Abstract
Although the impact of deaths occurring during the 1918–1919 influenza pandemic has been assessed in many archeo-epidemiologic studies, detailed estimates are not available for Portugal. We applied negative binomial models to monthly data on respiratory-related and all-cause deaths at the national and district levels from Portugal for 1916–1922. Influenza-related excess mortality was computed as the difference between observed and expected deaths. Poisson regression was used to estimate the association of geographic and sociodemographic factors with excess mortality. Two waves of pandemic influenza—July 1918 to January 1919 and April to May 1919—were identified, for which the excess all-cause death rate was 195.7 per 10,000 persons. All districts of Portugal were affected. The pandemic hit earlier in southeastern districts and the main cities, but excess mortality was highest in the northeast, in line with the high death burden experienced by northern Spanish provinces. During the period of intense excess mortality (fall/winter 1918–1919), population density was negatively associated with pandemic impact. This pattern changed during the March 1919 to June 1920 wave, when excess mortality increased with population density and in northern and western directions. Portuguese islands were less and later affected. Given the geographic heterogeneity evidenced in our study, subnational sociodemographic characteristics and connectivity should be integrated in pandemic preparedness plans.
Keywords: 1918 pandemic, excess mortality, influenza, Portugal, sociodemographic characteristics
The 1918–1919 influenza pandemic has been described as the infectious disease with the greatest impact on death in recent human history, with an estimated 20 million to 50 million of deaths (1). The highest mortality rate, disproportionally affecting young adults 20–40 years old, was observed during fall and winter 1918. The death impact on elderly populations varied across the world, probably owing to different immune backgrounds (2). Regions where a more intense spring and summer wave of the influenza pandemic was felt were less affected in the fall (3), suggesting cross-protection and supporting the circulation of related viruses in both waves (2). Other periods of excess mortality were described in subsequent winters (4, 5), but after 1919, the specific death rate in young adults declined and the mortality age profile aligned with that observed in years before 1918 (4).
The death rate attributed to the 1918–1919 pandemic was estimated at 11 per 1,000 persons in Europe, which corresponds to a relative excess risk of death of 86% and translates to a mortality excess of 2.6 million (about 1.1% of the European population) (6). Southern countries were hardest hit, with a relative excess in Italy of 172%, 102% in Portugal and Bulgaria, and 87% in Spain (6).
In 1918, Portugal was a predominantly rural country, and participation in World War I (1914–1918) aggravated hunger, food shortage, poverty, and social conflicts. It was a period of particular vulnerability marked by recurrent epidemic outbreaks such as exanthematous typhus (February to May 1918 and March to June 1919) (7, 8) and smallpox (1918) (8), in addition to the high burden of endemic diseases such as tuberculosis. Furthermore, the most intense influenza pandemic wave coincided with a troubled political period during October to December 1918, when there was a military uprising, a siege, and a general strike, which culminated in the assassination of the president of the Republic, Sidónio Pais, in December 1918. These problems did not prevent the collection of epidemiologic information and coordination of interventions by public health authorities to minimize the impact of the pandemic.
The first pandemic influenza cases were identified in May 1918 in southern Portugal (Vila Viçosa, Évora district) among farmers returning from the Spanish province of Badajoz; the infection rapidly spread across the country (9, 10). The pandemic reached Porto (the second most populated town) and Lisboa (the capital) in June and the Açores and Madeira archipelagos in September. The occurrence of the first severe cases of pneumonia in early September in the north of the country (Vila Nova de Gaia) marked the beginning of the second and lethal pandemic wave that rapidly spread throughout the mainland (11).
Although there are no official statistics of the deaths attributed to the 1918–1919 pandemic in Portugal, the overall death rate between 1917 and 1918 almost doubled from 220 to 420 per 10,000 persons and returned to prepandemic levels only after 1921 (12). This represents a crude excess death rate of 2%. In the same period, the influenza death rate increased 53-fold, from 1.8 per 10,000 to 96.2 per 10,000 persons (12). Death estimates for Portugal were reported in 2 international studies (3, 6); however, there were limitations to both studies. In 2006, Murray et al. (3) estimated an all-cause excess rate of 264 deaths per 10,000 persons for the period of 1918–1920, but this was based on annual deaths data, which lack specificity. In the second study, Ansart et al. (6) estimated an all-cause excess death of 223 per 10,000 persons for the period March 1918 to June 1919, based on monthly data. However, these data should be considered with caution because the authors reported that the 1918 pandemic first hit Finland in January 1918, followed by Portugal, Germany, and Bulgaria in March 1918, which contrasts with reports in contemporaneous newspapers and recent reviews (2). The impact of the 1918–1919 influenza pandemic in Portugal needs to be reviewed with a more consistent approach.
A detailed description of the spatiotemporal distribution of influenza deaths during the pandemic is lacking, and the heterogeneity between Portuguese cities remains unexplained. According to Sampaio, (5), influenza incidence was highest in cities in 1918, whereas the highest death rate was reported in rural areas. Differences in medical care and access to health care may have played a role in these pandemic burden differences, as may have nutrition, hygiene, and other socioeconomics factors. Sociodemographic factors were not correlated with the annual 1918 influenza death rate at the district and municipal levels (12). However, this observation could be biased by the very high proportion of deaths of unknown cause that were not considered in this study.
Given the lack of resolved death estimates for the 1918–1919 influenza pandemic in Portugal at national and regional levels, and the putative role of sociodemographic factors on the pandemic’s impact, we analyzed a detailed spatiotemporal data set of deaths to explore these questions. We estimated the excess mortality impact of the 1918–1919 influenza pandemic using data on all-cause and respiratory-related deaths in Portugal’s mainland districts and the Açores and Madeira archipelagos. We identified the beginning, peak, and duration of the different pandemic waves across Portugal. Finally, we identified the association between excess mortality and social, demographic, and geographic factors across Portugal.
METHODS
All data sets were compiled from the demographic statistics reports available from the Digital Library of Statistics Portugal portal (13). These digitized documents were printed and the data were manually entered into a database.
To estimate the impact of the 1918–1919 influenza pandemic in Portugal, we used monthly death time-series data from all causes and respiratory causes (including influenza, pulmonary tuberculosis, acute bronchitis, chronic bronchitis, and pneumonia) of death for the 17 mainland districts and the Açores and Madeira archipelagos from 1916 to 1922. These administrative areas (n = 19) hereafter are referred to as districts. Monthly district-level death rates were estimated on the basis of annual population estimates, obtained by linear interpolation of census data from 1911, 1920, and 1930.
District-level sociodemographic information was obtained for 1918 by linear interpolation of the 1911 and 1920 censuses. This information included population density (per square kilometer), proportion of the population aged 5–14 years, and illiteracy rate (among the population older than 7 years who could not read or write) (13). The prepandemic infant death rate, calculated from 1917 data, was also used (13). Infant death rates and literacy rates were considered indicators of the level of development of the regions. The percentage of the population aged 5–14 years was chosen as proxy for influenza transmission within the community, because children transmit influenza virus at a high rate. Population density is likely to be an indicator of exposure and economic development. Furthermore, we included capital district longitude and latitude to measure spatial distribution and account for spatial dependency (Web Table 1, available at https://academic.oup.com/aje).
To estimate national and district-level baseline death rates (all-cause or respiratory-related deaths) expected in the absence of the 1918–1919 influenza pandemic, we used an interrupted time-series approach. We standardized the monthly number of deaths to a fixed number of days each month (30.4 days) and excluded the extended pandemic period between June 1918 and May 1920 for model fitting. A negative binomial regression model was fitted to each time series, adjusting for seasonality (periods of 12 and 6 months) and time trends (third-degree polynomial), including population estimates as offset (Web Appendix). Separate models were fitted to each geographic area and cause of death. The expected number of deaths in the absence of pandemic influenza was obtained on the basis of model predictions. The prediction intervals were estimated using a parametric bootstrap method (14) that used 1,000 samples with replacement.
We evaluated the presence of overdispersion in the Poisson regression model (15). The prediction accuracy of negative binomial models was evaluated by a leave-one-out cross-validation procedure (14) and compared with Poisson models. Excess mortality periods were defined as those during which the observed number of deaths was greater than or equal to the upper limit of the 95% prediction interval.
The death burden of the 1918–1919 influenza pandemic was estimated as the difference between the observed and the expected number of deaths during periods of excess mortality. Because periods of excess mortality may vary by geographic area, we defined 4 pandemic phases to compare influenza dynamics at the district level. Phase 1 ran from June to August 1918 (summer), phase 2 from September 1918 to February 1919 (autumn and winter 1918–1919), phase 3 from March to September 1919 (spring and summer 1919), and phase 4 from October 1919 to June 1920. Excess mortality estimates were generated for each phase, geographic areas, and death outcome.
To measure the consistency between excess mortality estimates from all causes and respiratory diseases, we used the Spearman ρ correlation coefficient. Sociodemographic variables were categorized for analysis as follows: Population density and infant mortality rates were categorized by tertiles; literacy rate and percentage of population aged between 5–14 years were stratified according to the median. To explore the relationship between death rates and sociodemographic factors, we estimated crude and adjusted (Poisson regression) excess mortality rate ratios by category of sociodemographic variable. Excess mortality rate ratio confidence intervals were obtained using the robust sandwich covariance matrix estimator. Spatial correlation in the Poisson regression residuals was evaluated using the global Moran I statistics. All statistical analyses were performed using R, version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria) (16).
RESULTS
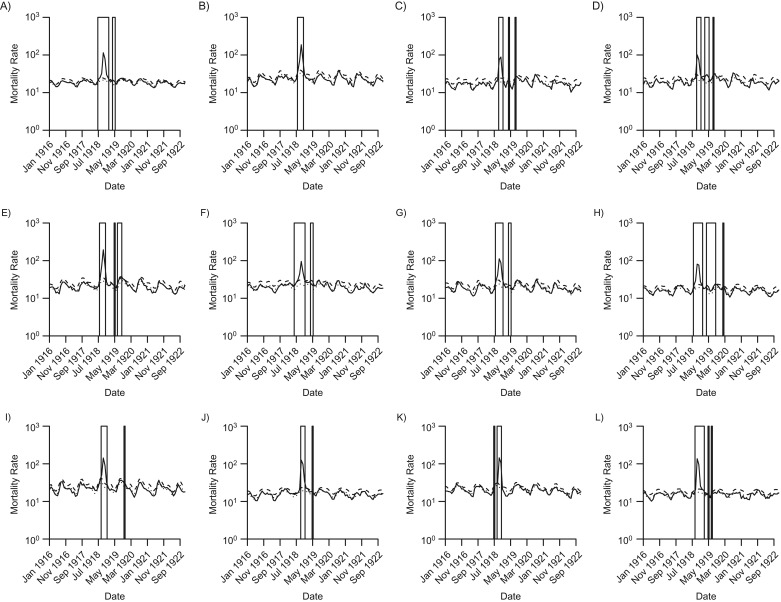
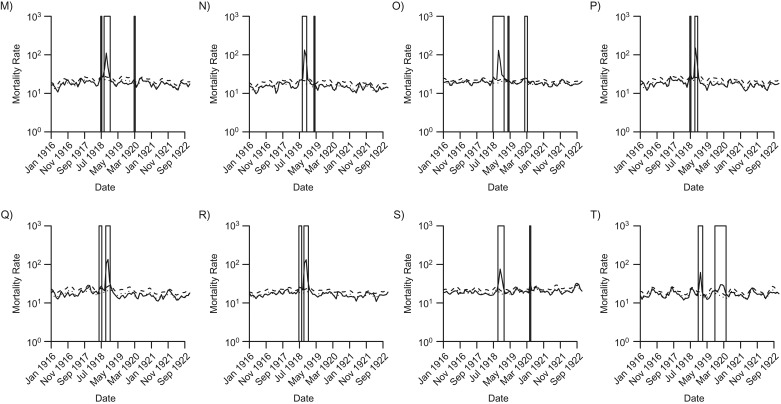
Negative binomial models presented better fits to the interrupted mortality time series than did Poisson regression models for most of the districts and all-cause deaths. All time series were overdispersed (Web Tables 2 and 3). Two periods of all-cause excess mortality were observed at the national level during the first year of circulation of the pandemic virus (June 1918 to June 1920). A first, extended pandemic period ran from July 1918 to January 1919, with a peak in October 1918. A second, shorter pandemic period was identified during April to May 1919, with a peak in April (Figure 1).
Figure 1.
Observed, baseline (in the absence of influenza pandemic impact), and upper 95% baseline prediction limit, monthly all-cause mortality rates per 10,000 inhabitants (in logarithm base 10 scale) from 1916 to 1922 in Portugal overall and 19 districts. Vertical boxes represent the periods with excess mortality, when observed all-cause mortality was above the 95% prediction limit of the baseline. (A) Portugal overall, (B) Bragança, (C) Viana do Castelo, (D) Braga, (E) Vila Real, (F) Porto, (G) Viseu, (H) Aveiro, (I) Guarda, (J) Coimbra, (K) Castelo Branco, (L) Leiria, (M) Portalegre, (N) Santarém, (O) Lisboa, (P) Évora, (Q) Beja, (R) Faro, (S) Açores, and (T) Madeira.
Overall, the 1918–1919 influenza pandemic was associated with an estimated 117,764 excess all-cause deaths, representing a rate of 195.7 deaths per 10,000 inhabitants. The highest impact was observed in the first pandemic period that extended from summer 1918 to winter 1918–1919 and accounted for 95% of excess deaths (186.88 per 10,000 inhabitants). The second period in spring 1919 accounted for 8.86 deaths per 10,000 inhabitants. The distribution of these periods of excess deaths was not homogenous at the district level, and 4 pandemic waves were revealed: summer 1918, fall/winter 1918–1919, spring 1919, and winter 1919–1920 (Table 1; Web Figures 1 and 2). Southeastern Portugal and the districts encompassing the main cities districts, Lisboa and Porto, were first hit. In the first wave (June to August 1918), excess mortality was identified in 11 districts, 6 of which were on the eastern border with Spain. The average all-cause mortality rate was 6.25 (range, 0 to 20.36 in Porto) per 10,000 inhabitants.
Table 1.
All-Cause Excess Mortality Rates According to the Defined 1918–1919 Influenza Pandemic Phase, Mainland Districts and Archipelagos of Madeira and Azores, Portugal
| Districta | Phase 1 | Phase 2 | Phase 3 | Phase 4 | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| June to August 1918 | September 1918 to February 1919 | March to September 1919 | October 1919 to June 1920 | |||||||
| Rateb | 95% CI | Rateb | 95% CI | Rateb | 95% CI | Rateb | 95% CI | Rateb | 95% CI | |
| Portugal | 8.82 | 4.54, 12.67 | 178.05 | 171.18, 185.54 | 8.86 | 5.65, 12.10 | 0.00 | 195.73 | 185.84, 206.00 | |
| Bragança | 11.09 | 4.28, 16.68 | 239.55 | 226.58, 251.09 | 0.00 | 0.00 | 250.20 | 234.38, 264.23 | ||
| Viana do Castelo | 0.00 | 133.66 | 124.12, 142.93 | 14.77 | 6.45, 22.20 | 0.00 | 148.01 | 134.94, 160.49 | ||
| Braga | 0.00 | 141.28 | 129.69, 151.68 | 41.42 | 28.65, 52.90 | 0.00 | 182.41 | 165.33, 200.02 | ||
| Vila Real | 8.82 | 4.54, 12.67 | 178.05 | 171.18, 185.54 | 8.86 | 5.65, 12.10 | 0.00 | 299.00 | 277.40, 320.60 | |
| Porto | 20.36 | 9.92, 29.83 | 130.64 | 117.06, 142.07 | 22.41 | 14.06, 29.40 | 0.00 | 173.10 | 152.22, 193.03 | |
| Viseu | 8.82 | 4.54, 12.67 | 178.05 | 171.18, 185.54 | 8.86 | 5.65, 12.10 | 0.00 | 207.18 | 190.20, 221.57 | |
| Aveiro | 7.06 | 3.99, 9.80 | 143.06 | 132.63, 152.75 | 30.22 | 22.29, 37.50 | 3.69 | 0.13, 6.65 | 183.89 | 167.42, 198.45 |
| Guarda | 0.00 | 212.12 | 197.07, 226.33 | 0.00 | 9.40 | 3.54, 14.41 | 221.07 | 204.63, 236.36 | ||
| Coimbra | 0.00 | 202.01 | 193.59, 209.08 | 5.08 | 2.17, 7.80 | 0.00 | 206.95 | 198.16, 214.99 | ||
| Castelo Branco | 4.94 | 0.73, 8.90 | 211.57 | 203.14, 219.05 | 0.00 | 0.00 | 216.43 | 207.56, 224.68 | ||
| Leiria | 0.00 | 218.04 | 208.16, 228.02 | 7.26 | 2.85, 11.60 | 0.00 | 225.20 | 213.80, 237.03 | ||
| Portalegre | 5.30 | 0.07, 9.63 | 143.04 | 132.24, 153.37 | 0.00 | 11.26 | 5.26, 16.57 | 159.47 | 144.76, 172.75 | |
| Santarém | 0.00 | 197.58 | 189.00, 205.02 | 4.94 | 0.95, 8.10 | 4.95 | 1.02, 8.54 | 207.36 | 196.63, 216.67 | |
| Lisboa | 12.48 | 7.45, 17.33 | 184.18 | 175.94, 192.17 | 4.22 | 1.21, 6.90 | 14.85 | 8.77, 20.23 | 215.43 | 202.78, 229.48 |
| Évora | 11.43 | 5.29, 17.10 | 176.53 | 168.94, 183.26 | 0.00 | 0.00 | 187.90 | 177.42, 197.54 | ||
| Beja | 15.01 | 6.45, 22.00 | 212.82 | 202.01, 223.33 | 0.00 | 0.00 | 227.49 | 213.32, 241.43 | ||
| Faro | 13.38 | 6.45, 19.36 | 222.29 | 214.48, 229.51 | 0.00 | 4.16 | 0.25, 7.10 | 239.55 | 228.24, 250.59 | |
| Açores | 0.00 | 106.35 | 99.06, 113.92 | 0.00 | 16.51 | 12.69, 19.63 | 122.48 | 113.31, 130.94 | ||
| Madeira | 0.00 | 58.46 | 52.20, 64.22 | 0.00 | 62.15 | 52.86, 71.69 | 121.14 | 109.00, 134.03 | ||
Abbreviation: CI, confidence interval.
a Districts are ordered from north to south, except the archipelagos of Açores and Madeira.
b Rate was calculated per 10,000 inhabitants.
The second pandemic phase (September 1918 to February 1919) had a much higher impact on all districts. The average all-cause mortality rate was 173.12 per 10,000 inhabitants, ranging from 130.64 in Porto to 239.55 per 10,000 in Bragança on the mainland. The archipelagos Açores and Madeira had the lowest excess mortality rates: 106.35 and 58.46 deaths per 10,000 inhabitants, respectively.
In Vila Real, Porto, Viseu, Aveiro, and Lisboa, the first and second pandemic phases were indistinguishable; excess mortality started in summer and extended to fall or winter (Web Figure 2). The third (March to September 1919) and fourth pandemic phases (October 1919 to June 1920) had a much smaller impact than the second. The highest impact of the third phase was observed in the north and on the west coast. The fourth phase had also a high impact on the islands, specifically in Madeira, where the all-cause excess mortality rate was higher than that seen in the second phase (62.15 per 10,000 inhabitants).
Overall, for the period 1918–1920, Vila Real, in northern Portugal, was the district with highest excess all-cause mortality rate (299.00 deaths per 10,000 inhabitants); the lowest rate was observed in Madeira, with 121.14 deaths per 10,000.
Considering excess mortality due to respiratory causes, we attribute 63,869 excess deaths to the full pandemic period (106.15 per 10,000) (Web Table 4, Web Figures 3–5). There was no clear correspondence between periods of excess mortality in respiratory-related and all-cause death data at the district level. The district with highest excess mortality rate due to respiratory causes was Castelo Branco (ranked seventh in all-cause deaths), whereas Madeira had the lowest rate. The correlation between all-cause and respiratory-related excess mortality was moderate at the district level (Spearman ρ = 0.56, 95% confidence interval (CI): 0.15, 0.81). When restricted to the second phase of the pandemic (September 1918 to February 1919), the correlation increased somewhat (Spearman ρ = 0.62, 95% CI: 0.23, 0.84).
Sociodemographic factors associated with excess deaths
There was no spatial dependency in the residuals of the Poisson regression models (Table 2). In the first pandemic phase (June to August 1918), longitude and latitude were the only significant predictors associated with excess mortality (Table 2). Excess mortality rates were higher in the eastern (adjusted mortality rate ratio (aMRR) = 4.47, 95% CI: 1.13, 19.66) and southern (aMRR = 0.56, 95% CI: 0.37, 0.85) directions.
Table 2.
All-Cause Excess Mortality Rate Distribution and Excess Mortality Rate Ratios, According to the District-Level Sociodemographic Characteristics, for the 4 Phases of the 1918–1919 Influenza Pandemic in Portugal
| Predictor | Ratea | MRR (Crude) | 95% CI | aMRRb | 95% CI |
|---|---|---|---|---|---|
| Phase 1 (June to August 1918)c | |||||
| Population density per km2 | |||||
| <49 | 7.35 | 1.00 | Referent | 1.00 | Referent |
| 49–101 | 4.73 | 0.64 | 0.23, 1.84 | 1.42 | 0.48, 4.18 |
| ≥101 | 9.43 | 1.28 | 0.52, 3.17 | 9.41 | 0.97, 91.21 |
| Illiteracy rate, % | |||||
| <73 | 8.86 | 1.00 | Referent | 1.00 | Referent |
| ≥73 | 5.90 | 0.67 | 0.28, 1.59 | 0.58 | 0.06, 5.57 |
| Infant mortality rate, per thousand | |||||
| <142 | 4.17 | 1.00 | Referent | 1.00 | Referent |
| 142–159 | 9.77 | 2.34 | 0.70, 7.81 | 1.58 | 0.49, 5.06 |
| ≥159 | 8.44 | 2.02 | 0.80, 5.11 | 0.76 | 0.23, 2.59 |
| Population aged 5–14 years, % | |||||
| <23 | 7.87 | 1.00 | Referent | 1.00 | Referent |
| ≥23 | 7.44 | 0.95 | 0.35, 2.57 | 0.98 | 0.36, 2.68 |
| Longitude | 1.67 | 0.99, 1.38 | 4.71 | 1.13, 19.66 | |
| Latitude | 1.04 | 0.81, 1.34 | 0.56 | 0.37, 0.85 | |
| Phase 2 (September 1918 to February 1919)c | |||||
| Population density per km2 | |||||
| <49 | 202.99 | 1.00 | Referent | 1.00 | Referent |
| 49–101 | 210.44 | 1.04 | 0.91, 1.18 | 1.11 | 0.93, 1.33 |
| ≥101 | 143.93 | 0.71 | 0.57, 0.88 | 0.73 | 0.56, 0.95 |
| Illiteracy rate, % | |||||
| <73 | 162.65 | 1.00 | Referent | 1.00 | Referent |
| ≥73 | 193.55 | 1.19 | 0.98, 1.44 | 0.88 | 0.73, 1.05 |
| Infant mortality rate, per thousand | |||||
| <142 | 189.08 | 1.00 | Referent | 1.00 | Referent |
| 142–159 | 155.59 | 0.82 | 0.63, 1.08 | 1.02 | 0.90, 1.15 |
| ≥159 | 183.87 | 0.97 | 0.80, 1.18 | 1.14 | 0.96, 1.35 |
| Population aged 5–14 years, % | |||||
| <23 | 176.18 | 1.00 | Referent | 1.00 | Referent |
| ≥23 | 176.15 | 1.00 | 0.84, 1.19 | 0.99 | 0.87, 1.11 |
| Longitude | 1.69 | 1.06, 1.08 | 1.05 | 1.03, 1.06 | |
| Latitude | 1.02 | 0.95, 1.09 | 0.99 | 0.96, 1.03 | |
| Phase 3–4 (March 1919 to June 1920)c | |||||
| Population density per km2 | |||||
| <49 | 3.47 | 1.00 | Referent | 1.00 | Referent |
| 49–101 | 11.12 | 3.20 | 0.92, 11.08 | 3.72 | 1.14, 12.16 |
| ≥101 | 26.60 | 7.66 | 2.40, 24.42 | 6.12 | 1.33, 28.16 |
| Illiteracy rate, % | |||||
| <73 | 22.75 | 1.00 | Referent | 1.00 | Referent |
| ≥73 | 10.22 | 0.45 | 0.20, 1.01 | 0.76 | 0.30, 1.96 |
| Infant mortality rate, per thousand | |||||
| <142 | 17.06 | 1.00 | Referent | 1.00 | Referent |
| 142–159 | 23.36 | 1.37 | 0.65, 2.90 | 0.93 | 0.54, 1.60 |
| ≥159 | 12.08 | 0.71 | 0.32, 1.56 | 1.85 | 0.75, 4.55 |
| Population aged 5–14 years, % | |||||
| <23 | 14.71 | 1.00 | Referent | 1.00 | Referent |
| ≥23 | 18.34 | 1.25 | 0.7, 2.21 | 1.56 | 0.78, 3.13 |
| Longitude | 0.93 | 0.91, 0.95 | 0.91 | 0.85, 0.97 | |
| Latitude | 1.10 | 0.91, 1.32 | 1.30 | 1.08, 1.58 |
Abbreviations: aMRR, adjusted mortality rate ratio; CI, confidence interval; MRR, mortality rate ratio.
a Rate was calculated per 10,000 inhabitants.
b Mortality rate ratio was adjusted by Poisson regression.
c Moran I statistics for model residuals were as follows: for phase 1, P = 0.637; for phase 2, P = 0.867; for phases 3 and 4, P = 0.820.
In the second pandemic phase, population density was associated with all-cause excess mortality. More specifically, the third tertile of population density (aMRR = 0.73, 95% CI: 0.56, 0.95) was protective, and the excess mortality rate increased with longitude (aMRR = 1.05, 95% CI: 1.03, 1.06).
Considering the third and fourth pandemic phases together, the positive predictors of excess mortality were latitude (aMRR = 1.30, 95% CI: 1.08, 1.58), with increased excess mortality rate in the northern direction, and in the second and third tertiles of population density. Longitude in these 2 phases was negatively associated with excess mortality (aMRR = 0.93, 95% CI: 0.85, 0.97), suggesting an increased excess mortality rate in the western direction.
DISCUSSION
To our knowledge, we have generated in this study the first estimates of excess mortality associated with the 1918–1919 pandemic in Portugal, using detailed primary data sources and up-to-date statistical methods. The 1918–1919 influenza pandemic was associated with an estimated 117,764 excess all-cause deaths, representing an excess mortality rate of 195.7 deaths per 10,000 inhabitants (95% CI: 185.8, 206.0). On a national scale, 2 main periods of excess mortality were identified—July 1918 to January 1919 and April to May 1919—however, the timing of excess mortality differed by district, with up to 4 waves identified during 1918–1920.
Our mortality estimate for Portugal is significantly lower than those reported in previous studies. Murray et al. (3) estimated an excess death rate of 264 per 10,000 persons and Ansart et al. (6) estimated 223 per 10,000 persons. It is plausible that the impact of the influenza pandemic in Portugal was overestimated in these studies. Murray et al. (3) analyzed annual time series, which is a less precise approach than modeling of monthly data. Although Ansart et al. (6) used monthly data, they reported Portugal was first affected in March 1918, which is inconsistent with official data published by Portuguese authorities (17). The first influenza pandemic cases were reported in the Évora district (southeastern Portugal) in May 1918 and were imported from Spain (17). These official reports, as well as 1918 Spanish and Portuguese press reports (18, 19), are more consistent with our findings of a rise in pandemic mortality in June 1918. We note that the excess mortality identified in March 1918 by Ansart et al. (6) coincided with an outbreak of exanthematous typhus (8).
The spatiotemporal pattern of all-cause excess mortality observed in our study is in accordance with data from Spain reported by Chowell et al. (20). During summer 1918, the most affected districts were located along the southeastern border with Spain, except the districts encompassing the main cities of Porto and Lisboa.
The early onset of the pandemic in southern Portugal, Lisboa, and Porto could reflect the main entry routes of the pandemic virus into Portugal in 1918 (21). At the time, international travel was primarily by boat and by land from Spain, mainly by railway or other terrestrial transportation.
Considering the total pandemic period 1918–1920, the most affected districts were located in northeastern Portugal (Bragança, Vila Real, and Guarda) and in the south (Beja and Faro). The most affected districts in the north of Portugal border with Zamora, Orense, and Salamanca, aligning with northwestern Spain and forming an Iberian cluster of a high excess mortality (20).
There was considerable variability in pandemic timing between districts, with 4 phases of excess mortality. The first, milder one started in June and ended in August 1918, although, in some districts, like Lisboa and Porto, this first period was indistinct from the later pandemic wave. The second pandemic wave had a 20-fold greater impact than did the summer period at the national level, affected all districts, and ran from September 1918 to February 1919. The third and fourth phases in spring 1919 and fall/winter 1919–1920 were milder. These patterns are concordant with the periods with excess mortality identified in Spain, with a delay of 1–2 months (20). Similar mortality patterns, with the brunt of mortality occurring in fall and winter 1918–1919, were observed in Europe (6) and other parts of the globe (3).
We found associations between all-cause excess mortality and geographic and sociodemographic factors, which differed by pandemic phase. During the summer phase, there was an association with longitude and latitude, reflecting the higher impact in southeastern Portugal. In the fall/winter 1918–1919 wave, excess mortality was negatively associated with population density, consistent with findings of a Spanish study (20). The geographic data indicate the second pandemic phase had higher impact in rural districts. On the other hand, during the drawn-out third and fourth phases, population density was positively associated with excess death rate. These results are consistent with the Portuguese health authority’s reports that described these later mortality waves as more prevalent in urban areas (5). During the third and fourth phases of the pandemic, the geography of excess mortality was the opposite of the first phase, with higher impact in the northern and western districts (including Azores and Madeira).
No association between sociodemographic factors and influenza mortality rates in 1918 was identified in previous studies in Portugal (12). This lack of association could be partly explained by the high rate of deaths of unknown cause reported in 1918 (44%), with considerable variation between districts, from 1.1% in Madeira to 82.4% in Bragança. The high rate of deaths with “unknown cause” limits the validity of any excess death estimate based on cause-specific mortality in Portugal and may explain the moderate correlation between all-cause and respiratory-related excess mortality in our data (Spearman ρ = 0.56, compared with 0.82 in Spain (20)).
Our study has some limitations. First, we used data published in demographic statistics documents that were scanned, printed, and manually entered in a database. Nevertheless, the times-series data were, overall, very consistent, except for cause-specific deaths in Bragança district (Web Figure 3). We used a nonspecific outcome, all-cause mortality, which could result in an overestimate of excess deaths, given that all-cause mortality includes deaths that could not be attributed to influenza infection (e.g., those related to injuries). However, with a very high and variable proportion of unspecified deaths, using excess deaths resulting from respiratory causes was not appropriate for the main analysis. On the other hand, the use of all-cause mortality time series has been shown to be a consistent approach to identify excess deaths attributable to influenza epidemics, especially in the case of the lethal 1915–1919 influenza pandemic. In addition, the all-cause excess mortality periods identified in the present study are consistent with those reported in the national (12, 17, 22) and international literature (20, 21).
We cannot fully exclude that our all-cause mortality estimates could be overestimated in some districts and periods. During the years 1918–1919, there were other concurrent epidemics with considerable impact on death rates, namely, exanthematous typhus during the months of March to June 1919 and a national smallpox epidemic from May 1918 to December 1918. These epidemics overlapped the identified periods of pandemic activity. However, smallpox and exanthematous typhus deaths correspond to only 2% of the total of deaths in those periods. Another limitation of our study was the lack of monthly data by age group that were not available at national or district levels and precluded any description of the heterogeneity of the pandemic impact by wave and age group, as described in other European countries (4).
In conclusion, our results clarify the impact of the 1918–1919 influenza pandemic in Portugal and provide updated and more accurate estimates at the national and subnational levels. We note remarkable consistencies with the pandemic dynamics in Spain, which shed light on the pandemic experience in the Iberian Peninsula. It is clear from this study that the influenza pandemic arrived in southern Portugal in summer, originating from Spain; thus, Portugal is 1 of the only countries that truly could name the 1918–1919 influenza pandemic the “Spanish flu” (10). In addition, by combining our results with those of Chowell et al. (20), we identified a cluster of high excess mortality in the northwestern Iberian Peninsula.
Overall, we found the 1918–1919 influenza pandemic in Portugal had a very high impact that extended from June 1918 to June 1920. Death rates varied considerably among districts and were mainly associated with several sociodemographic characteristics, including population density and a north-to-south and west-to-east gradient.
Archeo-epidemiologic studies of the kind we present are useful for pandemic preparedness because they may contribute to prioritization of preventive and prophylactic measures, not only according to known health risk factors but also to vulnerable sociodemographic groups. Knowledge of domestic and international population mobility also would be essential to establish active surveillance systems and build scenarios of pandemic spread.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Instituto Nacional de Saúde Dr. Ricardo Jorge, Lisboa, Portugal (Baltazar Nunes, Susana Silva, Ana Rodrigues, Rita Roquette, Inês Batista); Centro de Investigação em Saúde Pública, Escola Nacional de Saúde Pública, Universidade NOVA de Lisboa, Lisboa, Portugal (Baltazar Nunes); Department of Infectious Diseases, Instituto Nacional de Saúde Dr. Ricardo Jorge, Lisboa, Portugal (Helena Rebelo-de-Andrade); and Host-Pathogen Interaction Unit, Research Institute for Medicines (iMed.ULisboa), Faculdade de Farmácia, Universidade de Lisboa, Lisbon, Portugal (Helena Rebelo-de-Andrade).
Funding: none.
Conflict of interest: none declared.
Abbreviations
- CI
confidence interval
- aMRR
adjusted mortality rate ratio
REFERENCES
- 1. Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76(1):105–115. [DOI] [PubMed] [Google Scholar]
- 2. Simonsen L, Chowell G, Andreasen V, et al. . A review of the 1918 herald pandemic wave: importance for contemporary pandemic response strategies. Ann Epidemiol. 2018;28(5):281–288. [DOI] [PubMed] [Google Scholar]
- 3. Murray CJ, Lopez AD, Chin B, et al. . Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: a quantitative analysis. Lancet. 2006;368(9554):2211–2218. [DOI] [PubMed] [Google Scholar]
- 4. Erkoreka A. The Spanish influenza pandemic in occidental Europe (1918–1920) and victim age. Influenza Other Respir Viruses. 2010;4(2):81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sampaio A. Subsídios para o estudo da epidemiologia da gripe. Lisbon, Portugal: Edição de Autor; 1958. [Google Scholar]
- 6. Ansart S, Pelat C, Boelle PY, et al. . Mortality burden of the 1918–1919 influenza pandemic in Europe. Influenza Other Respir Viruses. 2009;3(3):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jorge R. Tifo exantemático ou tabardilho: relatório apresentados ao Conselho Superior de Higiene. Lisboa, Portugal: Imprensa Nacional; 1918. [Google Scholar]
- 8. de Morais JAD. Tifo epidémico em Portugal: um contributo para o seu conhecimento histórico e epidemológico. Med Interna (Bucur). 2008;15(3):214–223. [Google Scholar]
- 9. Jorge R. A influenza pneumónica: notas sobre a epidemia, comunicados e instruções da Direcção Geral da Saúde. Lisboa, Portugal: Conselho Superior de Higiene; 1918. [Google Scholar]
- 10. Jorge R. La grippe: Rapport préliminaire présenté à la Comission Sanitaire des pays Alliés dans sa session de mars 1919. Bull l’Office Int d’hygiène publique. 1919;XI(3):381. [Google Scholar]
- 11. Rebelo-De-Andrade H. Aspectos Epidemiológicos e Virológicos da Gripe: Desenvolvimento de um Sistema de Vigilância. Lisboa, Portugal: Universidade de Lisboa; 2001. [Google Scholar]
- 12. Frada J. A Gripe Pneumónica em Portugal Continental 1918. Lisboa, Portugal: SeteCaminhos; 2005. [Google Scholar]
- 13. Instituto Nacional de Estatística Biblioteca Digital Lisboa, Portugal: Instituto Nacional Estatística; 2018. http://inenetw02.ine.pt:8080/biblioteca/logon.do;jsessionid=6D32727EEDCD9F2223353F2D3D81DB70.
- 14. Davison AC, Hinkley DV. Bootstrap Methods and Their Application. New York, NY: Cambridge University Press; 2013. [Google Scholar]
- 15. Cameron AC, Trivedi PK. Regression-based tests for overdispersion in the Poisson model. J Econom. 1990;46(3):347–364. [Google Scholar]
- 16. R Core Team R: A Language and Environment for Statistical Computing Vienna, Austria: The R Foundation; 2017. https://www.r-project.org/.
- 17. Jorge R. A Influenzae e a Febre do Papatazes. Lisboa, Portugal: Imprensa Nacional de Lisboa; 1918. [Google Scholar]
- 18.La enfermedad de moda. La Manãna. May 23, 1918:11.
- 19.A gripe infeciosa. A Capital. June 17, 1918: 1.
- 20. Chowell G, Erkoreka A, Viboud C, et al. . Spatial-temporal excess mortality patterns of the 1918–1919 influenza pandemic in Spain. BMC Infect Dis. 2014;14:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Trilla A, Trilla G, Daer C. The 1918 “Spanish flu” in Spain. Clin Infect Dis. 2008;47(5):668–673. [DOI] [PubMed] [Google Scholar]
- 22. Sequeira A. A pneumónica. Med Interna (Bucur). 2001;8(1):49–55. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.