Abstract
Objective
The use of standing electronic scooters associated with micromobility applications (e‐scooters) has risen nationally. The aim of this study was to obtain a detailed view of soft tissue and bony craniofacial injury associated with e‐scooter‐related trauma.
Methods
Single‐institution retrospective case series of patients presenting to a level 1 trauma center emergency department or trauma unit with documented e‐scooter‐related craniofacial injury.
Results
Of 203 included patients, 188 (92.6%) patients sustained craniofacial injury. One hundred thirty‐one (64.5%) had exclusively soft tissue injury, 3 (1.5%) exclusively bony injury, 51 (25.1%) both soft and bony injuries, and twenty‐five (12.3%) patients sustained dental injury. Aesthetic units most frequently sustaining acute soft tissue injury were the forehead (n = 106, 34.6%), scalp (n = 36, 11.8%), chin (n = 34, 11.1%), upper lip (n = 32, 10.5%), and cheek (n = 31, 10.1%). Aesthetic subunits most often sustaining acute soft tissue injury included the brow (42, 13.7%), central forehead (39, 12.7%), lateral forehead (n = 25, 8.2%), and upper lip vermillion (n = 23, 7.5%). Craniofacial osseous fracture most often occurred in the orbit (n = 42, 24.6%) and maxilla (n = 40, 23.4%). Individual osseous segments most frequently sustaining acute fracture included the anterior maxillary sinus wall (n = 22, 12.9%), nasal bone (n = 20, 11.7%), lateral orbital wall (n = 16, 9.4%), orbital floor (n = 15, 8.8%), and zygomatic bone (13, 7.6%).
Conclusions
Our analysis demonstrates that most patients presenting to our center with craniofacial trauma sustained acute bony fracture, most often to the midface. Our data of common injuries associated with e‐scooter trauma could inform implementation in the form of facial safety equipment or safety skills training for e‐scooter riders.
Level of evidence
4
Keywords: craniofacial, electric, face, head, scooter, trauma
1. INTRODUCTION
Standing electronic scooters associated with micromobility smartphone applications (e‐scooters) were initially introduced in September 2017 in Santa Monica, California. 1 , 2 Over the subsequent years, multiple companies have joined the micromobility trend, resulting in the rapid expansion of e‐scooter availability and use. 3 By 2018, 38.5 million e‐scooter rides had been recorded on 85 000 e‐scooters in approximately 100 US cities. Southern Californian cities represented some of the densest areas of e‐scooter use, including San Diego which contains thousands of e‐scooters. 4
Concurrent with the growth in e‐scooter use, injuries related to their use have also increased. A dramatic rise in emergency department visits related to e‐scooter use has been observed nationally. Analysis of the National Electronic Injury Surveillance System from 2014 to 2018 demonstrated a 222% increase in age‐adjusted e‐scooter injury incidence and a 365% increase in age‐adjusted hospital admission, with the steepest rises occurring from 2017 to 2018. 5 Multiple case series in the United States have described total body injuries associated with e‐scooter‐related trauma, which can range in severity from mild contusion, abrasion, and laceration to severe injury necessitating intensive care or resulting in death. These studies found craniofacial soft tissue or bony injury to occur in 26% to 58% of patients presenting with e‐scooter‐related trauma. 6 , 7 , 8 , 9 However, the specific patterns of craniofacial injury secondary to e‐scooter‐related trauma remain incompletely characterized.
Given the rise in micromobility devices, e‐scooters represent an emerging mode of trauma with poorly understood patterns of craniofacial injury that will likely exert additional burdens on the health care system. The high proportion of craniofacial trauma in e‐scooter trauma patients necessitates a more detailed characterization of the bony and soft tissue injuries sustained in these patients. Such insights are likely to improve implementation of safety measures and the expedited evaluation and treatment for this growing trauma patient population.
2. METHODS
We performed a retrospective case series of all patients presenting with e‐scooter‐related injuries from April 2018 to September 2019 to the University of California San Diego (UCSD) Medical Center Emergency or Level 1 Trauma Departments. Patients were identified by query of the UCSD electronic medical record for encounters including terms related to face and/or head trauma and the term “scooter.” A database with predetermined variables was then populated via data abstraction from patient records by two independent reviewers. Exclusion criteria included nonmotorized scooter use, trauma from use of scooter as a weapon, and death prior to evaluation.
In addition to basic demographic information, data pertaining to soft tissue and bony injury were collected. Soft tissue injury information was determined from physical exam findings at presentation. The soft tissue injury was localized to the facial aesthetic subunit, and categorized into contusions, abrasions, lacerations, avulsions, burns, or injuries limited to tenderness to palpation. Bony injury information was gathered from the radiologist report of computed tomography studies. Dental injuries were recorded if dental fracture or avulsion was documented. Baseline characteristics were analyzed using descriptive statistics. Bony and soft tissue facial injuries were categorized into quintiles and projected onto skull or face illustrations in heat map formats using Adobe Photoshop. Each soft tissue or bony injury was considered as an individual injury and the total number of each respective injury category was considered the sum of individual injuries. Injuries without adequate information documented to specify facial or bony aesthetic subunit were excluded from the heat map projections.
3. RESULTS
In total, 206 patients presented with e‐scooter‐related injuries. Three patients were excluded due to nonmotorized scooter use, use of scooter as a weapon, and death prior to medical evaluation. Of the remaining 203 patients, the median age at injury was 36 years (interquartile range [IQR]: 27‐50). Seven (3.4%) patients were under 18 years old. Most patients were male (58.6%), of White race (60.6%), non‐Hispanic ethnicity (86.2%), and lived in San Diego county (50.2%). One hundred thirty‐nine (68.5%) patients presented by ambulance. The great majority of patients were driving the e‐scooter (99.0%). Many patients were intoxicated at the time of accident (54.2%), with substances including alcohol (93, 45.8%), methamphetamines (9, 4.4%), cannabis (15, 7.4%), and opioids (7, 3.4%; Table 1).
TABLE 1.
Baseline characteristics
| Variable | n | Percent | |
|---|---|---|---|
| Age, years | Median (IQR) | 36 (27‐50) | |
| Sex | Male | 119 | 58.6 |
| Female | 84 | 41.4 | |
| Race | White | 123 | 60.6 |
| Black | 9 | 4.4 | |
| Other | 55 | 27.1 | |
| Native Hawaiian or Pacific Islander | 2 | 1.0 | |
| Asian | 10 | 4.9 | |
| Unknown | 4 | 2.0 | |
| Ethnicity | Hispanic | 28 | 13.8 |
| Non‐Hispanic | 175 | 86.2 | |
| City of residence | San Diego | 76 | 37.4 |
| Other | 127 | 62.6 | |
| State of residence | California | 139 | 68.5 |
| Not California | 64 | 31.5 | |
| Tourism/visitor status | Yes (vacation or business) | 101 | 49.8 |
| No (in town) | 102 | 50.2 | |
| Required emergency medical service involvement | Yes | 129 | 63.5 |
| No | 74 | 36.5 | |
| Scooter driver | Yes | 201 | 99.0 |
| No | 2 | 1.0 | |
| Intoxicated a | Yes | 110 | 54.2 |
| No | 93 | 45.8 | |
| Alcohol use at time of injury | Yes | 93 | 45.8 |
| No | 110 | 54.2 |
Abbreviation: IQR, interquartile range.
Intoxicated status was indicated if medical record contained documentation that the patient appeared intoxicated based on the examining clinician's impression.
One hundred eighty‐eight (92.6%) patients presented with craniofacial injury, further categorized as follows: 131 (64.5%) were documented to sustain exclusively soft tissue injury, 3 (1.5%) exclusively bony injury, and 51 (25.1%) both soft and bony injuries. Twenty‐five (12.3%) patients sustained dental injury. Patients with soft tissue injury presented most often with lacerations (n = 121, 59.6%), abrasions (n = 98, 48.3%), or contusions (n = 75, 36.9%). Patients rarely presented with avulsion injury (8, 2.6%) or sole tenderness to palpation without visible evidence of tissue injury (7, 2.3%). Median laceration length was 2 cm (IQR: 1.5‐3.0, range: 0.1‐10).
Facial soft tissue injuries categorized by aesthetic subunit are presented in Figure 1 and Table 2. In total, 306 discrete facial soft tissue injuries were documented. The aesthetic unit that most frequently sustained acute soft tissue injury was the forehead (n = 106, 34.6%). The scalp (n = 36, 11.8%), chin (n = 34, 11.1%), upper lip (n = 32, 10.5%), and cheek (n = 31, 10.1%) were the next most frequently injured units and showed similar rates of soft tissue injury (Figure 1A). The aesthetic unit demonstrating a distinctly lower rate of soft tissue injury was the ear (n = 1, 0.3%).
FIGURE 1.
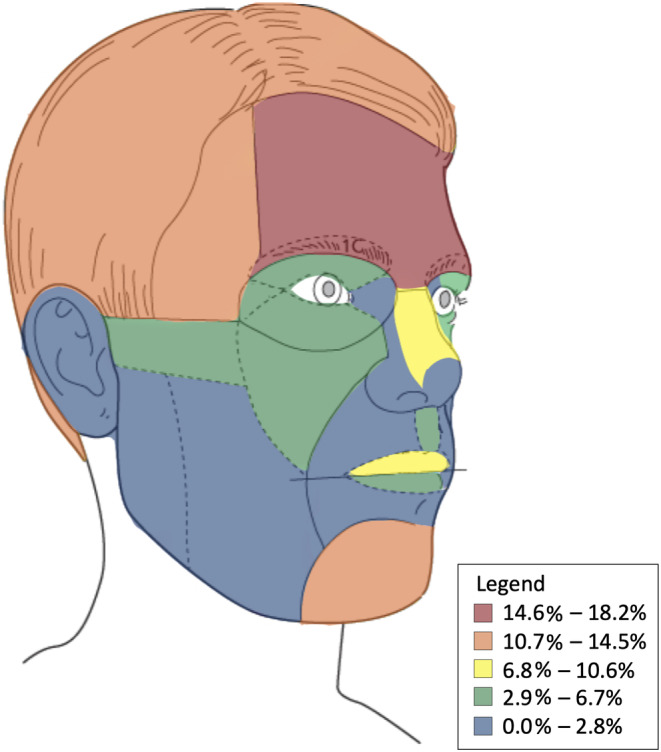
Facial soft tissue injury categorized by aesthetic subunit
TABLE 2.
Soft tissue injuries
| Aesthetic unit | Aesthetic subunit | Any soft tissue injury | Percent a |
|---|---|---|---|
| 1. Forehead | A. Central | 39 | 12.7 |
| B. Lateral | 25 | 8.2 | |
| C. Brow | 42 | 13.7 | |
| 2. Nose | A. Dorsum | 18 | 5.9 |
| B. Lateral wall | 0 | 0.0 | |
| C. Ala | 1 | 0.3 | |
| D. Tip | 0 | 0.0 | |
| E. Columella | 0 | 0.0 | |
| X. NOS b | 6 | 2.0 | |
| 3. Eyelid | A. Superior | 6 | 2.0 |
| B. Inferior | 4 | 1.3 | |
| C. Lateral canthus | 4 | 1.3 | |
| D. Medial canthus | 0 | 0.0 | |
| X. NOS b | 11 | 3.6 | |
| 4. Cheek | A. Infraorbital | 7 | 2.3 |
| B. Zygomatic | 3 | 1.0 | |
| C. Buccal | 1 | 0.3 | |
| D. Parotid‐masseteric | 0 | 0.0 | |
| X. NOS b | 20 | 6.5 | |
| 5. Upper lip | A. Philtrum | 7 | 2.3 |
| B. Lateral | 2 | 0.7 | |
| C. Vermillion | 23 | 7.5 | |
| 6. Lower lip | A. Central | 0 | 0.0 |
| B. Vermillion | 14 | 4.6 | |
| 7. Chin | 34 | 11.1 | |
| 8. Ear | A. Helix | 0 | 0.0 |
| B. Antihelix | 0 | 0.0 | |
| C. Concha | 1 | 0.3 | |
| D. Lobule | 0 | 0.0 | |
| E. Retroauricle | 0 | 0.0 | |
| X. NOS b | 1 | 0.3 | |
| 9. Scalp | 36 | 11.8 | |
| 10. Unspecified | 1 | 0.3 | |
| Total | 306 | 100.0 |
Percent of all soft tissue injuries.
NOS—not otherwise specified. Documentation did not contain adequate information to classify injury to specific aesthetic subgroup. These injuries were excluded from the soft tissue injuries heat map analysis displayed in Figure 1.
Higher resolution analysis was then performed with aesthetic subunits. Some aesthetic units, which in some cases lacked adequate information in the medical record to allow for further classification into subunits, were denoted as not otherwise specified (NOS): Cheek (nNOS = 20, 6.5% of all soft tissue injuries), eyelid (nNOS = 11, 3.6%), nose (nNOS = 6, 2.0%), ear (nNOS = 1, 0.3%) represented. These unclassifiable soft tissue injuries were thus excluded from the facial soft tissue subunit heatmap analysis. The aesthetic subunits most frequently sustaining acute soft tissue injury included the brow (42, 13.7%), central forehead (39, 12.7%), lateral forehead (n = 25, 8.2%), and upper lip vermillion (n = 23, 7.5%; Figure 1B).
Bony injuries are presented in Figure 2 and Table 3. In total, 171 discrete acute craniofacial osseous fractures were documented. The structures most often fractured included the orbit (n = 42, 24.6%) and maxilla (n = 40, 23.4%), each of which comprised nearly one quarter of all discrete bony fractures. The parietal (n = 3, 1.8%) and occipital (2, 1.2%) bones represented the least frequently fractured bones of the head. The individual osseous segments that most frequently sustained acute fracture included the anterior maxillary sinus wall (n = 22, 12.9%), nasal bone (n = 20, 11.7%), lateral orbital wall (n = 16, 9.4%), orbital floor (8.8%), and zygomatic bone (13, 7.6%). The osseous segments least frequently fractured included the petrous temporal bone (n = 1, 0.6%), mandibular subcondyle (n = 1, 0.6%), mandibular condyle (n = 2, 1.2%), posterior maxillary wall (n = 2, 1.2%), and mastoid temporal bone (n = 2, 1.2%).
FIGURE 2.
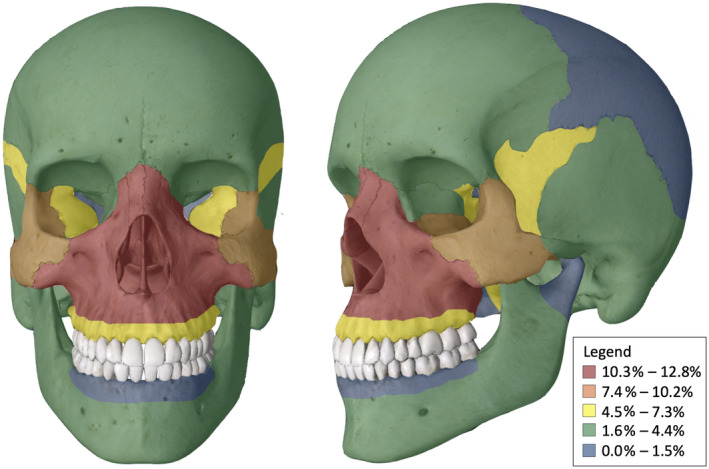
Bony craniofacial injury
TABLE 3.
Bony injuries
| Site | Subsite | n | Percent a |
|---|---|---|---|
| Frontal sinus | Anterior table | 5 | 2.9 |
| Posterior table | 5 | 2.9 | |
| Parietal bone | 3 | 1.8 | |
| Occipital bone | 2 | 1.2 | |
| Temporal | Mastoid | 2 | 1.2 |
| Petrous | 1 | 0.6 | |
| Squamous | 4 | 2.3 | |
| Zygomatic bone | 13 | 7.6 | |
| Maxillary bone | Anterior maxillary wall | 22 | 12.9 |
| Posterior maxillary wall | 2 | 1.2 | |
| Maxillary sinus, NOS b | 7 | 4.1 | |
| Maxillary alveolar ridge | 9 | 5.3 | |
| Nasal bone | 20 | 11.7 | |
| Orbit | Floor | 15 | 8.8 |
| Medial wall | 5 | 2.9 | |
| Lateral wall | 16 | 9.4 | |
| Roof | 6 | 3.5 | |
| Mandible | Condyle | 2 | 1.2 |
| Subcondyle | 1 | 0.6 | |
| Ramus | 4 | 2.3 | |
| Body | 3 | 1.8 | |
| Symphysis/parasymphysis | 5 | 2.9 | |
| Mandibular alveolar ridge | 3 | 1.8 | |
| Sphenoid bone | 9 | 5.3 | |
| Other facial bone fractures | 7 | 4.1 | |
| Total | 171 | 100.0 |
Percent of all bony injuries.
NOS—not otherwise specified. Documentation did not contain adequate information to classify injury to specific aesthetic subgroup. These injuries were excluded from the osseous injury heat map analysis displayed in Figure 2.
Of the 188 patients presenting with craniofacial injury, 13 patients (6.9%) presented with intracranial injury encompassing epidural, subdural, subarachnoid, and intraparenchymal hemorrhage. Of the 9 patients with sphenoid fractures, 3 (33%) sustained intracranial injury, and one of these patients developed cerebrospinal fluid leak. The remaining 10 intracranial injuries occurred in 4 patients with temporal bone fractures (2 squamous, 1 mastoid, and 1 petrous), 1 patient with zygomaticomaxillary complex fracture, and 5 patients without craniofacial osseous injury.
4. DISCUSSION
As e‐scooter use continues to increase, the literature has begun to examine the health care consequences related to this mode of transportation. This report presents a detailed view of the craniofacial soft tissue and bony injury sustained in e‐scooter‐related trauma. Our findings indicate that e‐scooter‐related craniofacial trauma occurs in a broad segment of the young adult to middle aged population, who are the most likely to ride e‐scooters. And our findings recapitulate existing findings in the literature that a large portion of those who present with e‐scooter‐related trauma are intoxicated.
Consistent with previous reports, facial lacerations were present in over half of patients. 7 Along with the high incidence of extremity injuries reported in the literature, our data corroborate the intuitive notion that many craniofacial injuries result from riders attempting to break their forward fall. 6 , 7 , 10 In comparison to seated vehicles, the scooter rider maintains a relatively high center of gravity predisposing the rider toward impacts of the face and hands when falling. Several studies have cited the head and face as the frequently affected anatomical regions in e‐scooter accidents, occurring in 20% to 58% of presenting patients. 6 , 7 , 8 , 11 , 12 , 13 Previous work has quantified the incidence of facial involvement in e‐scooter injuries. Trivedi et al focused specifically on craniofacial injuries following e‐scooter accidents, outlining the categorical severity (severe vs minor) as well as location of injury (upper, middle, or lower face). 7 Bresler et al reported type of facial injury (eg, closed head, laceration, or fracture). 13 However, no study to our knowledge has characterized the nature of e‐scooter‐related craniofacial injury.
The current study builds on these works to provide a more detailed picture of the craniofacial anatomy involved in e‐scooter‐related trauma. We elected to implement the facial aesthetic unit classification for localizing soft tissue trauma because it is a standardized method on which reconstructive technique is founded. 14 To achieve similar technical accuracy, bony injuries were classified based on the involved craniofacial bone(s). Our findings reflect the reality that craniofacial trauma is rarely confined to specific aesthetic units or bony segments by demonstrating that injuries often involved multiple contiguous aesthetic subunits and/or bony segments.
E‐scooter‐related soft tissue injury manifested most often in the form of lacerations and abrasions, injuries that are likely to leave lasting aesthetic defects on the face even if they are addressed in a timely and technically appropriate manner.
In our study, the forehead was the most common soft tissue region of the face injured. In regards to facial bone injury, the midface was the most common injured site. More broadly, soft tissue injury most often involved the forehead, scalp, and chin. The relatively high rate of soft tissue injury to the chin combined with paucity of lower face bony injury suggest that the lower face sustains lower‐energy e‐scooter‐related trauma. This notion also applies to the upper face, with the forehead demonstrating a high rate of soft tissue injury but the frontal bones showing relatively few e‐scooter‐related fractures. Conversely, bony injury most often involved the nasal bone, anterior maxillary sinus, lateral orbital wall, and zygoma, indicating that the midface is the most frequent region of bony injury involved in e‐scooter‐related craniofacial trauma.
In looking at the demographics, over 60% of the patients who had facial injuries from e‐scooters did not live in San Diego. Thus, either these out of town visitors were riding e‐scooters at disproportionately higher rates than the local residents or they may be less adept to control the e‐scooter and therefore more susceptible to craniofacial trauma. It remains unknown whether first‐time riders were the most vulnerable to facial injuries.
As research increasingly demonstrates the risks associated with e‐scooter use, the medical community can begin to identify preventable measures and advocate for improved safety surrounding these devices. Our review revealed over half of riders were intoxicated with either alcohol, or under the influence of tetrahydrocannabinol, methamphetamine, or diacetylmorphine [heroin]. These findings are corroborated by other studies and represent a dangerous and avoidable increase in risk to riders when operating e‐scooters. Our findings also confirm a small percentage of riders (3.4%) were under the age of 18 as seen in previous studies, demonstrating another potentially avoidable risk. Further investigation may underscore the importance of basic precautions when riding e‐scooters such as abstinence from substance use, being of the legal age (18) to ride an e‐scooter, and wearing a helmet when riding. While micromobility companies and local and state governments implement measures to improve e‐scooter safety, existing data suggest that riders often do not comply to company or governmental regulations regarding age limitations, protective equipment use, or intoxicated riding. 6 , 7 , 8 Moreover, given the high rate of significant craniofacial injury, our study indicates that scooter riders may benefit from facial protective helmets.
This retrospective study is subject to limitations associated with the reported data including the underreporting and nonspecific reporting of clinical findings. For example, it is likely that not every simple abrasion was recorded or specified by facial aesthetic subunit, especially in the setting of more severe injury. This may explain the few cases of patients who had bony injury without soft tissue injury. Intoxication data is also incomplete, as substance use may not have been documented by provider or reported accurately by patient. In addition, blood alcohol levels or urine toxicology screens were ordered in a subset of patients, therefore this retrospective review often relied on the documented clinical impression of the examining physician.
5. CONCLUSION
While e‐scooters represent a convenient and accessible mode of transportation, they are associated with a disproportionately high burden of craniofacial trauma, especially fractures of the midface. Our data of common injuries associated with e‐scooter trauma could inform implementation in the form of facial safety equipment or safety skills training for e‐scooter riders.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Faraji F, Lee JH, Faraji F, et al. Electric scooter craniofacial trauma. Laryngoscope Investigative Otolaryngology. 2020;5:390–395. 10.1002/lio2.380
Farhoud Faraji and Jason H. Lee contributed equally to this study.
REFERENCES
- 1. Bird Rides Inc . Santa Monica Mobility Pilot Program; 2018.
- 2. Hall M. Bird Scooters Flying Around. Santa Monica: CA, Santa Monica Daily Press; 2018. [Google Scholar]
- 3. Dickey MR. The Electric Scooter Wars of 2018. Bay Area: California, Techcrunch; 2018. [Google Scholar]
- 4.Shared Micromobility in the U.S.: 2018; 2019. https://nacto.org/shared-micromobility-2018/
- 5. Namiri NK, Lui H, Tangney T, Allen IE, Cohen AJ, Breyer BN. Electric scooter injuries and hospital admissions in the United States, 2014‐2018. JAMA Surg. 2020. https://jamanetwork.com/journals/jamasurgery/fullarticle/2758159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trivedi TK, Liu C, ALM A, et al. Injuries associated with standing electric scooter use. JAMA Netw Open. 2019;2:e187381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Trivedi B, Kesterke MJ, Bhattacharjee R, Weber W, Mynar K, Reddy LV. Craniofacial injuries seen with the introduction of bicycle‐share electric scooters in an urban setting. J Oral Maxillofac Surg. 2019;77:2292‐2297. [DOI] [PubMed] [Google Scholar]
- 8. Kobayashi LM, Williams E, Brown CV, et al. The e‐merging e‐pidemic of e‐scooters. Trauma Surg Acute Care Open. 2019;4:e000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. DiMaggio CJ, Bukur M, Wall SP, Frangos SG, Wen AY. Injuries associated with electric‐powered bikes and scooters: analysis of US consumer product data. Inj Prev. 2019. https://doi: 10.1136/injuryprev‐2019‐043418 [DOI] [PubMed] [Google Scholar]
- 10. Mayhew LJ, Bergin C. Impact of e‐scooter injuries on emergency department imaging. J Med Imaging Radiat Oncol. 2019;63:461‐466. [DOI] [PubMed] [Google Scholar]
- 11. Badeau A, Carman C, Newman M, Steenblik J, Carlson M, Madsen T. Emergency department visits for electric scooter‐related injuries after introduction of an urban rental program. Am J Emerg Med. 2019;37:1531‐1533. [DOI] [PubMed] [Google Scholar]
- 12. Bekhit MNZ, Le Fevre J, Bergin CJ. Regional healthcare costs and burden of injury associated with electric scooters. Injury. 2020; 51:271‐277. [DOI] [PubMed] [Google Scholar]
- 13. Bresler AY, Hanba C, Svider P, Carron MA, Hsueh WD, Paskhover B. Craniofacial injuries related to motorized scooter use: a rising epidemic. Am J Otolaryngol. 2019;40:662‐666. [DOI] [PubMed] [Google Scholar]
- 14. Gonzalez‐Ulloa M. Restoration of the face covering by means of selected skin in regional aesthetic units. Br J Plast Surg. 1956;9:212‐221. [DOI] [PubMed] [Google Scholar]


