered men, it does not rule out the possibility of testicular infection during the early and symptomatic stage of disease when other organs including heart and lung are infected. At least three studies have reported the presence of SARS-CoV, another pathogenic coronavirus, in the testes [9]. In the study by Xu et al. [9], testes from all six SARS-CoV patients displayed signs of orchitis and testicular damage including germ cell depletion and apoptotic death, and leukocyte infiltration in the interstitium. These findings set a precedent of coronavirus-induced orchitis and testicular dysfunctions.
Since ACE2 expression is high in testis, we speculate that during peak viremia, SARS-CoV-2 reaches testicular interstitium via blood route and LC might be one of the first target in the testes (Figure 1B). Virus infection in the LC may cause alterations in the steroidogenic pathways that may also explain the LC dysfunction and decreased serum T/LH ratio as reported by Ma and colleagues [8]. In addition, virus may infect SC, another ACE2 expressing cell type in the seminiferous tubules. Cytokines and chemokines induced by SARS-CoV-2 entry into the LC and SC may recruit peripheral immune cells including macrophages and virus-specific T cells that may further potentiate inflammation and orchitis in accordance with reported symptoms from 19% of patients in study by Pan et al. [6] but may also facilitate virus clearance. Since orchitis is not a common symptom reported in COVID-19 males, it is likely that the immunosuppressive properties of SC and testicular macrophages may play a critical role in suppressing inflammation and limiting virus-associated testicular damage unlike other organs. However, SARS-CoV-2-associated inflammation might transiently affect blood–testis barrier (BTB) integrity that may affect spermatogenesis. Therefore, urinogenital manifestations should be investigated in young men with COVID-19. Further studies using both in vitro 3D models [10] and animal models are warranted to characterize the effect of SARS-CoV-2 infection on testes function including hormone production, BTB integrity, and germ cell depletion to improve our understanding of the effect of this virus on reproductive health.
Acknowledgments
We appreciate Professor Stuart Howards (University of Virginia and Wake Forest School of Medicine) for his critical comments on this manuscript. Figure 1B was designed by authors using Biorender.com.
Conflict of interest
The authors have declared no conflict of interest.
Footnotes
† Grant Support: internal Funding Wake Forest Baptist Health University. This work was also supported by grants from R21AI140248-02 , NIAID, NIH (Verma/Sadri-Ardekani).
References
- 1. Borges do Nascimento IJ, Cacic N, Abdulazeem HM, Groote TC, Jayarajah U, Weerasekara I, Esfahani MA, Civile VT, Marusic A, Jeroncic A, Carvas Junior N, Pericic TP et al. Novel coronavirus infection (COVID-19) in humans: A scoping review and meta-analysis. J Clin Med 2020; 9:E941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen Y, Guo Y, Pan Y, Zhao ZJ. Structure analysis of the receptor binding of 2019-nCoV. Biochem Biophys Res Commun 2020; 525:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Qi F, Qian S, Zhang S, Zhang Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun 2020; 526:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in Spermatogonia, Leydig and Sertoli cells. Cells 2020; 9:920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pan PP, Zhan QT, Le F, Zheng YM, Jin F. Angiotensin-converting enzymes play a dominant role in fertility. Int J Mol Sci 2013; 14:21071–21086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan FXX, Guo J, Song Y, Li H, Patel DP, Spivak AM, Alukal JP, Zhang XXC, Li PS, Hotaling JM. No evidence of SARS-CoV-2 in semen of males recovering from COVID-19. Fertility and Sterility 2020. doi: 10.1016/j.fertnstert.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Song C, Wang Y, Li W, Hu B, Chen G, Xia P, Wang W, Li C, Diao F, Hu Z, Yang X, Yao B et al. Absence of 2019 novel coronavirus in semen and testes of COVID-19 patients. Biol Reprod 2020. doi: 10.1093/biolre/ioaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ma L, Xie W, Li D, Shi L, Mao Y, Xiong Y, Zhang Y, Zhang M. Effect of SARS-CoV-2 infection upon male gonadal function: A single center-based study. medRxiv 2020. doi: 10.1101/2020.03.21.20037267. [DOI] [Google Scholar]
- 9. Xu J, Qi L, Chi X, Yang J, Wei X, Gong E, Peh S, Gu J. Orchitis: A complication of severe acute respiratory syndrome (SARS). Biol Reprod 2006; 74:410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Strange DP, Zarandi NP, Trivedi G, Atala A, Bishop CE, Sadri-Ardekani H, Verma S. Human testicular organoid system as a novel tool to study Zika virus pathogenesis. Emerg Microbes Infect 2018; 7:82. [DOI] [PMC free article] [PubMed] [Google Scholar]


