Abstract
Providing flavored milk in school lunches is controversial, with conflicting evidence on its impact on nutritional intake versus added sugar consumption and excess weight gain. Nonindustry-sponsored studies using individual-level analyses are needed. Therefore, we conducted this mixed-methods study of flavored milk removal at a rural primary school between May and June 2012. We measured beverage selection/consumption pre- and post-chocolate milk removal and collected observation field notes. We used linear and logistic mixed models to assess beverage waste and identified themes in staff and student reactions. Our analysis of data from 315 unique students and 1,820 beverages choices indicated that average added sugar intake decreased by 2.8 g postremoval, while average reductions in calcium and protein consumption were negligible (12.2 mg and 0.3 g, respectively). Five thematic findings emerged, including concerns expressed by adult staff about student rebellion following removal, which did not come to fruition. Removing flavored milk from school-provided lunches may lower students’ daily added sugar consumption without considerably decreasing calcium and protein intake and may promote healthy weight.
Keywords: participatory research, elementary school, rural, flavored milk, school lunch, school nursing
Over the past two decades, medical and public health officials have recognized obesity and overweight in childhood as a public health crisis that contributes to an individual’s present and future health issues (Barlow, 2007; Ebbeling, Pawlak, & Ludwig, 2002; Institute of Medicine, 2012). In 2011–2012, 16.9% of children aged 2–19 in the United States were considered obese (Ogden, Carroll, Kit, & Flegal, 2014), and significant disparities in prevalence exist for children of lower socioeconomic status, non-White race/ethnicity, and geographic region (Singh, Kogan, Van Dyck, & Siahpush, 2008; Singh, Siahpush, & Kogan, 2010; Y. Wang & Beydoun, 2007). For example, children from rural areas may experience obesity rates more than 5% above the national average (A. M. Davis, Bennett, Befort, & Nollen, 2011). Dietary behaviors are among the key modifiable risk factors recommended to prevent childhood and adult obesity (Khan et al., 2009; Waters et al., 2011). Consumption of added sugar and sugar-sweetened beverages has been a particular focus of recent efforts (Gortmaker, Long, & Wang, 2009; Hu, 2013; Malik, Pan, Willett, & Hu, 2013; Miller et al., 2013; Te Morenga, Mallard, & Mann, 2013; Y. C. Wang, Bleich, & Gortmaker, 2008).
Changing school-provided meal options is one approach for promoting optimal dietary intake in children (Guinn, Baxter, Royer, & Hitchcock, 2013; Let’s Move!; U.S. Department of Agriculture, 2017; Vilsack, 2012). Flavored milk, with a sugar and calorie content nearly twice that of low-fat white milk, has been a target of such school-based interventions (Golub, Charlop, Groisman-Perelstein, Rud-dock, & Calman, 2011; Goto, Waite, Wolff, Chan, & Giovanni, 2013). However, because flavored milk may also be a means of supporting students’ calcium and mineral intake, removal from school lunches has been contested by local parents and health professionals (Cliff, 2011; Hanks, Just, & Wansink, 2014; Matheny, 2013; Nicklas, O’Neil, & Fulgoni, 2013; Quann & Adams, 2013).
Research on the associations between student consumption of flavored milk and other sugar-sweetened beverages on nutrition and weight gain is inconsistent (Briefel, Wilson, Cabili, & Hedley Dodd, 2013; Kaiser, Shikany, Keating, & Allison, 2013). Results from these studies are often suspect due to the use of problematic exposure measures (Archer, Hand, & Blair, 2013; Bucher Della Torre, Keller, Laure Depeyre, & Kruseman, 2015) such as dietary recall, which may not accurately represent children’s consumption patterns (Skinner, Steiner, & Perrin, 2012) and/or between group study designs. Additionally, industry sponsorship has raised concerns about study results (Bes-Rastrollo, Schulze, Ruiz-Canela, & Martinez-Gonzalez, 2013; Lesser, Ebbeling, Goozner, Wypij, & Ludwig, 2007); for example, many studies which show null findings or overall positive nutritional effects of flavored milk consumption are supported by or have ties to the dairy industry (Frary, Johnson, & Wang, 2004; Hanks et al., 2014; Johnson, Frary, & Wang, 2002; Murphy, Douglass, Johnson, & Spence, 2008; Nicklas et al., 2013; Quann & Adams, 2013). Thus, the research does not provide adequate evidence to guide school district policies on flavored milk provision during school lunches.
In 2011, a heated debate over the availability of flavored milk in school lunches emerged between parents in a rural central Oregon county (Cliff, 2011, 2012; Matheny, 2013). In a county where 81% of students were eligible for the free or reduced lunch program and obesity rates were higher than the state average (Winett, Gauntner, Becker, & Mladenovic, 2015), school nutrition represented an important opportunity for primary and secondary prevention by local health stakeholders. Some parents felt that flavored milk was a primary source of nutrients for the students (i.e., calcium and protein); while others felt the harms of the added sugar (and the potential weigh gain) outweighed these potential benefits. Given the need for research to inform this discussion, an emerging academic–community partnership leveraged this opportunity to conduct a mixed-methods community-based participatory research (CBPR) study to address the following aims: (1) measure the effect of removing the option of flavored milk on the consumption of water and unflavored milk among young, school children and (2) assess student and staff reactions to the elimination of flavored milk.
Method
For this study, we employed a concurrent, embedded mixed-methods design (Creswell, Klassen, Plano Clark, & Smith, 2011; Creswell & Plano Clark, 2011). We use quantitative data from our beverage waste study to evaluate change in student beverage consumption and qualitative data to characterize adult staff and student reactions before, during, and following the removal of chocolate milk from school lunch. This study was approved by the Oregon Health & Science University Institutional Review Board (IRB#8484).
Setting and Participants
The Milk Options Observation (MOO) Project emerged as part of a larger National Institute of Health-funded study to train and empower rural community stakeholders as partners in research (M. M. Davis et al., 2014; Young-Lorion et al., 2013). Described in detail elsewhere, the overarching study focused on transforming four regional community health improvement partnerships (CHIPs) into community health improvement and Research partnerships (CHIRPs) using a three-step intervention: (a) participating in an academic– community kickoff/orientation meeting, (b) engaging in eight brief research training modules, and (c) working with academic partners to develop and implement a CBPR study focused on childhood obesity (a community-identified health need; M. M. Davis et al., 2014). The present study, MOO, was conducted by one of the CHIP to CHIRP partners, the Mountain View CHIRP, in response to local needs.
MOO occurred at Madras Primary School (MPS), one of seven schools in the Jefferson County School District-509J in Oregon and the only school in the region serving kindergarten through second-grade students. CHIRP members had close ties with MPS (J.S. was the district nurse) and a history of conducting school-based studies to address local needs (Hunsberger, McGinnis, Smith, Beamer, & O’Malley, 2015; Hunsberger et al., 2014; McGinnis et al., 2010). The 509J district is comprised of 34% Latino, 34% American Indian/ Alaska Native, and 29% Caucasian students (Oregon Department of Education, 2014–2015a), and 76.6% of students at MPS qualify for free or reduced school lunch (Oregon Department of Education, 2014–2015b). Body mass index surveillance data collected during fall 2011, the same school year that this study was conducted, found that 23% of kindergarteners at the school were overweight and 27% were obese.
Procedures
Participant recruitment.
CHIRP members and academic partners obtained permission to conduct a beverage waste study and participant observations during lunch from the district superintendent, school principal, district food service manager, and district nurse. All MPS students (kindergarten through second grade) attending school during cafeteria observation days were eligible for the study; this included students eating school provided meals and meals brought from home. Three weeks prior to data collection, all parents were sent a letter that described the study and were provided an opportunity to excuse their students from the procedures. We received no opt out requests in response to the notification. For participant data to be included in the final sample, we required students to have at least one school-provided beverage measurement in each observation period.
Beverage options.
At the time of the study, MPS provided students with a choice between a flavored milk option (1% chocolate), 1% white milk, and nonfat white milk at lunch. Water was available in a fountain mounted on a wall in the cafeteria just outside the lunch line. However, in response to recommendations from school authorities, our study team paid for the school to reintroduce bottled water (8 ounce bottles) as a menu option at lunch 1 week prior to data collection and throughout the study period. Bottled water in this format at lunch was familiar to the students.1 Introduction prior to the study period facilitated further normalization of bottled water as an option, alleviated staff fears that students would “drink nothing” following chocolate milk removal, and it enabled the study team to quantify beverage selection and consumption in a standardized fashion for all available school-provided beverage options. Per school policies, students were allowed to take more than one type of beverage during a lunch period at no additional cost(i.e., milk and water) and they could pay to take a second beverage (i.e., two milks).
Data collection.
Data collection occurred over a 4-week period between May 7, 2012, and June 1, 2012, and included beverage waste measurements and participant observation (Bogdewic, 1999; Mack, Woodson, Macqueen, Guest, & Namey, 2005). School lunch time procedures remained generally unchanged during the study period. Academic- and community-based study team members conducted both beverages waste measurements and observations during six lunch sessions—prior to chocolate milk removal (n = 3) and during removal (n = 3). Beverage waste measurement and participant observations occurred on 3 days 1 week prior to chocolate milk removal (i.e., May 7, 10, and 11). Chocolate milk was removed starting May 14, and beverage waste measurements and participant observations were conducted weekly for the next 3 weeks (i.e., May 17, 24, and 31). Participant observation also occurred during lunch on June 1 when MPS reintroduced chocolate milk.
For beverage waste measurements, study team members applied coded numerical identifiers on all student beverage containers (including those brought from home and those available through the school) at the start of lunch and collected containers at the end of lunch. This enabled tracking beverage consumption for individual students. Beverage consumption was measured using standard beakers by two research team members to ensure accuracy. We recorded “no measurement amount” for measurements that equaled the quantity of the full container or when a container was unopened (i.e., no beverage had been consumed). For participant observations, one or two study team members were assigned to observe student and staff behaviors and to ask open-ended clarifying questions about beverage choices and views toward beverage removal. Team members took brief jottings during observations and turned them into rich, detailed field notes within 24 hours.
Data Analysis
Quantitative.
We recorded a total of 1,874 school-provided beverage choices from 360 unique students over the 6 days of observation. We excluded 45 students from the sample (12.5%) who did not have at least one school-provided beverage in each observation period due to school absences or because they exclusively brought drinks from home. We excluded data from 186 beverages brought from home (9% overall, 9% in preremoval, and 8% in postremoval period) due to heterogeneity in beverage type, size, and nutrient content. As displayed in Figure 1, our final analytic sample was 315 students and 1,820 beverage choices.
Figure 1.
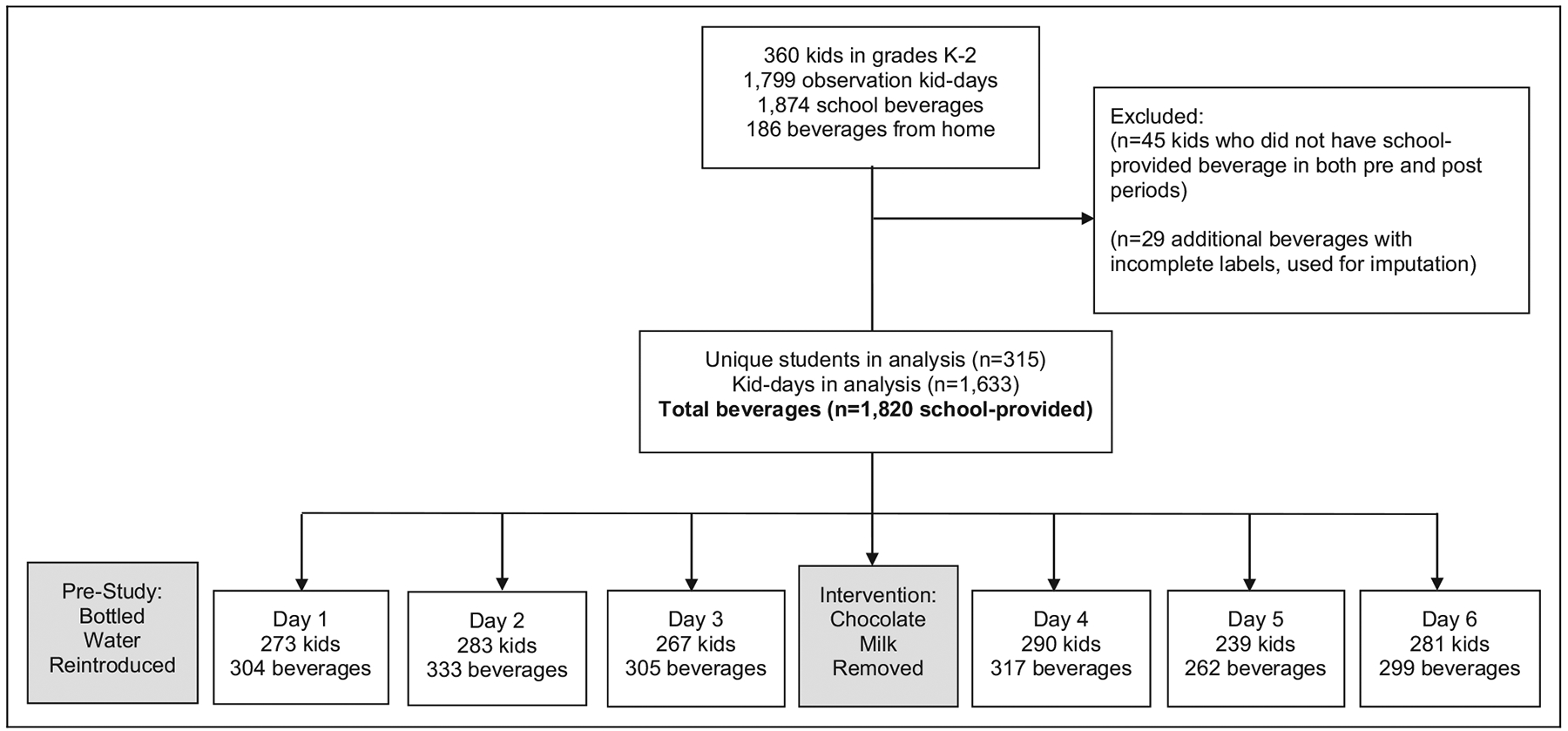
Participant enrollment information.
We classified the remaining beverages as chocolate milk, 1% milk, skim milk, or water; for some analyses, we combined 1% and skim milk into a single “white milk” category. In nine records where the observer indicated that a student took a beverage but did not record the amount consumed, we imputed the mean amount for that type of drink for that student’s grade level on the same day. We used the nutrition fact labels of the school-provided milk cartons to calculate nutrient and sugar consumption. For nutrient consumption, we assumed 300 mg of calcium and 8 g of protein per 8 ounces of milk, scaled to the actual amount consumed. For added sugar, we assumed 12 g per 8 ounces of chocolate milk or the difference in total sugars between chocolate and 1% milk.
To examine whether students drank more of certain types of beverages, we used two closely related models with beverage as the unit of analysis. First, we modeled the proportion of beverages chosen that had any measurable amount consumed (i.e., the difference between starting volume and ending volume was greater than 0) and then we limited our analytic data to consumed beverages and modeled the liquid ounces consumed. We included type of beverage and the number of drinks chosen (one versus two or three) as independent variables; taking three beverages only occurred 3 times. Because grade level was closely related to both race/ethnicity and age in our sample, we kept only grade level and gender in the final model as the potential confounders of greatest interest. For both models, we used population-averaged generalized linear models with generalized estimating equations to account for correlation between repeated observations on the same student. To model proportions, we used a log link and binomial distribution to estimate relative risk (RR) directly. Predictive margins estimated the mean proportions and mean ounces consumed for the two models, respectively.
In a second model, we estimated the change from pre- to postperiods in average ounces and nutrients consumed per lunch period, as well as ounces wasted, by students who drank chocolate milk and those who did not. We classified students as chocolate milk drinkers if they chose chocolate milk at least once, regardless of the amount consumed; otherwise, we classified them as chocolate abstainers. If a student took more than one beverage in a lunch period, the outcomes—mean ounces consumed or wasted, added sugar, protein, and calcium—were summed into a single record for the day. As independent variables, we included indicators for chocolate milk drinkers and pre-/postperiod along with their interaction, after we had checked for daily differences within pre-/postperiod by beverage type and found very little variation. We included gender, race/ethnicity, and grade level as potential confounders. Linear mixed models allowed us to include a random intercept for each student and random slope for pre-/postperiod, with exchangeable covariance. Although the outcome distributions were skewed, Lumley, Diehr, Emerson, and Chen (2002) have demonstrated that untransformed linear models in data sets of this size yield unbiased estimates of the mean, and we used robust (empirical) variance estimators to compensate for using the normal distribution.
From the same models, we estimated the differences between the changes, pre to post, among chocolate milk drinkers and abstainers, or “difference in differences” (Meyer, 1995). Many unmeasured influences could affect all students’ beverage consumption during lunch—a shortened lunch period, a change in weather—while only chocolate milk drinkers would be affected by removing chocolate milk. The differences in differences reflect the effect of removing chocolate milk above and beyond day-to-day variability. All statistical analyses were performed using SAS (version 9.4 for Windows) and Stata (version 14) software.
Qualitative.
We transferred observational field notes into to Atlas.ti (version 7) for data management and analysis. The multidisciplinary team (with expertise in school nursing, applied social psychology, qualitative research, community health development, and childhood obesity) used focused coding and grounded theory methods to analyze qualitative data (Miles & Huberman, 1994; Strauss & Corbin, 1990). Using an iterative process, three authors independently coded field notes (M.M.D., S.A., and J.S.); then met to discuss codes, identify emergent themes, and resolve discrepancies through consensus (Crabtree & Miller, 1999). Two authors (B.A.B. and P.M.) helped refine the emerging themes during an analysis retreat. The authors then presented the themes to the larger CHIRP group as a form of member checking and used the group’s feedback to produce the report of final themes and illustrative quotes. These methods (multiple reviewers, reflexivity, audit trail, and member checking) are associated with rigor in qualitative research (D. J. Cohen & Crabtree, 2008, n.d.; Malterud, 2001; Patton, 1999).
Results
Demographic characteristics for the 315 unique students included in the analysis appear in Table 1. Of these students, 79% (n = 249) chose chocolate milk at least once preintervention (aka “chocolate milk drinkers”). As detailed in Table 1, compared to chocolate milk drinkers, chocolate milk abstainers, those who never selected chocolate milk preremoval, were more likely to be female (p .043), Hispanic (p =.024), or in first grade (p < .001).
Table 1.
Participant Characteristics and Beverage Selection Habits of Chocolate Milk Drinkers (Chose Chocolate Milk at Least Once Prior to Removal) and Chocolate Abstainers.
| Total Sample (n = 315) n (%) |
Chocolate Milk Drinkers (n = 249) n (%) |
Chocolate abstainers (n = 66) n (%) |
p Value | |
|---|---|---|---|---|
| Gender | ||||
| Female | 156 (49.5) | 116 (46.6) | 40 (60.6) | .043 |
| Male | 159 (50.5) | 133 (53.4) | 26 (39.4) | |
| Race/ethnicity | ||||
| Non-Hispanic white | 109 (34.6) | 95 (38.2) | 14 (21.2) | .024 |
| Hispanic | 166 (52.7) | 122 (49.0) | 44 (66.7) | |
| Non-Hispanic other | 40 (12.7) | 32 (12.9) | 8 (12.1) | |
| Grade | ||||
| K | 112 (35.6) | 89 (35.7) | 23 (34.8) | <.001 |
| 1 | 104 (33.0) | 70 (28.1) | 34 (51.5) | |
| 2 | 99 (31.4) | 90 (36.1) | 9 (13.6) | |
| Observation days in school and drinking school-provided beverage (six possible) | ||||
| 6 | 116 (36.8) | 96 (38.6) | 20 (30.3) | .104 |
| 5 | 121 (38.4) | 99 (39.8) | 22 (33.3) | |
| 4 | 55 (17.5) | 39 (15.7) | 16 (24.2) | |
| 3 | 14 (4.4) | 9 (3.6) | 5 (7.6) | |
| 2 | 9 (2.9) | 6 (2.4) | 3 (4.5) | |
| Maximum drinks selected in a given lunch break | ||||
| 1 | 195 (61.9) | 144 (57.8) | 51 (77.3) | .003 |
| 2a | 120 (38.1) | 105 (42.2) | 15 (22.7) | |
| Beverage selections before removal (n = 942 beverage choices) | ||||
| Chocolate milk | 541 (57.4) | 541 (69.5) | — | <.001a |
| Water | 350 (37.2) | 218 (28.0) | 132 (80.5) | |
| White milk | 51 (5.4) | 19 (2.4) | 32 (19.5) | |
| Beverage selections after removal (n = 878 beverage choices) | ||||
| Water | 500 (56.9) | 366 (52.1) | 134 (76.6) | <.001 |
| White milk | 378 (43.1) | 337 (47.9) | 41 (23.4) | |
Exact test used rather than χ2.
Beverage Selection
Prior to removal, chocolate milk was the most common beverage selected (57.4%), while bottled water was most common (56.9%) after removal (see Table 1). White milk selection increased from 5.4% preremoval to 43.1% post-removal. Nearly 40% of students (38.1%, n = 120) took more than one beverage; significantly more chocolate milk drinkers than chocolate abstainers did so (42.2% versus 22.7%, p = .003). Chocolate milk drinkers’ beverage selection patterns were consistent from day to day within the pre- and postintervention observation periods (e.g., no significant differences in water consumption during preintervention study period). Chocolate milk abstainers’ beverage selection patterns were consistent across the full study period.
Beverage Consumption
Of the 1,820 school-provided beverages chosen by the students, a measurable amount was not consumed in 21% (n = 383). As displayed in Table 2, water was most often consumed when chosen (0.84 selected had some amount consumed), followed by white milk (0.80) and chocolate milk (0.71). On average, students drank 2.1 ounces more water and 1.1 ounces more white milk than chocolate milk (p < .001). Compared to students who took only one beverage, students who selected two to three beverages during a lunch period were more likely to drink any of it (RR 1.12, p < .001) and to drink 0.7 ounces more when they did (p < .001). There were significant differences in the average amount of beverage consumed by grade level; kindergarten students drank the most (5.4 ounces) and students in first grade drank the least (4.7 ounces).
Table 2.
Differences in Probability of Drinking a Chosen Beverage and Average Volume Consumed, by Type of Beverage and Student Characteristics (N = 315 students and 1,820 beverages)
| Beverage Chosen | Beverage Consumed | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Category | N chosen | Proportion with a measurable amount consumeda | RR | 95% Cl | P value | N consumedb | Mean (ounces) |
Difference (ounces) |
95% Cl | P value |
| Overall | 1,820 | 0.79 | 1,437 | 5.1 | ||||||
| Beverage type | ||||||||||
| Chocolate milk | 541 | 0.71 | [reference] | 385 | 3.8 | [reference] | ||||
| White milk | 429 | 0.80 | 1.12 | (1.04, 1.20) | 0.002 | 335 | 4.9 | + 1.1 | (0.8, 1.5) | <0.001 |
| Water | 850 | 0.84 | 1.18 | (1.10, 1.27) | <0.001 | 717 | 5.9 | +2.1 | (1.8, 2.5) | <0.001 |
| Number of beverages per lunch period | ||||||||||
| 1 only | 1,345 | 0.77 | [reference] | 1,041 | 4.9 | [reference] | ||||
| 2–3 | 475 | 0.86 | 1.12 | (1.07, 1.17) | <0.001 | 396 | 5.6 | +0.7 | (0.4, 0.9) | <0.001 |
| Grade level | ||||||||||
| Kindergarten | 690 | 0.82 | [reference] | 563 | 5.4 | [reference] | ||||
| Grade 1 | 514 | 0.79 | 0.97 | (0.90, 1.04) | 0.444 | 411 | 4.7 | −0.7 | (−1.1,−0.3) | <0.001 |
| Grade 2 | 616 | 0.76 | 0.92 | (0.86, 1.00) | 0.053 | 463 | 4.9 | −0.5 | (−0.8, −0.1) | 0.005 |
| Gender | ||||||||||
| Male | 949 | 0.77 | [reference] | 720 | 5.0 | [reference] | ||||
| Female | 871 | 0.81 | 1.06 | (1.00, 1,12) | 0.063 | 717 | 5.1 | +0.1 | (−0.2, 0.4) | 0.404 |
Note. RR = relative risk; CI = confidence interval
Predictive margins from population-averaged generalized linear model; probabilities and relative risk estimated with log-binomial (relative risk) regression.
Excludes beverage choices where the student did not drink a measurable amount, i.e. 0 ounces consumed.
Figure 2 shows the average volume of beverage wasted for each beverage type across the 6 observation days. As displayed in Table 3, the mean volume of milk consumed by students decreased by 0.3 ounces following removal of chocolate milk (95% CI [− 0.6, 0.0]) and water increased by 0.6 ounces (95% CI [0.3, 1.0]). For chocolate milk drinkers, the mean volume of milk consumed decreased by 0.4 ounces after removal (95% CI [− 0.7, 0.0]), while the mean volume of milk consumed by chocolate milk abstainers did not change significantly.
Figure 2.
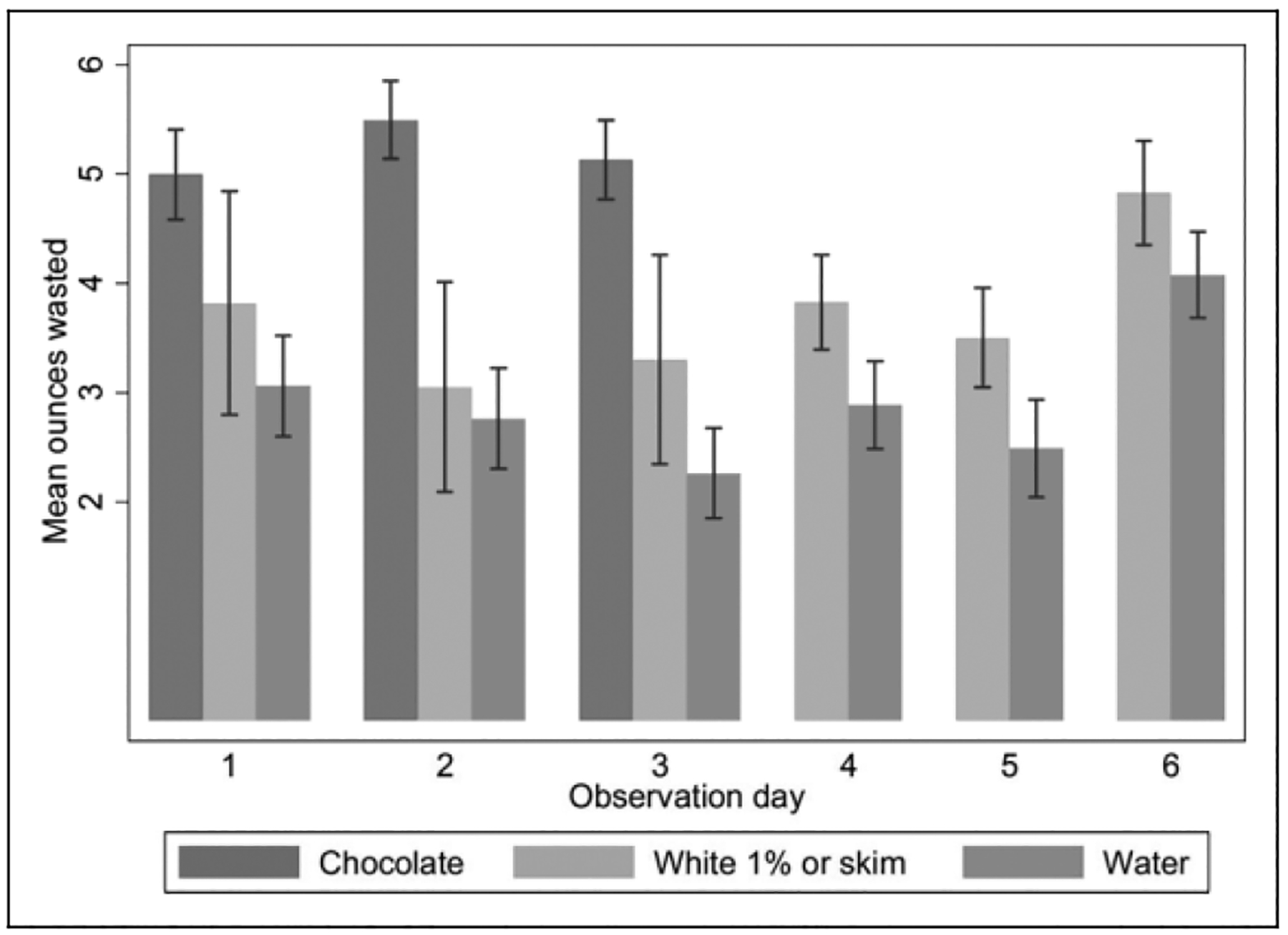
Mean ounces of beverage waste by beverage type and observation day (N = 1,820 beverages). Eight-ounce bottled waters were reintroduced at lunch time 1 week prior to any data collection. This was in response to staff concerns regarding beverage selection following chocolate milk removal to attenuate the novelty of bottled water on student beverage selection during data collection. Both beverage waste measurements and participant observation occurred on 6 total days. Observation days 1–3 occurred prior to chocolate milk removal and observation days 3–6 occurred after. Participant observation also occurred on the day when chocolate milk was reintroduced.
Table 3.
Differences in Average Calcium, Protein, and Added Sugar Intake for Chocolate Milk Drinkers and Chocolate Abstainers Before and After Removal.
| Before | After | Difference | 95% CI | p Value | AIa (%) | Discretionary Calories From Added Sugarb (%) | American Heart Association Limitc (%) | |
|---|---|---|---|---|---|---|---|---|
| All students | ||||||||
| Mean ounces | 4.5 | 4.8 | 0.3 | [0.0, 0.7] | .073 | |||
| Milk (oz) | 2.1 | 1.8 | −0.3 | [−0.6, 0.0] | .031 | |||
| Water (oz) | 2.4 | 3.0 | 0.6 | [0.3, 1.0] | <.001 | |||
| Calcium (mg) | 80.4 | 68.2 | −12.2 | [−23.3, −1.2] | .031 | −4.6 | ||
| Protein (g) | 2.1 | 1.8 | −0.3 | [−0.6, 0.0] | .031 | −3.3 | ||
| Added sugar (g) | 2.8 | 0.0 | −2.8 | [−3.1, −2.5] | <.001 | −25.7 | −33.6 | |
| Chocolate milk drinkers | ||||||||
| Mean ounces | 4.3 | 4.9 | 0.6 | [0.2, 1.0] | .005 | |||
| Milk (oz) | 2.4 | 2.0 | −0.4 | [−0.7, 0.0] | .033 | |||
| Water (oz) | 1.8 | 2.8 | 1.0 | [0.6, 1.3] | <.001 | |||
| Calcium (mg) | 90.4 | 75.9 | −14.5 | [−27.8, −1.2] | .033 | −5.4 | ||
| Protein (g) | 2.4 | 2.0 | −0.4 | [−0.7, 0.0] | .033 | −4.4 | ||
| Added sugar (g) | 3.5 | 0.0 | −3.5 | [−3.9, −3.1] | <.001 | −32.2 | −42.0 | |
| Chocolate milk abstainers | ||||||||
| Mean ounces | 5.4 | 4.7 | −0.7 | [−1.4, −0.1] | .024 | |||
| Milk (oz) | 1.1 | 1.0 | −0.1 | [−0.5, 0.3] | .712 | |||
| Water (oz) | 4.4 | 3.7 | −0.7 | [−1.3, −0.1] | .025 | |||
| Calcium (mg) | 40.1 | 37.2 | −2.9 | [−18.0, 12.3] | .712 | −1.1 | ||
| Protein (g) | 1.1 | 1.0 | −0.1 | [−0.5, 0.3] | .712 | −1.1 | ||
| Added sugar (g) | 0.0 | 0.0 | 0.0 | [0.0, 0.0] | .346 | 0.0 | 0.0 | |
| Difference-in-differences: Chocolate milk drinkers compared to abstainers | ||||||||
| Mean ounces | 1.3 | [0.6, 2.1] | <.001 | |||||
| Milk (oz) | −0.3 | [−0.8, 0.2] | .258 | |||||
| Water (oz) | 1.7 | [1.0, 2.4] | <.001 | |||||
| Calcium (mg) | −11.6 | [−31.8, 8.5] | .258 | −4.3 | ||||
| Protein (g) | −0.3 | [−0.8, 0.2] | .258 | −3.3 | ||||
| Added sugar (g) | −3.5 | [−3.8, −3.1] | <.001 | −32.2 | −42.0 | |||
Note. AI = adequate intake.
AI: Assuming lunch-specific guideline of 257 mg calcium and 9 g protein for children in Grades K–3 (Institute of Medicine, 2010).
Discretionary calories: Assuming 1/3 of 132 total discretionary calories (from solid fats and sugars) as 43.5 calories and 4 calories per gram of sugar for children aged 4–8 years with 1,600 daily calories (Johnson et al., 2009).
American Heart Association limit: Assuming 1/3 of suggested limit of 25 g (six teaspoons) of added sugars for children aged 4–8 years, as a portion of total discretionary calories for added sugars.
Nutrient and Sugar Intake
As displayed in Table 3, after chocolate milk removal, students consumed 2.8 g less added sugar (95% CI [− 3.1,−2.5]), 0.3 g less protein (95% CI [–0.6, 0.0]), and 12.2 mg less calcium (95% CI [−23.3, −1.2]) on average. This represents a 4.6% decrease in the 9 g adequate intake (AI) of protein and 3.3% decrease in the 257 mg AI of calcium for school lunches in K 3rd-grade students, as recommended by the Institute of Medicine (2010). Although chocolate milk drinkers consumed less milk overall after removal (−0.4 ounces, 95% CI [− 0.7, 0.0]), they displayed significant reductions in average added sugar consumption (−3.5 g, 95% CI [−3.9, −3.1]) while only slightly reducing average intake of protein (–0.4 g, 95% CI [–0.7, 0.0]) and calcium (–14.5 mg, 95% CI [−27.8, −1.2]). Chocolate milk abstainers showed no significant changes in nutrients consumption pre- and postintervention.
Following chocolate milk removal, changes in total milk, calcium, and protein intake were not significantly different for chocolate milk drinkers compared to abstainers (i.e., difference-in-differences estimates in Table 3). However, chocolate milk drinkers displayed a significant reduction in added sugar (−3.5 g, 95% CI [−3.8, −3.1]) and increases in mean ounces of overall beverage (1.3 ounces, 95% CI [0.6, 2.1]) and water (1.7 ounces, 95% CI [1.0, 2.4]) consumed as compared to chocolate abstainers.
Staff and Student Reactions
Table 4 presents five emergent themes and illustrative quotes from study field notes. First, school staff viewed chocolate milk as an important source of nutrients to the students; and second, they expressed concern that chocolate milk removal might lead to negative student behaviors. Third, students expressed varied views toward chocolate milk removal and no students rebelled following chocolate milk removal. Fourth, students reported selecting beverages based on familiarity and health impact while staff focused on the role that beverage placement and appearance played. A final theme focused on the short lunch period and limited amount of food and beverage consumed regardless of the presence or absence of chocolate milk.
Table 4.
Emergent Qualitative Themes and Illustrative Quotes Prior to and During Chocolate Milk Removal.
| Theme and Brief Description | Illustrative Quotes/Field Note Excerpts |
|---|---|
| School staff viewed chocolate milk as an important source of nutrients for students As in the larger community, adult staff at the school viewed chocolate milk as a source of nutrients, particularly for low-income students. Teachers and administrators generally felt the nutrition from chocolate milk outweighed the sugar content, particularly because students may not have access to healthy foods at home |
I talked with one of the first grade teachers who told me that, “The missing nutrients lost from removing chocolate milk would be hard to make up if chocolate milk was not an option for the students.” She also added that, “If the students didn’t have a choice of what type of milk to drink they would drink whatever was available, including white milk.” [Field notes, 6/4/2012] [Staff name]: There are 11 grams of sugar in white skim milk and 21 grams of sugar in chocolate skim milk—so even at a minimum you won’t get below 11 … I think the nutrition [in chocolate milk] outweighs the sugar. Many of these kids are without nutrition at home. [Field notes, 5/7/2012] |
| School staff expressed concerns about how students would behave if chocolate milk was removed Adult school employees expressed concern about how removal of chocolate milk might impact student behaviors. This influenced how some staff talked to students about the study. For example, one staff member reported that some school officials gave student verbal clues that they should “be angry” when chocolate milk was removed |
[Administrative leadership] comment that the kids are going to be mad when chocolate milk is removed—only about 20 white milks are taken each meal period and the rest are chocolate. [Field notes, 5/7/2012] [One staff member told the research team] … The [cooks] really psyched the kids out before the study started. Every day for two weeks before the study s/he warned the kids as they enter the lunch service area: “You better drink that chocolate milk because they are going to take it away in [daily countdown]!” This occurred on a daily basis throughout the entire lunch service. I think you should know this because I don’t think you can have an objective study if one of the cooks if frightening the kids and heightening the concerns about chocolate milk even before [the study] starts. [Field notes, 5/31/2012] |
| Students expressed varied views toward chocolate milk removal at lunch; no students rebelled following removal Students expressed diverse opinions regarding what they would drink if chocolate milk was removed. Following removal, many students were surprised, but there was not a large-sale upheaval or rebellion as anticipated by parents and staff prior to the study. This was a surprise to school staff and to many of the research team members |
At the start of the study, students expressed varied opinions regarding what they would drink if chocolate milk was removed. Some students reported their hate for white milk and commitment to chocolate milk through statements like the following: “I hate the blue [skim] milk,” “I will only drink chocolate milk,” and “If there was no chocolate milk I wouldn’t drink anything.” However, other students stated, “If there was no chocolate milk I would drink 1% or water.” [Field notes, 5/11/2012] … I was stationed by the milk cooler today [the first day of chocolate milk removal] …. The 1st grade classes were the first to pass through the line. The most common reaction comment was, “Where is the chocolate milk?” and “Why would you take it away?” Some of the students appeared surprised. One student said, “Gall dang it why would you do that?” [Field notes, 5/14/2012] |
| Factors associated with beverage selection: familiarity, health, placement, and appearance Students select their beverage of choice based on various reasons, the most prevalent being (a) familiarity with an option or (b) fear/uncertainty over the alternates. These students had various theories on the health benefits or harms of different beverages which influenced their selection Adult staff in contrast focused on the role that beverage placement and visual presentation played on drink selection. Adjusting the look of the milk cartons and providing water in little bottles, versus at a drinking fountain in the cafeteria, could increase selection of these choices |
Students reported that taste- or health-related factors were associated with their beverage selection choice. Common statements across students of all ethnicities and grades include concepts like: “[Milk] makes you healthy, and makes your bones strong,” “[Milk] helps when you eat spicy food,” or “Water is good for you.” A few students commented on the higher sugar content in chocolate milk. [Field notes, 5/24/2012] One first grade girl commented, “I have never tried white milk. I take chocolate milk, if available, if not I take water.”…. In a deeper discussion [with this student], I discovered that she was uncertain what was in the two differently labeled milks. She chose the chocolate milk because she knew what chocolate tasted like. She didn’t know what skim or 1% meant and she was actually frightened to try either of the two other milk options [Field notes, 5/24/2012] In contrast, staff focused on the role beverage placement and appearance played in student’s selection. One staff member comment that, “People ‘eat with their eyes’—it’s all about marketing to the students. She says things catch kid’s eyes and they want to eat it—that’s why they took the water. A few months back they had a new milk that they used at [another school] with a ‘moo moo’ logo on the front. It was skim milk but all the kids took it because they eat with our eyes” [Field notes, 5/ 7/2012] |
| School staff and study team members noted that the lunch period was too short and that there was a substantial amount of food and beverage waste The lunch period was short—regardless of whether chocolate milk was present or absent. Time to eat may be adequate if you are at the start of the lunch line (20 min) but not if you are at the end (5 min). Observers on the research team commented on the large amount of food and beverage waste regardless of the student’s choice |
One ofthe teachers talked with me about the limited time available for the students to eat. They have 20 min to go through the line, eat, and dump their trays… She worries that the kids do not have enough time to eat. She also states that many of the students eat all of their meals at the school and it is important that these kids have enough time to eat [Field notes, 5/11/12] At the end ofservice, a lot offood was disposed of. I believe this may be because not all ofthe students had enough time to finish their lunch and because portion sizes were quite large [Field notes, 5/10/12] [During lunch] most of the students were focused on eating and talking… Their teachers tell them when they only had two minutes left [for lunch], it did not seem like there was much time for them to eat at all, they were rushed to eat their food and move on [Field notes, 5/11/12] |
Discussion
Our study suggests that young, school-age children are able to transition away from flavored milk in school-provided lunches and that doing so can positively impact their nutritional intake. Similar to prior research (Hanks et al., 2014; Quann & Adams, 2013), we found the overall milk selection decreased after removal of chocolate milk. However, in our study, we found that compared to chocolate milk, students were significantly more likely to consume white milk and water when selected (RR 1.12 and 1.18, respectively) and to consume greater volumes (4.9 and 5.9 ounces, respectively). Therefore, although chocolate milk drinkers were less likely to consume any milk following removal, we saw only small decreases in the mean ounces of milk consumed in the total sample (–0.3 ounces) and in chocolate milk drinkers (–0.4 ounces). Across the sample, this led to a significant reduction in average added sugar intake (–2.8 g), but only small reductions in average protein and calcium intake (−0.3 g and −12.2 mg, respectively). Drink choices were largely consistent for chocolate milk abstainers across all study days, suggesting that these students were not affected by its removal. Difference-in-differences estimates showed the decrease in added sugar was significant, but the reduction in total milk, calcium, and protein intake was not significantly different between chocolate milk drinkers and chocolate milk abstainers. Although adult staff members were concerned about student reactions in response to chocolate milk removal, students accepted the change in stride.
Our findings emphasize the importance of considering individual-level data in beverage and plate waste studies to assess the impact of interventions on children’s diet and nutrition. Previous research on interventions involving removal of flavored milk from school lunches indicates that milk consumption decreased following removal based on aggregate measures of beverage selection and waste (Hanks et al., 2014; Quann & Adams, 2013). Nonintervention studies have emphasized the nutritional value of flavored milk, suggesting that students’ nutritional intake will be compromised in the absence of flavored milk (Frary et al., 2004; Johnson et al., 2002; Murphy et al., 2008). However, although we found similar effects when assessing the aggregate changes in beverage selection pre- and postintervention, our assessment of individual beverage consumption and subsequent nutrient intake provided a different picture. Specifically, the mean volume of milk consumed by students changed by a negligible amount, 0.3 fluid ounces (less than two teaspoons), and the difference between chocolate milk drinkers and abstainers was not significant. Decreases in protein and calcium intake were also small at 0.3 g and 12.2 mg, respectively; for comparison, a six-inch tortilla contains 1.4-g protein and 19-mg calcium (U.S. Department of Agriculture & Service, 2015). While there are no standard recommended daily allowances for sugar intake for children, the American Heart Association currently suggests limiting intake to 25 g per day in this age-group (Johnson et al., 2009); 3.5 g is an important reduction relevant to this limit. When we project the 3.5 g average decrease in daily sugar intake over the course of a school year—the average amount of sugar consumed by chocolate milk drinkers in our study prior to removal—our findings suggest that removing chocolate milk from school lunches translates into eliminating 588 g sugar, 2,352 calories, and 2/3 pounds of weight per student per year.
Interventions to help schools become health-promoting environments are a central component of a broader approach and growing evidence base for addressing environmental factors that contribute to childhood obesity (Gortmaker et al., 2015; Institute of Medicine, 2012; Waters et al., 2011). Children’s dietary habits are influenced by their physical, social, and media environments, making schools— where children consume 50% of their daily calories and spend a majority of their waking hours—a critical context for shaping food and beverage choices as well as influencing the dietary requests children make at home (Institute of Medicine, 2006, 2010, 2012). Briefel and colleagues (2013) evaluated home and school beverage consumption and found that flavored milk consumption was highest in school and accounted for an average of 1.5 teaspoons of added sugar daily. Although our study showed removing flavored milk reduced daily added sugar intake by a smaller margin (3.5 g), it indicates an opportunity to make school environments more health-promoting by influencing student beverage preferences and reducing added sugar intake.
Another avenue to improve student’s beverage consumption behaviors during school-provided meals is to focus on increasing consumption of white milk to support mineral and nutrient intake. Short of removing flavored milk from school-provided meals, other studies have examined interventions to make white milk more convenient, attractive, and normative as an alternative approach to changing student behaviors (Goto et al., 2013; Hanks, Just, & Wansink, 2013). Interestingly, our qualitative findings revealed that although adult staff indicated that students selected beverages based on placement and appearance, students reported that they chose beverages based on familiarity and perceived nutritional benefit. Our quantitative finding that 21% of all selected beverages were not consumed by students during the study and our qualitative finding of short lunch periods with extensive waste suggest that extending school lunch length and promoting beverage consumption may present additional areas for improvement. Additionally, some students may benefit from interventions to increase nutrition education and opportunities to sample white milk.
This study provides an example of how engaging community partners in all phases of research can help clarify and address local health needs. Schools lend themselves to community–academic partnerships to explore programs that address school meal options and other interventions (J. F. Cohen et al., 2012; Golub et al., 2011). Following data collection and analysis, CHIRP members shared the results of the pilot study with the local school board and other stake-holders. However, the opposition to changing district policy was evident; a milk producer used the meeting as a venue to distribute chocolate milk samples. Subsequently, Oregon State University Extension SNAP-Ed (2014) released a policy statement, supporting the availability of flavored milk in Oregon schools and opposing strategies that aim to eliminate flavored milk. As we observed during the intervention, chocolate milk removal provoked numerous concerns among adult staff members who were wary of the change and in some cases communicated warnings directly to the students. Similar to Golub and colleagues’ findings from changing milk options in New York City schools, future efforts to change local school lunch options may require education to address the concerns of adults rather than students, as well as education to win local policy maker support in the face of pressure from the dairy industry (Golub et al., 2011).
Limitations
There are several important limitations to this study. First, we assessed the effects of flavored milk removal at one rural primary school serving students in kindergarten through second grade. Student and staff behaviors may have been influenced by the presence of outside adult observers and findings may not be generalizable to other schools, student populations, or age-groups. Second, our study had a limited time frame with six beverage waste data collection days occurring over approximately 2 months’ time. Therefore, we were unable to assess the longer term effects of flavored milk removal on students’ behavior or health outcomes. Additionally, the reintroduction of bottled water as a beverage option 1 week prior to the start of the study may have influenced student beverage selection, as the novel option may have been more attractive to students than if it was already established as a regular part of the school lunch choices. However, bottled water consumption did not significantly differ across the 3 days prior to chocolate milk removal, suggesting that reintroducing bottled water at lunch 1 week in advance of data collection was effective. Despite these limitations, we anticipate that findings can inform both school policy and future research applications.
Conclusions
Our study shows that removing flavored milk from school-provided lunches can lower students’ daily added sugar consumption with only minimal decreases in calcium and protein intake. Although overall rates of milk selection declined following the removal of chocolate milk, analyses of individual-level beverage waste data showed the average amount of milk consumed decreased by a negligible amount. Our difference-in-differences estimates further indicated that following chocolate milk removal reduction in ounces of milk, calcium, and protein were not significantly different between chocolate milk drinkers and chocolate milk abstainers, while reductions in added sugar were significant. These results highlight the importance of looking at individual-level beverage and plate waste data in subsequent studies assessing changes in student consumption and nutritional intake from school-provided meals.
Our findings provide important insight on the experiences and views of primary school students and staff with regard to flavored milk and other school-provided beverage options. Although some adult staff members expressed concerns about negative student reactions following chocolate milk removal, this change was largely accepted by students. In combination with other interventions to help schools become health-promoting environments, interventions that reduce the availability of flavored milk may be a strategy to promote healthful diet and prevent childhood obesity. Rigorous, nonindustry-sponsored research using individual-level beverage consumption is needed to understand the effects of chocolate milk removal across student populations and age-groups, as well as to assess the long-term impacts on student behaviors and health outcomes.
Implications for School Nursing Practice
Students receive a majority of their nutrition from school settings, especially students from families with lower social economic status. Thus, school nurses can have a large impact on student health by advocating for health food and beverage options at lunch, ensuring adequate time for students to consume their meals, and to use teachable moments within the school day to educate students and staff about healthy eating and drinking habits.
Our qualitative findings show that students are open to the removal of flavored milk during lunch, and our quantitative findings indicate that removal led to a reduction in daily added sugar consumption with only minimal decreases in calcium and protein intake. Thus, school nurses can use this as an example of the ability to guide families and students through small changes that can have a positive effect on their health. Furthermore, school nurses can play an essential role in community-based research to address student population health issues. This role should be explored to support policy changes locally that affect the health of the students and staff of that community.
Acknowledgments
We greatly appreciate the efforts of Mountain View Community Health Improvement and Research Partnership members who contributed to study design and helped collect data: Marissa Becker, Shawn Gaddy Winsor, Carolyn Harvey, Glenda Hyde, Barb Ibrahim, Tom Machala, Danita Macy, Teresa Martin, Tryna Muilenburg, and Katie Russell. We are also grateful to Madras Primary School for their participation and valuable assistance in conducting this study. Molly Hamlin assisted with data collection and provided input on early manuscript versions. Robyn Pham provided editorial support with manuscript revisions.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a Community Engagement Supplement to the Oregon Clinical and Translational Research Institute at Oregon Health & Science University (National Center for Advancing Translational Sciences of the National Institute of Health award numbers UL1TR000128 and ACTRI0601). Dr. Davis is supported in part by an Agency for Healthcare Research & Quality-Funded Patient Centered Outcomes Research K12 award (Award Number 1 K12 HS022981 01).
Author Biographies
Melinda M. Davis, PhD, is a research assistant professor at the Department of Family Medicineand OHSU-PSU School of Public Health and the director of Community Engaged Research, Oregon Rural Practice-Based Research Network, Oregon Health & Science University, Portland, OR, USA.
Margaret Spurlock, MPH, is a School-Based Health Center program coordinator at Oregon Health & Science University, Portland, OR, USA.
Katrina Ramsey, MPH, is the biostatistician at the OHSU-PSU School of Public Health, Oregon Health & Science University, Portland, OR, USA.
Jamie Smith, MPH, BSN, RN, NCSN, is a school nurse consultant at the Adolescent and School Health Program, Oregon Public Health Division, Portland, OR, USA.
Beth Ann Beamer, RN, is a family and community health coordinator and county leader of Warm Springs Extension, Warm Springs, OR, USA.
Susan Aromaa, MS, is a program manager at the Center for Evidence-Based Policy, Oregon Health & Science University, Portland, OR, USA.
Paul B. McGinnis, MPA, is a Coordinated Care Organization Integration Director at the Greater Oregon Behavioral Health Inc., The Dalles, OR, USA.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Earlier in the school year, 8-ounce bottled water was available as a beverage option to students as they came through the lunch line. However, a water fountain was installed in the cafeteria and bottled water was removed in order to minimize waste and to reduce costs.
References
- Archer E, Hand GA, & Blair SN (2013). Validity of U.S.nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS One, 8, e76632. doi: 10.1371/journal.pone.0076632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow SE (2007). Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics, 120, S164–S192. doi: 10.1542/peds.2007-2329C [DOI] [PubMed] [Google Scholar]
- Bes-Rastrollo M, Schulze MB, Ruiz-Canela M, & Martinez-Gonzalez MA (2013). Financial conflicts of interest and reporting bias regarding the association between sugar-sweetened beverages and weight gain: A systematic review of systematic reviews. PLoS Medicine, 10, e1001578; discussion e1001578. doi: 10.1371/journal.pmed.1001578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdewic SP (1999). Participant observation In Crabtree BF, & Miller WL (Eds.), Doing qualitative research (2nd ed., pp. 47–70). Thousand Oaks, CA: Sage. [Google Scholar]
- Briefel RR, Wilson A, Cabili C, & Hedley Dodd A (2013). Reducing calories and added sugars by improving children’s beverage choices. Journal of the Academy of Nutrition and Dietetics, 113, 269–275. doi: 10.1016/j.jand.2012.10.016 [DOI] [PubMed] [Google Scholar]
- Bucher Della Torre S, Keller A, Laure Depeyre J, & Kruseman M (2015). Sugar-sweetened beverages and obesity risk in children and adolescents: A systematic analysis on how methodological quality may influence conclusions. Journal of the Academy of Nutrition and Dietetics. doi: 10.1016/j.jand.2015.05.020 [DOI] [PubMed] [Google Scholar]
- Cliff P (2011, November 20). School debate over flavored milk:Bend-La Pine district, parents weigh nutritional value and sugar content. The Bulletin. [Google Scholar]
- Cliff P (2012, April 27). Flavored milk ban urged, Online petition targets Bend-La Pine cafeterias. The Bulletin. [Google Scholar]
- Cohen DJ, & &Crabtree BF. (2008). Evaluative criteria for qualitative research in health care: Controversies and recommendations. Annals of Family Medicine, 6, 331–339. doi: 10.1370/afm.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DJ, & &Crabtree BF. (n.d.) Qualitative research guidelines project. Retrieved from http://www.qualres.org/HomeMemb-3696.html [Google Scholar]
- Cohen JF, Smit LA, Parker E, Austin SB, Frazier AL,Economos CD, & Rimm EB (2012). Long-term impact of a chef on school lunch consumption: Findings from a 2-year pilot study in Boston middle schools. Journal of the Academy of Nutrition and Dietetics, 112, 927–933. doi: 10.1016/j.jand.2012.01.015 [DOI] [PubMed] [Google Scholar]
- Crabtree BF, & Miller WL (1999). Doing qualitative research (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Creswell JW, Klassen AC, Plano Clark VL, & Smith KC. (2011). Best practices for mixed methods research in the health sciences. National Institutes of Health; Retrieved from http://obssr.od.nih.gov/training/mixed-methods-research/ [Google Scholar]
- Creswell JW, & Plano Clark VL (2011). Designing and conducting mixed methods research (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Davis MM, Aromaa S, McGinnis PB, Ramsey K, Rollins N, Smith J, … Fagnan LJ. (2014). Engaging the under-served: A process model to mobilize rural community health coalitions as partners in translational research. Clinical and Translational Science, 7, 300–306. doi: 10.1111/cts.12168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AM, Bennett KJ, Befort C, & Nollen N (2011). Obesity and related health behaviors among urban and rural children in the United States: Data from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006. Journal of Pediatric Psychology, 36, 669–676. doi: 10.1093/jpepsy/jsq117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebbeling CB, Pawlak DB, & Ludwig DS (2002). Childhood obesity: Public-health crisis, common sense cure. The Lancet, 360, 473–482. doi: 10.1016/s0140-6736(02)09678-2 [DOI] [PubMed] [Google Scholar]
- Frary CD, Johnson RK, & Wang MQ (2004). Children and adolescents’ choices of foods and beverages high in added sugars are associated with intakes of key nutrients and food groups. Journal of Adolescent Health, 34, 56–63. doi: 10.1016/s1054-139x(03)00248-9 [DOI] [PubMed] [Google Scholar]
- Golub M, Charlop M, Groisman-Perelstein AE, Ruddock C, & Calman N (2011). Got low-fat milk? How a community-based coalition changed school milk policy in New York City. Family & Community Health, 34, S44–S53. doi: 10.1097/FCH.0b013e318202a7dd [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL, … Wang YC. (2015). Cost effectiveness of childhood obesity interventions: Evidence and methods for choices. American Journal of Preventive Medicine, 49, 102–111. doi: 10.1016/j.amepre.2015.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gortmaker SL, Long MW, & Wang YC (2009). The negative impact of sugar-sweetened beverages on children’s health. Princeton, NJ: Retrieved from http://healthyeatingresearch.org/wp-content/uploads/2013/12/HER-SSB-Synthesis-091116_FINAL.pdf [Google Scholar]
- Goto K, Waite A, Wolff C, Chan K, & Giovanni M (2013). Do environmental interventions impact elementary school students’ lunchtime milk selection? Applied Economic Perspectives and Policy, 35, 360–376. doi: 10.1093/aepp/ppt004 [DOI] [Google Scholar]
- Guinn CH, Baxter SD, Royer JA, & Hitchcock DB (2013). Explaining the positive relationship between fourth-grade children’s body mass index and energy intake at school-provided meals (breakfast and lunch). Journal of School Health, 83, 328–334. doi: 10.1111/josh.12035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanks AS, Just DR, & Wansink B (2013). Smarter lunch-rooms can address new school lunchroom guidelines and childhood obesity. Journal of Pediatrics, 162, 867–869. doi: 10.1016/j.jpeds.2012.12.031 [DOI] [PubMed] [Google Scholar]
- Hanks AS, Just DR, & Wansink B (2014). Chocolate milk consequences: A pilot study evaluating the consequences of banning chocolate milk in school cafeterias. PLoS One, 9, e91022. doi: 10.1371/journal.pone.0091022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu FB (2013). Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obesity Reviews, 14, 606–619. doi: 10.1111/obr.12040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsberger M, McGinnis P, Smith J, Beamer BA, & O’Malley J (2015). Calorie labeling in a rural middle school influences food selection: Findings from community-based participatory research. Journal of Obesity, 2015, 531690. doi: 10.1155/2015/531690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsberger M, McGinnis P, Smith J, Beamer BA, & O’Malley J, Mountain View Community Health, I., & Research, P. (2014). Elementary school children’s recess schedule and dietary intake at lunch: A community-based participatory research partnership pilot study. BMC Public Health, 14, 156. doi: 10.1186/1471-2458-14-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2006). Food marketing to children and youth: Threat or opportunity? Retrieved from http://www.nap.edu/catalog/11514/food-marketing-to-children-and-youth-threat-or-opportunity [Google Scholar]
- Institute of Medicine. (2010). School meals: Building blocks for healthy children. Washington, DC: Retrieved from http://www.fns.usda.gov/sites/default/files/SchoolMealsIOM.pdf [Google Scholar]
- Institute of Medicine. (2012). Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: Retrieved from http://iom.nationalacademies.org/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, & Lustig RH, … Prevention. (2009). Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation, 120, 1011–1020. doi: 10.1161/CIRCULATIONAHA.109.192627 [DOI] [PubMed] [Google Scholar]
- Johnson RK, Frary C, & Wang M (2002). The nutritional consequences of chocolate milk consumption by school-aged students and adolescents in the United States. Journal of the American Dietetic Association, 102, 853–856. [DOI] [PubMed] [Google Scholar]
- Kaiser KA, Shikany JM, Keating KD, & Allison DB (2013). Will reducing sugar-sweetened beverage consumption reduce obesity? Evidence supporting conjecture is strong, but evidence when testing effect is weak. Obesity Reviews, 14, 620–633. doi: 10.1111/obr.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan LK, Sobush K, Keener D, Goodman K, Lowry A, & Kakietek J, … Prevention. (2009). Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recommendations and Reports, 58, 1–26. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19629029 [PubMed] [Google Scholar]
- Lesser LI, Ebbeling CB, Goozner M, Wypij D, & Ludwig DS (2007). Relationship between funding source and conclusion among nutrition-related scientific articles. PLoS Medicine, 4, e5. doi: 10.1371/journal.pmed.0040005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Let’s Move! Healthy Schools. n.d. Retrieved from https://letsmove.obamawhitehouse.archives.gov/
- Lumley T, Diehr P, Emerson S, & Chen L (2002). The importance of the normality assumption in large public health data sets. Annual Review of Public Health, 23, 151–169. doi: 10.1146/annurev.publhealth.23.100901.140546 [DOI] [PubMed] [Google Scholar]
- Mack N, Woodson C, Macqueen K, Guest G, & Namey E (2005). Module 2: Participant observation Qualitative research methods: A data collector’s field guide (pp. 12–28). USAID/ Family Health International; Retrieved from https://www.fhi360.org/resource/qualitative-research-methods-data-collectors-field-guide. [Google Scholar]
- Malik VS, Pan A, Willett WC, & Hu FB (2013). Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. American Journal of Clinical Nutrition, 98, 1084–1102. doi: 10.3945/ajcn.113.058362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malterud K (2001). Qualitative research: Standards, challenges, and guidelines. Lancet, 358, 483–488. doi: 10.1016/s0140-6736(01)05627-6 [DOI] [PubMed] [Google Scholar]
- Matheny S (2013, September 11). Milk debate flavored with controversy. The Madras Pioneer. [Google Scholar]
- McGinnis PB, Hunsberger M, Davis M, Smith J, Beamer BA, & Hastings DD (2010). Transitioning from CHIP to CHIRP: Blending community health development with Community-based Participatory Research. Family & Community Health, 33, 228–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer BD (1995). Natural and quasi-experiments in economics. Journal of Business & Economic Statistics, 13, 151–161. doi: 10.2307/1392369 [DOI] [Google Scholar]
- Miles MB, & Huberman AM (1994). Qualitative data analysis (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Miller PE, McKinnon RA, Krebs-Smith SM, Subar AF, Chriqui J, Kahle L, & Reedy J (2013). Sugar-sweetened beverage consumption in the U.S.: Novel assessment methodology. American Journal of Preventive Medicine, 45, 416–421. doi: 10.1016/j.amepre.2013.05.014 [DOI] [PubMed] [Google Scholar]
- Murphy MM, Douglass JS, Johnson RK, & Spence LA (2008). Drinking flavored or plain milk is positively associated with nutrient intake and is not associated with adverse effects on weight status in US children and adolescents. Journal of the American Dietetic Association, 108, 631–639. doi: 10.1016/j.jada.2008.01.004 [DOI] [PubMed] [Google Scholar]
- Nicklas TA, O’Neil CE, & Fulgoni VL (3rd ed.). (2013). The nutritional role of flavored and white milk in the diets of children. Journal of School Health, 83, 728–733. doi: 10.1111/josh.12087 [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2014). Prevalence of childhood and adult obesity in the United States, 2011–2012. Journal of the American Medical Association, 311, 806–814. doi: 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oregon Department of Education. (2014–2015a). Student ethnicity: Jefferson county school district 509J. Retrieved from http://www.oregon.gov/ode/reports-and-data/students/Pages/Student-Enrollment-Reports.aspx [Google Scholar]
- Oregon Department of Education. (2014–2015b). Students eligible for free or reduced lunch: Jefferson county school district 509J. Retrieved from http://www.ode.state.or.us/sfda/reports/r0061Select2.asp [Google Scholar]
- Oregon State University Extension SNAP-Ed. (2014, September 26). [OSU Extension SNAP-Ed Policy Statement: Flavored Milk in Schools]. [Google Scholar]
- Patton MQ (1999). Enhancing the quality and credibility of qualitative analysis. Health Services Research, 34, 1189–1208. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1089059/ [PMC free article] [PubMed] [Google Scholar]
- Quann EE, & Adams D (2013). Impact on milk consumption and nutrient intakes from eliminating flavored milk in elementary schools. Nutrition Today, 48, 127–134. doi: 10.1097/NT.0b013e3182941d6a [DOI] [Google Scholar]
- Singh GK, Kogan MD, Van Dyck PC, & Siahpush M (2008). Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: Analyzing independent and joint associations. Annals of Epidemiology, 18, 682–695. doi: 10.1016/j.annepidem.2008.05.001 [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, & Kogan MD (2010). Rising social inequalities in US childhood obesity, 2003–2007. Annals of Epidemiology, 20, 40–52. doi: 10.1016/j.annepidem.2009.09.008 [DOI] [PubMed] [Google Scholar]
- Skinner AC, Steiner MJ, & Perrin EM (2012). Self-reported energy intake by age in overweight and healthy-weight children in NHANES, 2001–2008. Pediatrics, 130, e936–e942. doi: 10.1542/peds.2012-0605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AL, & Corbin JM (1990). Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park, CA: Sage. [Google Scholar]
- Te Morenga L, Mallard S, & Mann J (2013). Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. British Medical Journal, 346, e7492. doi: 10.1136/bmj.e7492 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. (2017). HealthierUS School Challenge. Retrieved from http://www.fns.usda.gov/hussc/healthierus-school-challenge-smarter-lunchrooms [Google Scholar]
- U.S. Department of Agriculture & Service, A. R. (2015). USDA national nutrient database for standard reference, release 28. Retrieved from http://ndb.nal.usda.gov/ndb/search/list [Google Scholar]
- Vilsack TJ. (2012). The healthy, hunger-free kids act—Building healthier schools. Childhood Obesity, 8, 4. doi: 10.1089/chi.2011.0800.vils [DOI] [PubMed] [Google Scholar]
- Wang Y, & Beydoun MA (2007). The obesity epidemic in the United States—Gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews, 29, 6–28. doi: 10.1093/epirev/mxm007 [DOI] [PubMed] [Google Scholar]
- Wang YC, Bleich SN, & Gortmaker SL (2008). Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics, 121, e1604–e1614. doi: 10.1542/peds.2007-2834 [DOI] [PubMed] [Google Scholar]
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, … Summerbell CD. (2011). Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews, 12, CD001871. doi: 10.1002/14651858.CD001871.pub3 [DOI] [PubMed] [Google Scholar]
- Winett L, Gauntner C, Becker T, & Mladenovic J (2015). State of our health 2015: Key health indicators for Oregonians. Portland, OR. Retrieved from http://www.ohsu.edu/xd/education/student-services/about-us/provost/upload/state-of-our-health-2015.pdf [Google Scholar]
- Young-Lorion J, Davis MM, Kirks N, Hsu A, Slater JK, Rollins N, … McGinnis P. (2013). Rural Oregon community perspectives: Introducing community-based participatory research into a community health coalition. Progress in Community Health Partnerships, 7, 313–322. doi: 10.1353/cpr.2013.0032 [DOI] [PMC free article] [PubMed] [Google Scholar]


