Abstract
Objectives:
Renal replacement therapy in coronavirus disease 2019 patients is complicated by increased activation of the coagulation system. This may worsen the quality of hemodialysis and contribute to a shortage of dialysis machines as well as plastic disposables during the pandemic. This study describes a simple and safe protocol of anticoagulation with low-molecular-weight heparin in combination with bedside sustained low-efficiency hemodialysis in coronavirus disease 2019 patients.
Design:
Monocentric observational cross-over trial investigating sustained low-efficiency hemodialysis with unfractionated heparin following sustained low-efficiency hemodialysis with low-molecular-weight heparin.
Setting:
Coronavirus disease 2019-ICU in a German Tertiary Care University Hospital.
Patients:
Three consecutive severe coronavirus disease 2019 patients receiving nine sustained low-efficiency hemodialysis therapies with unfractionated heparin followed by 18 sustained low-efficiency hemodialysis therapies with low-molecular-weight heparin.
Interventions:
Switch from IV unfractionated heparin to subcutaneous low-molecular-weight heparin enoxaparin in therapeutic doses for patients receiving bedside sustained low-efficiency hemodialysis.
Measurements and Main Results:
Nine renal replacement therapy sessions in patients anticoagulated with high doses of unfractionated heparin had to be discontinuated prematurely because of clotting of tubes or membrane and poor quality of hemodialysis. In the same patients, the switch to anticoagulation with therapeutic doses of the low-molecular-weight heparin enoxaparin allowed undisturbed bedside sustained low-efficiency hemodialysis for at least 12 hours. Quality of hemodialysis was excellent, no bleeding event was observed.
Conclusions:
Systemic anticoagulation with subcutaneous enoxaparin provides an effective and safe renal replacement procedure in critically ill patients with coronavirus disease 2019 and hypercoagulability. The protocol reduces the risk of filter clotting, blood loss, and poor dialysis quality and may also prevent systemic thromboembolism.
Keywords: acute kidney injury, anticoagulation, coronavirus disease 2019, enoxaparin, hemodialysis, heparin, renal replacement therapy
Acute kidney injury (AKI) and hypercoagulability causing thromboembolic events are frequent complications in coronavirus disease 2019 (COVID-19). During ICU treatment, 29%–50% of COVID-19 patients develop AKI, which contributes to increased mortality (1). In Europe, at least 46% of COVID-19 patients with Acute Respiratory Distress Syndrome require some form of renal replacement therapy (RRT) (2). It has become apparent that the increased demand could cause significant shortage of dialysis machines as well as supply with disposables like membranes (3). With more than 30%, the prevalence of thromboembolic complications in critical ill COVID-19 patients is remarkably high (4). Clotting of the hemodialysis filter and extracorporeal circuit in patients with COVID-19 has been observed frequently despite systemic anticoagulation with high doses of unfractionated heparin (UFH) or argatroban (a direct antagonist of factor II). Clotting not only limits treatment efficacy but also contributes to shortages of dialysers and plastic disposals during the coronavirus pandemic. The renal community has therefore prioritized anticoagulation in COVID-19 patients requiring RRT (5).
MATERIAL AND METHODS
The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All specific national laws have been observed. The local ethics committee approved the analysis and publication of the data (EK 10016/20, Chairman Prof. R. Korinthenberg). Data of three consecutive patients with failing RRT during anticoagulation with UFH have been collected and then patients were switched to therapeutic anticoagulation with enoxaparin. The low-molecular-weight heparin (LMWH) enoxaparin, in comparison to UFH, not only targets against coagulation factor IIa (prothrombin) but also against factor Xa. Activity against factor Xa is five times higher in relation to activity against factor IIa. The coagulation cascade is therefore inhibited at an earlier step by enoxaparin compared with UFH. Patients with AKI and need for RRT received 0.8 mg (80 IU)/kg bodyweight subcutaneous enoxaparin twice a day aiming for antifactor-Xa acitivty of 0.5–1.0 IU/mL (determined 4 h after subcutaneous injection by BIOPHEN Heparin LRT Assay) to achieve effective systemic anticoagulation. Patients were connected to the SLED Genius system (Fresenius Medical Care, Bad Homburg, Germany) using an 8-French double-lumen catheter. The Genius system is based on a single-pass batch setup and consists of a 75 L glass tank completely filled with ultrapure dialysate. During the treatment, fresh dialysate is taken from the top of the tank and is returned to the bottom after passing the dialyser (6, 7).
The extracorporeal system was primed with 1000 IU enoxaparin in the arterial tubing line. The dialyser used was FX60 (Fresenius Medical Care) containing a 1.4-m2 high-flux polysulfone “Helixone” membrane. Dialysate fluids were bicarbonate buffered. Blood flow was kept at 160 mL/min and ultrafiltration rate was adjusted in a range of 50–250 mL/h by the discretion of the treating physician.
RESULTS
Nine hemodialysis therapies (SLED with Genius system as well as continuous hemodialysis with Fresenius Multifitrate system) during anticoagulation with high doses of heparin had to be discontinued prematurely because of clotting and insufficient quality of dialysis. Using the LMWH enoxaparin in the same patients, we performed 18 consecutive uneventful bedside Genius hemodialysis therapies each for at least 12 hours. See Table 1 for demographics and Figure 1 for treatment details. The antifactor-Xa-activity was determined hourly and showed values within the target range in 98% of measurements. Importantly, no major bleeding event occurred. Hemodialysis quality in terms of potassium and creatinine clearance as well as fluid removal was excellent; the supine or prone position of patients on invasive ventilator therapy did not affect the outcome.
TABLE 1.
Demographic and Treatment Details of the Three Coronavirus Disease 2019 Patients Included in this Analysis
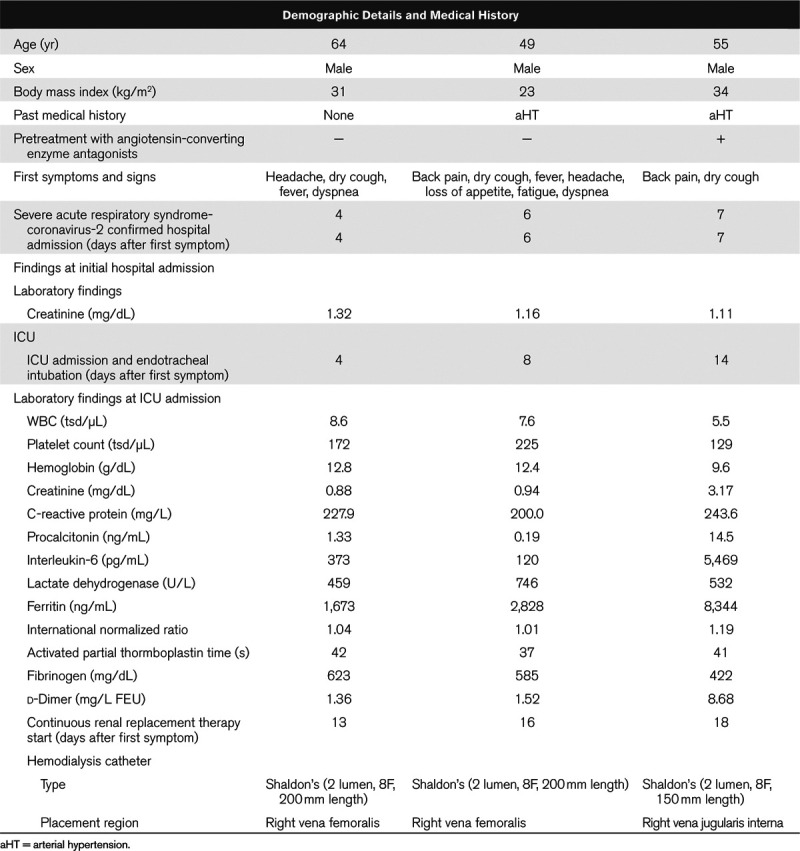
Figure 1.
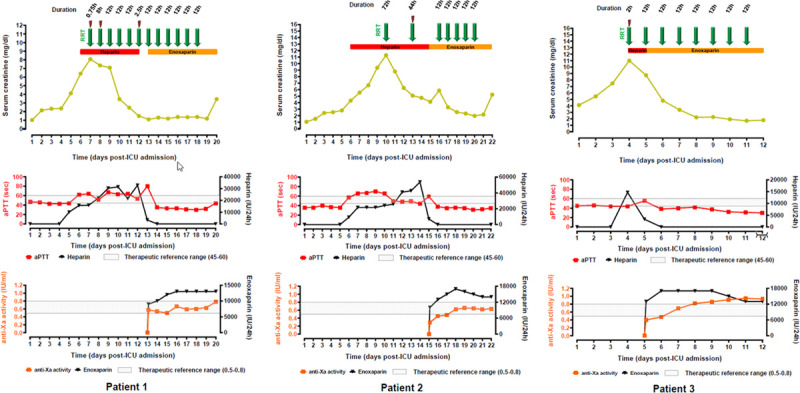
Time course of creatinine, activated partial thromboplastin time (aPTT), antifactor-Xa-activity, applied daily doses of heparin, and enoxaparin. Each green arrow indicates one episode of hemodialysis, duration of successful dialyses in hr; red flash-symbol indicates clotting of the hemodialyzer.
DISCUSSION
COVID-19 patients are at risk for AKI for several reasons. Dehydration due to prolonged fever predisposes patients to kidney injury. In patients with cytokine release syndrome (“cytokine storm”), high intrarenal inflammatory response contributes to hypoperfusion-related injury of the renal tubules. Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) has also been reported to invade renal tubular cells and podocytes (8).
COVID-19 may also be associated with hypercoagulability. Abnormal coagulation characterized by elevated levels in procoagulant factors (e.g., fibrinogen) and d-dimers is a predictor for disease severity and poor prognosis in patients with COVID-19. It is assumed that overwhelming systemic thrombin activation (“thrombin burst”) due to endothelial damage (9) is a major cause of hypercoagubality in COVID-19 patients. UFH and argatroban direct against the activation of thrombin. LMWH therefore inhibits the coagulation cascade at an earlier step and thus downregulates the conversion of prothrombin to thrombin. Recently published reports suggest that LMWHs decrease hypercoagulability and dampen the downstream thrombotic results of the marked inflammatory response associated with COVID-19 (10). These perceptions prompted us to switch our regimen of therapeutic anticoagulation to the LMWH enoxaparin in all COVID-19 patients with elevated d-dimer levels as marker of hypercoagulability.
Out of necessity, we combined therapeutic anticoagulation with enoxaparin and SLED in treatment of COVID-19 patients. The very high success rate was surprising and helped us to overcome potential shortages of dialysis machines and disposables.
This trial lacks from the partly retrospective design and the small amount of dialysis therapies included. During the COVID-19 pandemic, however, there was urgent need to find pragmatic solutions for the treatment of the first wave of patients flooding the ICUs in Europe. Rapid publishing may help other intensivists to take advantage of our experiences.
CONCLUSIONS
Systemic anticoagulation with subcutaneous enoxaparin in combination with the Genius system provides an effective and safe renal replacement procedure in critically ill patients with COVID-19 and hypercoagulability. This protocol reduces the risk of filter clotting, blood loss, and poor dialysis quality and may also prevent systemic thromboembolism. Furthermore, this approach may help to preserve resources during the coronavirus pandemic.
Footnotes
Drs. Neumann-Haefelin and Widmeier contributed equally in this work and both should be considered as first author.
Drs. Neumann-Haefelin, Widmeier, and Kalbhenn developed the idea and the protocol; Drs. Widmeier and Kalbhenn created the graphics; Drs. Kaufmann, Bansbach, and Heinrich treated the patients, supervised the therapy, and collected the data; Dr. Walz is the head of the renal division; Dr. Bürkle is the head of the Department of Anaesthesiology and Critical Care and both gave valuable inspiration and support; Dr. Kalbhenn wrote the raw manuscript, coordinated the project, and is the corresponding author. All authors had full access to the complete data provided and revised the manuscript. All agreed to the final version and gave their consent for publication.
The article processing charge was funded by the Baden-Wuerttemberg Ministry of Science, Research and Art and the University of Freiburg in the funding programme Open Access Publishing.
The study was performed at the Tertiary Care University hospital, Freiburg, Germany, and was financed by departmental resources.
Demographic and specific laboratory details of the patients were anonymously collected. Protocol-based ICU therapy is covered by the general contract governing medical treatment. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All specific national laws have been observed. The local ethics committee approved the analysis and publication of the data (EK 10016/20, Chairman Prof. R. Korinthenberg).
The legal representatives of all three patients gave their written informed consent for analysis and publication of data. The datasets are available from the corresponding author on reasonable request.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; 323:1775–1776 [DOI] [PubMed] [Google Scholar]
- 2.Intensive Care National Audit & Research Centre. ICNARC Report on COVID-19 in Critical Care. Available at: https://www.icnarc.org/About/Latest-News/2020/04/04/Report-On-2249-Patients-Critically-Ill-With-Covid-19. Accessed March 27, 2020
- 3.Mahase. .: Covid-19: Increasing demand for dialysis sparks fears of supply shortage. BMJ 2020; 369:m1588. [DOI] [PubMed] [Google Scholar]
- 4.Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research 2020; 191:145–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NHS–England. Clinical Guide for Acute Kidney Injury in Hospitalised Patients With COVID-19 Outside the Intensive Care Unit During the Coronavirus Pandemic. Available at: https://www.england.nhs.uk/coronavirus/secondary-care/other-resources/specialty-guides/. Accessed April 14, 2020
- 6.Frank RD, Müller U, Lanzmich R, et al. Anticoagulant-free Genius haemodialysis using low molecular weight heparin-coated circuits. Nephrol Dial Transplant 2006; 21:1013–1018 [DOI] [PubMed] [Google Scholar]
- 7.Eloot S, Van Biesen W, Dhondt A, et al. Evidence for internal filtration in the Genius system, performing slow low efficient daily dialysis in the intensive care unit. Blood Purif 2008; 26:460–467 [DOI] [PubMed] [Google Scholar]
- 8.Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020 Apr 9 doi: 10.1016/j.kint.2020.04.003. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varga Z, Flammer AJ, Steiger P, et al. Electron microscopy of SARS-CoV-2: A challenging task—Authors’ reply. Lancet 2020; 395:e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]


