Abstract
Objectives:
Respiratory failure with mechanical ventilation is a limited labor-intensive resource that is associated with high mortality. Understanding the longitudinal national epidemiology is essential for the organization of healthcare resources.
Design:
Serial cross-sectional study.
Setting:
The 2002–2017 Healthcare Utilization Project’s National Inpatient Sample datasets.
Interventions:
None.
Measurements:
We use six diagnosis codes and five procedural codes from International Classification of Diseases, 9th Revision, Clinical Modification, and 19 diagnosis codes and 15 procedures codes from International Classification of Diseases, 10th Revision, Clinical Modification to examine national epidemiology of different case definitions for respiratory failure.
Results:
In the United States in 2017, there were an estimated 1,146,195 discharges with a diagnosis of respiratory failure and procedural code for mechanical ventilation, with an average length of stay of 10.5 days and hospital charge of $158,443. Over the study period, there was an 83% increase in incidence from 249 to 455 cases per 100,000 adults with a 48% decrease in hospital mortality from 34% to 23%. Exploring a case definition that captures only diagnosis codes for respiratory failure, there was a 197% increase in annual incidence, from 429 to 1,275 cases per 100,000 adults with a 57% decrease in hospital mortality from 28% to 12%. For invasive mechanical ventilation without a requisite diagnosis code, there was no change in incidence over the study period, with the 2017 incidence at 359 cases per 100,000 adults, but a 19% decrease in hospital mortality from 37% to 30%. For the noninvasive mechanical ventilation procedural codes, there was a 437% increase in incidence from 41 to 220 cases per 100,000 adults, with a 38% decrease in hospital mortality from 16% to 10%.
Conclusions:
Examining different case definitions for respiratory failure, there was a large increase in the population incidence and decrease in the hospital mortality for respiratory failure diagnosis codes with more modest changes procedural codes for invasive mechanical ventilation. There was a large increase in incidence of noninvasive mechanical ventilation.
Keywords: epidemiology, health services research, mechanical ventilation, respiratory failure
Respiratory failure is a life-threatening condition that requires high resource utilization and that is associated with significant acute mortality, particularly when requiring mechanical ventilation, a potentially life-saving intervention that is a limited, costly, and labor-intensive resource. Furthermore, survivors of respiratory failure face significant subsequent physical, psychologic, and cognitive morbidity (1–3). Given the costly public health and health systems burden of this medical condition (4), it is critical to understand the longitudinal incidence and epidemiology of respiratory failure in the United States in order estimate the breadth, evolving patient characteristics, and trajectory of this public health problem. In addition to the importance of continued surveillance of respiratory failure for estimating public health burden, there have been important changes in the critical care ecosystem throughout the early 2000s that conceivably affect the care of patients with respiratory failure. These include technological changes such as widespread use of noninvasive mechanical ventilation (NIV), development of high flow oxygen delivery devices, and propagation of the electronic health record; treatment advances with the diffusion of lung protective ventilation practices and validation of prone positioning for advanced forms of respiratory failure; and work force changes in the growing roles of respiratory therapists, physician assistants, and nurse practitioners. These changes warrant continued longitudinal epidemiologic study of the resource utilization and outcomes of those with respiratory failure in the United States.
In this study, we aim to describe the epidemiology of respiratory failure in the United States from 2002 to 2017 utilizing the largest publicly available hospital discharge dataset to produce national estimates. First, we seek to strengthen on previously deployed methodology by expanding the level of analytic detail to include multiple respiratory failure case definitions to provide a more granular view of the use of mechanical ventilation, tracheostomy, and extracorporeal membrane oxygenation (ECMO) resources and outcomes of different case definitions of respiratory failure (5–7). Then from this multifaceted analysis, we narrow the focus onto a single, conceptually specific case definition to provide greater detail on patient characteristics of respiratory failure and mechanical ventilation in the United States during the study period.
MATERIALS AND METHODS
Study Design and Data Sources
This is a serial cross-sectional study utilizing the 2002–2014 and 2016–2017 Healthcare Utilization Project’s National Inpatient Sample (NIS). The NIS is a complex, stratified sample of administrative hospital discharge records from nonfederal, short-term hospitals from participating states and is the largest publicly available all-payer inpatient healthcare database in the United States, including more than 7 million hospital stays per year (8). There have been important changes in the annual sample over our study period: 1) the number of participating states increased from 35 to 48, including the District of Columbia; 2) in 2012 the sample no longer included long-term acute care hospitals; 3) in 2012 the sample design changed from a sample of all discharges from selected hospitals to a selected sample of discharges from all available hospitals; and 4) in 2015 diagnosis and procedure reporting changed from International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) coding to the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) (8). To facilitate national estimation in trend analyses across these years, the NIS constructed new sampling weights (9). In addition to NIS, we used the annual U.S. Census Bureau annual population estimates for those greater than or equal to 18 years old for the denominators in the calculation of annual incidences (10, 11). The 2015 year was not included in this analysis, given that the ICD coding changed during the year, preventing the use of standard methods for making annual estimates with either coding system for that year.
Participants and Variables
We identified respiratory failure discharges by ICD-9-CM and ICD-10-CM diagnosis and procedure codes (eTables 1–3, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). For our case definitions, we used procedure codes to define those cases of respiratory failure that required invasive mechanical ventilation (IMV), NIV, temporary tracheostomy, or ECMO (eTables 1–3, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). Other patient and hospital variables included in the analyses were available from NIS. The NIS produces specific derived variables to facilitate analyses, including chronic comorbidities constructed as dichotomous variables using the Elixhauser taxonomy, two four-category ordinal variables for severity of illness and risk of mortality, and a clinical classification software that reclassifies thousands of ICD codes into a smaller number of clinically meaningful categories which we used to identify principal diagnoses (12–14). We excluded those under 18 years old and those who were transferred in from another hospital. Of note, throughout the study period, the proportion of annual respiratory failure cases receiving ECMO were less than 1% and from 2002 to 2017 the proportion of patients where race/ethnicity was missing ranged from 8% to 25%; therefore, while these results are included in eTables 5, a and b, and 6 (Supplemental Digital Content 1, http://links.lww.com/CCX/A180), they are not presented here.
Statistical Analysis
This is a descriptive analysis utilizing the SAS 9.4 (SAS Institute, Cary, NC) “SURVEY” family of procedures to account for the complex, stratified sample design of the NIS and produce weighted, national estimates. As such, we present no unweighted data. We replaced the original sample weights with the trend weights that NIS constructed to facilitate multiyear trend analyses across the 2012 sample redesign (9). We used the “DOMAIN” statement in the SAS SURVEY procedures to generate national estimates that account for the excluded discharges in variance estimate calculations (15). Nonoverlapping 95% CIs are used to make inferences about significant differences between estimates from the independent annual samples. These CIs appear in the tables of the article and online supplement but are not presented in article text to facilitate readability. All figures were created using the “ggplot2” 3.2.1 package in RStudio 1.1.463 (RStudio, Inc., Boston, MA; http://www.rstudio.com/). For the analytic approach, we first examined each respiratory failure case definition separately then constructed an inclusive case definition of respiratory failure as a discharge with any of the diagnosis codes for respiratory failure and any of the procedural codes for endotracheal intubation or mechanical ventilation present among the discharge record.
This work was performed with publicly available, de-identified data and therefore is not consider human subjects research or require Institutional Review Board review.
RESULTS
Incidence and Mortality of Composite Case Definitions of Respiratory Failure and Mechanical Ventilation
In the United States in 2017, there were an estimated 3,213,030 hospital discharges with a diagnosis code of respiratory failure, 903,745 discharges with a procedure code for IMV, 555,605 discharges with a procedural code for NIV, and 1,146,195 discharges with a diagnosis of respiratory failure and a procedural code for IMV or NIV (totals for other years available in eTable 4, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). From 2002 to 2017, the national adult annual incidence of respiratory failure increased and the hospital mortality decreased by varying magnitudes depending on the configuration of the composite ICD-9-CM case definition (Figs. 1 and 2; and eTable 5, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). When combining all respiratory failure “diagnosis” codes, there was a 197% increase in incidence, from 429 to 1,275 cases per 100,000 adults per year with a 57% decrease in hospital mortality from 28% to 12%. When combining IMV procedure codes only without a requisite respiratory failure diagnosis code, there was no significant change in the incidence but a 19% decrease in hospital mortality from 37% to 30%. When examining the incidence of NIV procedural code alone, there was a 437% increase in incidence from 41 to 220 cases per 100,000 adults, with a 38% decrease in hospital mortality from 16% to 10%. When combining all respiratory failure diagnosis codes and requiring an accompanying mechanical ventilation codes (endotracheal intubation, IMV, or NIV), there was an 83% increase in incidence from 249 to 455 cases per 100,000 adults with a 48% decrease in hospital mortality from 34% to 23%.
Figure 1.
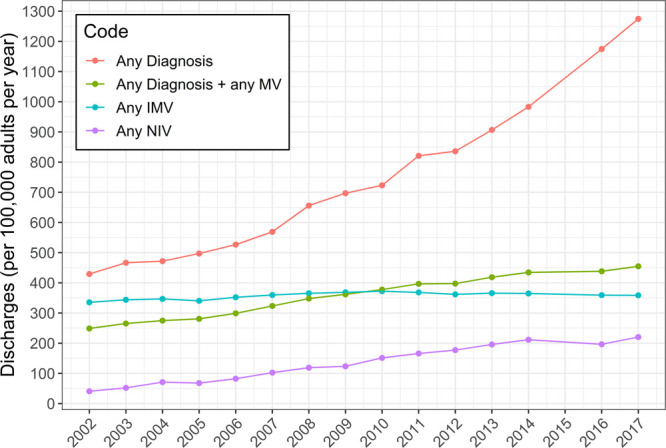
National annual incidence of composite diagnosis and mechanical ventilation (MV) codes for respiratory failure, 2002–20171. 1Annual estimate was not calculated for 2015. Any diagnosis = a discharge containing any of the diagnosis codes for respiratory failure, any diagnosis + any MV = a discharge with any of the diagnosis codes for respiratory failure plus any procedural codes for invasive MV (IMV) or noninvasive MV (NIV), any IMV = a discharge containing any of the procedural codes for endotracheal intubation or IMV, any NIV = a discharge with a procedural code for NIV.
Figure 2.
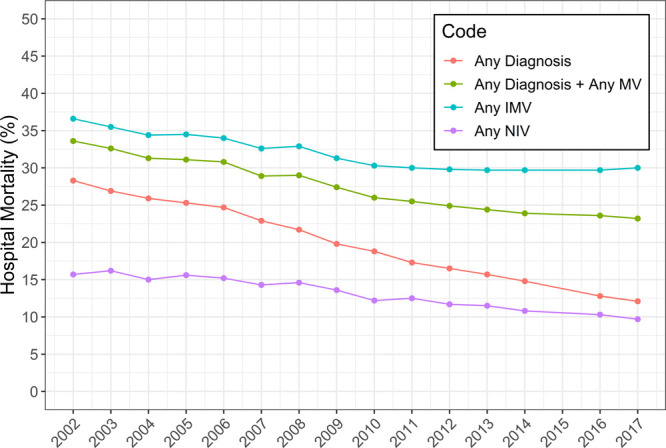
Hospital mortality for composite diagnosis and mechanical ventilation (MV) codes for respiratory failure, 2002–20171. 1Annual estimate was not calculated for 2015. Any diagnosis = a discharge containing any of the diagnosis codes for respiratory failure, any diagnosis + any MV = a discharge with any of the diagnosis codes for respiratory failure plus any procedural codes for invasive MV (IMV) or noninvasive MV (NIV), any IMV = a discharge containing any of the procedural codes for endotracheal intubation or IMV, any NIV = a discharge with a procedural code for NIV.
Patient Characteristics and Outcomes of Respiratory Failure With Mechanical Ventilation
To capture a single population conceptually encompassing of clinical respiratory failure for more detailed analysis, for this part of the results, we narrow the focus to a single case definition of respiratory failure: discharges with any diagnosis code for respiratory failure with any procedure code for mechanical ventilation (endotracheal intubation, IMV, and NIV) in order to provide a more in-depth description of patient characteristics (annual data tables in full in eTables 6–10, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). Utilizing this case definition, comparing 2002 to 2017 there have been changes in the characteristics of patients with respiratory failure and mechanical ventilation (Table 1): increases in the proportion of patients between 18 and 29 and 50–69 years old with decreases in the proportions of patients 40–49 and greater than or equal to 70 years old, decrease in the proportion of female patients, increase in the proportion of patients with Medicaid as the primary expected payor source and coincident decrease in the proportion with private insurance as the payor.
TABLE 1.
Characteristics of Patients With Respiratory Failure and Mechanical Ventilation
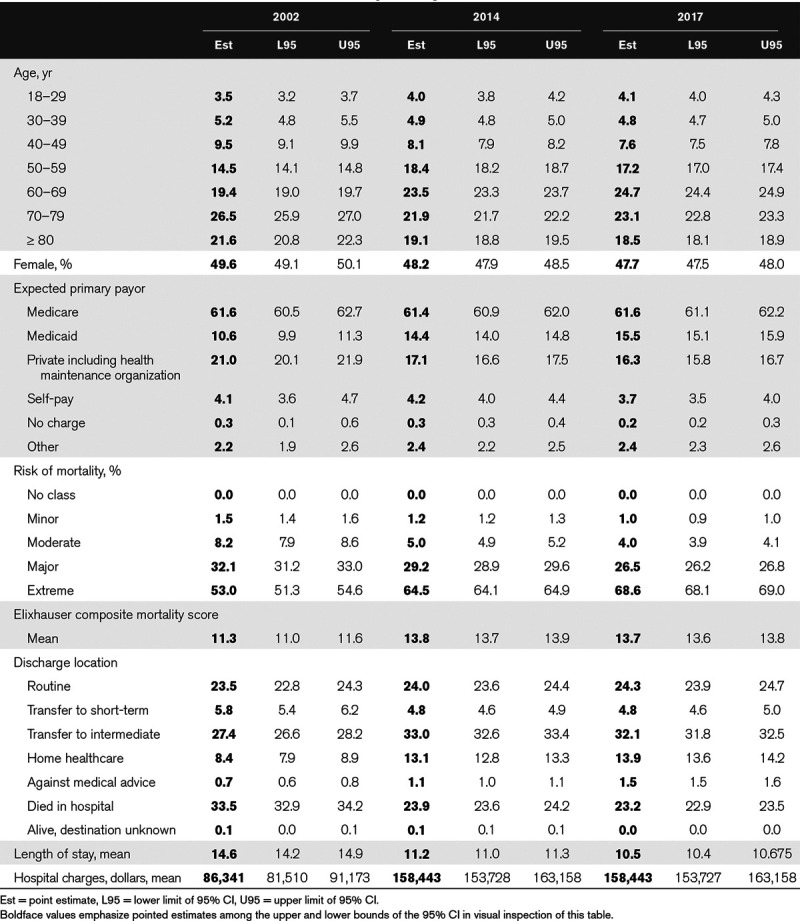
Regarding chronic medical comorbidities, the mean Elixhauser mortality score increased from 11 to 14 from 2002 to 2017 (Table 1). The chronic comorbidities that at least doubled in prevalence were deficiency anemias, rheumatoid arthritis, depression, complicated diabetes mellitus, drug abuse, hypertension, hypothyroidism, liver disease, obesity, and renal failure. The chronic comorbidities that did not increase in prevalence were HIV/AIDS, pulmonary circulation disorders, lymphoma, and metastatic cancer. The chronic comorbidities that decreased were blood loss anemia, uncomplicated diabetes mellitus, and solid tumors without metastases. Of note, complicated and uncomplicated diabetes mellitus, peptic ulcer disease, and pulmonary circulation disorders had greater than 25% changes from 2014 to 2016, when underlying ICD coding scheme changed. From 2002 to 2017, the proportion of patients categorized with an extreme risk of dying increased from 53% to 69%, while the proportion categorized with a major risk of dying decreased from 32% to 27%. There were also changes in the most frequent principal diagnosis categories among discharges with respiratory failure and mechanical ventilation (Table 10, Supplemental Digital Content 1, http://links.lww.com/CCX/A180). In 2002, the two most frequent principal diagnosis categories were respiratory failure and pneumonia accounting for 21% and 8%, respectively. In 2017, the two most common principal diagnosis categories were septicemia and respiratory failure at 25% and 17%, respectively.
Regarding the hospital outcomes of patients with respiratory failure and mechanical ventilation, while the hospital mortality decreased from 2002 to 2017 as mentioned above, the discharges dispositions of hospital survivors also changed. There were increases in the proportions of patients discharged to home healthcare (from 8% to 14%) and transfers to intermediate care facilities (from 27% to 32%). There was an accompanying decrease in the mean length of stay in the hospital from 15 to 11 days but an increase in the mean total charges for the hospital stay from $86,341 to $158,443.
DISCUSSION
In this report, we describe the national epidemiology of respiratory failure in the United States from 2002 to 2017, first exploring three composite definitions then a single composite definition in greater detail. Taken together, we distill several key findings. First, the use of diagnosis codes for respiratory failure increased significantly over the study period. Second, when comparing a composite case definition including all diagnosis codes for respiratory failure to case definitions of IMV and NIV, there has been a very large increase in the incidence of NIV (437%), a large increase in the incidence of diagnosis codes (197%), but no significant increase in the incidence of IMV. Finally, every composite case definition had a decrease in unadjusted hospital mortality.
This study is descriptive by design so any explanations of the observed trends are speculative. The disproportionate increase in diagnosis codes to procedural codes indicative of respiratory failure may be due to several reasons. This observation may arise from a true increase in incidence, an increase in recognition, an increase in code utilization, or a combination of these factors. More specifically, the disproportionate increases may have resulted from an increase in utilization of diagnosis codes as part of an “upcoding” phenomenon to optimize hospital billing and adjusted mortality metrics, decrease in utilization of IMV for respiratory failure in favor of noninvasive strategies, an increase in palliative approaches, or a combination of these factors. The findings regarding hospital mortality provide some further detail on this evolving pattern of administrative epidemiology. When utilizing a composite definition of diagnosis codes, there is a large decrease (57%) in hospital mortality over the study period resulting in a relatively low 2017 mortality of 12%, yet when including a requisite for a procedure codes for mechanical ventilation or only using procedure codes for IMV the declines are more modest (48% and 19%, respectively) and the resultant 2017 hospital mortality similarly higher (23% and 30%, respectively). This again may suggest that providers are increasingly applying diagnosis codes to less severe cases of respiratory failure cases, utilizing strategies to reduce IMV and improve outcomes, or utilizing more palliative care resulting in lower use of IMV and in-hospital mortality. However, the speculation that some of the improvements in mortality reflect improvements in care are supported by a more granular international study of mechanical ventilation (16).
After exploring various types of respiratory failure and composite case definitions, we chose a single composite definition of respiratory failure with mechanical ventilation to describe patient characteristics and outcomes in more detail. We chose this definition as it seems to capture a case definition that is conceptually most specific to patients that require mechanical ventilation for reasons of respiratory failure rather than for other reasons such as for an operation or procedure. With this focus in mind, we find that the population of patients with respiratory failure with mechanical ventilation has undergone several changes over time. As mentioned above, over the study period, the hospital mortality decreased from 34% to 23%. It is important to interpret this in the context of several of the changing patient characteristics over the study period: 1) there were decreases in the proportions of patients in age groups greater than or equal to 70 years old; 2) there were increases in proportions of patients with many classes of chronic comorbidities; 3) there was an increase in the proportion of patients in the highest risk category of severity of illness; and 4) there was an increase in the proportion (27% to 32%) of patients discharged to an intermediate care facility with a concomitant decrease in mean length of stay in the hospital. We speculate that these changes result from an increase in the use of palliative care for older individuals, and a combination of an increasingly sick and “multi-morbid” population with increases in the use of coding for comorbid conditions. Regarding the discharge disposition, in the NIS, the transfer to intermediate care disposition includes transfers to inpatient hospice, skilled nursing, inpatient rehabilitation, and long-term care facilities. Although the NIS does not have the granularity to elucidate all of the mechanisms of decreased hospital mortality, these observations leave open the possibility that this may be explained by increases in discharges to facilities such that mortality is not occurring in the hospital and captured in the NIS data. An alternative or perhaps coincident interpretation that is supported by more granular evidence is that hospital length of stay and mortality have improved despite increases in the severity of illness of patients due to improving critical care (16).
CONCLUSIONS
The growing population incidence of respiratory failure shows that this is a public health and health resource problem that will likely continue to outpace the rate of population growth. The coincident lower proportions of use of IMV in older populations and decreasing hospital mortality suggest that this is not just a symptom of an aging population but may be due to a population with increasing amounts of comorbid conditions, severity of illness, and acute event survivability to be able to be admitted for similar or recurrent conditions. In this regard, our health system needs continued attention to its capacity to address and allocate resources to this annually growing need over the long-term. Furthermore, more research is needed to understand the how seasonal and regional variations in the incidence of respiratory failure affect the short-term surge capacity for the limited resource of mechanical ventilation given known annual surges during the winter months in the northern hemisphere and current and future pandemics of respiratory viruses.
Footnotes
This work was primarily performed at Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine, Atlanta, GA.
Dr. Kempker received support from the Agency for Healthcare Quality and Research (K08HS025240) and has received consulting fees from Grifols. Dr. Martin received research support from the National Institutes of Health’s National Center for Advancing Translational Science (UL1 TR-002378) and the Marcus Foundation and has served as a consultant for Grifols. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Brummel NE, Balas MC, Morandi A, et al. Understanding and reducing disability in older adults following critical illness. Crit Care Med. 2015; 43:1265–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hashem MD, Nallagangula A, Nalamalapu S, et al. Patient outcomes after critical illness: A systematic review of qualitative studies following hospital discharge. Crit Care. 2016; 20:345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hopkins RO, Suchyta MR, Kamdar BB, et al. Instrumental activities of daily living after critical illness: A systematic review. Ann Am Thorac Soc. 2017; 14:1332–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bice T, Cox CE, Carson S. Cost and health care utilization in ARDS–different from other critical illness? Semin Respir Crit Care Med. 2013; 34:529–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stefan MS, Shieh MS, Pekow PS, et al. Epidemiology and outcomes of acute respiratory failure in the United States, 2001 to 2009: A national survey. J Hosp Med. 2013; 8:76–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walkey AJ, Wiener R. Use of noninvasive ventilation in patients with acute respiratory failure, 2000-2009: A population-based study. Ann Am Thorac Soc. 2013; 10:10–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wunsch H, Linde-Zwirble WT, Angus DC, et al. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010; 38:1947–1953 [DOI] [PubMed] [Google Scholar]
- 8.Healthcare Cost and Utilization Project. Introduction to the HCUP National Inpatient Sample (NIS) 2014.. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2014.jsp. Accessed January 16, 2020 2016
- 9.Healthcare Cost and Utilization Project (HCUP). Trend Weights for HCUP NIS Data. 2015. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp. Accessed January 16, 2020
- 10.U.S. Census Bureau Population Division. Table 1. Intercensal Estimates of the Resident Population by Sex and Age for the United States: April 1, 2000 to July 1, 2010. 2011. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed January 7, 2020
- 11.U.S. Census Bureau Population Division. Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2014. 2015. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed January 7, 2020
- 12.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-9-CM. 2017. Available at: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed January 16, 2020
- 13.Healthcare Cost and Utilization Project. Elixhauser Comorbidity Software, Version 3.7. 2017. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed January 16, 2020
- 14.Healthcare Cost and Utilization Project. Overview of Disease Severity Measures Disseminated With the Nationwide Inpatient Sample (NIS) and Kids’ Inpatient Database (KID). 2005. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/OverviewofSeveritySystems.pdf. Accessed January 16, 2020
- 15.SAS Institute Inc. The SURVEYMEANS Procedure. 2011. Available at: https://support.sas.com/documentation/cdl/en/statug/63962/HTML/default/viewer.htm#statug_surveymeans_sect011.htm. Accessed January 16, 2020
- 16.Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013; 188:220–230 [DOI] [PubMed] [Google Scholar]


