Abstract
Background. To inform planning for an influenza pandemic, we estimated US demand for N95 filtering facepiece respirators (respirators) by healthcare and emergency services personnel and need for surgical masks by pandemic patients seeking care.
Methods. We used a spreadsheet-based model to estimate demand for 3 scenarios of respirator use: base case (usage approximately follows epidemic curve), intermediate demand (usage rises to epidemic peak and then remains constant), and maximum demand (all healthcare workers use respirators from pandemic onset). We assumed that in the base case scenario, up to 16 respirators would be required per day per intensive care unit patient and 8 per day per general ward patient. Outpatient healthcare workers and emergency services personnel would require 4 respirators per day. Patients would require 1.2 surgical masks per day.
Results and Conclusions. Assuming that 20% to 30% of the population would become ill, 1.7 to 3.5 billion respirators would be needed in the base case scenario, 2.6 to 4.3 billion in the intermediate demand scenario, and up to 7.3 billion in the maximum demand scenario (for all scenarios, between 0.1 and 0.4 billion surgical masks would be required for patients). For pandemics with a lower attack rate and fewer cases (eg, 2009-like pandemic), the number of respirators needed would be higher because the pandemic would have longer duration. Providing these numbers of respirators and surgical masks represents a logistic challenge for US public health agencies. Public health officials must urgently consider alternative use strategies for respirators and surgical masks during a pandemic that may vary from current practices.
Keywords: influenza pandemic, respiratory protective devices
From April 2013 to June 2014, there have been 450 cases and 165 deaths attributed to influenza A (variant H7N9), a virus not previously reported in humans [1]. The US Centers for Disease Control and Prevention (CDC) examined the potential effect on public health should sustained human to human transmission of this novel influenza strain be observed and determined the options for mitigating its spread domestically under this scenario. As part of this effort, we estimated the potential demand for N95 filtering facepiece respirators (N95 FFRs, hereby called respirators) and surgical masks by healthcare personnel, critical first responders—such as emergency medical services (EMS), police, and fire personnel, and for surgical masks for suspected pandemic influenza patients, in a variety of potential pandemic scenarios, and under various utilization behaviors. N95 Filtering Facepiece Respirators are one of the most commonly used respiratory devices available and are so named because they are intended to prevent the user from exposure to pathogens by filtering at least 95% of airborne particles that pass through the filter media. There are other types of respirators that may be used for personal protection. Besides disposable N95 FFRs, there are reusable elastic or rubber respirators (often called elastomeric respirators) and powered air-purifying respirators (PAPRs).
Respirators, in conjunction with environmental and administrative controls, are considered to be an important component of infection control strategy for healthcare and response workers during an influenza pandemic. During the 2009 H1N1 pandemic, CDC recommended respirators to healthcare workers (HCWs) and first responders when “caring for persons with known, probable or suspected 2009 H1N1 or influenza-like illness (ILI)” [2]. Similar recommendations are likely to be made during the next pandemic.
To date, the few studies that have quantified the potential demand for respirators and surgical masks in the event of an influenza pandemic have either assumed constant respirator and surgical mask use or use proportional to the epidemiologic curve of the pandemic [3–7] (see Supplementary Appendix I for a review). We present a model that provides estimates of the potential demand for respirators and surgical masks during a pandemic for a variety of severity and attack rate scenarios. These estimates will aid public health officials to plan how many respirators and surgical masks to stockpile and provide the basis for plans to quickly dispense them.
METHODS
Modeling Approach Overview
We developed a spreadsheet model (Microsoft Excel, Microsoft Corp., Redmond, Washington) to estimate the demand during an influenza pandemic for respirators and surgical masks. We used 4 standardized pandemic scenarios [8], with 2 attack rates (20%, 30%) and 2 levels of severity (defined by hospitalization, emergency department [ED] visits, and EMS transportation rates, see Table 1). To estimate the number of pandemic cases, the 4 scenarios (standard across all influenza modeling activities) were characterized as follows: (1) high clinical severity, 30% (high) attack rate, (2) low clinical severity, 20% (low) attack rate, (3) high clinical severity, 20% attack rate, and (4) low clinical severity 30% attack rate (Table 1) [8]. The resulting estimated epidemiologic curves did not take into account any mitigation efforts, such as vaccine or nonpharmaceutical control measures, and were 41–45 weeks in duration for the low attack rate scenario (peak: 20–23 weeks) and 26–29 weeks in duration for the high attack rate scenario (peak: 12–14 weeks).
Table 1.
Input Parameters Used to Calculate the Number of Patients With ILI Interacting With Healthcare Personnel in Different Settings and Usage by Scenario
| Input | Lower Bound | Upper Bound | Source |
|---|---|---|---|
| Low severity scenario | |||
| % cases, hospitalized | 0.8 | 1.5 | [9] |
| % cases, visit EDa | 6 | 12 | [10] |
| % cases, transported by EMSb | 1 | 2 | [11] |
| High severity scenario | |||
| % cases, hospitalized | 3 | 5 | [9] |
| % cases, visit EDa | 24 | 39 | [10] |
| % cases, transported by EMSb | 2 | 4 | [11] |
| All scenarios | |||
| Pandemic case to ILI case multiplierc | 1.39 | 1.70 | [12] |
| % cases, seek outpatient care | 40 | 56 | [13] |
| % of hospitalizations requiring ICU | 20 | 26 | [14–16] |
| Length of stay (days) | |||
| ED | 1 | ||
| ICU | 8 | 10 | Adapted from [17] |
| General ward | 7 | 11 | Adapted from [17] |
| Workforce | |||
| Police officers in US (millions)d/% with public contact | 0.45/90 | 0.58/90 | [18, 19] |
| Firefighters in US (millions)e/% with public contact | 0.34/90 | 1.10/90 | [19, 20] |
| Hospital Workersf/% with patient contact | 6 053 103/33 | [19, 21] | |
| Outpatient healthcare workersg/% with patient contact | 3 205 399/67 | [19, 21] | |
| ED workers/% with patient contact | 131 588/100 | [22, 23] (as) | |
| EMS workersh/% with patient contact | 296 937/90 | [21] (as) | |
| Nursing home workersi/% with patient contact | 3 426 571/25 | [19, 21] | |
| Demographics | |||
| United States population (millions) | 316 | [24] | |
| % United States population 65+, in nursing homes | 4 | [25, 26] | |
Abbreviations: (as), assumed; ED, emergency department; EMS, emergency medical service; ICU, intensive care unit; ILI, influenza-like illness.
a The number of ED visits was considered to be 7.8 greater than the number of Hospital Visits.
b Approximately 12% of ED patients were transported by EMS.
c At peak, 72% of specimens tested positive for influenza. 20% reduction assumed for upper bound of multiplier. For the sensitivity analysis, we considered a time varying pandemic case to ILI multiplier between 5.00 (in the beginning and end of the pandemic most cases are ILI, values adapted from [12, 17]), and 1.39 at peak.
d Police officers: lower bound = # of sworn officers; higher bound = # of sworn officers and civilian police officers.
e Firefighters: lower bound = # of professional firefighters; higher bound = # of professional firefighters and volunteer firefighters.
f Includes workers in NAICS 622 (Hospitals). Includes Federal, State, Local, and Private Institutions, for 2013. (NAICS: North American Industry Classification System).
g Includes workers in NAICS 6211 (Office of Physicians) and NAICS 6214 (Outpatient care centers). Includes Federal, State, Local, and Private Institutions, for 2013.
h Includes workers in NAICS 621 493 (Freestanding emergency medical centers) and NAICS 62 191 (Ambulance Services). Includes Federal, State, Local, and Private Institutions, for 2013.
i Includes workers in NAICS 623 (Nursing and residential care facilities). Includes Federal, State, Local, and Private Institutions, for 2013.
Our model estimated need for respirators by personnel working in hospital intensive care units (ICU), hospital general wards (GW), EDs, outpatient care settings, nursing homes, and by first responders (eg, EMS, police officers, and firefighters). We also calculated surgical mask demand used in an attempt to slow onward disease transmission, for patients with suspected infection with the pandemic strain (“source control”).
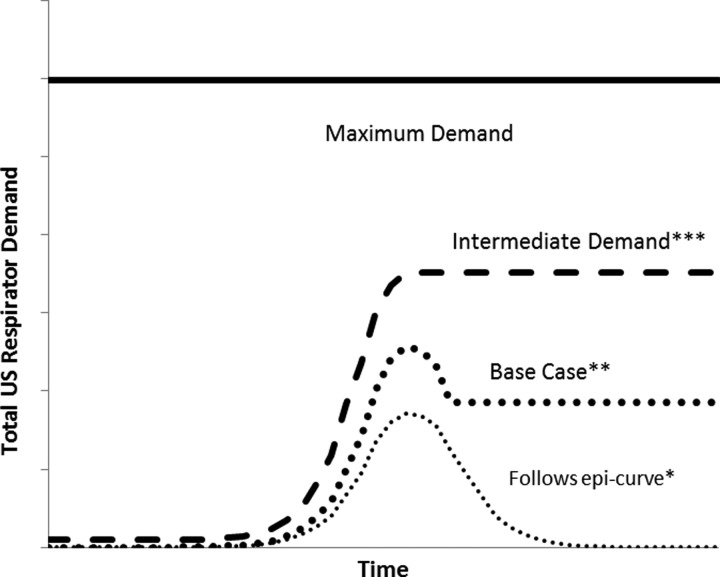
For each of the 4 pandemic scenarios, we modeled 3 respirator distribution scenarios: base case, intermediate demand, and maximum demand scenarios (Figure 1). In the base case distribution scenario, overall demand for respirators was proportionate to the number of patients over time until shortly after the pandemic peaked and then constant afterward. This relayed the fact that, in some sectors (ICU, GW, and nursing homes), testing patients for infection with the pandemic strain would be possible, whereas, in others (ED, first responders, and in outpatient care settings), testing would not be available or feasible on-site. In the latter, supply of respirators for HCWs was assumed to grow with the epidemic curve until it peaked, and to remain stable once there was a perception of need (after the peak). Total respirator need was the sum of the demand in all sectors (see Supplementary Appendix II for details).
Figure 1.
Schematic of alternative structures to modeling total N95 filtering facepiece respirators (respirators) use. *Example of demand that follows the epidemic curve. **In the Base Case, demand for respirators among intensive care unit, general ward, and nursing home workers was assumed to follow the epidemic curve; demand for respirators among first responders and those working in outpatient settings was assumed to follow the Intermediate Demand model. ***All sectors assumed to follow the Intermediate Demand model.
For our intermediate demand model, we assumed the demand for respirators would start with the pandemic and would increase proportionally to the epidemic curve until peak usage. Thereafter, and until the end of the pandemic, demand among all healthcare, ED workers, and first responders remained equal to peak demand (Figure 1, Supplementary Appendix II). This is different from the base case model, which considered that, for the ICU, GW, and nursing homes, need was proportional to pandemic patients throughout the pandemic. We assumed, for the maximum demand scenario, that all eligible healthcare and emergency response workers would use respirators from the beginning of the pandemic until its end, regardless of how many contacts they had with patients who were clinically ill with pandemic influenza (ie, maximum precaution scenario; Figure 1). We assumed that usage rates remained the same throughout the pandemic by HCWs and patients (Table 2).
Table 2.
Input Respirator and Surgical Mask Usage Parameters by Settinga
| Variable (Unit) | Respirators |
Surgical Masks |
Source | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | ||
| Base case | |||||
| ICU (per patient/day) | 12 | 16 | 2 | 2 | CDC Task Force |
| GW (per patient/day) | 8 | 8 | 2 | 2 | |
| ED (per worker/day; per patient/day) | 4 | 4 | 1.2b | 1.2b | |
| Outpatient (per worker/day; per patient visit) | 4 | 4 | 1.2b | 1.2b | |
| Nursing homes (per patient) | 3 | 4 | 1.2b | 1.2b | |
| EMS (per worker/day; per patient/day) | 4 | 4 | 1.2b | 1.2b | |
| Police (per worker/day) | 4 | 4 | 0 | 0 | |
| Fire personnel (per worker/day) | 4 | 4 | 0 | 0 | |
| Maximum demand and intermediate demand | |||||
| ICU (per worker/day) | 4 | 4 | [19], CDC Taskforce | ||
| GW (per worker/day) | 4 | 4 | |||
| ED (per worker/day) | 4 | 4 | |||
| Outpatient (per worker/day) | 4 | 4 | |||
| Nursing homes (per worker/day) | 1 | 1 | |||
| EMS (per worker/day) | 4 | 4 | |||
| Police (per worker/day) | 4 | 4 | |||
| Fire personnel (per worker/day) | 4 | 4 | |||
Abbreviations: CDC, Centers for Disease Control and Prevention; ED, emergency department; EMS, emergency medical service; GW, general ward; ICU, intensive care unit.
a All values held constant throughout the pandemic.
b Not a whole number on account of patients being accompanied by additional persons (eg, family members) who would be provided masks as well.
Finally, we conducted sensitivity analyses in which we analyzed the effect of demand reduction strategies, such as using respirators by HCWs for more than 1 patient contact.
Base Case
For the base case scenario, we estimated demand for respirators among ICU, GW, and nursing home workers by multiplying predicted number of pandemic patients per day by the number of times patients had contact with providers (Supplementary Appendix II). As a result, in the ICU, GW, and nursing homes, total demand was proportional to the total number of patient-provider encounters. We assumed that patients in ICUs had contact with 12 to 16 HCWs per day (Table 2), and so 12–16 respirators would be needed in the ICU per patient per day (each provider is assumed to need one respirator per patient encounter). We assumed patients in GWs had contact with 8 HCWs per day (Table 2). We used a range of length-of-stay of 8–10 days for ICU patients, and 7–11 days for GW patients (Table 1).
We assumed that HCWs in EDs, outpatients settings, as well as first responders, used 4 respirators per day at the beginning of the pandemic (Table 2). We further assumed that the number of workers having contact with pandemic patients would proportionally increase as the number of pandemic patients increased (ie, follow the epidemic curve upward). After the pandemic peaked, the number of workers using respirators would remain fixed. Finally, we considered that only 90% of first responders, 67% of HCWs in outpatient settings, 25% of nursing home workers, and 100% of ED workers would have contact with patients (Tables 1 and 2).
HCWs in EDs, nursing homes, and outpatients settings, as well as first responders are likely to deal with patients with influenza-like illness (ILI), in addition to those with confirmed influenza. We used data from the 2009 H1N1 pandemic and assumed that there were 1.39 to 1.7 patients with ILI for each case of pandemic influenza (Table 1; [12]). We also assumed, for the same calculations, that 40%–56% of all pandemic patients would seek medical care [13]. We supposed, for all 3 scenarios, that changes in pandemic severity affected hospitalization, ED, and transportation by EMS rates but did not affect the proportion of ILI patients interacting in outpatient settings.
Intermediate Demand
For this scenario, we assumed respirator use among all HCWs and first responders increased proportionally to the epidemic curve until the pandemic peaked. Thereafter, and until the end of the pandemic, demand remained equal to peak demand. HCWs in nursing homes were assumed to use 1 respirator per day, all others were assumed to use 4 respirators per day (Table 2).
Maximum Demand
For the Maximum Demand scenario, we assumed the need for respirators across all HCWs and first responders was constant throughout the pandemic. As in the Intermediate Demand scenario, all HCWs (but workers in nursing homes) were assumed to need 4 respirators per day (Table 2).
Demand for Surgical Masks
For all scenarios, we estimated the number of surgical masks required for source control in all settings (hospital, nursing homes, outpatient settings, and EMS) by multiplying the weekly number of ILI patients by the number of masks per patient per day and by the number of days patients would spend in each setting (Table 1).
Sensitivity Analysis
Demand Reduction Strategies for Respirators in the Base Case
To characterize the lowest bound of needed supply of respirators, we chose the base case distribution scenario to evaluate 3 additional strategies designed to potentially reduce respirator demand. Demand reduction strategy 1 included using the same respirator to attend to several patients in different settings such as the ICU, GW, ED, nursing homes, outpatient clinics, and police and fire (Supplementary Appendix III: Table AIII-1), donning (putting on), and doffing (removing) the respirator in between patients (limited FFR reuse [27–29]). Demand reduction strategy 2 consisted of limited respirator reuse by personnel in the hospital settings (ICU, GW, ED) and nursing homes; and use of surgical masks instead of respirators in outpatient clinics and by EMS, fire, and police responders, with removing and putting on the same surgical mask for different suspected pandemic patients in these settings. Surgical mask use was also included for source control in all settings. Finally, demand reduction strategy 3 consisted of substituting respirators with elastomeric respirators (a reusable respirator that can provide N95 or higher level of protection and that could be issued to an individual HCW for use throughout a pandemic or shared between HCWs after following the manufacturer's recommendations for disinfection) in the ICU and ED settings, limited reuse of respirators in hospital GWs, in nursing homes, and EMS settings, and use of surgical masks in outpatient clinics and by fire and police responders, with removing and putting on the same surgical mask for different suspected pandemic patients in these settings. Again, use of surgical masks was included for source control, as in the second demand reduction strategy (Supplementary Appendix III: Table AIII-1).
Respirator and Surgical Mask Usage Rates
We conducted a univariate sensitivity analysis to examine the effect of respirator usage rates on total demand in the base case scenario. We chose the high severity and low attack rate scenario for this analysis and decreased/increased the lower bound of usage rates in each setting by a factor of 50%. We also compared results obtained with the assumed rates of usage with results found using rates adapted from the literature (Supplementary Appendix III: Table AIII-2, Appendix I). Separately, we analyzed the impact of assuming a time varying ILI to case ratio on the estimates and varied this ratio between a maximum of 5.00 in the beginning and end of the pandemic (20% of all cases seen are pandemic cases) and minimum of 1.39 during the peak (72% of all cases are pandemic cases).
RESULTS
In the low attack rate/low severity scenario, the pandemic caused around 63 million symptomatic cases, 0.5–1.0 million hospitalizations, and 0.1–0.3 million ICU admissions. In the high attack rate/high severity scenario, the pandemic caused approximately 94 million symptomatic cases, 2.8–4.7 million hospitalizations, and 0.6–1.2 million ICU admissions [8].
Base Case, Intermediate, and Maximum Demand Scenarios
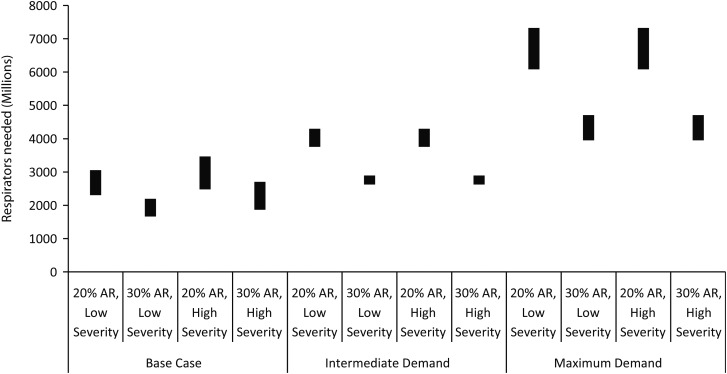
In the base case, the estimated total demand for respirators ranged from 1.7 billion (lower bound) in the high attack rate/low severity scenario to 3.5 billion (higher bound) in the low attack rate/high severity scenario (Figure 2). The estimated need for respirators was higher for the low attack rate/low severity scenario than for the high attack rate/high severity scenario because of differences in pandemic duration: 41–45 weeks for the low attack rate and 26–29 weeks for the high attack rate scenario. For all scenarios, 0.1–0.4 billion surgical masks would be needed for source control (Figure 3).
Figure 2.
Demand for N95 filtering facepiece respirators (respirators) for different models and scenarios. For each scenario and distribution model, ranges result from variations in respirator use rates and epidemiologic and healthcare use parameters. Abbreviation: AR, attack rate.
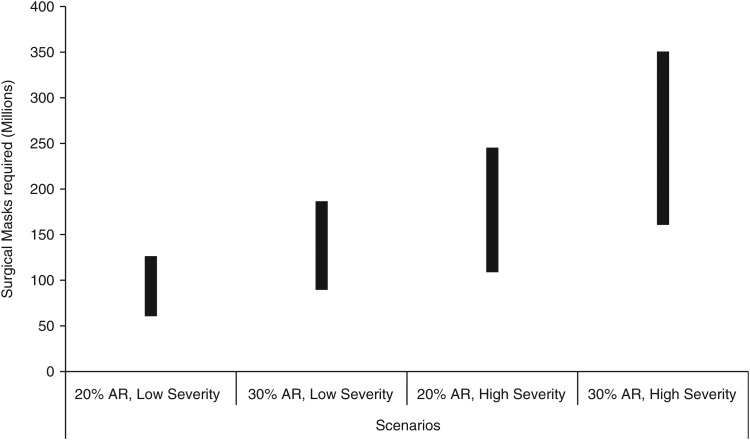
Figure 3.
Surgical mask demand by pandemic scenario. For each scenario, ranges result from variations in surgical mask use rates and epidemiologic and healthcare use parameters. Surgical mask demand is the same for the base, intermediate, and maximum scenario, as it is meant for source control and the number of patients is proportional to the epidemic curve. Abbreviation: AR, attack rate.
In all scenarios, the demand for respirators by personnel in outpatient settings exceeded demand in other settings and comprised approximately one-half of total demand in the low severity scenario. In the low severity scenarios, the hospital settings accounted for the least use, with only approximately one-tenth of total use. For the high severity scenario, police, fire services, EMS, and nursing home settings comprised approximately one-third of the total respirator demand. The remaining respirators were used in the outpatient setting (from one-third to approximately one-half), and a smaller portion in the hospital setting (up to almost one-third in the high severity/high attack rate scenario).
Results were especially sensitive to assumptions regarding use behavior in different settings, as relayed by different use models (Figure 2). In particular, the base case scenario assumption that ILI recognition is possible in some healthcare settings (and that only HCWs interfacing with ILI patients would require respirators) results in a reduction of up to 1.5 billion respirators, when compared with the intermediate demand scenario (where respirator use surges with the pandemic but then remains constant from the peak until the pandemic resolves) among low and high attack rate scenarios. If comparing the base case distribution scenario with the maximum demand distribution scenario, the difference is up to 4.3 billion for the low attack rate and higher duration scenarios and up to 2.5 billion respirators for the high attack rate and lower duration scenarios.
The difference between estimates obtained with the intermediate demand model and the maximum demand model is also substantial for the low attack rate scenarios (Figure 2). The difference between the two models is up to 3.0 billion for the low attack rate scenario; the maximum demand model always yields higher estimates. The primary factor driving the different respirator estimates among these two models is the duration of the pandemic. Therefore, the largest differences in demand estimates between these two models are observed among the pandemic scenarios of greater duration (low attack rate scenarios).
The estimated number of surgical masks required for source control varied from 0.1 billion in the low attack rate/low severity scenario to 0.4 billion in the high attack rate/high severity scenario (Figure 3). Between approximately one and two-thirds of required surgical masks would be used by patients in the hospital, in the low and high severity scenarios. The remaining surgical masks would be used by ill persons mainly in outpatient settings. Estimates of surgical mask use in nursing homes and by patients transported by EMS ranged from 2 to 9 million (2%–3% of total demand), across all scenarios.
Sensitivity Analysis
Effect of Demand Reduction Strategies
Our analyses indicated that demand reduction strategies can have a substantial effect on projected total respirator use, especially if surgical masks or elastomeric respirators are used to substitute for respirators (Table 3). For demand reduction strategy 1 (using the same respirator to attend to several patients in different settings such as the ICU, GW, ED, nursing homes, outpatient clinics, and police and fire), limited reuse of respirators across all settings in the base case demand model reduced demand by approximately 76% across all scenarios.
Table 3.
Total Demand for N95 Filtering Facepiece Respirators (Respirators) and Effect of Demand Reduction Strategies 1–3 on Total Demand for Respirators (in Millions)
| Model | Pandemic Scenario | Lower Bound | Upper Bound |
|---|---|---|---|
| Base case | 20% AR, low severity | 2302 | 3053 |
| 30% AR, low severity | 1662 | 2194 | |
| 20% AR, high severity | 2476 | 3467 | |
| 30% AR, high severity | 1867 | 2703 | |
| Demand reduction strategy 1 | 20% AR, low severity | 573 | 754 |
| 30% AR, low severity | 412 | 536 | |
| 20% AR, high severity | 610 | 838 | |
| 30% AR, high severity | 454 | 638 | |
| Demand reduction strategy 2 | 20% AR, low severity | 20 | 56 |
| 30% AR, low severity | 25 | 66 | |
| 20% AR, high severity | 57 | 139 | |
| 30% AR, high severity | 67 | 169 | |
| Demand reduction strategy 3 | 20% AR, low severity | 61 | 80 |
| 30% AR, low severity | 48 | 74 | |
| 20% AR, high severity | 83 | 138 | |
| 30% AR, high severity | 78 | 154 |
Effect of demand reduction strategies was calculated assuming the base case distribution scenario. Description of demand reduction strategies: Demand reduction strategy 1: limited reuse of respirators across all settings; Demand reduction strategy 2: limited reuse of respirators in intensive care unit (ICU), general ward (GW), emergency department (ED), and nursing homes, and substitution of surgical masks for respirators in outpatient clinics, emergency medical service (EMS), and for fire and police responders, with removing and putting on the same surgical masks for different patients in these settings; Demand reduction strategy 3: partial substitution of respirators by elastomeric respirators in the ICU and ED settings; limited reuse of respirators in GWs, nursing homes, and EMS settings, with use of surgical masks in outpatient clinics and by fire and police responders (removing and putting on the same surgical masks for different patients).
Abbreviation: AR, attack rate.
For demand reduction strategy 2 (limited respirator reuse by personnel in the hospital settings and nursing homes; and use of surgical masks instead of respirators in outpatient clinics and by EMS, fire, and police responders), demand for respirators was <7% of original demand across all scenarios, requiring a minimum of 20 million of these respirators in the low attack rate/low severity scenario and a maximum of 169 million respirators in the high attack rate/high severity scenario (Table 3). This reduction was largely the result of eliminating demand for respirators among police, fire, outpatient, and EMS.
Demand reduction strategy 3 (substituting respirators with reusable, elastomeric respirators in hospital ICUs and EDs, limited reuse of respirators in hospital GWs, in nursing homes, and EMS settings, and use of surgical masks in outpatient clinics and by fire and police responders) had slightly less of an effect than demand reduction strategy 2, mainly because demand for respirators by EMS (a setting where an intermediate demand behavior was assumed) was not eliminated. Demand for respirators varied between 48 million in the high attack rate/low severity scenario and 154 million in the high attack rate/high severity scenario (Table 3).
However, demand reduction strategies 2 and 3 required a substantially higher number of surgical masks to replace respirators. Across all scenarios and courses of action, total demand for surgical masks increased to 894 million for the low attack rate (and higher duration)/ high severity scenario, and to 787 million for the high attack rate (and smaller duration)/high severity scenario.
Respirator and Surgical Mask Use Parameters
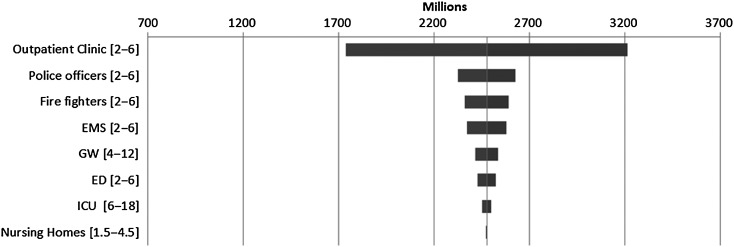
Demand estimates were sensitive to respirator use parameters, especially to respirator use in the outpatient setting. A 50% decrease in the use of respirators in the outpatient setting resulted in approximately 700 million fewer respirators being required (Figure 4). The sectors in which respirator use parameters had the next greatest effect were police, fire services, and EMS, where use was modeled with an intermediate demand approach. The lesser influence of respirator use parameters in these sectors, if compared with the outpatient sector, was due to the fewer number of HCWs working in these sectors. There were approximately 6 times the number of HCWs in outpatient settings compared with the number of police officers, and there were 9 times more HCWs in outpatient settings than professional firefighters.
Figure 4.
Variation of demand for N95 filtering facepiece respirators (respirators) with usage rates for different settings; for the base case (bars are centered around approximately 2.5B, the estimated demand for respirators for the 20% Attack Rate; high severity scenario; each bar shows the minimum and maximum demand obtained when varying the parameters in the interval featured on the left axis). Interpretation: if respirator use rate in the outpatient sector changes to 2/day/healthcare worker (50% reduction), total demand for respirators reduces to 1.7 billion). Abbreviations: ED, emergency department; EMS, emergency medical service; GW, general ward; ICU, intensive care unit.
Variations in the demand for respirators in the ICU and nursing home settings had decreasing influence on the demand for respirators because we assumed that patients with ILI would be recognized in these settings and demand was driven by the number of people with ILI seeking care. In particular, by varying the respirator use rate in ICU to 50% of the original value, demand for respirators decreased by 26 million (it would conversely increase by 26 million if the use rate would increase to 150% of the original value; Figure 4).
We also abstracted respirator use multipliers from the literature (Supplementary Appendix III: Table AIII-2; Appendix I) and used these values to compute respirators required by healthcare providers. Using these multipliers, without use of any reduction strategies, the number of respirators required varied from1.6 billion to 3.4 billion across all scenarios; similar to results obtained in the base case demand scenario.
Finally, assuming a time varying ILI to case ratio did not impact the base case results significantly but had a slightly greater impact on the lower bound estimated for demand reduction strategies 2 and 3. Base case estimates increased by a maximum of only 5%; however, the lower bound of need for demand reduction strategies 2 and 3 increased by <26% and <15%, respectively.
DISCUSSION
We calculated that, in the base case scenario (base case model) from 1.7 billion to 3.5 billion respirators will be required for HCWs and first responders in the hospital, outpatient, nursing home, EMS, and the fire and police sector in the event of an influenza pandemic. In addition, 0.1–0.4 billion surgical masks will be required for source control. Estimates were sensitive to respirator use rates, especially in the outpatient setting, followed by police and fire (other settings in which demand was proportional to the size of the workforce). Projected demand was especially sensitive to assumptions regarding use in different sectors. For instance, assuming constant respirator use throughout the pandemic resulted in an estimated demand for respirators of up to 7.3 billion.
We have used conservative assumptions regarding patient-provider contacts. In our base case scenario, we assumed ICU patients would have 12–16 contacts with HCWs and so 12–16 respirators would be needed per patient per day. In comparison, Murray et al [17] estimated, in Vancouver, Canada, that during the 2009 pandemic, “… 498 respirators and 494 masks …were used per patient with laboratory-confirmed H1N1 influenza infection.” Although we have made several sensitivity analyses to respirator usage rates, the possibility of pandemic cases generating excessive demand remains open, given the few data points available, and underscoring the great need of planning for respirator and surgical mask during a pandemic. To note, demand for respirators and surgical masks for household use and by groups of workers that have routine contact with the public and may desire protection may further decrease available supplies.
Another limitation of our calculations is that they were based on a hypothetical, unmitigated influenza pandemic and limitless care capacity by healthcare providers. Interventions, such as school closings, prompt treatment of ill persons, and mass vaccination campaigns, may reduce the spread of the pandemic and, hence, the need for respirators and masks. Capacity constraints could prevent delivery of care to all persons and also the number of required respirators and surgical masks. However, we do not know by what percentage these other interventions would reduce potential demand for respirator and surgical masks. Vaccines could, as in 2009, be delivered in notable amounts only after the pandemic peak [30].
Additionally, respirators are just one component of infection control recommendations for mitigation of influenza risk and this paper does not attempt to model the use of other resources (such as administrative and engineering controls as well as the use of face shields, eye shields, and airborne isolation rooms), which may be in limited supply during a pandemic. We also did not attempt to model other strategies that could have an impact on total demand, such as chemoprophylaxis (medication for the purposes of preventing disease), or other use strategies for respirators, such as extended use (not removing the respirator between patients). We expect that extended use could further diminish total need, however, the amount by which it would do so depends on rate of contact with patients by HCW and setting, a quantity difficult to estimate. We did model the impact of limited reuse on total demand. However, such estimates were obtained under the assumption of complete compliance by healthcare providers, which may be problematic [31, 32].
Our study suggests that, during a pandemic, usual standards of care for workers in contact with the ill from respiratory diseases such as influenza may not be feasible as it would involve an impractical demand for respirators and surgical masks. The domestic respiratory protective device industry currently manufactures product needed to meet anticipated normal market demands with minimal room for instant ability ramping up of production (surge). Surge capacity may increase over time (6 weeks to 4 months) but ability to surge is contingent on multiple factors including availability of manufacturing capacity and raw materials, and sustained demand for products [Personal communication, A. Patel, CDC, Atlanta]. Thus, although guidance for crisis standards of care exist [33, 34], the predicted gap between needed facial protective equipment and existent capacity may become so large as to warrant further exploration of alternative strategies. In our model, the use of durable elastomeric respirators that can be issued to a healthcare provider and reused repeatedly over the course of a pandemic could substantially reduce the supply-demand gap. However, elastomeric respirators have not been widely used in healthcare settings, and we cannot predict how well they will be accepted and if healthcare providers will adhere to recommendations for these devices.
These findings underscore the need for policy makers, leaders of healthcare organizations, and ethicists, to urgently consider strategies for use of respirators during a pandemic that may vary from current practices, including incorporating other types of respirators such as elastomerics and PAPRs, extended and limited reuse strategies for respirators, and other mitigation strategies, such as source, administrative, and environmental control measures, in order to optimize HCW protection.
Supplementary Material
Notes
Acknowledgments. The authors thank Stephen Redd (Influenza Coordination Unit) for guidance; Tim Lant, Mary Beth Hill-Harmon, Sid Baccam, Dylan George, and Jason Asher (Biomedical Advanced Research Development Authority) for useful discussions and advice; Lisa Delaney (National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention [CDC]) for information regarding the definition and limits of demand reduction strategies; Anita Patel (Office Of Public Health Preparedness And Response, CDC) for communications regarding production of respirators and surgical masks; Matt Biggerstaff (Influenza Division, CDC) for information regarding healthcare use rates; Carter Mecher (Department of Veterans Affairs) for information regarding the healthcare workforce; Cathy Young (National Center for Emerging and Zoonotic Diseases) for a careful review of the document; and Manoj Gambhir (CDC) for support regarding the adaptation of the transmission model. We also thank CDC's Medical Care and Countermeasures Task Force and the Health Economics Modeling Unit for informative discussions and advice.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Supplement sponsorship. This article appears as part of the supplement titled “CDC Modeling Efforts in Response to a Potential Public Health Emergency: Influenza A(H7N9) as an Example,” sponsored by the CDC.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. World Health Organization. Human infections with avian influenza A(H7N9) virus, 2014. Available at: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/riskassessment_h7n9_27june14.pdf?ua=1 Accessed 5 March 2015.
- 2. National Institute for Occupational Safety and Health (NIOSH) CDC. Interim Guidance on Infection Control Measures for 2009 H1N1 Influenza in Healthcare Settings, Including Protection of Healthcare Personnel. Available at: http://www.cdc.gov/h1n1flu/guidelines_infection_control.htm Accessed 5 March 2015. [PubMed]
- 3. Hashikura M, Kizu J. Stockpile of personal protective equipment in hospital settings: preparedness for influenza pandemics. Am J Infect Control 2009; 37:703–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Krumkamp R, Kretzschmar M, Rudge JW, et al. Health service resource needs for pandemic influenza in developing countries: a linked transmission dynamics, interventions and resource demand model. Epidemiol Infect 2011; 139:59–67. [DOI] [PubMed] [Google Scholar]
- 5. Putthasri W, Lertiendumrong J, Chompook P, Tangcharoensathien V, Coker R. Capacity of Thailand to contain an emerging influenza pandemic. Emerg Infect Dis 2009; 15:423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Radonovich LJ, Magalian PD, Hollingsworth MK, et al. Stockpiling supplies for the next influenza pandemic. Emerg Infect Dis 2009; 15:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Phin NF, Rylands AJ, Allan J, et al. Personal protective equipment in an influenza pandemic: a UK simulation exercise. J Hosp Infect 2009; 71:15–21. [DOI] [PubMed] [Google Scholar]
- 8. Meltzer MI, Gambhir M, Atkins CY, Swerdlow DL. Standardizing scenarios to assess the need to respond to an influenza pandemic. Clin Infect Dis 2015; 60(suppl 1):S1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reed C, Biggerstaff M, Finelli L, et al. Novel framework for assessing epidemiologic effects of influenza epidemics and pandemics. Emerg Infect Dis 2013; 19:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Uscher-Pines L, Elixhauser A. Statistical Brief #147: Emergency Department Visits and Hospital Inpatient Stays for Seasonal and 2009 H1N1 Influenza, 2008–2009. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/statbriefs.jsp Accessed 5 March 2015. [PubMed]
- 11. Greenko J, Mostashar F, Fine A, Layton M. Clinical evaluation of the Emergency Medical Services (EMS) ambulance dispatch-based syndromic surveillance system, New York City. J Urban Health 2003; 80(Suppl 1):i50–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fowlkes A, Dasgupta S, Chao E, et al. Estimating influenza incidence and rates of influenza-like illness in the outpatient setting. Influenza Other Respir Viruses 2012; 7:694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Biggerstaff M, Jhung M, Kamimoto L, Balluz L, Finelli L. Self-reported influenza-like illness and receipt of influenza antiviral drugs during the 2009 pandemic, United States, 2009–2010. Am J Public Health 2012; 102:e21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. O'Riordan S, Barton M, Yau Y, Read SE, Allen U, Tran D. Risk factors and outcomes among children admitted to hospital with pandemic H1N1 influenza. CMAJ 2010; 182:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bagdure D, Curtis DJ, Dobyns E, Glode MP, Dominguez SR. Hospitalized children with 2009 pandemic influenza A (H1N1): comparison to seasonal influenza and risk factors for admission to the ICU. PLoS One 2010; 5:e15173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Presanis AM, De Angelis D, New York City Swine Flu Investigation Team, et al. The severity of pandemic H1N1 influenza in the United States, from April to July 2009: a Bayesian analysis. PLoS Med 2009; 6:e1000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Murray M, Grant J, Bryce E, Chilton P, Forrester L. Facial protective equipment, personnel, and pandemics: impact of the pandemic (H1N1) 2009 virus on personnel and use of facial protective equipment. Infect Control Hosp Epidemiol 2010; 31:1011–6. [DOI] [PubMed] [Google Scholar]
- 18. US Department of Justice (USDJ), Bureau of Justice Statistics. Law Enforcement Management and Administrative Statistics: Local Police Departments, 2003. Available at: http://bjs.gov/content/pub/pdf/lpd03.pdf Accessed 5 March 2015.
- 19. US Department of Labor, Occupational Safety and Health Administration. Proposed Guidance on Workplace Stockpiling of Respirators and Facemasks for Pandemic Influenza. Available at: https://www.osha.gov/dsg/guidance/proposedGuidanceStockpilingRespirator.pdf Accessed 5 March 2015.
- 20. Karter MJS, Gary P. US Fire Department Profile through 2011, 2012.
- 21. Quarterly Census of Employment and Wages. Available at: http://data.bls.gov/cgi-bin/dsrv?en. Accessed 5 March 2015.
- 22. McGinnis S, Moore J, Armstrong D. The Emergency Care Workforce in the US. Center for Health Workforce Studies, 2006.
- 23. Top 10 Physician Specialties. Available at: http://www.billianshealthdata.com/news/vitals/InFocus/Top_10_Physician_Specialties Accessed 5 March 2015.
- 24. US Census Bureau. Annual Estimates of the Resident Population: 1 April 2010 to 1 July 2013, 2014.
- 25. Nursing Home Care. Available at: http://www.cdc.gov/nchs/fastats/nursing-home-care.htm Accessed 5 March 2015.
- 26. US Census Bureau. Resident Population by Age and Sex: 1980 to 2010. Available at: http://www.census.gov/compendia/statab/2012/tables/12s0007.pdf Accessed 5 March 2015.
- 27. Fisher EM, Shaffer RE. Considerations for recommending extended use and limited reuse of filtering facepiece respirators in health care settings. J Occup Environ Hyg 2014; 11:D115–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. National Institute for Occupational Safety and Health (NIOSH) CDC. Pandemic Planning: Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings. Available at: http://www.cdc.gov/niosh/topics/hcwcontrols/RecommendedGuidanceExtUse.html Accessed 5 March 2015.
- 29. Bergman MS, Viscusi DJ, Zhuang Z, Palmiero AJ, Powell JB, Shaffer RE. Impact of multiple consecutive donnings on filtering facepiece respirator fit. Am J Infect Control 2012; 40:5. [DOI] [PubMed] [Google Scholar]
- 30. Borse RH, Shrestha SS, Fiore AE, et al. Effects of vaccine program against pandemic influenza A(H1N1) virus, United States, 2009–2010. Emerg Infect Dis 2013; 19:439–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hines L, Rees E, Pavelchak N. Respiratory protection policies and practices among the health care workforce exposed to influenza in New York State: Evaluating emergency preparedness for the next pandemic. Am J Infect Control 2014; 42:240–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Beckman S, Materna B, Goldmacher S, et al. Evaluation of respiratory protection programs and practices in California hospitals during the 2009–2010 H1N1 influenza pandemic. Am J Infect Control 2013; 41:1024–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Crisis Standards of Care: A Toolkit for Indicators and Triggers. Available at: http://iom.edu/Reports/2013/Crisis-Standards-of-Care-A-Toolkit-for-Indicators-and-Triggers.aspx Accessed 5 March 2015. [PubMed]
- 34. Centers for Disease Control and Prevention (CDC). Interim Guidance for Infection Control Within Healthcare Settings When Caring for Patients with Confirmed, Probable, or Cases Under Investigation of Avian Influenza A(H7N9) Virus Infection. Available at: http://www.cdc.gov/flu/avianflu/h7n9-infection-control.htm Accessed 5 March 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.