Abstract
Background
Health care workers (HCW) are at high risk of developing physical/mental health outcomes related to coronavirus syndromes. Nature and frequency of these outcomes are undetermined.
Methods
PRISMA/MOOSE-compliant (PROSPERO-CRD42020180205) systematic review of Web of Science/grey literature until 15th April 2020, to identify studies reporting physical/mental health outcomes in HCW infected/exposed to Severe Acute Respiratory Syndrome -SARS-, Middle East Respiratory Syndrome -MERS-, Novel coronavirus -COVID-19-. Proportion random effect meta-analyses, I2 statistic, quality assessment and sensitivity analysis.
Results
115 articles were included (n=60,458 HCW, age 36.1±7.1, 77.1% female). Physical health outcomes: 75.9% HCW infected by SARS/MERS/COVID-19 reported fever (95%CI=65.9–83.7%, k=12, n=949), 47.9% cough (95%CI=39.2–56.8%, k=14, n=970), 43.6% myalgias (95%CI=31.9–56.0%, k=13, n=898), 42.3% chills (95%CI=20.2–67.9%, k=7, n=716), 41.2% fatigue (95%CI=18.2–68.8%, k=6, n=386), 34.6% headaches (95%CI=23.1–48.2%, k=11, n=893), 31.2% dyspnoea (95%CI=23.2–40.5%, k=12, n=1003), 25.3% sore throat (95%CI=18.8–33.2%, k=8, n=747), 22.2% nausea/vomiting (95%CI=14.9–31.8%, k=6, n=662), 18.8% diarrhoea (95%CI=11.9–28.4%, k=9, n=824). Mental health outcomes: 62.5% HCW exposed to SARS/MERS/COVID-19 reported general health concerns (95%CI=57.0–67,8%, k=2, n=2254), 43.7% fear (95%CI=33.9–54.0%, k=4, n=584), 37.9% insomnia (95%CI=30.9–45.5%, k=6, n=5067), 37.8% psychological distress (95%CI=28.4–48.2%, k=15, n=24,346), 34.4% burnout (95%CI=19.3–53.5%, k=3, n=1337), 29.0% anxiety features (95%CI=14.2–50.3%, k=6, n=9191), 26.3% depressive symptoms (95%CI=12.5–47.1%, k=8, n=9893), 20.7% post-traumatic stress disorder features (95%CI=13.2–31%, k=11, n=3826), 16.1% somatisation (95%CI=0.2–96.0%, k=2, n=2184), 14.0% stigmatisation feelings (95%CI=6.4–28.1%, k=2, n=411).
Limitations
Limited amount of evidence for some outcomes and suboptimal design in several studies included.
Conclusions
SARS/MERS/COVID-19 have a substantial impact on the physical and mental health of HCW, which should become a priority for public health strategies.
Keywords: Coronavirus, COVID-19, SARS, MERS, Health care workers, Meta-analysis
1. Introduction
The novel "SARS-CoV-2" or "2019-nCoV" coronavirus disease (COVID-19) identified in Wuhan is not the first coronavirus to have quickly spread and caused havoc in the 21st century. The SARS-CoV identified in Canton (Severe Acute Respiratory Syndrome, SARS hereby), became the first zoonosis of this century (2002) (Chen et al., 2006), followed by the MERS-CoV (Middle East Respiratory Syndrome MERS hereby), identified in 2012 in Saudi Arabia. These three syndromes can be transmitted by mildly ill, pre-symptomatic or asymptomatic infected individuals (Shah et al., 2020) and are putting healthcare systems under unprecedented pressure (Holmes et al., 2020; Shah et al., 2020; Xiang et al., 2020). Half of the general population rated the psychological impact of the COVID-19 outbreak as being moderate or severe (Wang et al., 2020). However, the World Health Organisation has identified health care workers (HCW) as a group at particular risk of developing a wide range of physical/mental problems as a result of working directly or indirectly with COVID-19 patients (Koh et al., 2003). HCW are particularly exposed to the threat of transmission (Huang et al., 2020) because of their frontline work with patients with high viral loads and suboptimal personal protection equipment (Christian et al., 2004; Ehrlich et al., 2020; Nam et al., 2017). At the same time, severe stress, high emotional load, long working hours, concerns of being infected or infecting their relatives, lack of adequate support in the working environment and lack of effective supportive treatments can affect HCW's mental health (Moazzami et al., 2020; Vieta et al., 2020).
Despite the profound impact of these syndromes on HCW's physical/mental health, to our knowledge, no systematic review has comprehensively appraised the burden (type and frequency) of these outcomes in the current literature. Profiling the impact of SARS/MERS/COVID-19 on the HCW's health is pivotal to inform detection, monitoring and preventive/treatment strategies. The current systematic review and meta-analysis provide the first quantitative evidence synthesis of the impact of SARS/MERS/COVID-19 on physical and mental health outcomes of HCW.
2. Methods
This study (study protocol registered on PROSPERO-CRD42020180205) was conducted in accordance with “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) (Moher et al., 2009) (eTable I) and “Meta-analyses Of Observational Studies in Epidemiology” (MOOSE) checklist (Stroup et al., 2000) (eTable II), following “EQUATOR Reporting Guidelines” (Altman et al., 2008).
2.1. Search strategy and selection criteria
A systematic literature search was carried out by two independent researchers (GSP, AC) using the following keywords: “SARS” OR “COV” OR “coronavirus” OR “MERS” OR “Orthocoronavirinae” OR “Severe Acute Respiratory Syndrome” OR “Middle East Respiratory Syndrome” OR "CoV-19” OR “SARS-CoV” OR "SARS-CoV-2” OR "2019 nCoV" OR “2019nCoV” OR "2019 novel coronavirus" OR "COVID 19" OR "new coronavirus" OR "novel coronavirus" OR "SARS CoV-2" OR “Wuhan coronavirus” OR "COVID 19" OR "2019-nCoV" AND “professionals” OR “worker*” OR “doctor*” OR “nurse*” OR “occupation*” OR “employee*” OR “healthcare provider*” OR “healthcare worker*” OR “healthcare employee*” OR “personnel” OR “emergency worker” OR “paramedic*”. First, Web of Science database (Clarivate Analytics) was searched, incorporating the Web of Science Core Collection, the BIOSIS Citation Index, the KCI-Korean Journal Database, MEDLINE®, the Russian Science Citation Index, and the SciELO Citation Index, from inception until 15th April 2020. Second, given that this field is rapidly developing, we searched the preprint servers medRxiv, psyArXiv and bioRxiv for the terms ‘coronavirus’ or ‘COVID-19’ from 1st January 2020 until 15th April 2020. Third, we searched references from included studies and reviews that were screened during the literature search. We screened articles identified as abstracts, and after excluding those that did not meet our inclusion criteria, the full texts of the remaining articles were assessed for eligibility and decisions made about their inclusion.
2.2. Condition and individuals being studied
Inclusion criteria for the systematic review were a) individual studies with primary data (including letters, commentaries, qualitative studies and conference proceedings) or grey literature, b) focusing on HCW (including physicians, nurses, trainees and other health professionals) exposed to or infected by SARS/MERS/COVID-19 (see below), c) reporting physical or mental health outcomes, d) sample size >5 and e) written in English. Exclusion Criteria were a) reviews, clinical cases, or study protocols, b) reporting outcomes on populations other than HCW, including the general population, c) with sample size ≤5. For the meta-analysis, additional inclusion criteria were a) reporting meta-analysable data and b) non-overlapping samples (overlap was determined by looking at the type of population and country in which the study was carried, and the study with the largest sample was then selected).
2.3. Data extraction
Two researchers (GSP, JVS) independently extracted data from all the included studies. The two databases were then cross-checked, and discrepancies were resolved through consensus under the supervision of a senior researcher (PFP). A summary of selected variables included: first author and year of publication, country, topic investigated, HCW category involved, sample size, age (mean± SD), sex (% female), physical/mental health, data source, quality assessment (see below) and key findings.
2.4. Risk of bias (quality) assessment
Risk of bias was assessed using a modified version of the Mixed Methods Appraisal Tool (MMAT) as per protocol (detailed in eMethods 1). MMAT is considered the best and most comprehensive tool available for appraising multi-method studies (Behghadami et al., 2019).
2.5. Strategy for data synthesis
First, we provided a systematic synthesis (reported in the supplementary material) of the findings from the included studies structured around physical/mental health outcomes, and type of coronavirus syndromes (MERS vs SARS vs COVID-19). Second, we performed meta-analyses using, as primary effect size, the proportion (% and SE) of physical or mental health outcomes in HCW with a SARS/MERS/COVID-19 infection or exposed to SARS/MERS/COVID-19 (for details on the definition of the infection/exposure status see eMethods 2). The meta-analyses were split across physical and mental health outcomes—as operationalised by each individual study—and included both pooled and stratified estimates across SARS vs MERS vs COVID-19. Heterogeneity among studies was assessed using the Q statistic, with the proportion of the total variability in effect size estimates evaluated using the I² index (with an I2>50% representing significant heterogeneity) (Lipsey and Wilson, 2000). Random-effect models were employed as heterogeneity was expected to be high (DerSimonian and Laird, 1986). Publication biases were not assessed because studies included in proportion meta-analyses are non-comparative; thus, there are no "negative" or "undesirable" results or study characteristics like significant levels that may have biased publications (Maulik et al., 2011). We further conducted meta-analytical regression analyses (when data were available) to estimate the association between the analysed outcomes and: (i) sex, (ii) age, (iii) study quality, (iv) professional category (physicians vs nurses vs multi-professional samples) and (v) data source (self-administered questionnaires/surveys vs interviews/evaluations). All analyses were conducted using Comprehensive Meta-Analysis (CMA) V3 (Borenstein et al., 2013).
3. Results
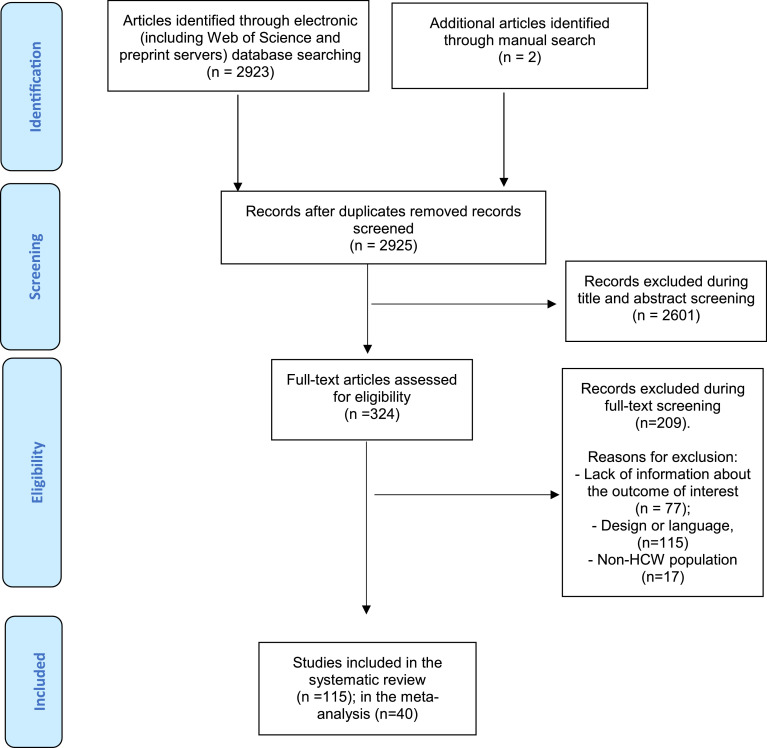
The literature search yielded 2,925 citations (2,923 through electronic database searching and 2 through manual search), which were screened for eligibility; 324 articles were assessed in full text, and 209 were excluded (reasons for exclusion are detailed in eTable III). The final database for the systematic included 115 studies (Fig. 1 ): 65 (56.5%) focused on SARS, 26 (22.6%) on MERS and 24 (20.9%) on COVID-19; 11 (9.6%) were qualitative studies, 3 (2.6%) non-randomised interventional studies and 101 (87.8%) quantitative studies. The full database included 60,458 HCW (35,905 SARS; 5,246 MERS; 19,307 COVID-19). The total sample size of the included studies ranged from 7 (Almutairi et al., 2018; Memish et al., 2013) to 10,511 (Koh et al., 2005) HCW (eTable IV-VI). The mean age of the sample was 36.1±7.1 years ranging from 23 (Wong et al., 2004b) to 69.4 (Ran et al., 2020) years; 77.1% were female. 90 (78.3%) studies included HCW from Asia, 18 (15.7%) HCW from America, 4 (3.5%) from Europe and 3% (2.6%) from more than one continent. In 64 (55.7%) studies, HCW completed self-administered questionnaires/surveys; in 51 (44.3%) studies, HCW were evaluated or interviewed by a professional. Most studies (85; 73.9%) investigated more than one HCW category; 19 studies (16.5%) focused on nurses, 9 (7.8%) on physicians, 1 (0.9%) on medical students and 1 (0.9%) on social workers. Forty studies were included in the meta-analysis (Fig. 1), focusing on physical health outcomes in HCW infected by SARS/MERS/COVID-19 and mental health outcomes in HCW exposed to SARS/MERS/COVID-19 (see eTables IV-VI).
Fig. 1.
PRISMA 2009 Flow Diagram.
3.1. Physical health outcomes in HCW with SARS/MERS/COVID-19 infection
The top 10 most frequently reported physical health symptoms in those with SARS/MERS/COVID-19 infection are displayed in Table 1 , Fig. 2 and systematically described in the eTables IV-VI. The meta-analysis revealed that 75.9% of HCW with SARS/MERS/COVID-19 infection reported fever (95%CI=65.9–83.7%, k=12, n=949), 47.9% cough (95%CI=39.2–56.8%, k=14, n=970), 43.6% myalgias (95%CI=31.9–56.0%, k=13, n=898), 42.3% chills (95%CI=20.2–67.9%, k=7, n=716), 41.2% fatigue (95%CI=18.2–68.8%, k=6, n=386), 34.6% headaches (95%CI=23.1–48.2%, k=11, n=893), 31.2% dyspnoea (95%CI=23.2–40.5%, k=12, n=1003), 25.3% sore throat (95%CI=18.8–33.2%, k=8, n=747), 22.2% nausea/vomiting (95%CI=14.9–31.8%, k=6, n=662) and 18.8% diarrhoea (95%CI=11.9–28.4%, k=9, n=824) (Table 1, Fig. 2). Heterogeneity was statistically significant (I2=70.9–95.9%) and sensitivity analyses revealed that chills, fatigue and sore throat were more frequent (p<0.001, p<0.001, p=0.018 respectively) in SARS (73.8%, 80.0%, 28.7% respectively) compared to MERS (30.0%, 25.6%, 24.5% respectively) and COVID-19 (4.5%, 38.0%, 20.7% respectively, Table 1, Fig. 2).
Table 1.
Meta-analytical proportion of physical health outcomes in HCW with SARS/MERS/COVID-19 infection.
| Symptom | Group | No. of studies | Sample size | Random effects model |
z Score | P | Test for Heterogeneity |
Between-group heterogeneity |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proportion | 95 % CI | Q | I2 | P | Q | P | |||||||
| Chills | Any coronavirus | 7 | 716 | 0.423 | 0.202 | 0.679 | −0.573 | 0.566 | 149.675 | 95.991 | <0.001 | 46.067 | <0.001 |
| SARS | 4 | 315 | 0.738 | 0.560 | 0.862 | 2.558 | 0.011 | 16.363 | 81.666 | 0.001 | |||
| MERS | 1 | 283 | 0.300 | 0.249 | 0.356 | −4.521 | <0.001 | <0.001 | <0.001 | 1.000 | |||
| COVID-19 | 2 | 118 | 0.045 | 0.019 | 0.101 | −6.832 | <0.001 | 0.117 | <0.001 | 0.733 | |||
| Cough | Any coronavirus | 14 | 970 | 0.479 | 0.392 | 0.568 | −0.452 | 0.651 | 72.720 | 82.125 | <0.001 | 2.803 | 0.246 |
| SARS | 5 | 329 | 0.368 | 0.234 | 0.527 | −1.635 | 0.102 | 20.764 | 80.736 | <0.001 | |||
| MERS | 4 | 341 | 0.487 | 0.271 | 0.708 | −0.111 | 0.912 | 15.340 | 80.443 | 0.002 | |||
| COVID-19 | 5 | 300 | 0.562 | 0.397 | 0.715 | 0.732 | 0.464 | 29.397 | 86.393 | <0.001 | |||
| Diarrhoea | Any coronavirus | 9 | 824 | 0.188 | 0.119 | 0.284 | −5.332 | <0.001 | 59.340 | 86.518 | <0.001 | 4.814 | 0.090 |
| SARS | 2 | 209 | 0.274 | 0.083 | 0.610 | −1.343 | 0.179 | 3.895 | 74.326 | 0.048 | |||
| MERS | 2 | 315 | 0.306 | 0.197 | 0.443 | −2.724 | 0.006 | 2.147 | 53.433 | 0.143 | |||
| COVID-19 | 5 | 300 | 0.120 | 0.054 | 0.247 | −4.441 | <0.001 | 20.664 | 80.642 | <0.001 | |||
| Dyspnoea | Any coronavirus | 12 | 1003 | 0.312 | 0.232 | 0.405 | −3.806 | <0.001 | 66.182 | 83.379 | <0.001 | 5.117 | 0.077 |
| SARS | 4 | 313 | 0.330 | 0.171 | 0.542 | −1.582 | 0.114 | 19.851 | 84.888 | <0.001 | |||
| MERS | 3 | 322 | 0.538 | 0.262 | 0.793 | 0.250 | 0.803 | 15.307 | 86.934 | <0.001 | |||
| COVID-19 | 5 | 368 | 0.202 | 0.114 | 0.331 | −4.009 | <0.001 | 21.753 | 81.612 | <0.001 | |||
| Fatigue | Any coronavirus | 6 | 386 | 0.412 | 0.182 | 0.688 | −0.609 | 0.543 | 96.695 | 94.829 | <0.001 | 48.167 | <0.001 |
| SARS | 1 | 193 | 0.800 | 0.738 | 0.851 | 7.704 | <0.001 | <0.001 | <0.001 | 1.000 | |||
| MERS | 2 | 51 | 0.256 | 0.155 | 0.393 | −3.305 | 0.001 | 0.315 | <0.001 | 0.575 | |||
| COVID-19 | 3 | 142 | 0.380 | 0.153 | 0.674 | −0.789 | 0.430 | 18.582 | 89.237 | <0.001 | |||
| Fever | Any coronavirus | 12 | 949 | 0.759 | 0.659 | 0.837 | 4.595 | <0.001 | 71.019 | 84.511 | <0.001 | 4.716 | 0.095 |
| SARS | 4 | 315 | 0.963 | 0.763 | 0.995 | 3.056 | 0.002 | 12.166 | 75.341 | 0.007 | |||
| MERS | 3 | 334 | 0.671 | 0.342 | 0.889 | 1.021 | 0.307 | 15.716 | 87.274 | <0.001 | |||
| COVID-19 | 5 | 300 | 0.714 | 0.576 | 0.820 | 2.959 | 0.003 | 20.445 | 80.435 | <0.001 | |||
| Headaches | Any coronavirus | 11 | 893 | 0.346 | 0.231 | 0.482 | −2.211 | 0.027 | 118.565 | 91.566 | <0.001 | 2.933 | 0.231 |
| SARS | 4 | 313 | 0.518 | 0.307 | 0.723 | 0.160 | 0.873 | 26.797 | 88.805 | <0.001 | |||
| MERS | 3 | 334 | 0.274 | 0.077 | 0.629 | −1.271 | 0.204 | 21.756 | 90.807 | <0.001 | |||
| COVID-19 | 4 | 246 | 0.232 | 0.071 | 0.545 | −1.704 | 0.088 | 47.147 | 93.637 | <0.001 | |||
| Myalgias | Any coronavirus | 13 | 898 | 0.436 | 0.319 | 0.560 | −1.013 | 0.311 | 106.415 | 88.723 | <0.001 | 40.447 | <0.001 |
| SARS | 5 | 329 | 0.633 | 0.542 | 0.716 | 2.826 | 0.005 | 7.636 | 47.613 | 0.106 | |||
| MERS | 4 | 341 | 0.409 | 0.193 | 0.667 | −0.676 | 0.499 | 23.126 | 87.027 | <0.001 | |||
| COVID-19 | 4 | 228 | 0.178 | 0.042 | 0.515 | −1.885 | 0.059 | 48.198 | 93.776 | <0.001 | |||
| Nausea/ vomits | Any coronavirus | 6 | 662 | 0.222 | 0.149 | 0.318 | −5.030 | <0.001 | 22.105 | 77.380 | 0.001 | 1.896 | 0.387 |
| SARS | 2 | 207 | 0.276 | 0.219 | 0.341 | −6.198 | <0.001 | 0.282 | <0.001 | 0.595 | |||
| MERS | 2 | 315 | 0.283 | 0.151 | 0.467 | −2.283 | 0.022 | 3.234 | 69.083 | 0.072 | |||
| COVID-19 | 2 | 140 | 0.071 | 0.008 | 0.428 | −2.211 | 0.027 | 5.170 | 80.657 | 0.023 | |||
| Sore throat | Any coronavirus | 8 | 747 | 0.253 | 0.188 | 0.332 | −5.539 | <0.001 | 24.034 | 70.874 | 0.001 | 8.075 | 0.018 |
| SARS | 2 | 209 | 0.287 | 0.117 | 0.549 | −1.613 | 0.107 | 4.584 | 78.187 | 0.032 | |||
| MERS | 3 | 334 | 0.245 | 0.202 | 0.294 | −8.825 | <0.001 | 0.618 | <0.001 | 0.734 | |||
| COVID-19 | 3 | 204 | 0.207 | 0.079 | 0.443 | −2.365 | 0.018 | 14.175 | 85.890 | 0.001 | |||
COVID-19: novel coronavirus 19; MERS: Middle East Respiratory Syndrome; SARS: Severe Acute Respiratory Syndrome.
Fig. 2.
Top 10 Most frequently reported physical health outcomes in HCW with SARS/MERS/COVID-19 infection.
3.2. Mental health outcomes in HCW exposed to SARS/MERS/COVID-19
The top 10 most frequently reported symptoms in SARS/MERS/COVID-19 are displayed in Table 2 , Fig. 3 ) and systematically described in the eTables IV-VI. The meta-analysis revealed that 62.5% HCW exposed to SARS/MERS/COVID-19 reported general health concerns (95%CI=57.0–67.8%, k=2, n=2254), 43.7% fear (95%CI=33.9–54.0%, k=4, n=584), 37.9% insomnia (95%CI=30.9–45.5%, k=6, n=5067), 37.8% psychological distress (95%CI=28.4–48.2%, k=15, n=24,346), 34.4% burnout (95%CI=19.3–53.5%, k=3, n=1337), 29.0% anxiety features (95%CI=14.2–50.3%, k=6, n=9191), 26.3% depressive symptoms (95%CI=12.5–47.1%, k=8, n=9893), 20.7%, post-traumatic stress disorder (PTSD) features (95%CI=13.2–31%, k=11, n=3826), 16.1% somatisation (95%CI=0.2–96.0%, k=2, n=2184) and 14.0% stigmatisation feelings (95%CI=6.4–28.1%, k=2, n=411) (Table 1, Fig. 2). Heterogeneity was substantial (I2=70.2–99.7%) and sensitivity analyses revealed that PTSD features were more frequent (p<0.001) in MERS (40.7%) than in SARS (16.7%) and COVID-19 (7.7%, Table 2, Fig. 3).
Table 2.
Meta-analytical proportion of mental health outcomes in HCW exposed to SARS/MERS/COVID-19
| Symptom | Group | No. of studies | Sample size | Random effects model |
z Score | P | Test for Heterogeneity |
Between-group heterogeneity |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proportion | 95 % CI | Q | I2 | P | Q | P | |||||||
| Psychological distress | Any coronavirus | 15 | 24346 | 0.378 | 0.284 | 0.482 | −2.293 | 0.022 | 2572.027 | 99.456 | <0.001 | 1.102 | 0.576 |
| SARS | 10 | 17144 | 0.409 | 0.293 | 0.536 | −1.406 | 0.160 | 1358.872 | 99.338 | <0.001 | |||
| MERS | 2 | 413 | 0.323 | 0.216 | 0.453 | −2.638 | 0.008 | 2.235 | 55.249 | 0.135 | |||
| COVID-19 | 3 | 6789 | 0.299 | 0.089 | 0.652 | −1.13 | 0.258 | 780.733 | 99.744 | <0.001 | |||
| Anxiety features | Any coronavirus | 6 | 9191 | 0.290 | 0.142 | 0.503 | −1.935 | 0.053 | 1318.346 | 99.621 | <0.001 | 0.557 | 0.456 |
| SARS | 2 | 1475 | 0.457 | 0.051 | 0.930 | −0.122 | 0.903 | 214.086 | 99.533 | <0.001 | |||
| COVID-19 | 4 | 7716 | 0.222 | 0.127 | 0.358 | −3.660 | <0.001 | 329.839 | 99.090 | <0.001 | |||
| PTSD features | Any coronavirus | 11 | 3826 | 0.207 | 0.132 | 0.310 | −4.851 | <0.001 | 390.38 | 97.438 | <0.001 | 22.741 | <0.001 |
| SARS | 7 | 2570 | 0.167 | 0.126 | 0.220 | −9.354 | <0.001 | 51.138 | 88.267 | <0.001 | |||
| MERS | 3 | 786 | 0.407 | 0.199 | 0.656 | −0.722 | 0.470 | 82.561 | 97.578 | <0.001 | |||
| COVID-19 | 1 | 470 | 0.077 | 0.056 | 0.105 | −14.355 | <0.001 | <0.001 | <0.001 | 1.000 | |||
| Depressive symptoms | Any coronavirus | 8 | 9893 | 0.263 | 0.125 | 0.471 | −2.212 | 0.027 | 1898.27 | 99.631 | <0.001 | 1.153 | 0.283 |
| SARS | 4 | 2177 | 0.368 | 0.126 | 0.701 | −0.761 | 0.447 | 478.474 | 99.373 | <0.001 | |||
| COVID-19 | 4 | 7716 | 0.179 | 0.067 | 0.401 | −2.659 | 0.008 | 791.154 | 99.621 | <0.001 | |||
| Insomnia | Any coronavirus | 6 | 5067 | 0.379 | 0.309 | 0.455 | −3.079 | 0.002 | 134.201 | 96.274 | <0.001 | 0.999 | 0.317 |
| SARS | 3 | 1577 | 0.295 | 0.107 | 0.593 | −1.369 | 0.171 | 102.890 | 98.056 | <0.001 | |||
| COVID-19 | 3 | 3490 | 0.445 | 0.382 | 0.509 | −1.685 | 0.092 | 29.322 | 93.179 | <0.001 | |||
| Burnout | Any coronavirus | 3 | 1337 | 0.344 | 0.193 | 0.535 | −1.61 | 0.107 | 67.959 | 97.057 | 0.000 | 0.964 | 0.326 |
| SARS | 2 | 1305 | 0.382 | 0.195 | 0.613 | −1.001 | 0.317 | 65.953 | 98.484 | <0.001 | |||
| COVID-19 | 1 | 32 | 0.250 | 0.130 | 0.426 | −2.691 | 0.007 | 0.000 | 1.000 | <0.001 | |||
| Stigmatisation feelings | Any coronavirus | 2 | 411 | 0.140 | 0.064 | 0.281 | −4.073 | 0.000 | 8.816 | 88.658 | 0.003 | N.a. | |
| SARS | 2 | 411 | 0.140 | 0.064 | 0.281 | −4.073 | 0.000 | 8.816 | 88.658 | 0.003 | |||
| Fear | Any coronavirus | 4 | 584 | 0.437 | 0.339 | 0.540 | −1.196 | 0.232 | 11.813 | 74.603 | 0.008 | 1.217 | 0.270 |
| SARS | 3 | 557 | 0.416 | 0.311 | 0.530 | −1.446 | 0.148 | 9.874 | 79.744 | 0.007 | |||
| MERS | 1 | 27 | 0.540 | 0.355 | 0.714 | 0.415 | 0.678 | <0.001 | <0.001 | 1.000 | |||
| General health concern | Any coronavirus | 2 | 2254 | 0.625 | 0.570 | 0.678 | 4.341 | 0.000 | 3.351 | 70.161 | 0.067 | N.a. | |
| SARS | 2 | 2254 | 0.625 | 0.570 | 0.678 | 4.341 | 0.000 | 3.351 | 70.161 | 0.067 | |||
| Somatisation | Any coronavirus | 2 | 2184 | 0.161 | 0.002 | 0.960 | −0.672 | 0.502 | 334.981 | 99.701 | <0.001 | N.a. | |
| SARS | 2 | 2184 | 0.161 | 0.002 | 0.960 | −0.672 | 0.502 | 334.981 | 99.701 | <0.001 | |||
COVID-19: novel coronavirus 19; MERS: Middle East Respiratory Syndrome; PTSD: post-traumatic stress disorder; SARS: Severe Acute Respiratory Syndrome.
Fig. 3.
Top 10 Most frequently reported mental health outcomes in HCW exposed to SARS/MERS/COVID-19.
3.3. Quality assessment and meta-regressions
The quality of the included studies was 3.2±0.9 and ranged from 1 to 5. This was 2.3±0.5 in non-randomised studies, 3.7±0.6 in qualitative studies and 3.2±0.9 in quantitative descriptive studies (eTables IV-VI). Female sex was associated with higher prevalence of myalgias (β=0.041, p=0.001) and sore throat (β=0.035, p=0.004) (eTable VII). Psychological distress was associated with female sex (β=0.032, p=0.002), younger age (β=-0.106, p<0.001), and professional category (β=-2.760, p<0.001): studies including nurses were associated to higher psychological distress than studies including only physicians (p<0.001) or including multi-professional samples (p<0.001) (eTable VIII). No other meta-regressions resulted significant.
4. Discussion
To the best of our knowledge, this is the first systematic review to have comprehensively addressed the impact of SARS/MERS/COVID-19 on both physical and mental health of HCW. With 115 individual studies and 60,458 individuals included and several outcomes investigated, this study demonstrated that SARS/MERS/COVID-19 have a substantial impact on HCW's physical and mental health.
This meta-analysis identified for the first time the most frequent physical health outcomes in HCW infected by SARS/MERS/COVID-19. Fever was the most frequent symptom in HCW (75.9%); it was more frequent in the general population with COVID-19 infection (meta-analyses: 85.6–88.7% (Hu et al., 2020; Li et al., 2020a; Rodriguez-Morales et al., 2020; Zhu et al., 2020)) and similarly frequent in the general population with MERS infection (meta-analysis: 77% (Badawi and Ryoo, 2016)). Cough appeared slightly less frequently in HCW (47.9%) than in the general population with COVID-19 infections (meta-analyses: 57.6–68.6% (Hu et al., 2020; Li et al., 2020a; Rodriguez-Morales et al., 2020; Zhu et al., 2020)). Conversely, myalgias in HCW (43.6%) were more frequent than in the general population with COVID-19 infections (meta-analyses: myalgia/fatigue=35.8% (Li et al., 2020a); muscle soreness=33% (Zhu et al., 2020)). Our sensitivity analyses found that chills (42.3% across all SARS/MERS/COVID-19) were more frequent in HCW with SARS (73.8%) than MERS (30.0%) and particularly COVID-19 (4.5%) infection; frequency of chills in HCW with SARS infection was comparable to the general population (SARS: 74.0–75.5% (Liu et al., 2003; Tiwari et al., 2003)). Frequency of fatigue in HCW (41.2%) was also comparable to the general population with COVID-19 infection (meta-analyses: 42.4–46.1% (Hu et al., 2020; Zhu et al., 2020)). Furthermore, in the general population, fatigue appears more frequently in SARS (60-70% (Huo et al., 2003; Xu et al., 2003)) than in COVID-19 (meta-analyses: 42.4–46.1% (Hu et al., 2020; Zhu et al., 2020)), in line with our sensitivity analyses (fatigue in HCW: SARS=80.0%, MERS=25.6%, COVID-19=38.0%). Frequency of dyspnoea in HCW (31.2%) was comparable (Hu et al., 2020; Li et al., 2020a; Rodriguez-Morales et al., 2020; Zhu et al., 2020) to the general population with COVID-19 infection (meta-analyses: 21.4–45.6% (Hu et al., 2020; Rodriguez-Morales et al., 2020; Zhu et al., 2020)) but lower than in the general population with MERS infection (meta-analysis: 68% (Badawi and Ryoo, 2016)). Frequency of headaches (34.6%), nausea/vomiting (22.2%) and diarrhoea (18.8%) in HCW were as frequent as in the general population with COVID-19 infection (meta-analyses: headaches=8–15.4% (Rodriguez-Morales et al., 2020; Zhu et al., 2020); nausea/vomiting=3.9–10.2% (Li et al., 2020a; Zhu et al., 2020); diarrhoea=4.8-12.9% (Cheung et al., 2020; Li et al., 2020a; Rodriguez-Morales et al., 2020; Zhu et al., 2020)). Frequency of sore throat (25.3%) was similar between HCW and the general population infected by COVID-19 (meta-analysis: 11.0–21.9% (Li et al., 2020a; Rodriguez-Morales et al., 2020)), but lower than in the general population affected with MERS (meta-analysis: 39% (Badawi and Ryoo, 2016)). However, while our sensitivity analyses found a higher prevalence of sore throat in HCW with SARS (28.7%) compared to COVID-19 infection (20.7%), this effect was not observed in the general population (SARS: 13–25% (Hui et al., 2003), COVID-19 11.0–21.9% (Li et al., 2020a; Rodriguez-Morales et al., 2020)).
Whether these differences are due to differential reporting of symptoms by HCW or by a specific clinical course of these syndromes remains unclear. However, since the meta-regressions revealed that findings were not affected by the type of data source, it is possible to speculate that differences in the frequency of symptoms may characterise specific clinical manifestations of SARS/MERS/COVID-19 in HCW. The repeated exposure to high viral loads from contaminated patients (Liu et al., 2020) can interact with high environmental stress—which is known to affect the immune system (Troyer et al., 2020)—and theoretically account for some of these findings. Overall, the impact of SARS/MERS/COVID-19 infection on the physical health of HCW is profound, to the point that it has been identified as the most common cause of death for physicians during the outbreak (Li et al., 2020b), particularly general practitioners and emergency department physicians (Ing et al., 2020).
This is also the first meta-analysis that is specifically addressing mental health outcomes in HCW exposed to SARS/MERS/COVID-19. As global public health concerns, general health concerns represent the most frequent issue in HCW (62.5% according to our results) and a main topic in the general population (Hamid et al., 2020; Nickell et al., 2004; Paudel et al., 2020). In some vulnerable groups as pregnant women, general health concerns cumulate to 94.6% (Du et al., 2020). General health concerns are typically high when the outbreak starts (80.3%), intensify even further over its course (up to 88.6%) and decline (75.4%) once the acute phase has resolved (Ro et al., 2017). During pandemics/epidemics, fear of contracting coronaviruses has often been associated with psychological distress (Shacham et al., 2020). Accordingly, fear (43.7%) was the second most frequent mental health issue in HCW, although less common than in the general population during SARS epidemic (individual studies: 60–70% (Bener and Al-Khal, 2004; Chen et al., 2004; Yip et al., 2007)), possibly because of higher health literacy in HCW (Al Sayah et al., 2013). While the frequency of psychological distress in HCW (37.8%) was similar to that observed in the general population (SARS:39% (DiGiovanni et al., 2004)), our meta-regression analyses found that psychological distress was particularly common in HCW subgroups (see below). Frequency of poor sleep during a COVID-19 outbreak was 18.2% in the general population (Huang and Zhao, 2020), about half of what we observed in HCW (37.9%). This may be due to long shifts and working hours that typically characterise HCW's clinical duties during epidemics/pandemics (Puliatti et al., 2020). A frequently associated feature was burnout—already high in ordinary times for HCW (Adriaenssens et al., 2015)—which peaked to 34.4% in HCW exposed to SARS/MERS/COVID-19; burnout is reported to be particularly high in nurses working long hours with MERS patients (Kim and Choi, 2016). Level of burnout is hardly ever reported or evaluated in the general population, but it has been related to physical distance from the epicentre of pandemic/epidemic outbreaks, with an inverted U-shaped relationship (Zhang et al., 2020a). Our meta-analysis also showed a higher frequency of anxiety (29.0%) and depressive (26.3%) features in HCW compared to the general population with SARS/MERS infection (meta-analyses: depression=15% (Rogers et al., 2020); anxiety disorders=14.8% (Rogers et al., 2020)), although the current meta-analysis was not restricted to categorical diagnoses. Furthermore, the SARS outbreak has resulted in historically high suicide rates in the general population (Cheung et al., 2008; Yip et al., 2010); suicide cases related to COVID-19 have been already reported, also in HCW (Jun et al., 2020). However, it is not known how risk of suicide is in HCW compared to the general population.
Although the frequency of PTSD features in HCW exposed to SARS/MERS/COVID-19 appeared lower (20.7%) than in the general population with SARS/MERS infection (meta-analysis: PTSD=32.5% (Rogers et al., 2020)), PTSD symptoms usually appear months after the traumatic experience, and it may be too early in the case of COVID-19 pandemic. In fact, mental health in SARS was found to be more impaired in the phase following the acute outbreak than in the initial phase (Chong et al., 2004). Future research should evaluate a potential increase in PTSD symptoms in HCW exposed to COVID-19 after the present study. An alternative explanation is that HCW may have fewer risk factors for PTSD, such as a history of physical diseases or a family history of psychiatric disorders (Tortella-Feliu et al., 2019). Our sensitivity analyses showed that— among HCW— PTSD features were more frequent in MERS (40.7%) than in SARS (16.7%) and COVID-19 (7.7%); this could relate to the higher levels of trauma associated with the overall higher mortality rates of MERS (Ahmed, 2017) in the general population (MERS=35% (Yan et al., 2020)-41% (Ahmed, 2017); SARS 9.6% (Yan et al., 2020)- 21% (Chang et al., 2020); COVID-19 2% (Yan et al., 2020)-5% (Li et al., 2020a)). HCW also experience higher levels of somatisation (16.1%) than the general population (0.4%) (Zhang et al., 2020b). Finally, 14.0% of HCW reported having stigmatisation feelings, albeit less frequently than the general population (39.5%) (DiGiovanni et al., 2004); some HCW expressed that people avoided not only them, due to their job, but also their families (Koh et al., 2005).
Overall, the findings of the current study may have some clinical implications. First, they clearly confirm that HCW are as essential as a fragile population which is put under high physical and mental health burden during SARS/MERS/COVID-19. Although HCW´s dedication and commitment outweigh the risk and their willingness to fight SARS/MERS/COVID-19 (Aldrees et al., 2017; Hussein, 2004; Imai et al., 2005), HCW recognise to be at risk, mostly because of the lack of personal protective equipment (Iacobucci, 2020), high working pressure (Bai et al., 2020; Lung et al., 2009; Shih et al., 2007) and suboptimal training/confidence when working in extreme circumstances (Hsu et al., 2006). Second, these findings inform the detection and recognition of core physical and mental health outcomes in HCW during SARS/MERS/COVID-19 epidemics/pandemics. Given the logistic challenges of conducting research during infective outbreaks, focusing on the most frequent outcomes that are reported in HCW may represent a pragmatic advantage. For example, the vast majority of HCW (77%) were females, and our meta-regressions demonstrated that female HCW were more frequently displaying myalgias and sore throat, while young HCW, females and nurses were particularly vulnerable to SARS/MERS/COVID-19-related psychological distress. These findings can be used to develop gender/age- (or professional group-) sensitive guidelines for recognising the physical and mental health burden of these syndromes. In fact, some professional bodies are already developing specific recommendations for vulnerable categories such as pregnant HCW women (who are at risk of complications themselves and their neonates (Khan et al., 2020)), older HCW or HCW with a history of chronic diseases (Kowalski et al., 2020). While the physical health of HCW is more frequently monitored, the current findings may guide healthcare providers and policymakers to implement systematic screenings for HCW's mental health. Third, the current findings can be used to design or refine preventive approaches. Services for individuals at Clinical High Risk for Psychosis (Fusar-Poli et al., 2020; Kotlicka-Antczak et al., 2020; Salazar de Pablo et al., 2019) may leverage our findings to refine preventive approaches. For example, there is emerging evidence that Covid-19 may increase the incidence of short-lived psychotic episodes (Anmella et al., 2020; Valdés-Florido et al., 2020; Zulkifli et al., 2020) also termed as brief and limited intermittent psychotic symptoms (Castagnini and Fusar-Poli, 2017; Fusar-Poli et al., 2016; Fusar-Poli et al., 2017; Fusar-Poli et al., 2019; Minichino et al., 2019; Rutigliano et al., 2018). Our review found that HCW presented with full-blown disorders as acute stress disorder (Bai et al., 2004) or PTSD (Lee et al., 2018). Outside HCW, severe mental disorders have been detected after coronavirus syndromes (Rogers et al., 2020). This evidence suggests that monitoring for emerging mental disorders should become a cornerstone of preventive care during pandemics. Preventive approaches may include education programmes targeting HCW to inform them about their risk of developing specific physical/mental health outcomes while providing direct or indirect care to SARS/MERS/COVID-19 patients. HCW may be particularly reluctant to disclose their problems (Chen et al., 2020; Shanafelt et al., 2020) to minimise the burden on their relatives (Chen et al., 2020) or because they over consider themselves self-reliant (Shanafelt et al., 2020). Because the current study concurrently appraises both physical and mental health outcomes, it is particularly suited to inform cross-cutting approaches such as interventions designed to enhance resilience and therefore impact both physical and mental health (Maunder et al., 2008). It may be possible to screen those HCW at a high risk of developing psychiatric disorders using instruments that have been validated to detect emerging severe mental disorders (Fusar-Poli et al., 2020), such as the Comprehensive Assessment of At Risk Mental States (Yung et al., 2005), the Structured Interview for Bipolar At Risk States (Fusar-Poli et al., 2018) and the PredictD (King et al., 2008). New screening instruments are being validated to identify individuals with mental health concerns in the general population with specific reference to the current COVID-19 pandemic (Lee, 2020). These approaches could be extended to all categories which this review found to be impacted by SARS/MERS/COVID-19: physicians (Grace et al., 2005), nurses (Su et al., 2007), health care assistants (Poon et al., 2004), students (Wong et al., 2004a), social workers (Gearing et al., 2007) and trainees (Rambaldini et al., 2005). Fourth, the current findings can serve as real-world targets to inform the development of effective treatments for restoring the impaired physical health and mental health of HCW, which are currently limited. Globally, substantial research investments are being deployed to establish effective treatments for physical and mental health outcomes in HCW, in particular leveraging the potential of eHealth and telemedicine during epidemics/pandemics (Moazzami et al., 2020; Whaibeh et al., 2020; Williamson et al., 2020).
This study has several limitations. First, despite our comprehensive approach, there was a limited amount of evidence to provide stratified results for the proportion of stigma, general health concern and somatisation in HCW exposed to MERS or COVID-19. Also, some emerging symptoms that have only recently been detected in the general population such as anosmia were not extensively reported in HCW, thus preventing their inclusion in the current meta-analysis. Second, heterogeneity was substantial in the evaluated outcomes. We conducted meta-analytical regression analyses to evaluate the influence of several variables on our results. Third, despite our meta-regressions, we were unable to quantify the impact of ethnic, clinical and treatment factors, or healthcare system differences, which may act as confounding factors. Forth, HCW exposed to SARS/MERS/COVID-19 may also have been infected but be asymptomatic, and infection status may have gone unnoticed by researchers. Also, it may not have been possible to detect all the symptoms that appeared in HCW. These are intrinsic limitations of the underlying primary research. Fifth, we excluded studies not published in English. This may have resulted in the exclusion of some studies, particularly from Asian countries. However, we were able to detect 115 individual studies with our approach, 90 of which were conducted in Asia. Sixth, the main symptoms of SARS in general population have not been subjected to a comprehensive meta-analysis, limiting comparative analyses with our results. Finally, because of the challenges in conducting research during a pandemic, several studies had a suboptimal design; the data source was controlled in meta-regression analyses revealing no impact on the results.
5. Conclusions
SARS/MERS/COVID-19 have a substantial impact on the physical and mental health of HCW, which should become a priority for public health strategies.
Declaration of Competing Interest
Dr Catalan has received personal fees from Janssen. Dr Fusar-Poli has received grants from Lundbeck and personal fees from Lundbeck, Menarini and Angelini. Dr Arango has been a consultant to or has received honoraria or grants from Acadia, Angelini, Gedeon Richter, Janssen Cilag, Lundbeck, Otsuka, Roche, Sage, Servier, Shire, Schering Plough, Sumitomo Dainippon Pharma, Sunovion and Takeda. Dr Moreno has acted as consultant or participated in DMC for Janssen, Servier, Lundbeck, Nuvelution, Angelini and Otsuka.
Acknowledgments
Funding/Support
Dr Salazar de Pablo and Dr. Vaquerizo-Serrano are supported by the Alicia Koplowitz Foundation. Dr Arango and Dr Moreno have been supported by the Spanish Ministry of Science and Innovation. Instituto de Salud Carlos III (SAM16PE07CP1, PI16/02012, PI19/024), co-financed by ERDF Funds from the European Commission, “A way of making Europe”, CIBERSAM. Madrid Regional Government (B2017/BMD-3740 AGES-CM-2), European Union Structural Funds. European Union Seventh Framework Program under grant agreements FP7-4-HEALTH-2009-2.2.1-2-241909 (Project EU-GEI), FP7- HEALTH-2013-2.2.1-2-603196 (Project PSYSCAN) and FP7- HEALTH-2013-2.2.1-2-602478 (Project METSY); and European Union H2020 Program under the Innovative Medicines Initiative 2 Joint Undertaking (grant agreement No 115916, Project PRISM, and grant agreement No 777394, Project AIMS-2-TRIALS), Fundación Familia Alonso, and Fundación Alicia Koplowitz and Fundación Mutua Madrileña. Dr Fusar-Poli is supported by the PSYSCAN project through the European Commission.
Acknowledgments
We are grateful to Dr Julia de Pablo (Gros Health Centre, Osakidetza-Basque Health Service, San Sebastián, Spain) and Dr Paula Martinez-Pascual (Department of ENT, Hospital General Gregorio Marañón, Madrid, Spain) for their external advice on the diagnosis of coronavirus syndromes and the physical impact on healthcare workers.
Contributions
Dr Salazar de Pablo had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; Study concept and design: Salazar de Pablo, Fusar-Poli; Acquisition of data: Salazar de Pablo, Vaquerizo-Serrano, Catalan, Fusar-Poli; Statistical analysis: Salazar de Pablo, Fusar-Poli; Interpretation of data: All authors; Drafting of the manuscript: Salazar de Pablo, Fusar-Poli. Administrative, technical, or material support: Fusar-Poli. Critical revision of the manuscript for important intellectual content: All authors.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.06.022.
Appendix. Supplementary materials
References
- Adriaenssens J., De Gucht V., Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int. J. Nurs. Stud. 2015;52:649–661. doi: 10.1016/j.ijnurstu.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Ahmed A.E. The predictors of 3-and 30-day mortality in 660 MERS-CoV patients. BMC Infect. Dis. 2017;17 doi: 10.1186/s12879-017-2712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Sayah F., Majumdar S.R., Williams B., Robertson S., Johnson J.A. Health literacy and health outcomes in diabetes: a systematic review. J. Gen. Intern. Med. 2013;28:444–452. doi: 10.1007/s11606-012-2241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldrees T., Al Ghobain M., Alenezi A., Alqaryan S., Aldabeeb D., Alotaibi N., Alzahrani K., Alharethy S. Medical residents' attitudes and emotions related to Middle East respiratory syndrome in Saudi Arabia A cross-sectional study. Saudi Med. J. 2017;38:942–947. doi: 10.15537/smj.2017.9.20626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almutairi A.F., Adlan A.A., Balkhy H.H., Abbas O.A., Clark A.M. Exploring the experiences of healthcare providers who survived MERS-CoV in Saudi Arabia. J. Infect. Public Health. 2018;11:187–191. doi: 10.1016/j.jiph.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman D.G., Simera I., Hoey J., Moher D., Schulz K. EQUATOR: reporting guidelines for health research. Lancet. 2008;371:1149–1150. doi: 10.1016/S0140-6736(08)60505-X. [DOI] [PubMed] [Google Scholar]
- Anmella G., Fico G., Roca A., Gómez M., Vázquez M., Murru A., Pacchiarotti I., Verdolini N., Vieta E. Unravelling potential severe psychiatric repercussions on healthcare professionals during the COVID-19 crisis. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int. J. Infect. Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai Y., Lin C.C., Lin C.Y., Chen J.Y., Chue C.M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004;55:1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- Bai, Y., Wang, X., Huang, Q., Wang, H., Gurarie, D., Ndeffo-Mbah, M., Fan, F., Fu, P., Horn, M., Xu, S., Mondal, A., Juang, X., Zhao, H., 2020. SARS-CoV-2 infection in health care workers: a retrospective analysis and a model study, medRxiv. [DOI] [PMC free article] [PubMed]
- Behghadami M.A., Janati A., Sadeghi-Bazargani H., Gholizadeh M., Rahmani F., Arab-Zozani M. Assessing preparedness of non-hospital health centers to provide primary emergency care; a systematic review. Bull. Emerg. Trauma. 2019;7:201–211. doi: 10.29252/beat-070301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bener A., Al-Khal A. Knowledge, attitude and practice towards SARS. J. R. Soc. Promot. Health. 2004;124:167–170. doi: 10.1177/146642400412400408. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L., Higgins J., Rothstein H. In: Biostat E., editor. 2013. Version 3. Version 3NJ. [Google Scholar]
- Castagnini A.C., Fusar-Poli P. Diagnostic validity of ICD-10 acute and transient psychotic disorders and DSM-5 brief psychotic disorder. Eur. Psychiatry. 2017;45:104–113. doi: 10.1016/j.eurpsy.2017.05.028. [DOI] [PubMed] [Google Scholar]
- Chang D., Xu H., Rebaza A., Sharma L., Dela Cruz C.S. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir. Med. 2020;8:E13. doi: 10.1016/S2213-2600(20)30066-7. -E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staffs anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43:215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.M., Perng R.P., Chu H., Tsai C.M., Whang-Peng J. Impact of severe acute respiratory syndrome on the status of lung cancer chemotherapy patients and a correlation of the signs and symptoms. Lung Cancer. 2004;45:39–43. doi: 10.1016/j.lungcan.2004.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung K.S., Hung I.F., Chan P.P., Lung K.C., Tso E., Liu R., Ng Y.Y., Chu M.Y., Chung T.W., Tam A.R., Yip C.C., Leung K.H., Yim-Fong Fung A., Zhang R.R., Lin Y., Cheng H.M., Zhang A.J., To K.K., Chan K.H., Yuen K.Y., Leung W.K. Gastrointestinal Manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C., Huang T.L., Wen J.K., Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Christian M.D., Loutfy M., McDonald C., Martinez K.F., Ofner M., Wong T., Wallington T., Gold W.L., Mederski B., Green K., Low D.E., Team S.I. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg. Infect. Dis. 2004;10:287–293. doi: 10.3201/eid1002.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- DiGiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterror. 2004;2:265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- Du L., Gu Y.B., Cui M.Q., Li W.X., Wang J., Zhu L.P., Xu B. Investigation on demands for antenatal care services among 2 002 pregnant women during the epidemic of COVID-19 in Shanghai. Zhonghua Fu Chan Ke Za Zhi. 2020;55:160–165. doi: 10.3760/cma.j.cn112141-20200218-00112. [DOI] [PubMed] [Google Scholar]
- Ehrlich H., McKenney M., Elkbuli A. Protecting our healthcare workers during the COVID-19 pandemic. Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., Cappucciati M., Bonoldi I., Hui L.M.C., Rutigliano G., Stahl D.R., Borgwardt S., Politi P., Mishara A.L., Lawrie S.M., Carpenter W.T., McGuire P.K. Prognosis of brief psychotic episodes a meta-analysis. Jama Psychiatry. 2016;73:211–220. doi: 10.1001/jamapsychiatry.2015.2313. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Cappucciati M., De Micheli A., Rutigliano G., Bonoldi I., Tognin S., Ramella-Cravaro V., Castagnini A., McGuire P. Diagnostic and prognostic significance of brief limited intermittent psychotic symptoms (BLIPS) in individuals at ultra high risk. Schizophr. Bull. 2017;43:48–56. doi: 10.1093/schbul/sbw151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., De Micheli A., Chalambrides M., Singh A., Augusto C., McGuire P. Unmet needs for treatment in 102 individuals with brief and limited intermittent psychotic symptoms (BLIPS): implications for current clinical recommendations. Epidemiol. Psychiatr. Sci. 2019;29:e67. doi: 10.1017/S2045796019000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., De Micheli A., Rocchetti M., Cappucciati M., Ramella-Cravaro V., Rutigliano G., Bonoldi I., McGuire P., Falkenberg I. Semistructured interview for bipolar at risk states (SIBARS) Psychiatry Res. 2018;264:302–309. doi: 10.1016/j.psychres.2018.03.074. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Salazar de Pablo G., Correll C.U., Meyer-Lindenberg A., Millan M.J., Borgwardt S., Galderisi S., Bechdolf A., Pfennig A., Kessing L.V., van Amelsvoort T., Nieman D.H., Domschke K., Krebs M.O., Koutsouleris N., McGuire P., Do K.Q., Arango C. Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2019.4779. [DOI] [PubMed] [Google Scholar]
- Gearing R.E., Saini M., McNeill T. Experiences and implications of social workers practicing in a pediatric hospital environment affected by SARS. Health Soc. Work. 2007;32:17–27. doi: 10.1093/hsw/32.1.17. [DOI] [PubMed] [Google Scholar]
- Grace S.L., Hershenfield K., Robertson E., Stewart D.E. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. 2005;46:385–391. doi: 10.1176/appi.psy.46.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamid S., Mir M.Y., Rohela G.K. Novel coronavirus disease (COVID-19): a pandemic (epidemiology, pathogenesis and potential therapeutics) New Microbes New Infect. 2020;35 doi: 10.1016/j.nmni.2020.100679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu C.-C., Chen T., Chang M., Chang Y.-K. Confidence in controlling a SARS outbreak: Experiences of public health nurses in managing home quarantine measures in Taiwan. Am. J. Infect. Control. 2006;34:176–181. doi: 10.1016/j.ajic.2005.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Sun J., Dai Z., Deng H., Li X., Huang Q., Wu Y., Sun L., Xu Y. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J. Clin. Virol. 2020;127 doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L., Lin G., Tang L., Yu L., Zhou Z. Special attention to nurses' protection during the COVID-19 epidemic. Critical Care. 2020;24 doi: 10.1186/s13054-020-2841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol. Health Med. 2020:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Hui D.S., Wong P.C., Wang C. SARS: clinical features and diagnosis. Respirology. 2003;8(Suppl):S20–S24. doi: 10.1046/j.1440-1843.2003.00520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huo N., Lu H., Xu X., Wang G., Li H., Li J., Wang J., Nie L., Gao X., Zhang Z., Li Y., Zhuang H. The clinical characteristics and outcome of 45 early stage patients with SARS. Beijing Da Xue Xue Bao Yi Xue Ban. 2003;35(Suppl):19–22. [PubMed] [Google Scholar]
- Hussein A. Guest Editorial: SARS - future considerations for nurses. J. Adv. Nurs. 2004;45:111–112. doi: 10.1111/j.1365-2648.2004.02907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci G. Covid-19: doctors still at "considerable risk" from lack of PPE, BMA warns. Bmj-Br. Med. J. 2020;368 doi: 10.1136/bmj.m1316. [DOI] [PubMed] [Google Scholar]
- Imai T., Takahashi K., Hoshuyama T., Hasegawa N., Lim M.K., Koh D. SARS risk perceptions in healthcare workers, Japan. Emerg. Infect. Dis. 2005;11:404–410. doi: 10.3201/eid1103.040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ing, E., Xu, A., A., S., Torun, N., 2020. Physician Deaths from Corona Virus Disease (COVID-19), medRxiv. [DOI] [PMC free article] [PubMed]
- Jun J., Tucker S., Melnyk B. Clinician mental health and well-being during global healthcare crises: evidence learned from prior epidemics for COVID-19 pandemic. Worldviews Evidence-based Nurs. 2020 doi: 10.1111/wvn.12439. [DOI] [PubMed] [Google Scholar]
- Khan S., Jun L., Nawsherwan, Siddique R., Li Y., Han G., Xue M., Nabi G., Liu J. Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women. Clin. Microbiol. Infect.: Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2020 doi: 10.1016/j.cmi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.S., Choi J.S. Factors Influencing emergency nurses' burnout during an outbreak of middle east respiratory syndrome coronavirus in Korea. Asian Nurs. Res. 2016;10:295–299. doi: 10.1016/j.anr.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M., Walker C., Levy G., Bottomley C., Royston P., Weich S., Bellón-Saameño J.A., Moreno B., Svab I., Rotar D., Rifel J., Maaroos H.I., Aluoja A., Kalda R., Neeleman J., Geerlings M.I., Xavier M., Carraça I., Gonçalves-Pereira M., Vicente B., Saldivia S., Melipillan R., Torres-Gonzalez F., Nazareth I. Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: the PredictD study. Arch. Gen. Psychiatry. 2008;65:1368–1376. doi: 10.1001/archpsyc.65.12.1368. [DOI] [PubMed] [Google Scholar]
- Koh D., Lim M.K., Chia S.E. SARS: health care work can be hazardous to health. Occup. Med.-Oxf. 2003;53:241–243. doi: 10.1093/occmed/kqg090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V., Tan B.H., Wong K.S., Chew W.M., Tang H.K., Ng W., Muttakin Z., Emmanuel S., Fong N.P., Koh G., Kwa C.T., Tan K.B.C., Fones C. Risk perception and impact of Severe Acute Respiratory Syndrome (SARS) on work and personal lives of healthcare workers in Singapore - What can we learn? Med. Care. 2005;43:676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- Kotlicka-Antczak M., Podgórski M., Oliver D., Maric N.P., Valmaggia L., Fusar-Poli P. Worldwide implementation of clinical services for the prevention of psychosis: The IEPA early intervention in mental health survey. Early Interv. Psychiatry. 2020 doi: 10.1111/eip.12950. [DOI] [PubMed] [Google Scholar]
- Kowalski L.P., Sanabria A., Ridge J.A., Ng W.T., de Bree R., Rinaldo A., Takes R.P., Makitie A.A., Carvalho A.L., Bradford C.R., Paleri V., Hartl D.M., Poorten V.V., Nixon I.J., Piazza C., Lacy P., Rodrigo J.P., Guntinas-Lichius O., Mendenhall W.M., D'Cruz A., Lee A.W.M., Ferlito A. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020 doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020:1–9. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.-R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comp. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B., Zhang H.Y., Sun W., Wang Y. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Zhang J., Xiao S., Sun L. Characteristics of health worker fatality in China during the outbreak of COVID-19 infection. J. Infect. 2020 doi: 10.1016/j.jinf.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey M., Wilson D. Sage Publications; Thousand Oaks, CA: 2000. Practical Meta-analysis. [Google Scholar]
- Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J., Wang Z., Li J., Feng C., Zhang Z., Wang L., Peng L., Chen L., Qin Y., Zhao D., Tan S., Yin L., Xu J., Zhou C., Jiang C., Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z.Y., Li T.S., Wang Z., Xu Z.J., Wang H.L., Yu Y., Du T.K., Bai Y., Qiu Z.F., Lü W., Fan H.W., Ma X.J., Zhou B.T., Wang A.X., Cai B.Q., Deng G.H., Ni A.P. Clinical features and therapy of 106 cases of severe acute respiratory syndrome. Zhonghua Nei Ke Za Zhi. 2003;42:373–377. [PubMed] [Google Scholar]
- Lung F.-W., Lu Y.-C., Chang Y.-Y., Shu B.-C. Mental symptoms in different health professionals during the SARS attack: a follow-up study. Psychiatr. Q. 2009;80:107–116. doi: 10.1007/s11126-009-9095-5. [DOI] [PubMed] [Google Scholar]
- Maulik P.K., Mascarenhas M.N., Mathers C.D., Dua T., Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res. Dev. Disab. 2011;32:419–436. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- Maunder R.G., Leszcz M., Savage D., Adam M.A., Peladeau N., Romano D., Rose M., Schulman R.B. Applying the lessons of SARS to pandemic influenza an evidence-based approach to mitigating the stress experienced by healthcare workers. Can. J. Public Health-Revue Can. Sante Publ. 2008;99:486–488. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish Z.A., Zumla A.I., Assiri A. Middle east respiratory syndrome coronavirus infections in health care workers. N Engl. J. Med. 2013;369:884–886. doi: 10.1056/NEJMc1308698. [DOI] [PubMed] [Google Scholar]
- Minichino A., Rutigliano G., Merlino S., Davies C., Oliver D., De Micheli A., Patel R., McGuire P., Fusar-Poli P. Unmet needs in patients with brief psychotic disorders: Too ill for clinical high risk services and not ill enough for first episode services. Eur. Psychiatry. 2019;57:26–32. doi: 10.1016/j.eurpsy.2018.12.006. [DOI] [PubMed] [Google Scholar]
- Moazzami B., Razavi-Khorasani N., Dooghaie Moghadam A., Farokhi E., Rezaei N. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J. Clin. Virol.: Off. Publ. Pan Am. Soc. Clin. Virol. 2020;126 doi: 10.1016/j.jcv.2020.104345. -104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam H.-S., Yeon M.-Y., Park J.W., Hong J.-Y., Son J.W. Healthcare worker infected with Middle East Respiratory Syndrome during cardiopulmonary resuscitation in Korea, 2015. Epidemiol. Health. 2017;39 doi: 10.4178/epih.e2017052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E.G. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Can. Med. Assoc. J. 2004;170:793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paudel S., Dangal G., Chalise A., Bhandari T.R., Dangal O. The coronavirus pandemic: what does the evidence show? J. Nepal Health Res. Council. 2020;18:1–9. doi: 10.33314/jnhrc.v18i1.2596. [DOI] [PubMed] [Google Scholar]
- Poon E., Liu K.S., Cheong D.L., Lee C.K., Yam L.Y.C., Tang W.N. Impact of severe respiratory syndrome on anxiety levels of front-line health care workers. Hong Kong Med. J. = Xianggang yi xue za zhi. 2004;10:325–330. [PubMed] [Google Scholar]
- Puliatti S., Eissa A., Eissa R., Amato M., Mazzone E., Dell'Oglio P., Sighinolfi M.C., Zoeir A., Micali S., Bianchi G., Patel V., Wiklund P., Coelho R.F., Bernhard J.-C., Dasgupta P., Mottrie A., Rocco B. COVID-19andUrology: a comprehensive review of the literature. BJU Int. 2020 doi: 10.1111/bju.15071. [DOI] [PubMed] [Google Scholar]
- Rambaldini G., Wilson K., Rath D., Lin Y.L., Gold W.L., Kapral M.K., Straus S.E. The impact of severe acute respiratory syndrome on medical house staff - A qualitative study. J. Gen. Internal Med. 2005;20:381–385. doi: 10.1111/j.1525-1497.2005.0099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran L., Chen X., Wang Y., Wu W., Zhang L., Tan X. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2020 doi: 10.1093/cid/ciaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro J.S., Lee J.S., Kang S.C., Jung H.M. Worry experienced during the 2015 Middle East Respiratory Syndrome (MERS) pandemic in Korea. PLoS One. 2017;12 doi: 10.1371/journal.pone.0173234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P., Alvarado-Arnez L.E., Bonilla-Aldana D.K., Franco-Paredes C., Henao-Martinez A.F., Paniz-Mondolfi A., Lagos-Grisales G.J., Ramírez-Vallejo E., Suárez J.A., Zambrano L.I., Villamil-Gómez W.E., Balbin-Ramon G.J., Rabaan A.A., Harapan H., Dhama K., Nishiura H., Kataoka H., Ahmad T., Sah R., https://www.lancovid.org, L.A.N.o.C.D.-C.-R.L.-E.a. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutigliano G., Merlino S., Minichino A., Patel R., Davies C., Oliver D., De Micheli A., McGuire P., Fusar-Poli P. Long term outcomes of acute and transient psychotic disorders: The missed opportunity of preventive interventions. Eur. Psychiatry. 2018;52:126–133. doi: 10.1016/j.eurpsy.2018.05.004. [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G., Catalan A., Fusar-Poli P. Clinical validity of DSM-5 attenuated psychosis syndrome: advances in diagnosis, prognosis, and treatment. JAMA Psychiatry. 2019 doi: 10.1001/jamapsychiatry.2019.3561. [DOI] [PubMed] [Google Scholar]
- Shacham M., Hamama-Raz Y., Kolerman R., Mijiritsky O., Ben-Ezra M., Mijiritsky E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17082900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah K., Kamrai D., Mekala H., Mann B., Desai K., Patel R.S. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12 doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Shih F.-J., Gau M.-L., Kao C.-C., Yang C.-Y., Lin Y.-S., Liao Y.-C., Sheu S.-J. Dying and caring on the edge: Taiwan's surviving nurses' reflections on taking care of patients with severe acute respiratory syndrome. Appl. Nurs. Res. 2007;20:171–180. doi: 10.1016/j.apnr.2006.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Su T.-P., Lien T.-C., Yang C.-Y., Su Y.L., Wang J.-H., Tsai S.-L., Yin J.-C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007;41:119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari A., Chan S., Wong A., Tai J., Cheng K., Chan J., Tsang K., Hospital, N.T.F.o.A.-S.o.Q.M. Severe acute respiratory syndrome (SARS) in Hong Kong: patients' experiences. Nurs. Outlook. 2003;51:212–219. doi: 10.1016/j.outlook.2003.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tortella-Feliu M., Fullana M.A., Pérez-Vigil A., Torres X., Chamorro J., Littarelli S.A., Solanes A., Ramella-Cravaro V., Vilar A., González-Parra J.A., Andero R., Reichenberg A., Mataix-Cols D., Vieta E., Fusar-Poli P., Ioannidis J.P.A., Stein M.B., Radua J., Fernández de la Cruz L. Risk factors for posttraumatic stress disorder: an umbrella review of systematic reviews and meta-analyses. Neurosci. Biobehav. Rev. 2019;107:154–165. doi: 10.1016/j.neubiorev.2019.09.013. [DOI] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdés-Florido M.J., López-Díaz Á., Palermo-Zeballos F.J., Martínez-Molina I., Martín-Gil V.E., Crespo-Facorro B., Ruiz-Veguilla M. Reactive psychoses in the context of the COVID-19 pandemic: clinical perspectives from a case series. Rev. Psiquiatr. Salud Ment. 2020 doi: 10.1016/j.rpsm.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieta E., Perez V., Arango C. Psychiatry in the aftermath of COVID-19. Rev Psiquiatr Salud Ment. 2020 doi: 10.1016/j.rpsm.2020.04.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaibeh E., Mahmoud H., Naal H. Telemental health in the context of a pandemic: the COVID-19 experience. Curr. Treat. Options Psychiatry. 2020:1–5. doi: 10.1007/s40501-020-00210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson V., Murphy D., Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup. Med. (Oxf., Engl.) 2020 doi: 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J., Cheung E.P.T., Cheung V., Cheung C., Chan M.T.Y., Chua S.E., McAlonan G.M., Tsang K.W.T., Ip M.S.M. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med. Teacher. 2004;26:657–659. doi: 10.1080/01421590400006572. [DOI] [PubMed] [Google Scholar]
- Wong T.W., Lee C.K., Tam W., Lau J.T.F., Yu T.S., Lui S.F., Chan P.K.S., Li Y.G., Bresee J.S., Sung J.J.Y., Parashar U.D., Outbreak Study G. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg. Infect. Dis. 2004;10:269–276. doi: 10.3201/eid1002.030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.T., Jin Y., Cheung T. Joint International collaboration to combat mental health challenges during the coronavirus disease 2019 pandemic. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.1057. [DOI] [PubMed] [Google Scholar]
- Xu J., Yang M., Liu Z. Clinical analysis of patients with severe acute respiratory syndrome in Beijing area. Zhonghua Jie He He Hu Xi Za Zhi. 2003;26:683–685. [PubMed] [Google Scholar]
- Yan Y., Shin W.I., Pang Y.X., Meng Y., Lai J., You C., Zhao H., Lester E., Wu T., Pang C.H. The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: recent advances, prevention, and treatment. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17072323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip H.K., Tsang P.C., Samaranayake L.P., Li A.H. Knowledge of and attitudes toward severe acute respiratory syndrome among a cohort of dental patients in Hong Kong following a major local outbreak. Commun. Dent. Health. 2007;24:43–48. [PubMed] [Google Scholar]
- Yip P.S., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010;31:86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
- Yung A.R., Yuen H.P., McGorry P.D., Phillips L.J., Kelly D., Dell'Olio M., Francey S.M., Cosgrave E.M., Killackey E., Stanford C., Godfrey K., Buckby J. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust. N. Z. J. Psychiatry. 2005;39:964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- Zhang S.X., Huang H., Wei F. Geographical distance to the epicenter of Covid-19 predicts the burnout of the working population: Ripple effect or typhoon eye effect? Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.-R., Wang K., Yin L., Zhao W.-F., Xue Q., Peng M., Min B.-Q., Tian Q., Leng H.-X., Du J.-L., Chang H., Yang Y., Li W., Shangguan F.-F., Yan T.-Y., Dong H.-Q., Han Y., Wang Y.-P., Cosci F., Wang H.-X. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Ji P., Pang J., Zhong Z., Li H., He C., Zhang J., Zhao C. Clinical characteristics of 3,062 COVID-19 patients: a meta-analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulkifli N., Sivapatham S., Guan N. Brief psychotic disorder in relation to coronavirus, COVID-19 outbreaks: a case report. Malays. J. Psychiatry. 2020;2020:29. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.