When we entered cardiology training, we never expected to think of our own safety before initiating chest compressions on a pulseless patient. Yet, the novel coronavirus disease 2019 (COVID-19) pandemic has raised new questions, including issues of clinician safety during cardiopulmonary resuscitation (CPR).
CPR and endotracheal intubation are aerosol-generating procedures. According to the Centers for Disease Control and Prevention, aerosolizing procedures should be performed with personal protective equipment (PPE) consisting of eye protection, N95 respirators, gloves, and gowns in airborne infection isolation rooms given the higher risk of viral transmission.1 In New York City, the need for intensive care unit capacity has surpassed the number of negative-pressure rooms. Most intubated patients are placed in non–negative-pressure rooms where CPR should, in theory, be avoided given the risks of dislodgement of the endotracheal tube and aerosolization of secretions. Furthermore, there are already dramatic PPE shortages. These resource constraints challenge our ability to comply with Centers for Disease Control and Prevention recommendations. Because of the complex realities of resuscitation in the COVID-19 era, we encourage a national conversation on the following 4 points.
First, how can we better identify patients who would not want CPR? As clinicians, one of our priorities has been, and continues to be, to provide patients with care aligned with their values and preferences in the event that they become critically ill. Advanced care planning is more imperative now than ever, particularly among older adults with chronic, life-limiting illnesses who are at higher risk for severe infection. Ideally, these conversations should occur before patients become infected and present to the hospital. Primary care clinicians or specialists who have longitudinal relationships with patients can address advanced care planning during outpatient visits scheduled for other reasons or during dedicated telemedicine visits.2 In addition, patients and families can be directed to online resources to guide these conversations and to facilitate completion of physician order for life-sustaining treatments forms.2 At the time of hospital admission, all patients should have conversations with their clinicians about goals of care and preferences for resuscitation, regardless of their COVID-19 status; however, these conversations should be prioritized in older patients with multiple comorbidities who test positive. Some institutions have also created palliative care telehealth services to assist frontline clinicians with reaching out to family members beginning in the emergency room. These services can dedicate time to having these important family discussions via phone or video conference because most hospitals now restrict inpatient visitation. Whenever feasible, primary team members should also partake in these conversations and revisit goals of care as a patient’s clinical status changes.
Second, when CPR is performed, it should be done as safely as possible. This means that all healthcare providers must don full PPE (including N95s) before entering the room even if it delays resuscitation efforts. Moreover, all patients at hospitals in regions with a high prevalence of COVID-19 should be assumed to have COVID-19 at the time of cardiac arrest, and providers should use appropriate PPE. Because full PPE may not be routinely available outside of dedicated COVID-19 units, hospitals should consider adding PPE to code carts and equipping all code blue team members with full PPE at the start of their shifts. In addition, the number of providers involved in a resuscitation effort should be limited to reduce total exposure and PPE use. Several additional strategies have been suggested to mitigate the risk associated with CPR (Figure). For example, some have suggested increasing the use of external mechanical chest compression devices to reduce the risk to personnel when available. Others have suggested that plastic sheets be placed between the patient and the provider performing chest compressions to minimize aerosolization. In patients who are not already intubated, a high-efficiency particulate air filter may be considered during bag-mask ventilation. When an invasive airway is secured, endotracheal intubation should be performed by the provider with the most experience with airway management using video-laryngoscopy to minimize the number of attempts and the risk of transmission.3
Figure.
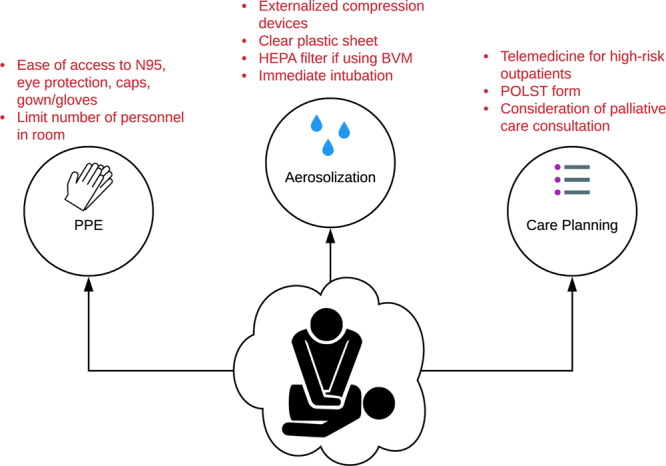
Challenges in and potential solutions for the administration of cardiopulmonary resuscitation (CPR) during the coronavirus disease 2019 (COVID-19) pandemic. BVM indicates bag-valve mask ventilation; HEPA, high-efficiency particulate air; POLST, physician order for life-sustaining treatments; and PPE, personal protective equipment.
Third, more data are needed to clarify which patients with COVID-19 are least likely to benefit from CPR. Epidemiological data suggest that risk factors for mortality include older age, higher Sequential Organ Failure Assessment score, and elevated D-dimer.4 Other markers of poor prognosis include severe lymphopenia, elevated troponin, elevated creatinine, and high inflammatory markers. However, information on survivability of in-hospital cardiac arrest is lacking. Having studies that quantify CPR outcomes in these patients and identify which groups (if any) are more likely to survive to hospital discharge is critical.
Finally, guidance from professional societies and biomedical ethicists about how and when to perform CPR is needed. Some extreme views on this topic have already emerged, including calls for a universal do-not-resuscitate policy for patients infected with COVID-19.5 Although such a radical approach may violate our Hippocratic instincts, a business-as-usual approach is probably not appropriate either. As the COVID-19 pandemic has evolved, some medical societies and institutions have started the conversation about finding a middle ground. For example, the Belgian Society of Emergency and Disaster Medicine and Belgian Resuscitation Council joint statement suggests that CPR be avoided when provider safety cannot be guaranteed or there is low likelihood of a good functional outcome. Although blanket statements by professional societies may not capture the nuances of these scenarios, they underscore the very real risk posed to healthcare providers during CPR without adequate protection. Drawing lines in either direction is fraught with logistical and ethical angst, but for this precise reason, professional standards are needed so that frontline providers are not making these decisions alone.
As trainees, so much of our learning is focused on doing: instinctively taking someone with ST-segment elevations to the cardiac catheterization laboratory or starting chest compressions when there is no pulse. But knowing when not to do something is often much harder. Particularly as our patients are fighting and dying in hospitals isolated from their loved ones, we must balance efforts to preserve their lives with the importance of bringing dignity to their deaths while doing our best to stay safe in the process.
Disclosures
None.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html. Accessed March 27, 2020.
- 2.Curtis JR, Kross EK, Stapleton RD. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19) [published online March 27, 2020]. JAMA. doi: 10.1001/jama.2020.4894. doi:10.1001/jama.2020.4894. [DOI] [PubMed] [Google Scholar]
- 3.Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fann E, Oczkowski S, Levy MM, Derde L, Dzierba A, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) [published online March 27, 2020]. Crit Care Med. doi: 10.1097/CCM.0000000000004363. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cha AE. The Washington Post; 2020. Mar 25, Hospitals consider universal do-not-resuscitate orders for coronavirus patients. https://www.washingtonpost.com/health/2020/03/25/coronavirus-patients-do-not-resucitate/. Accessed April 3, 2020. [Google Scholar]


