Adults hospitalized with 2009 pandemic influenza were younger than those hospitalized in previous influenza seasons and more likely to have lower respiratory tract complications and corresponding indicators of severe illness including intensive care admission, mechanical ventilation, or death.
Keywords: seasonal influenza, pandemic influenza, hospitalization, pneumonia
Abstract
Background. Persons with influenza can develop complications that result in hospitalization and death. These are most commonly respiratory related, but cardiovascular or neurologic complications or exacerbations of underlying chronic medical conditions may also occur. Patterns of complications observed during pandemics may differ from typical influenza seasons, and characterizing variations in influenza-related complications can provide a better understanding of the impact of pandemics and guide appropriate clinical management and planning for the future.
Methods. Using a population-based surveillance system, we compared clinical complications using International Classification of Diseases, Ninth Revision (ICD-9) discharge diagnosis codes in adults hospitalized with seasonal influenza (n = 5270) or 2009 pandemic influenza A(H1N1) (H1N1pdm09; n = 4962).
Results. Adults hospitalized with H1N1pdm09 were younger (median age, 47 years) than those with seasonal influenza (median age, 68 years; P < .01), and differed in the frequency of certain underlying medical conditions. Whereas there was similar risk for many influenza-associated complications, after controlling for age and type of underlying medical condition, adults hospitalized with H1N1pdm09 were more likely to have lower respiratory tract complications, shock/sepsis, and organ failure than those with seasonal influenza. They were also more likely to be admitted to the intensive care unit, require mechanical ventilation, or die. Young adults, in particular, had 2–4 times the risk of severe outcomes from H1N1pdm09 than persons of the same ages with seasonal influenza.
Conclusions. Although H1N1pdm09 was thought of as a relatively mild pandemic, these data highlight the impact of the 2009 pandemic on the risk of severe influenza, especially among younger adults, and the impact this virus may continue to have.
(See the Editorial Commentary by Warren-Gash on pages 175–6.)
Influenza causes considerable morbidity during each annual influenza season. Although influenza is most often a self-limited respiratory illness, severe illness including hospitalization and death can occur as a result of complications stemming from the influenza virus infection. In the United States, an estimated 100 000–300 000 hospitalizations [1] and 3300–48 000 deaths [2] are attributable to influenza each year. Since the 1960s, several factors have been recognized to increase the risk for complications of influenza, including extremes of age, certain underlying chronic diseases, and pregnancy [3, 4].
The most common influenza-associated complications are pulmonary, especially pneumonia, but a number of organ systems can be affected [5]. Cardiovascular complications, such as myocardial infarction, have been associated with antecedent respiratory infection, including influenza [6]. Neurologic complications including seizures and encephalopathy have also been documented among persons with influenza [7], more often observed in children [8]. Complications may also result from the exacerbation of underlying chronic medical conditions following infection, such as asthma, chronic obstructive pulmonary disease (COPD), or heart disease [9, 10].
In April 2009, the influenza A(H1N1)pdm09 virus (H1N1pdm09) caused the first influenza pandemic in >40 years [11]. Patterns of complications among persons with influenza may differ between influenza pandemics and annual seasons due to either differences in age groups most affected or virulence of circulating strains. An appreciation of particular patterns of complications and how they may differ during an influenza pandemic can help in understanding the clinical impact of the 2009 pandemic, guide clinicians toward the most effective diagnosis and management of patients with influenza, and assist in future resource planning.
Several studies have described patients hospitalized with H1N1pdm09, including those with influenza-related complications, in case series or at single-hospital sites or geographic areas [8, 12–17]. However, there has been limited evaluation of influenza-related complications in a large multicenter population of adults hospitalized with influenza during multiple influenza seasons, with the ability to directly compare complications from seasonal and pandemic influenza and with a large enough sample size to assess more rare complications. In this analysis, we describe data on >9000 adult patients during 2005–2010 from the Emerging Infections Program (EIP) Influenza Surveillance Network, a population-based surveillance system in the United States for patients hospitalized with laboratory-confirmed influenza. The purpose of this analysis was to describe and compare influenza-associated complications among adults hospitalized with H1N1pdm09 and seasonal influenza. Complications among children in this network have been previously described [18].
METHODS
Study Population and Case Definitions
Since 2005, the EIP influenza surveillance network has conducted population-based surveillance of adults hospitalized with laboratory-confirmed influenza virus infection, using a standardized surveillance protocol in 240 hospitals of 10 geographically diverse surveillance areas across the United States. Included in this analysis are adult patients hospitalized with laboratory-confirmed influenza identified in EIP during 2005–2010.
An adult is included in EIP influenza surveillance if he/she is ≥18 years of age, resides in the surveillance area, and is hospitalized with laboratory confirmation of influenza virus infection. Laboratory testing for influenza is ordered at the discretion of clinicians providing medical care, and confirmation may include a positive result from viral culture, direct or indirect fluorescent antibody staining, rapid antigen test, reverse transcription polymerase chain reaction (PCR), or documentation of a positive test result in a patient's medical record. Patients are identified through hospital laboratory and admission databases, infection control logs, and hospital discharge data for patients with a documented positive influenza test. Through medical record review, data are collected for each patient regarding demographic characteristics, medical history, clinical course, and outcomes (eg, admission to intensive care unit, mechanical ventilation, or death), as well as the first 9 discharge codes using the International Classification of Diseases, Ninth Revision (ICD-9).
Patients identified through surveillance were classified as having seasonal influenza (hospitalized 1 October 2005–14 April 2009) or H1N1pdm09 (hospitalized 15 April 2009–30 April 2010). Patients hospitalized during the pandemic period but known to be infected with influenza B viruses or seasonal influenza A subtypes were excluded.
Complications were classified based on ICD-9 discharge codes and included from the following categories: pulmonary, cardiovascular, neurologic, metabolic, musculoskeletal, cerebrovascular, and endocrine. A complete list of included complications and associated ICD-9 codes are included in Supplementary Data.
Data Analysis
Clinical characteristics of patients and frequencies of complications were compared using χ2 tests for categorical variables, and medians and distributions of continuous variables were compared using the Wilcoxon-Mann-Whitney test. To control for the contribution of age and underlying medical condition to the risk of complications, we calculated adjusted relative risks of complications in patients with H1N1pdm09 compared with patients with seasonal influenza using multivariable log-binomial regression. All analyses were performed using SAS software version 9.2 (Cary, North Carolina).
RESULTS
A total of 5959 adult patients with influenza were identified through EIP surveillance during the seasonal influenza periods from 1 October 2005 through 14 April 2009, and 5446 adult patients were identified during the pandemic period 15 April 2009–30 April 2010. Among adults identified during the pandemic period, 66 (1.2%) were excluded because they were infected with influenza B viruses (n = 52) or seasonal influenza A virus subtypes (n = 14 for H3N2). Unknown subtypes were assumed to be the predominant H1N1pdm09. In addition, a total of 689 (11.6%) patients with seasonal and 418 (7.8%) patients with pandemic influenza were excluded from the analysis because they were missing ICD-9 code data. Patients without ICD-9 data did not differ in risk of intensive care unit (ICU) admission, mechanical ventilation, or death. The data collection instrument captures the first 9 ICD-9 codes; among included patients, 5388 (52.7%) had all 9 ICD-9 code fields completed.
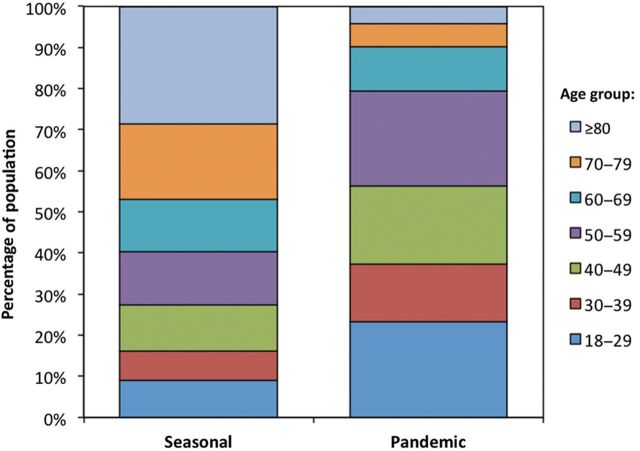
Adults hospitalized with H1N1pdm09 were younger (median age, 47 years) than those with seasonal influenza (median age, 68 years) (P < .01; Table 1). Figure 1 shows the substantial differences in the age distribution of patients during the seasonal and pandemic periods. During the seasonal influenza period, the largest proportional age group of patients was ≥80 years of age (29%), whereas this age group represented the smallest fraction of patients with pandemic influenza (4%), and only 21% of patients hospitalized with H1N1pdm09 were ≥60 years of age. Fewer than half of patients had documented influenza vaccination in either group, although significantly more during prepandemic seasons (46%) than during the pandemic season (23%; P < .001), when vaccine was not available until after the peak of the fall wave. Antiviral treatment was higher during the pandemic, with 83% of patients receiving antiviral medications compared with 54% during prepandemic seasons (P < .001).
Table 1.
Characteristics of Adults Hospitalized With Laboratory-Confirmed Seasonal or Pandemic Influenza
| Characteristic | Seasonal 2005–2009 (n = 5270) |
Pandemic 2009–2010 (n = 4962) |
P Value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Demographics | |||||
| Age, y, median (IQR) | 68 (48–82) | 47 (31–58) | <.01 | ||
| Male sex | 2282 | 43.3 | 2061 | 41.4 | .05 |
| Underlying medical conditions | |||||
| None | 839 | 15.9 | 1005 | 20.3 | <.01 |
| Chronic pulmonary disease | 1987 | 37.7 | 2110 | 42.5 | <.01 |
| Asthma | 902 | 17.1 | 1493 | 30.1 | <.01 |
| COPD | 1096 | 20.8 | 717 | 14.4 | <.01 |
| Other chronic lung disease | 220 | 4.2 | 159 | 3.2 | <.01 |
| Chronic cardiovascular disease | 2210 | 41.9 | 999 | 20.1 | <.01 |
| Chronic metabolic disease | 2156 | 40.9 | 1584 | 31.9 | <.01 |
| Diabetes | 1408 | 26.7 | 1139 | 23.0 | <.01 |
| Renal disease | 786 | 14.9 | 498 | 10.0 | <.01 |
| Neurologic | 781 | 14.8 | 466 | 9.4 | <.01 |
| Neuromuscular disease | 278 | 5.3 | 217 | 4.4 | .03 |
| Seizure disorder | 194 | 3.7 | 190 | 3.8 | .75 |
| Cognitive dysfunction | 450 | 8.5 | 204 | 4.1 | <.01 |
| Cancer/immunosuppressive | 751 | 14.3 | 739 | 14.9 | .30 |
| Cancer | 262 | 5.0 | 197 | 4.0 | .02 |
| Immunosuppressive condition | 599 | 11.4 | 645 | 13.0 | .01 |
| Pregnant | 165 | 3.1 | 430 | 8.7 | <.01 |
| Outcome | |||||
| Length of stay, d, median (IQR) | 4 (2–6) | 3 (2–6) | .38 | ||
| Intensive care admission | 808 | 15.3 | 1165 | 23.4 | <.001 |
| Mechanical ventilation | 471 | 8.9 | 643 | 12.9 | <.001 |
| Death | 191 | 3.6 | 198 | 4.0 | .35 |
Abbreviations: COPD, chronic obstructive pulmonary disease; IQR, interquartile range.
Figure 1.
Age distribution of adults hospitalized with seasonal or pandemic influenza, 2005–2010, United States.
Patients hospitalized during the pandemic were only slightly less likely to have a documented underlying medical condition than during the seasonal influenza period (80% vs 84%; P < .01); however, the types of medical conditions reported varied between the 2 groups (Table 1). Patients hospitalized with H1N1pdm09 were more likely than patients with seasonal influenza to have asthma or be pregnant; they were substantially less likely to have COPD or other chronic lung diseases, chronic cardiovascular disease, or chronic metabolic diseases (Table 1).
A greater percentage of adults hospitalized with H1N1pdm09 were admitted to the ICU (23%) or required mechanical ventilation (13%) than adults hospitalized with seasonal influenza (15% ICU, P < .001; 9% mechanical ventilation, P < .001). Mortality was similar in both groups (4%) (Table 1).
We examined several complications affecting a number of organ systems (Table 2). Among seasonal patients, 64% had at least 1 of the included complications recorded, compared with 71% of patients with H1N1pdm09 (P < .01). Overall, patients with 1 of the included complications had 5.5% risk of mortality compared with 0.3% mortality in patients without any of the included complications (P < .001; relative risk = 15.4 after controlling for age and underlying condition). Whereas pulmonary complications were the most commonly recorded during both periods (Table 2), there was a significant difference between the 2 periods, with 55% of seasonal influenza patients having at least 1 recorded pulmonary complication, compared with 64% of patients with H1N1pdm09 (P < .001). Of pulmonary complications, pneumonia was the most commonly recorded (seasonal: 35%, pandemic: 43%, P < .01). Other common complications included renal failure (12% among both seasonal and pandemic patients, P = .99), cardiovascular complications (seasonal, 6%; pandemic, 5%; P = .02), and shock/sepsis (seasonal, 6%; pandemic, 10%; P < .01). Neurologic, musculoskeletal, cerebrovascular, and endocrine complications were also noted, but less frequently (<5% of seasonal or pandemic patients).
Table 2.
Frequency of Complications Among Persons Hospitalized With Laboratory-Confirmed Seasonal or Pandemic Influenza, as Categorized by ICD-9 Code
| Complication | Seasonal (n = 5270) |
Pandemic (n = 4962) |
P Value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Any | 3393 | 64.4 | 3529 | 71.1 | <.001 |
| Pulmonary, any | 2893 | 54.9 | 3190 | 64.3 | <.001 |
| Pneumonia | 1868 | 35.4 | 2122 | 42.8 | <.001 |
| COPD exacerbation | 608 | 11.5 | 406 | 8.2 | <.001 |
| Respiratory failure/arrest | 583 | 11.1 | 878 | 17.7 | <.001 |
| Asthma exacerbation | 540 | 10.2 | 808 | 16.3 | <.001 |
| Pulmonary collapse | 142 | 2.7 | 117 | 2.4 | .28 |
| Pleural effusion/empyema | 138 | 2.6 | 121 | 2.4 | .56 |
| Hemoptysis | 36 | 0.7 | 75 | 1.5 | <.001 |
| Acute respiratory distress syndrome | 27 | 0.5 | 98 | 2.0 | <.001 |
| Pneumothorax | 13 | 0.2 | 38 | 0.8 | <.001 |
| Metabolic failure, any | 648 | 12.3 | 618 | 12.5 | .81 |
| Acute renal failure | 646 | 12.3 | 608 | 12.3 | .99 |
| Acute hepatic failure | 11 | 0.2 | 38 | 0.8 | <.001 |
| Cardiovascular, any | 333 | 6.3 | 258 | 5.2 | .02 |
| Myocardial infarction | 175 | 3.3 | 78 | 1.6 | <.001 |
| Acute heart failure | 57 | 1.1 | 84 | 1.7 | .01 |
| Arterial or venous embolism | 50 | 0.9 | 35 | 0.7 | .18 |
| Pulmonary embolism | 25 | 0.5 | 43 | 0.9 | .01 |
| Carditis | 20 | 0.4 | 16 | 0.3 | .63 |
| Cardiac arrest | 19 | 0.4 | 25 | 0.5 | .27 |
| Malignant hypertension | 23 | 0.4 | 19 | 0.4 | .67 |
| Acute ischemic heart disease | 12 | 0.2 | 4 | 0.1 | .06 |
| Shock/sepsis, any | 321 | 6.1 | 479 | 9.7 | <.001 |
| Disseminated intravascular coagulation | 13 | 0.2 | 18 | 0.4 | .29 |
| Neurologic, any | 223 | 4.2 | 185 | 3.7 | .19 |
| Altered mental status | 123 | 2.3 | 69 | 1.4 | <.001 |
| Encephalopathy | 61 | 1.2 | 64 | 1.3 | .54 |
| Convulsions | 86 | 1.6 | 34 | 0.7 | <.01 |
| Meningitis | 19 | 0.4 | 23 | 0.5 | .42 |
| Anoxic brain damage | 16 | 0.3 | 21 | 0.4 | .26 |
| Encephalitis/myelitis | 8 | 0.2 | 2 | 0.0 | .11 |
| Coma | 7 | 0.1 | 10 | 0.2 | .41 |
| Guillain-Barré/polyneuropathy | 0 | 0 | 7 | 0.1 | .006 |
| Musculoskeletal, any | 110 | 2.1 | 86 | 1.7 | .19 |
| Rhabdomyolysis | 108 | 2.0 | 68 | 1.4 | .01 |
| Myositis | 2 | 0.0 | 6 | 0.1 | .17 |
| Critical illness myopathy | 1 | 0.0 | 13 | 0.3 | <.01 |
| Cerebrovascular, any | 69 | 1.3 | 59 | 1.2 | .58 |
| Cerebral infarction | 33 | 0.6 | 29 | 0.6 | .79 |
| Cerebral hemorrhage | 12 | 0.2 | 6 | 0.1 | .20 |
| Cerebral edema | 3 | 0.1 | 7 | 0.1 | .17 |
| Endocrine, any | 42 | 0.8 | 63 | 1.3 | .02 |
| Diabetic ketoacidosis | 33 | 0.6 | 59 | 1.2 | <.01 |
| Diabetic hyperosmolarity | 5 | 0.1 | 1 | 0.0 | .22 |
| Diabetic coma | 4 | 0.1 | 4 | 0.1 | .99 |
Abbreviations: COPD, chronic obstructive pulmonary disease; ICD-9, International Classification of Diseases, Ninth Revision.
Although the frequency of many complications differed between the seasonal and pandemic period, for some the associations were no longer significant after we controlled for patients' ages and underlying medical condition(s), indicating that the risk of those complications did not differ during the pandemic for persons of similar age and medical history. These complications included exacerbations of asthma and COPD, most cardiovascular and neurologic complications, and musculoskeletal, cerebrovascular, and endocrine complications (Table 3).
Table 3.
Risk of Selected Complications in Adults Hospitalized With Influenza and Comparison of Pandemic and Seasonal Influenzaa
| Complication | % of Total | Adjusted RRb | 95% CI |
|---|---|---|---|
| Any | 67.7 | 1.12 | 1.09–1.15 |
| Pulmonary, any* | 59.5 | 1.14 | 1.11–1.18 |
| Pneumonia* | 39.0 | 1.33 | 1.26–1.40 |
| Respiratory failure/arrest* | 14.3 | 1.76 | 1.58–1.96 |
| Asthma exacerbation | 13.2 | 0.97 | .89–1.06 |
| Acute exacerbation of COPD | 9.9 | 0.97 | .86–1.09 |
| Pulmonary collapse | 2.5 | 0.96 | .73–1.25 |
| Pleural effusion/empyema | 2.5 | 1.17 | .89–1.53 |
| Acute respiratory distress syndrome* | 1.2 | 3.02 | 1.92–4.75 |
| Hemoptysis* | 1.1 | 1.75 | 1.14–2.67 |
| Metabolic failure, any* | 12.4 | 1.33 | 1.19–1.48 |
| Acute renal failure* | 12.3 | 1.31 | 1.17–1.47 |
| Shock/sepsis* | 7.8 | 1.70 | 1.46–1.97 |
| Cardiovascular, any* | 5.8 | 1.38 | 1.16–1.64 |
| Acute myocardial infarction | 2.5 | 1.03 | .78–1.37 |
| Acute heart failure* | 1.4 | 3.35 | 2.34–4.79 |
| Other, combined | 2.3 | 1.13 | .85–1.49 |
| Neurologic, any | 4.0 | 1.12 | .91–1.38 |
| Altered mental status | 1.9 | 0.91 | .66–1.26 |
| Encephalopathy* | 1.2 | 1.54 | 1.05–2.27 |
| Other, combined | 1.1 | 1.17 | .78–1.76 |
| Musculoskeletal | 1.9 | 0.92 | .68–1.25 |
| Rhabdomyolysis | 1.7 | 0.77 | .56–1.07 |
| Cerebrovascular, any | 1.3 | 1.20 | .82–1.76 |
| Endocrine, any | 1.0 | 0.88 | .60–1.27 |
| Other | |||
| ICU* | 19.3 | 1.55 | 1.42–1.69 |
| Mechanical ventilation* | 10.9 | 1.50 | 1.33–1.70 |
| Death* | 3.8 | 1.58 | 1.28–1.96 |
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; RR, relative risk.
a For complications occurring in at least 1% of patients.
b Relative risk of selected complications using negative-binomial regression among persons with H1N1pdm09 compared with seasonal influenza, controlling for age (18–39 years, 40–64 years, ≥65 years) and the following types of underlying medical condition: pulmonary, cardiovascular, metabolic, neurologic, cancer/immunosuppression, pregnancy.
*P < .05.
There were several complications, however, that were significantly more likely to occur among adults hospitalized with H1N1pdm09 than adults with seasonal influenza, even after controlling for age and underlying medical conditions (Table 3). These were most commonly respiratory complications such as pneumonia (adjusted relative risk [aRR] = 1.3) and respiratory failure (aRR = 1.8), as well as nonrespiratory complications such as renal failure (aRR = 1.3) and shock/sepsis (aRR = 1.7). Some other, less frequent complications were also more likely among patients hospitalized with H1N1pdm09 including acute respiratory distress syndrome (aRR = 3.0), acute heart failure (aRR = 3.4), hemoptysis (aRR = 1.8), and encephalopathy (aRR = 1.5). We further found that adults hospitalized with H1N1pdm09 were approximately 1.5 times more likely to experience clinical outcomes such as ICU admission, mechanical ventilation, or death than those hospitalized with seasonal influenza, after controlling for age and underlying conditions.
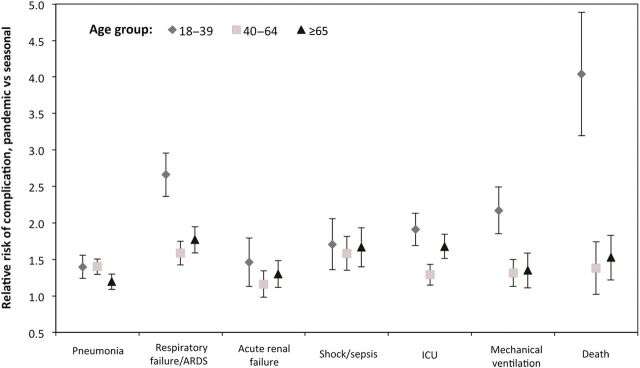
To examine whether these associations were modified by age, we repeated the analysis in 3 age strata: 18–39 years, 40–64 years, and ≥65 years (Figure 2). Young adults <40 years of age hospitalized with H1N1pdm09 were particularly affected, with approximately 2.5 times the risk of respiratory failure, twice the risk of ICU admission or mechanical ventilation, and 4 times the risk of death compared with adults <40 years hospitalized with seasonal influenza.
Figure 2.
The relative risk of selected complications (with 95% confidence intervals) among patients hospitalized with pandemic influenza vs seasonal influenza, stratified by age. Abbreviations: ARDS, acute respiratory distress syndrome; ICU, intensive care unit.
DISCUSSION
Although the 2009 influenza pandemic is considered to have been a relatively mild pandemic, especially when compared with the previous 3 documented influenza pandemics, many serious complications did occur. We found that compared with adults hospitalized during 4 previous influenza seasons, those hospitalized with pandemic influenza were younger and more likely to have lower respiratory tract complications (including pneumonia) and corresponding indicators of severe illness (including shock/sepsis and acute organ failure), even after controlling for differences in age and comorbidities. Furthermore, adults hospitalized with influenza during the pandemic were also more likely to be admitted to the ICU, require mechanical ventilation, or die during hospitalization.
These findings are consistent with observations from previous influenza pandemics, which have noted an increased risk of lower respiratory tract complications, including viral pneumonia with or without bacterial coinfection [19, 20]. Likewise, the findings from this large case series are similar to a few smaller recent studies that were able to directly compare adults with H1N1pdm09 or seasonal influenza. In Hong Kong, adults hospitalized with H1N1pdm09 had a significantly greater frequency of complications and mortality despite being younger than patients hospitalized with influenza in 2007–2008 [14]. A small study of patients hospitalized with influenza in Australia in 2009 found an increased risk of admission to intensive care among persons infected with H1N1pdm09 vs co-circulating seasonal influenza strains [21], whereas patients with outpatient medically attended H1N1pdm09 in the United States experienced a greater risk of pneumonia than patients with seasonal influenza H1N1 or H3N2 in previous seasons [22]. Postpandemic, 2 studies have also found an increased risk of pneumonia [23] or ICU admission/death [24] among patients with H1N1pdm09 compared with those with other seasonal influenza strains. During a pandemic, the spread of an antigenically novel influenza virus against which there is limited preexisting immunity may be expected to result in an increased risk of severe respiratory complications compared with annually circulating strains of seasonal influenza.
One notable hallmark of the 2009 influenza pandemic was the increased risk of influenza among younger persons, which was reflected in the substantial differences in the age distribution we observed between adults hospitalized with pandemic or seasonal influenza. Whereas this trend is often seen during influenza pandemics [25], some degree of cross-reactive immunity among persons of older ages may have contributed to relatively low levels of infection with H1N1pdm09 in older adults [26]. Although we did find that all adults had a higher risk of respiratory complications and severe outcomes with H1N1pdm09 than seasonal influenza, we further stratified by age and found that younger adults aged <40 years were particularly affected, including a 4 times greater risk of death during the pandemic compared with adults of similar age hospitalized with seasonal influenza.
This trend toward more severe illness, especially in younger persons, has important implications for clinical management during pandemics, as younger persons are also likely to have different comorbidities that need to be managed in parallel. As we found, patients hospitalized during the pandemic were more likely to have asthma or be pregnant, medical histories associated with younger age. While we did not have data on obesity for hospitalized patients prior to the pandemic, other studies have indicated that morbid obesity was associated with hospitalization during the pandemic even in the absence of other medical conditions [27], and thus may be a frequent comorbidity seen among younger adults with severe influenza. Conversely, adults hospitalized during the pandemic were less likely to have conditions such as COPD, chronic heart disease, or chronic metabolic diseases, which are more prevalent among older adults.
Consistent with these differences in age and medical history, the overall pattern of other complications observed among patients hospitalized with influenza during the 2009 pandemic differed from that observed during previous seasonal epidemics. During the pandemic, for example, there were fewer exacerbations of COPD or acute myocardial infarctions, but more hospitalizations with acute complications of asthma. Much of these differences in frequency were attributable to differences in age and corresponding underlying comorbidities, as the risk of such complications did not differ during the pandemic for individuals of similar ages and medical history. Nonetheless, there was a different distribution of complications during the pandemic and as clinicians may expect to encounter a younger demographic of patients with severe influenza during pandemics, the approach to resource planning for patients and their associated medical complications may need to reflect these differences.
Finally, an increased incidence of influenza in the population during the pandemic resulted in a corresponding increased incidence of hospitalization compared with previous influenza seasons [28]. In 1 year during the pandemic, we identified 5446 patients with H1N1pdm09 in the same surveillance areas, similar in number to 4 previous influenza seasons combined (n = 5959). An increase in the number of hospitalizations during a pandemic not only affects demands on hospital capacity, but also means an increased number of patients with complications that may require additional resources, staffing, and equipment (eg, supplemental oxygen, mechanical ventilation, dialysis) to effectively manage them.
This analysis is subject to some limitations. First, complications were classified based on ICD-9 discharge coding and were not confirmed with medical record review; however, our frequencies were similar to other smaller series of hospitalized patients during the 2009 pandemic that used chart review and/or radiology for confirmation of complications [12–14]. While we also cannot exclude the possibility of changes in ICD-9 coding practices during the pandemic, this surveillance system has been operating using standardized methods and in the same sites across all of the included years and when we compared the distributions of other recorded ICD-9 codes between patients before and during the pandemic (Supplementary Data), there were no differences in the proportion coded for pneumonia and influenza, any respiratory disease, or respiratory and circulatory diseases. Second, only the first 9 discharge ICD-9 codes were captured during data collection. Approximately half of the included patients had 9 codes recorded; thus, we were unable to determine if they had additional codes in which one of the included complications were recorded. However, we considered acute and often severe complications, which may have been more likely to be listed higher among discharge codes.
Finally, patients included in this surveillance system are tested for influenza at the discretion of the treating clinicians; thus, some patients who truly had influenza but were not tested would not be represented in our analysis. This may be especially true of patients who do not present with a typical influenza-like illness, but with complications of underlying medical conditions or other nonrespiratory complications. In this study population, approximately 5% of patients did not have any respiratory ICD-9 code (Supplementary Data), and about 12% of patients with 1 of the included complications did not have a respiratory complication (Table 2). These complications may be underrepresented if physicians are less likely to test such patients for influenza. Likewise, an increased use of the more sensitive PCR to diagnose influenza during the pandemic could have increased the detection of influenza during 2009.
In the largest case series describing clinical complications of influenza, we observed a greater proportion of lower respiratory complications and severe outcomes among persons hospitalized with influenza during the 2009 pandemic compared to previous influenza seasons. In addition, although the risk of many other complications did not differ for persons of similar age and medical history, these were often less likely overall because of the younger age of patients with severe influenza during the pandemic. Understanding the patterns of influenza-associated complications and how those may differ during influenza pandemics can help direct clinicians toward the most effective management of ill patients and assist in resource planning for future seasons and pandemics. Although the 2009 pandemic was thought of as relatively mild, these data highlight the impact of this pandemic on increasing the risk of severe illness from influenza, especially among younger adults, and the impact this virus may continue to have in the future.
Supplementary Material
Notes
Acknowledgments. The authors thank the following persons for their assistance with data collection: Erin Parker, MPH, Lauren Pasutti, MPH, and Susan Brooks, MPH (California EIP); Kimberly Yousey-Hindes, MPH, CPH, (Connecticut EIP, Yale School of Public Health, New Haven); Kyle Openo, MPH and Olivia Almendares, MPH (Georgia EIP); Sara Vetter and Dave Boxrud (Minnesota Public Health Laboratory); Nancy Spina, MPH (New York State Department of Health); Maria Gaitan (Center for Community Health, University of Rochester School of Medicine and Dentistry and New York State EIP); Brenda Barnes, RN, Karen Leib, RN, and Katie Dyer (Tennessee EIP).
Financial support. The analysis and manuscript preparation were completed as part of official duties at the Centers for Disease Control and Prevention.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Zhou H, Thompson WW, Viboud CG, et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis. 2012;54:1427–36. doi: 10.1093/cid/cis211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Estimates of deaths associated with seasonal influenza—United States, 1976–2007. MMWR Morb Mortal Wkly Rep. 2010;59:1057–62. [PubMed] [Google Scholar]
- 3.Burney LE. Influenza immunization: statement. Public Health Rep. 1960;75:944. [PMC free article] [PubMed] [Google Scholar]
- 4.Fiore AE, Shay DK, Broder K, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep. 2009;58:1–52. [PubMed] [Google Scholar]
- 5.Rothberg MB, Haessler SD, Brown RB. Complications of viral influenza. Am J Med. 2008;121:258–64. doi: 10.1016/j.amjmed.2007.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis. 2009;9:601–10. doi: 10.1016/S1473-3099(09)70233-6. [DOI] [PubMed] [Google Scholar]
- 7.Studahl M. Influenza virus and CNS manifestations. J Clin Virol. 2003;28:225–32. doi: 10.1016/s1386-6532(03)00119-7. [DOI] [PubMed] [Google Scholar]
- 8.Glaser CA, Winter K, Dubray K, et al. A population-based study of neurologic manifestations of severe influenza A(H1N1)pdm09 in California. Clin Infect Dis. 2012;55:514–20. doi: 10.1093/cid/cis454. [DOI] [PubMed] [Google Scholar]
- 9.Rohde G, Wiethege A, Borg I, et al. Respiratory viruses in exacerbations of chronic obstructive pulmonary disease requiring hospitalisation: a case-control study. Thorax. 2003;58:37–42. doi: 10.1136/thorax.58.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Browne LR, Gorelick MH. Asthma and pneumonia. Pediatr Clin North Am. 2010;57:1347–56. doi: 10.1016/j.pcl.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Dawood FS, Jain S, Finelli L, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 12.Jain S, Benoit SR, Skarbinski J, Bramley AM, Finelli L; Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Influenza-associated pneumonia among hospitalized patients with 2009 pandemic influenza A (H1N1) virus—United States, 2009. Clin Infect Dis. 2012;54:1221–9. doi: 10.1093/cid/cis197. [DOI] [PubMed] [Google Scholar]
- 13.Jain S, Kamimoto L, Bramley AM, et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April–June 2009. N Engl J Med. 2009;361:1935–44. doi: 10.1056/NEJMoa0906695. [DOI] [PubMed] [Google Scholar]
- 14.Lee N, Chan PK, Lui GC, et al. Complications and outcomes of pandemic 2009 influenza A (H1N1) virus infection in hospitalized adults: how do they differ from those in seasonal influenza? J Infect Dis. 2011;203:1739–47. doi: 10.1093/infdis/jir187. [DOI] [PubMed] [Google Scholar]
- 15.Louie JK, Acosta M, Winter K, et al. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302:1896–902. doi: 10.1001/jama.2009.1583. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen-Van-Tam JS, Openshaw PJ, Hashim A, et al. Risk factors for hospitalisation and poor outcome with pandemic A/H1N1 influenza: United Kingdom first wave (May-September 2009) Thorax. 2010;65:645–51. doi: 10.1136/thx.2010.135210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riquelme R, Torres A, Rioseco ML, et al. Influenza pneumonia: a comparison between seasonal influenza virus and the H1N1 pandemic. Eur Respir J. 2011;38:106–11. doi: 10.1183/09031936.00125910. [DOI] [PubMed] [Google Scholar]
- 18.Dawood FS, Chaves SS, Perez A, et al. Complications and associated bacterial coinfections among children hospitalized with seasonal or pandemic influenza, United States, 2003–2010. J Infect Dis. 2013 doi: 10.1093/infdis/jit473. [DOI] [PubMed] [Google Scholar]
- 19.Louria DB, Blumenfeld HL, Ellis JT, Kilbourne ED, Rogers DE. Studies on influenza in the pandemic of 1957–1958. II. Pulmonary complications of influenza. J Clin Invest. 1959;38(1 pt 2):213–65. doi: 10.1172/JCI103791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murata Y, Walsh EE, Falsey AR. Pulmonary complications of interpandemic influenza A in hospitalized adults. J Infect Dis. 2007;195:1029–37. doi: 10.1086/512160. [DOI] [PubMed] [Google Scholar]
- 21.Dalton CB, Cretikos MA, Durrheim DN, Seppelt IM, Rawlinson WD, Dwyer DE. Comparison of adult patients hospitalised with pandemic (H1N1) 2009 influenza and seasonal influenza during the “PROTECT” phase of the pandemic response. Med J Aust. 2010;192:357–8. doi: 10.5694/j.1326-5377.2010.tb03547.x. author reply. [DOI] [PubMed] [Google Scholar]
- 22.Belongia EA, Irving SA, Waring SC, et al. Clinical characteristics and 30-day outcomes for influenza A 2009 (H1N1), 2008–2009 (H1N1), and 2007–2008 (H3N2) infections. JAMA. 2010;304:1091–8. doi: 10.1001/jama.2010.1277. [DOI] [PubMed] [Google Scholar]
- 23.Rahamat-Langendoen JC, Tutuhatunewa ED, Scholvinck EH, et al. Influenza in the immediate post-pandemic era: a comparison with seasonal and pandemic influenza in hospitalized patients. J Clin Virol. 2012;54:135–40. doi: 10.1016/j.jcv.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Chaves SS, Aragon D, Bennett N, et al. Patients hospitalized with laboratory-confirmed influenza during the 2010–2011 influenza season: exploring disease severity by virus type and subtype. J Infect Dis. 2013;208:1305–14. doi: 10.1093/infdis/jit316. [DOI] [PubMed] [Google Scholar]
- 25.Simonsen L, Clarke MJ, Schonberger LB, Arden NH, Cox NJ, Fukuda K. Pandemic versus epidemic influenza mortality: a pattern of changing age distribution. J Infect Dis. 1998;178:53–60. doi: 10.1086/515616. [DOI] [PubMed] [Google Scholar]
- 26.Hancock K, Veguilla V, Lu X, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009;361:1945–52. doi: 10.1056/NEJMoa0906453. [DOI] [PubMed] [Google Scholar]
- 27.Morgan OW, Bramley A, Fowlkes A, et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS One. 2010;5:e9694. doi: 10.1371/journal.pone.0009694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shrestha SS, Swerdlow DL, Borse RH, et al. Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009–April 2010) Clin Infect Dis. 2011;52(suppl 1):S75–82. doi: 10.1093/cid/ciq012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.