Graphical abstract
Key Words: COVID-19, imaging, pandemic
In the pre-coronavirus-2019 (COVID-19) era, on any given day in the United States, thousands of patients required not only clinic visits but also a multitude of imaging and other diagnostic services for confirmatory diagnoses, assessments of their clinical courses, or planning of therapeutic interventions. During that time, cardiovascular imagers have had to balance their responsibilities among imaging laboratories, patient care, teaching house staff, and other clinical and administrative duties. This encapsulated cardiovascular imagers’ lives, and in the last few months, it all has changed! In unimaginable ways, our lives and those of all others have been disrupted due to the COVID-19 outbreak. Each of our respective cities represents “hot zones” for the virus. Our health systems have transformed into acute care hospitals, often overflowing beyond capacity and overwhelmed by the severity of illness and frequent specter of death. For some cities, like New York City and New Orleans, it seemed instantaneous that our centers were inundated with critically ill COVID-19 patients, nearly exhausting supplies of needed medical equipment and placing an enormous burden on all medical staff. While other cities, such as Boston and Detroit, had a delayed onset of the pandemic, which provided time for planning and execution of a response. In all, the COVID-19 outbreak dramatically impacted all of our medical centers.
As our hospitals have been dramatically repurposed to care for COVID-19 patients, our lives as cardiovascular imagers and researchers have been put “on pause,” causing considerable uncertainty about the future of our specialty. Will we regain the imaging volumes that largely included elective procedures? Given the astronomical financial losses faced by our health systems, will our careers face major hurdles in turn affecting our lives? These are but a few of the stressors that we continue to face in these challenging times.
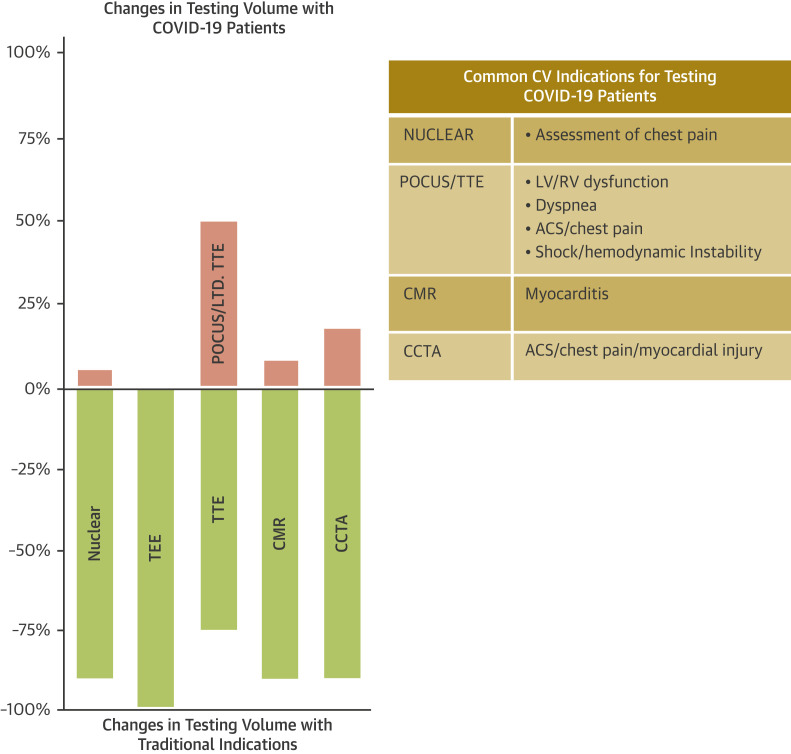
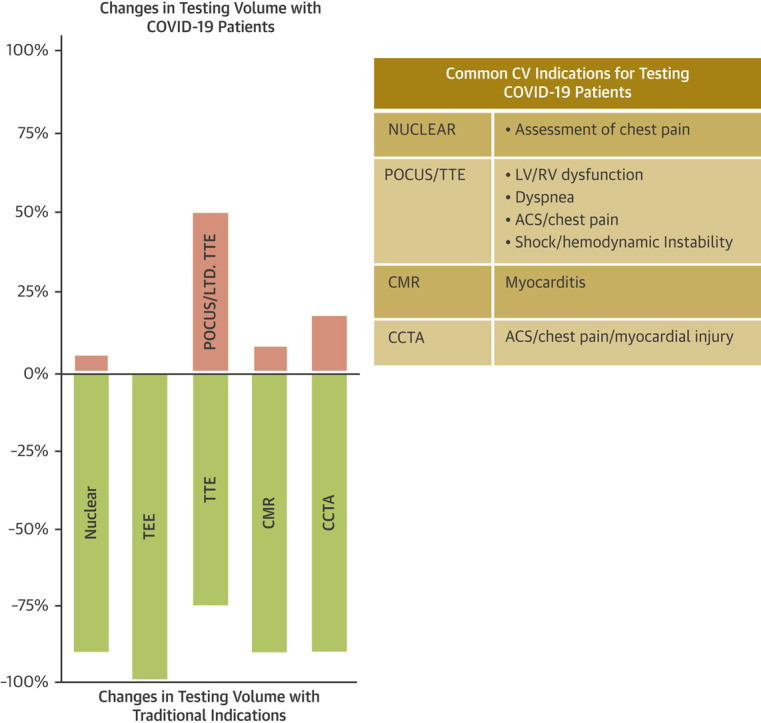
Across our hospitals, nearly all elective procedures, including a large volume of patients with planned stress tests, were deferred, and most were rescheduled into June or later (Figure 1 ). Throughout the pandemic, the loss of our normal activities as clinicians created a vacuum and heightened the anxiety regarding the future of medicine. For researchers, all activities outside of critical care investigation are on hold, leaving concerns regarding the tremendous loss in investigative momentum, the timely completion of projects, and the potential cancellations of funded research activities. Grant timelines and time-sensitive research costs place further effects on the stress of researchers.
Figure 1.
Changes in Testing Volume From Conventional Utilization to Testing of COVID-19 Patients
These data are based on an aggregate response from all participating health care systems. ACS = acute coronary syndrome; CCTA = coronary computed tomographic angiography; CMR = cardiac magnetic resonance; POCUS/LTD = point of care ultrasound/limited; RV/LV = right ventricular/left ventricular; TEE = transesophageal echocardiography; TTE = transthoracic echocardiography.
In some cases, the rapid transformation of hospitals required imagers to promptly pivot to new and often foreign services to aid in the care of COVID-19 patients. Some imagers have been deployed outside of cardiology into various clinical duties including workforce health services, fever clinics, intensive care units, and medical wards caring for patients infected with COVID-19. In this “all hands on deck” approach, we all came together to provide patient care that we learned largely during medical school. Some institutions preferred to redeploy only clinicians with more recent training in general internal medicine, whereas other health systems retrained physicians, with some imagers finding themselves in the throes of an overwhelmed emergency department or intensive care unit. Often, physicians were required to rapidly learn the standards of care for COVID-19 patients, with its many evolving therapeutic approaches and without a deepened understanding of this or other viruses, as is the case for cardiovascular care. This further added to the everyday stress of “leaving” cardiology to serve a role for which we were not formally trained. At the same time, we are in awe of all our colleagues (including nurses, respiratory therapists, and many others) who have risen to this challenge to take care of each person, providing the best care during this unprecedented time.
Some cardiology care was provided in a limited direct manner but largely through telehealth services; albeit not all patients have this capability. Not being able to review vital signs, listen to a murmur, or examine an electrocardiogram puts constraints on what a cardiovascular specialist can do remotely. It is challenging to gauge a patient’s level of symptom instability or clinical worsening through remote interaction, often staccato in course, and without our usual tools available in the outpatient clinic. These interactions often left us feeling that many questions were unanswered and with residual concern about the patient’s state and need for intensified cardiovascular care, which we were unprepared to provide.
At its onset, COVID-19 was deemed primarily a respiratory disease, but we rapidly recognized multiorgan involvement with distinct and devastating cardiovascular manifestations. For the sickest patients, acute cardiac decompensation was observed, whereas others had elevated troponin levels, raising concern for an initial diagnosis of acute myocardial infarction. Many cardiovascular imagers struggled to find solutions as to what if any imaging modality would yield informative findings across the diverse cardiovascular differential including causes of arrhythmia, ischemia, thromboembolism, or heart failure. A smattering of procedures were done, including stress testing to assess chest pain, cardiac magnetic resonance to assess myocarditis, and coronary computed tomographic angiography in the patient with acute myocardial infarction or convalescent chest pain (Figure 1). However, the most common indication for imaging a COVID-19 patient was the use of a focused (not comprehensive) echocardiogram for assessment of biventricular (global and regional) function, chest pain, or dyspnea. Across institutions, the use of imaging varied widely and largely depending on expertise. The lack of uniformity in practices left sizeable gaps in our knowledge about pathophysiology and further questions about the appropriateness of imaging in the COVID setting. In many cases, we devised our own evaluation algorithms with the imaging societal guidelines helpful but often published after our own institutions cared for hundreds if not thousands of COVID-19 patients. In many instances, we learned novel imaging approaches and clinical insights, shared with others on social media and other online interactive platforms.
The necessity for imaging the COVID-19 patient prompted major concerns regarding safety and potential exposure to all laboratory staff and clinicians. This is especially so for imaging procedures such as transesophageal echocardiography, with a high potential for aerosolization of the virus. For this and other procedures (such as exercise testing) came appropriate concern over staff exposure and transmission of the virus. This apprehension was exacerbated given the shortages of personal protective equipment initially unavailable for staff in imaging laboratories.
Safety concerns were even more worrisome with bedside echocardiography, given the proximity of the sonographer to a patient. As such, we spent considerable time developing novel imaging protocols to shorten imaging time, limiting staff exposure to infectious patients, and providing rapid sterilization of imaging equipment and facilities. Although this may seem simple, no level of detail could be overlooked, including air circulation times in the imaging laboratories or at the patient’s bedside. There always seemed to be some level of detail initially overlooked that became critical to create an optimal safe environment for all health care workers.
Safety concern also extended to our imaging trainees, who found themselves in the trenches practicing ventilator management and critical care. Many of them, both dedicated imaging and senior cardiology fellows, who allocated much of this year to acquiring critical imaging skills necessary for their professional growth, are in danger of not achieving the usual milestones necessary for completing their fellowships, although relaxation of training criteria is being considered by the Accreditation Council for Graduate Medical Education. Many trainees from outside the United States were asked to promptly return to their home countries, often at the request of their governments, with likely numerous challenges to returning. The interruption in their training and disruption in their specialty goals further adds to the emotional burden related to the outbreak.
As we now strategize about reopening, our attention is increasingly shifted toward a safe reintroduction of cardiovascular services. Such planning involves multiple levels of complexities and unknown factors regarding the optimal approach for universal or selected COVID-19 screening of candidates for cardiovascular imaging. Ideally, all of this information would be known before the patient arrives to our imaging facility. Questions arise as to whether reconfiguring waiting rooms and other measures of physical distancing or universal masking will be enough; and can we maintain an adequate supply of personal protective equipment as we start to perform procedures with a moderate risk of viral aerosolization, such as exercise testing? We also now approach the use of cardiovascular imaging differently and often consider its necessity or how much testing is really needed to care for a patient. Thus, issues of appropriateness combined with streamlined, focused protocols are very much at the forefront of our strategies for reopening. Reservations persist about the use of certain procedures, such as transesophageal echocardiography, with high risk of exposure for medical staff and consideration of replacement procedures with an improved safety profile (e.g., cardiac computed tomography versus transesophageal echocardiography for the evaluation of endocarditis). A final challenge is communicating all this information to our colleagues and patients, assuring them that we are working diligently to reopen our imaging laboratories with a primary focus on safety for all patients and staff.
What has happened over the past few months is unimaginable, and its emotional toll on our lives has yet to be fully realized. There are so many ways that these challenges have added stress to our day, for example, anxiety related to the potential shortages of personal protective equipment, concern over cutbacks or potential furloughs, salary reductions, redeployment to new areas in medicine, and the shutting down of our research laboratories. Although this is a personal account of the impact on the COVID-19 pandemic on cardiovascular imagers, our current environment is saturated with an emotional toll on the medical staff, families, public health officials, and the general community, especially the fear within vulnerable communities at high risk for the virus. The COVID-19 infection hit our hospitals at a time when cardiovascular services, particularly imaging, were dealt harsh cuts in reimbursement. In many ways, the devastation caused by the COVID-19 pandemic has further compounded a very challenging imaging environment leaving even more instability regarding its future.
Yet, in the midst of all of this, we impatiently await for all of this to pass and look ahead to the post-COVID-19 storm. We must remind ourselves that many cardiology patients left unattended will require more intense care for critical aortic stenosis, heart failure, and chronic coronary disease. We also do not yet realize the long-term impact of COVID-19 on the cardiovascular system. Millions of patients have had their imaging procedures and directed care interrupted. How will we care for the millions of patients who had cardiovascular care deferred remains unknown, but we are eager to put as many pieces of our lives back together as is possible. It is impossible to tell what the new normal will look like, but one thing is clear, ahead is a long road of learning, adapting, and collaborating as we inch beyond the flattening curve.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose. James Udelson, MD, served as Guest Editor for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Cardiovascular Imagingauthor instructions page.