The term chronic obstructive pulmonary disease (COPD) is applied to patients with chronic bronchitis and/or emphysema. COPD affects up to 10% of the adult population aged >40 years and is the fourth most common cause of death worldwide.1, 2 It is increasing in prevalence particularly in women,1, 2 and is commonly associated with cardiovascular disease, depression, gastro-oesophageal reflux, osteoporosis and cancer.3, 4 Severity of COPD can be easily assessed objectively by spirometry5 (Table 30.1 ) and functionally based upon dyspnoea and exercise capacity6 (Table 30.2 ).
Table 30.1.
Global Initiative for Obstructive Lung Disease (GOLD) criteria for COPD severity based upon spirometry5
| FEV1/FVC (%) | FEV1 (% PREDICTED) | |
|---|---|---|
| 1 | <70 | >80 |
| 2 | <70 | 50–80 |
| 3 | <70 | 30–50 |
| 4 | <70 | <30 |
Table 30.2.
The body mass index, airflow obstruction, dyspnoea and exercise capacity (BODE) index (maximum is 10)6*
| SCORE | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| FEV1 (% predicted) | >65 | 50–64 | 36–49 | <35 |
| Six-minute walk distance | >350 | 250–350 | 150–250 | <150 |
| Modified MRC dyspnoea score | 0–1 | 2 | 3 | 4 |
| Body mass index | >21 | <21 | ||
The 4-year survival rates are 80% for a score of 2, 70% for 3–4, 60% for 5–6 and 20% for scores 7–10.
Modified Medical Research Council (MRC) score is from zero (no dyspnoea) to 4 (extreme dyspnoea upon getting dressed or leaving the house). FEV1 = forced expiratory volume in 1 second.
An acute exacerbation of COPD (AECOPD) is defined as ‘an event in the natural course of the disease characterised by change in dyspnoea, cough or sputum’.4 AECOPD is the commonest admission diagnosis in UK general hospitals (~ 16% of admissions).4 Patients with an AECOPD have an in-hospital mortality of 3–8%, and a 30-day mortality of 14–26% (compared with 8% for myocardial infarction).2, 3, 4, 7, 8, 9 Cautious oxygen delivery and non-invasive ventilatory (NIV) support have been the major advances in therapy in the past decade, which have resulted in a reduced need for invasive mechanical ventilation (IMV) and improved survival. The need for either IMV or NIV ventilatory support in AECOPD varies considerably across continents: for example in the UK, IMV and NIV are used in 1% and 11% of admissions respectively,8 whereas in the USA they are used in 3% and 5% of admissions respectively.9
Aetiology
The causes of COPD can be divided into environmental and host factors. Environmental factors include tobacco smoke, air pollution, indoor fumes (e.g. indoor cooking with solid biomass fuel) and poor socioeconomic status. The biggest single factor in over 95% of patients with COPD is tobacco smoking (Fig. 30.1 ). However, only approximately 15% of smokers develop COPD. Marijuana smoking may cause premature and quite advanced bullous emphysema compared with tobacco smokers, owing to extremely hot and toxic inhaled smoke held at peak inspiration for prolonged periods of time.3 Host factors are the balance between circulating proteases and antiproteases (e.g. α-1 antitrypsin deficiency) and the intake of antioxidant vitamins (A, C, E).10
Figure 30.1.
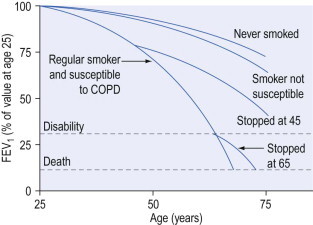
Decline in lung function with age in different smoking categories. FEV1 = forced expiratory volume in 1 second; COPD = chronic obstructive pulmonary disease.
Pathophysiology
Reduced expiratory air flow in COPD is due to both increased airway resistance and reduced lung elastic recoil. Airway resistance is increased by mucosal oedema and hypertrophy, secretions, bronchospasm, airway tortuosity and air-flow turbulence and loss of lung parenchymal elastic tissues that normally support the small airways. Loss of lung elastic recoil pressure is due both to loss of lung elastin and to loss of alveolar surface tension from alveolar wall destruction.
Reduced lung elastic recoil decreases expiratory air flow by reducing the alveolar pressure driving expiratory air flow and by reducing the intraluminal airway pressure, which normally distends small airways during expiration. Forced expiration increases alveolar driving pressure, but also causes dynamic airway compression resulting in no improvement or sometimes reduction in expiratory air flow. These factors are present in varying proportions, depending on the degree of chronic bronchitis and emphysema and the individual patient.
Air-flow limitation results in prolonged expiration, pulmonary hyperinflation, inspiratory muscle disadvantage, increased work of breathing and the sensation of dyspnoea. All these factors are worsened during an exacerbation of COPD.
Pulmonary hyperinflation has both static and dynamic components. The static component remains at the end of an expiratory period long enough for all expiratory air flow to cease (30–120 s), enabling the lungs and chest wall to reach their static functional residual capacity (FRC). This component of hyperinflation is due to loss of parenchymal elastic recoil, chest wall adaptation11 and airway closure, which occurs throughout expiration. Dynamic pulmonary hyperinflation is the further increase in hyperinflation due to slow expiratory air flow not allowing completion of expiration before the arrival of the next breath. The extent of dynamic hyperinflation depends on the severity of air-flow obstruction, the amount inspired (tidal volume) and the expiratory time.12 Chest wall hyperinflation leads to suboptimal muscle length–tension relationships and mechanical disadvantage, thereby predisposing patients to respiratory muscle fatigue as the work of breathing increases, particularly if associated with myopathic situations (steroids, electrolyte disturbances).13, 14 Minor reductions in lung function due to infection, mild cardiac failure or atelectasis increase the work of breathing, due to increases in both respiratory impedance and dead space. With acute changes in workload, rapid decompensation with ventilatory failure and acute hypercapnia may occur.
Although chronic hypercapnia, as a consequence of reducing minute ventilation, is a fatigue-sparing mechanism that occurs in some patients, this is usually accompanied by renal compensation with retention of bicarbonate ions to correct the low pH. This has the additional effect of reducing the respiratory distress caused by hypercapnic acidosis. Central respiratory drive may also be impaired, or poorly responsive to physiological triggers – hypoxaemia or hypercapnia – and lead to chronic hypercapnia. This may occur in the setting of sleep (i.e. obstructive sleep apnoea),11 obesity or drugs (e.g. sedatives, antiepileptics, alcohol).
Hypoxia and vascular wall changes lead to pulmonary vasoconstriction, pulmonary hypertension, cor pulmonale, V/Q mismatching and the development of shunts.
Chronic bronchitis or emphysema?
The value of labelling patients as chronic bronchitis or emphysema is uncertain as the two disease processes usually coexist and the principles of management are similar. Five pathophysiological processes may be present to varying degrees in each patient with COPD: (1) inflammatory airway narrowing (bronchiolitis), (2) loss of connective tissues tethering airways, (3) loss of alveoli and capillaries, (4) hyperinflation, and (5) increased pulmonary vascular resistance. Early/mild COPD tends to be dominated by bronchiolitis with a minimal component of emphysema, whereas when COPD becomes severe the reverse is true. However, recognition that COPD is dominated by one of these patterns is helpful with regard to clinical pattern and prognosis.
Precipitants of acute respiratory failure
In approximately 50% of patients there is an infective cause, in 25% heart failure and in the remaining 25% retained secretions, air pollution, coexistent medical problems (e.g. pulmonary embolus, medication compliance or side-effects) or no cause can be identified (Box 30.1 ).14, 15
Box 30.1. Precipitants of acute respiratory failure in chronic obstructive pulmonary disease.
Infective (including aspiration)
Left ventricular failure (systolic and diastolic failure)
Sputum retention (postoperative, traumatic)
Pulmonary embolism
Pneumothoraces and bullae
Uncontrolled oxygen
Sedation
Medication – non-compliance or side-effects
Nutritional (K, PO4, Mg deficiency, CHO excess)
Sleep apnoea
Infection
The most common bacterial isolates are Streptococcus pneumoniae and Haemophilus influenzae in 80% of exacerbations. S. viridans, Moraxella (previously Branhamella) catarrhalis, Mycoplasma pneumoniae and Pseudomonas aeruginosa may also be found. Viruses can be isolated in 20–30% of exacerbations and include rhinovirus, influenza and parainfluenza viruses, coronaviruses and occasionally adenovirus, and respiratory syncytial virus. Whether these organisms are pathogens or colonisers is often unclear. Background microbiological agents are identified in 48% of stable COPD, compared with 70% during an AECOPD.16, 17 Pneumonia has been estimated to account for 20% of presentations requiring mechanical ventilation.4
Heart failure
Left ventricular (LV) systolic failure may result from coexisting ischaemic heart disease, fluid overload, tachyarrhythmias or biventricular failure secondary to cor pulmonale. LV diastolic failure occurs commonly and is precipitated by hypoxaemia, tachycardia, pericardial constraint due to intrinsic positive end-expiratory pressure (PEEPi) or right ventricular (RV) dilation.11, 18, 19 Increased work of breathing related to COPD will also increase by up to 10-fold the amount of blood flow to the respiratory pump muscles,20 thereby causing an increased demand upon the overall cardiac output. In patients with borderline cardiac status, this may precipitate heart failure. The components of RV and LV failure can be accurately distinguished by Doppler echocardiography. Pulmonary congestion can be difficult to diagnose because of the abnormal breath sounds and chest X-ray appearance that are commonly present in COPD. In a recent publication, 51% of patients with acute exacerbation of COPD had echocardiographic evidence of left heart failure (systolic 11%, diastolic 32%, systolic and diastolic 7%).11 A further study of CT and MR scanning and echocardiography in a large community population (15% of whom had COPD) identified that severity of emphysema on CT scanning indirectly correlated with left ventricular end-diastolic volume, stroke volume and cardiac output.18 These authors concluded that increasing severity of COPD was associated with worsening cardiac function.
Uncontrolled oxygen
This may precipitate acute hypercapnia in patients with more severe COPD, due to: (1) shunting blood to low-V/Q lung units and increasing dead space, (2) loss of hypoxic drive, (3) dissociation of CO2 from Hb molecule (Haldane effect), and (4) anxiolysis and reduction in tachypnoea.21 Major randomised controlled trials have indicated significant reductions in need for IMV, hospital length of stay and mortality with controlled (or targeted at a specific  range – e.g. 88–92%) oxygen therapy compared with uncontrolled oxygen therapy in ambulances,22 emergency rooms23 and hospital wards.8
range – e.g. 88–92%) oxygen therapy compared with uncontrolled oxygen therapy in ambulances,22 emergency rooms23 and hospital wards.8
Diagnosis and assessment
The clinical examination findings of COPD should be confirmed and severity quantified by spirometry (see Tables 30.1 and 30.2). In mild stable disease (e.g. forced expiratory volume in 1 second (FEV1) >50% predicted normal), an expiratory wheeze on forced expiration and mild exertional dyspnoea may be the only symptoms.
In moderate-severity COPD (e.g. FEV1 30–50% predicted normal), modest to severe exertional dyspnoea is associated with clinical signs of hyperinflation (ptosed upper border of liver beyond the 4th intercostal space anteriorly and loss of cardiac percussion) and signs of increased work of breathing (use of accessory muscles and tracheal tug).
In severe stable COPD (e.g. FEV1 < 30% predicted normal), marked accessory muscle use is associated with tachypnoea at rest, pursed-lip breathing, hypoxaemia and signs of pulmonary hypertension (RV heave, loud and palpable pulmonary second sound and elevated a-wave in jugular venous pressure (JVP)) and cor pulmonale (elevated JVP, hepatomegaly, ankle swelling).
In severe unstable COPD, there is marked tachypnoea at rest, hypoxaemia and tachycardia, and, in some, signs of hypercapnia (dilated cutaneous veins, blurred vision, headaches, obtunded mentation, and confusion).
Clinical examination may also identify associated medical conditions that might have precipitated the exacerbation such as crackles and bronchial breathing due to infection, crackles and cardiomegaly related to heart failure or mediastinal shift related to a pneumothorax. Acute respiratory failure (ARF) in COPD can present with two distinct clinical patterns15 (Table 30.3 ), namely relatively thin and normocapnic or obese and hypercapnic.
Table 30.3.
Clinical differences between normocapnic and hypercapnic chronic obstructive pulmonary disease
NORMOCAPNIC ( 35–45 mmHg) 35–45 mmHg) |
HYPERCAPNIC ( > 45 mmHg) > 45 mmHg) |
|---|---|
| Emphysema > chronic bronchitis | Chronic bronchitis > emphysema |
| Thin | Obese |
| Pursed-lip breathing | Central nervous system depression: consider the role of oxygen therapy |
| Accessory muscle use | Alcohol, sedatives, analgesics |
| Hyperinflated | Sleep-related hypoventilation |
| Right heart failure late | Right heart failure early |
Basic investigations such as spirometry are very useful for confirming a clinical diagnosis and determining severity of disease. An FEV1/VC ratio <70% with an FEV1 of 50–80% predicted normal without a bronchodilator response usually indicates mild COPD. A significant bronchodilator response, which implies asthma, is regarded as a 12% or greater increase and 200 mL increase in either FEV1 or VC. An FEV1 30–50% predicted normal indicates moderately severe COPD and FEV1 < 30% predicted normal indicates severe COPD.5
Flow–volume curves usually demonstrate reduced expiratory flow rates at various lung volumes and the characteristic concave expiratory flow pattern. Lung volumes measured by either helium dilution or plethysmography show elevated total lung capacity, FRC and residual volume. Characteristically, the residual volume/total lung capacity ratio is >40% in COPD and represents intrathoracic gas trapping. The total lung carbon monoxide (TLCO) uptake is a measurement of alveolar surface area and its reduction approximates the amount of emphysema present (usually <80% predicted normal).
A chest X-ray will commonly show hyperinflated lung fields, as suggested by 10 ribs visible posteriorly, six ribs visible anteriorly or large air space anterior to heart (>⅓ of the length of the sternum), flattened diaphragms (best seen on lateral chest X-ray) and a paucity of lung markings. Pulmonary hypertension is manifested by enlarged proximal and attenuated distal vascular markings and by RV and atrial enlargement. Lung bullae may be evident.
A high-resolution computed tomographic (CT) scan of the chest (1–2 mm slices) can demonstrate characteristic appearance and regional distribution of emphysema. It can also assess any coexistent bronchiectasis, LV failure24 and pulmonary fibrosis. Such scans are less sensitive than standard chest CT scans (1 cm slice) for detecting pulmonary lesions (e.g. neoplasms). Nuclear ventilation perfusion scans can also provide a characteristic appearance of COPD.
An electrocardiogram (ECG) is commonly normal but may show features of right atrial or RV hypertrophy and RV strain, including P pulmonale, right-axis deviation, dominant R-waves in V1–2, right bundle-branch block, ST depression and T-wave flattening or inversion in V1–3. These changes may be chronic or may develop acutely if there is significant increase in pulmonary vascular resistance during the illness. The ECG may also show coexistent ischaemic heart disease, tachycardia and atrial fibrillation. Occasionally, continuous ECG monitoring is required to identify transient arrhythmias, which may also precipitate acute deterioration. Plasma brain natriuretic peptide (BNP) levels may also assist in the diagnosis of heart failure (elevated BNP) from pulmonary causes (low BNP) in patients under 70 years free of renal impairment.25
Differential diagnosis
The history of chronic asthma is one of long-term dyspnoea, wheeze and cough, usually at night or upon exercise, beginning in childhood with clear-cut precipitating agents (e.g. weather, dust, pets, drugs) and a favourable response to either steroids or inhaled β2-agonists. Late-onset asthma (>40 years of age) is not uncommon and is often associated with recurrent gastro-oesophageal reflux. In both forms of asthma, TLCO is normal. There is usually a bronchodilator response in the FEV1 if the patient has unstable asthma. In patients in whom asthma is considered but lung function tests are normal, the FEV1 response to an inhalational challenge (e.g. methacholine or hypertonic saline) may assist in discriminating asthma from other causes of dyspnoea.
Bronchiolitis obliterans is a condition that presents as a fixed air-flow obstruction following a viral illness, inhalation of toxic fumes, following bone marrow or heart/lung transplantation, or related to drugs (e.g. penicillamine). It generally begins as a cough some weeks after insult and insidious onset of dyspnoea. There is a broad spectrum of radiological appearances from normal to reticulonodular to diffuse nodular. Lung tissue via bronchoscopy or by thoracoscopy is required for diagnosis. Histologically, there is a characteristic chronic bronchiolar inflammation appearance, and if granulation tissue extends into the alveoli it is referred to as bronchiolitis obliterans or organising pneumonia. Removal of the offending agent and instigation of steroids are generally associated with a favourable prognosis.
Bronchiectasis is often associated with fixed mild to moderate air-flow obstruction. A chronic productive cough (daily for 2 consecutive years) is characteristic. Clinical features such as clubbing, localised pulmonary crackles and a characteristic appearance on high-resolution CT, with dilated or plugged small airways at least twice the size of accompanying blood vessel, assist in the diagnosis.
Congestive heart failure (CHF) may be a differential diagnosis of COPD, or simply coexist, as both disorders are common in smokers.11 Orthopnoea and paroxysmal nocturnal dyspnoea are features that correlate with heart failure severity. A past history of myocardial ischaemia or atrial fibrillation should alert one to the possibility of heart failure. An echocardiogram and high-resolution CT (looking for shift in interstitial oedema with changes in posture from supine to prone)24 are sensitive markers of CHF.
Assessment of respiratory failure
An acute exacerbation of COPD (AECOPD) is defined as ‘an event in the natural course of the disease characterised by change in dyspnoea, cough or sputum’.4
Arterial blood gases are mandatory to assess hypoxia, hypercapnia and acid–base status. Chronic hypercapnia may be recognised by a bicarbonate level >30 mmol/L and a base excess >4 mmol/L indicating renal compensation. However, other causes of high serum bicarbonate need to be excluded (e.g. diuretic therapy, high-dose steroids or high-volume gastric fluid loss), or chronic hypercapnia may be incorrectly assumed and the severity of COPD overestimated. Renal compensation for chronic hypercapnia will increase the serum bicarbonate by approximately 4 mmol/L for each 10 mmHg (1.33 kPa) of chronic  rise above 40 mmHg (5.3 kPa), in order to return pH to the low-normal range. Irrespective of the COPD patient's usual
rise above 40 mmHg (5.3 kPa), in order to return pH to the low-normal range. Irrespective of the COPD patient's usual  level, an acute increase in
level, an acute increase in  leads to a decreased arterial pH. This indicates that compensatory mechanisms are exhausted and there is an increased risk of respiratory collapse. The agreement between arterial and peripheral venous blood gases in terms of pH or
leads to a decreased arterial pH. This indicates that compensatory mechanisms are exhausted and there is an increased risk of respiratory collapse. The agreement between arterial and peripheral venous blood gases in terms of pH or  is extremely poor (±0.1 and ±25 mmHg (0.013 and 3.25 kPa) respectively).26 Thus the use of peripheral venous blood gases to assess respiratory failure should be used with great caution.
is extremely poor (±0.1 and ±25 mmHg (0.013 and 3.25 kPa) respectively).26 Thus the use of peripheral venous blood gases to assess respiratory failure should be used with great caution.
Management of respiratory failure
Non-ventilatory management
Oxygen therapy
Oxygen given by low-flow intranasal cannulae or 24–35% Venturi mask should be titrated to achieve a saturation ( ) of 88–92% as these levels will avoid significant increases in
) of 88–92% as these levels will avoid significant increases in  in the majority of COPD patients with ARF. Increases in
in the majority of COPD patients with ARF. Increases in  are most common in patients with initial
are most common in patients with initial  > 50 mmHg (6.5 kPa) and pH < 7.35.27 Excessive oxygen therapy is the cause of increased hypercapnia in a third of acidotic AECOPD patients.8 For this reason, ABGs should be repeated 1 hour following initiation of oxygen therapy, as with NIV, to ensure an optimal direction of improvement in the underlying AECOPD. If the rise in
> 50 mmHg (6.5 kPa) and pH < 7.35.27 Excessive oxygen therapy is the cause of increased hypercapnia in a third of acidotic AECOPD patients.8 For this reason, ABGs should be repeated 1 hour following initiation of oxygen therapy, as with NIV, to ensure an optimal direction of improvement in the underlying AECOPD. If the rise in  is excessive (>10 mmHg or 1.33 kPa), then
is excessive (>10 mmHg or 1.33 kPa), then  should be reduced, titrating
should be reduced, titrating  to 2–3% below the previous value, and arterial blood gases should be repeated. If no
to 2–3% below the previous value, and arterial blood gases should be repeated. If no  rise occurs with oxygen therapy, then a higher
rise occurs with oxygen therapy, then a higher  may be targeted with repeat ABG.
may be targeted with repeat ABG.
Inadequate reversal of hypoxia (e.g.  < 85%) is suggestive of an additional problem such as pneumonia, pulmonary oedema or embolus, or a pneumothorax. Investigation of this should commence and a higher O2 delivery system should be used (see Ch. 28). Although high levels of O2 should be avoided, reversal of hypoxia is important and O2 should not be withheld in the presence of hypercapnia, or withdrawn if it worsens.
< 85%) is suggestive of an additional problem such as pneumonia, pulmonary oedema or embolus, or a pneumothorax. Investigation of this should commence and a higher O2 delivery system should be used (see Ch. 28). Although high levels of O2 should be avoided, reversal of hypoxia is important and O2 should not be withheld in the presence of hypercapnia, or withdrawn if it worsens.
Bronchodilators
Bronchodilators are routinely given in all acute exacerbations of COPD because a small reversible component of air-flow obstruction is common, and bronchodilators improve mucociliary clearance of secretions. A large meta-analysis of 22 large randomised controlled long-term trials of ambulatory COPD patients involving anticholinergics and/or β2-agonists (short- and long-acting) over 3–60 months indicated that anticholinergics are more favourable than placebo in terms of acute exacerbations and hospitalisations.3, 28 There were no favourable advantages with β2-agonists compared with placebo for acute exacerbations or hospitalisations, and placebo was better than β2-agonists in terms of respiratory death.28 There is a cardiovascular risk if given in excessive doses.29
Anticholinergic agents, such as ipratropium bromide, have been shown to have a similar or greater bronchodilator action than β-agonists in COPD,4, 5 and also to have fewer side-effects and no tachyphylaxis. Anticholinergic agents should be used routinely in AECOPD. An ipratropium bromide nebule of 0.5 mg in 2 mL should be nebulised initially 2-hourly, then every 4–6 hours. Long-term use of ipratropium bromide has been shown to reduce the incidence of exacerbations23 and is therefore recommended for chronic use in ambulatory COPD. Long-acting anticholinergics (e.g. tiotropium) offer potential of once-daily dosing.
Nebulised β-agonists are also effective bronchodilators in COPD,4, 5 although they may cause tachycardia, tremor, mild reductions in potassium and  (due to pulmonary vasodilatation) and tachyphylaxis. As in asthma, lactic acidosis may also occur with excessive β-agonists, either nebulised or intravenous. Nebulised β-agonists (e.g. salbutamol, terbutaline or fenoterol) given 2–4-hourly should be used routinely in combination with ipratropium. This combination has been shown to be more effective than either agent alone. Parenteral sympathomimetic agents are not recommended for routine use. In stable patients, long-term use of β-agonists may improve symptoms of dyspnoea, particularly in the subgroup of COPD with an objective bronchodilator response.
(due to pulmonary vasodilatation) and tachyphylaxis. As in asthma, lactic acidosis may also occur with excessive β-agonists, either nebulised or intravenous. Nebulised β-agonists (e.g. salbutamol, terbutaline or fenoterol) given 2–4-hourly should be used routinely in combination with ipratropium. This combination has been shown to be more effective than either agent alone. Parenteral sympathomimetic agents are not recommended for routine use. In stable patients, long-term use of β-agonists may improve symptoms of dyspnoea, particularly in the subgroup of COPD with an objective bronchodilator response.
Steroids
In acute exacerbations of COPD, short-term steroids have been shown to improve air-flow obstruction30 including those patients requiring mechanical ventilation for COPD.31 Doses similar to those for acute asthma should be used. Methylprednisolone 0.5 mg/kg, given 6-hourly for 72 hours, was used in the study by Albert et al,30 demonstrating benefit in patients with an exacerbation of COPD. Current American Thoracic Society guidelines recommend the equivalent to oral prednisolone at 0.5 mg/kg body weight for up to 10 days, then ceasing; however, this will depend upon the response to treatment, and their premorbid use.5 Steroids should be avoided if the deterioration is clearly due to bacterial pneumonia without bronchospasm.
Longer-term oral steroids in COPD are associated with a substantial increased risk of side-effects (osteoporosis, diabetes, peptic ulcer, myopathy, systemic hypertension, fluid retention, weight gain), and are therefore not recommended.5 A small group of patients (15%) may demonstrate a significant bronchodilator response; coexistent asthma is likely in these patients and longer-term high-dose (usually inhaled) steroids may be necessary. In the majority of patients, long-term inhaled steroids do not improve lung function or survival; however, they may improve quality of life and reduce admissions.5
Antibiotics
Antibiotics have an accepted role in the treatment of infection-induced exacerbations of COPD.4 Amoxicillin is a suitable first-line agent against Haemophilus influenzae and Streptococcus pneumoniae for outpatient exacerbations. Serious exacerbations requiring hospital admission require newer agents such as ciprofloxacin or a third-generation cephalosporin. Antibiotics for pneumonia are discussed elsewhere in this volume.
Aminophylline
Aminophylline is a weak bronchodilator in COPD. It improves diaphragm contractility, stimulates respiratory drive, improves mucociliary transport and right heart function, is anti-inflammatory and is a weak diuretic.32, 33 Some studies have shown no benefit and significant side-effects,34 whereas others have shown small benefit35 in stable COPD. For an exacerbation, aminophylline (loading dose 5–6 mg/kg i.v. over 30 minutes, followed by an infusion of 0.5 mg/kg per hour). Serum theophylline levels must be monitored regularly to reduce risk of toxicity.
Anticoagulants
Subcutaneous heparin (e.g. 5000 units b.d.) is recommended as a prophylactic measure against venous thromboembolism. There is no evidence for warfarinisation in COPD patients with pulmonary hypertension.
Electrolyte correction
Electrolyte correction is important. Hypophosphataemia,13 hypomagnesaemia,36 hypocalcaemia14 and hypokalaemia may impair respiratory muscle function. Hyponatraemia may occur with inappropriate antidiuretic hormone release or with excess use of diuretics and inappropriate intravenous fluids.
Nutrition
Nutrition is important, as patients with severe COPD are often undernourished – a subnormal BMI is a risk factor for mortality in COPD. Excessive carbohydrate calories should be avoided as this increases CO2 production (by >15%) and may worsen respiratory failure. Low-carbohydrate/high-fat combinations are preferred in ARF during spontaneous ventilation.
Chest physiotherapy
Chest physiotherapy should be initiated and regularly repeated as both a curative and preventive measure. Encouragement of coughing and deep breathing are the two most important factors. ‘Bubble positive expiratory pressure (PEP)’ is an inexpensive method of assisting sputum clearance in patients with retained secretions or those having difficulty expectorating.
Nebulised mucolytic agents
Nebulised mucolytic agents, such as N-acetylcysteine, continue to be proposed, although their benefit has never been established in acute exacerbations of COPD. Oral mucolytics have been shown to reduce cough frequency and severity in stable COPD.37
Non-invasive ventilation (NIV)
NIV, a technique in which ventilatory support is provided via a nasal or facial mask without endotracheal intubation, is now a routine standard of care for AECOPD. When applied well, NIV has the same physiological effect as IMV.38 Two landmark randomised controlled trials in intensive care wards in 199539 and in general medical wards in 200140 clearly indicated a role for NIV in hypercapnic AECOPD. Since then, there have been several randomised controlled trials and meta-analyses of NIV in hypercapnic AECOPD which have demonstrated improved respiratory physiology, reduced mortality (up to 12 months), reduced iatrogenic complications, reduced need for intubation and mechanical ventilation and reduced length of stay in hospital.8, 9, 41, 42 All studies have shown good tolerance of the technique (>80% of patients), with few side-effects, improvements in both oxygenation and  compared with medically treated control patients.
compared with medically treated control patients.
Two important reviews of acute NIV use in AECOPD from the USA and the UK have been recently been published. In the USA between 1998 and 2008, the use of NIV increased (from 1.0 to 4.5% of all admissions) and IMV decreased (from 6.0 to 3.5%) with NIV eclipsing IMV in 2008.9 Associated with this significant change in pattern of ventilatory support was an overall reduction in mortality in those started on NIV or IMV early.9 In the UK, during a 3-month snapshot of 232 hospitals during 2008, 11% of all admissions with AECOPD received NIV.8 Oxygen toxicity was found to occur in a third of hypercapnic AECOPD.8 In both USA and UK studies, NIV failure with transfer to IMV was associated with greatest mortality (estimated to be ~ 30 (USA)–40 (UK)%) compared with successfully used NIV (6 (USA)–11 (UK)%) and non-hypercapnic COPD (~ 3% USA, 5% UK).
The goal of NIV is: (1) to unload respiratory muscles and augment ventilation and oxygenation, reduce CO2 and correct acidosis until the underlying problem can be reversed; (2) when applied intermittently, to offset the adverse effects of sleep- or position-induced adverse changes to ventilation, increased upper airway resistance and lung volume.
Indications for NIV are a deterioration of COPD with: (1) acute dyspnoea; (2) respiratory rate >28 breaths/min; (3)  > 45 mmHg (5.85 kPa) with a pH < 7.35, despite optimal medical treatment and not related to excessive supplemental oxygen. Although these indications are for mild exacerbations, most randomised studies have used these as entry guidelines.8, 41, 42 Initial guidelines recommended NIV use to be limited to patients with pH in the range 7.25–7.35; however, recent evidence suggests that NIV is useful even in those patients with lower pH values (to as low as 7.0) and associated more severe hypercapnia (as high as 140 mmHg (18.2 kPa)).43
> 45 mmHg (5.85 kPa) with a pH < 7.35, despite optimal medical treatment and not related to excessive supplemental oxygen. Although these indications are for mild exacerbations, most randomised studies have used these as entry guidelines.8, 41, 42 Initial guidelines recommended NIV use to be limited to patients with pH in the range 7.25–7.35; however, recent evidence suggests that NIV is useful even in those patients with lower pH values (to as low as 7.0) and associated more severe hypercapnia (as high as 140 mmHg (18.2 kPa)).43
Included in the indications are recently extubated patients in whom NIV has been shown to reduce re-intubation rates significantly.44, 45 Recently NIV has been advocated for use in patients with hypoxic respiratory failure,46 but success is significantly less in the setting of hypoxaemia and either normocapnia or hypocapnia. NIV may also have a role in some patients where mechanical ventilation is considered inappropriate.
Side-effects of NIV include discomfort, intolerance, skin necrosis, gastric distension and aspiration. Pressure support has been reported as better tolerated than assist/control.47 End-of-life plans should be considered in all patients with AECOPD, particularly those undergoing NIV, as ~ 20% of patients will fail to respond or deteriorate. This period of time on NIV can be used to assess resuscitation status.
Invasive mechanical ventilation
When respiratory failure progresses despite aggressive conservative management, including NIV, invasive mechanical ventilatory (IMV) support may be necessary. The decision to ventilate requires careful consideration in some patients who may have near-end-stage lung disease and whose quality of life may not justify aggressive treatment. This decision requires consideration of the outcome of ARF.
An episode of ARF further decreases survival (Fig. 30.2 ). ARF precipitated only by bronchitis has a better outcome, whereas ARF due to more serious causes such as pneumonia, LV failure and pulmonary embolus has a worse outcome, and studies including all such outcomes have lower survival rates.
Figure 30.2.
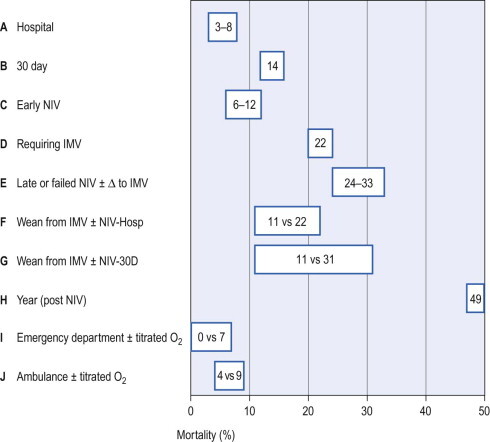
Estimated mortality for groups of patients with acute exacerbations of COPD. A and B groups: refer to in-hospital and 30-day mortality;8, 9 C group: refers to early institution of NIV;8, 9 D group: refers to patients requiring IMV;9 E group: refers to hypercapnic AECOPD patients either failing NIV and needing IMV, or those identified late as requiring NIV;8, 9 F and G groups: weaned from IMV and randomised to either immediate NIV or not (i.e. randomised controlled trial) with in-hospital and 30-day mortality;44 H group: 1-year mortality post NIV;7 I and J groups: effect of titrated versus untitrated oxygen at emergency department23 and ambulance.22
If ARF requires IMV, survival decreases further still (see Fig. 30.2). Although only 18 to 3.5%9 of patients with AECOPD require IMV, and 4.59 to 11%8 need NIV, the short-term survival in this more severe subset is still good, with a hospital survival rate in some series as high as 90%, but 2- and 3-year survival is significantly lower. The severity of ARF and the severity of underlying COPD based on FEV1, lifestyle score and dyspnoea score are also predictors of outcome. Lifestyle and dyspnoea categories may be the most useful factors in the decision to withhold IMV. Lifestyle categories 3 (house-bound and at least partly dependent) and 4 (bed- or chair-bound) indicate both a poor outcome48 and quality of life that may not justify aggressive treatment.
Thus IMV may be withheld in end-stage lung disease, when low survival, poor quality of life or permanent ventilator dependence is likely. If end-stage lung disease is suspected but there is insufficient information, then a brief trial of aggressive therapy, including IMV, should be undertaken and subsequently withdrawn if unsuccessful. Despite this, most patients with COPD who present with ARF do not have end-stage disease and, although their immediate problems may be life threatening, their short-term outcome is sufficiently good to justify full active treatment.
Invasive mechanical ventilation technique
The goals of IMV in COPD are to support ventilation while reversible components improve, to allow respiratory muscle to rest and recover whilst preventing wasting from total inactivity and to minimise dynamic hyperinflation. This is usually best accomplished with low-level ventilatory support. Patients requiring low-level support may be commenced on 8–15 cmH2O pressure support, with 3–8 cmH2O PEEP. Patients who are completely exhausted, post arrest, comatose or not tolerating pressure support alone should be commenced or transferred to synchronised intermittent mandatory ventilation mode.
Excessive dynamic hyperinflation must be avoided by using a low-minute ventilation – 115/mL per kg is a guideline6 – and allowing adequate time for expiration. This should be achieved by the use of a small tidal volume (8 mL/kg) and a ventilator rate <14 breaths/min.12 Dynamic hyperinflation can be assessed clinically by visualising the expiratory flow–time curve, and by measuring plateau airway pressure (P plat) or PEEPi. P plat should be measured by applying an end-inspiratory pause of 0.5 seconds. This should be applied only following a single breath as it shortens expiratory time and if it is applied to a series of breaths it increases dynamic hyperinflation, resulting in an increased P plat level and increased risk to the patient. If P plat is >25 cmH2O, there is likely to be excessive dynamic hyperinflation, and the ventilator rate should be reduced. However, P plat may be high without dynamic hyperinflation if chest wall compliance is low. Intrinsic PEEP measured as a prolonged end-expiratory pause more directly assesses dynamic hyperinflation. Provided PEEPi is accurately measured, it is a useful tool to follow dynamic hyperinflation. In severe air-flow limitation it may be necessary to accept low levels of PEEPi, but as PEEPi rises above 8–10 cmH2O further prolongation of expiratory time must be considered. Although still controversial, the use of a high inspiratory flow rate is recommended12, 49 as it results in a shorter inspiratory time and hence a longer expiratory time for a given ventilatory rate. It has been shown to reduce dynamic hyperinflation and alveolar pressure12 further and to improve gas exchange.49
If dynamic hyperinflation is excessive and causing circulatory compromise or risk of barotrauma, then minute ventilation should be decreased, hypercapnic acidosis accepted and spontaneous ventilation, which will only increase dynamic hyperinflation, should be discouraged by sedation. Muscle relaxants should be avoided unless essential. When dynamic hyperinflation is critical during controlled mechanical ventilation, PEEPi increases pulmonary hyperinflation and should not be applied.50
If dynamic hyperinflation is not excessive then spontaneous ventilation should be encouraged to promote ongoing respiratory muscle activity and to minimise wasting. Flow-by, pressure support and low-level CPAP may all reduce the work of spontaneous breathing and promote a better ventilatory pattern. CPAP approximately equal to the level of PEEPi is most commonly recommended.51 Care must be taken with all of these supports as each can increase dynamic hyperinflation by a different mechanism, leading to circulatory compromise or risk of barotrauma. Flow-by increases resistance through the expiratory valve, pressure support increases tidal volume and may increase inspiratory time, and CPAP reduces threshold load and makes ventilator triggering easier in patients with PEEPi.
Weaning from invasive mechanical ventilation
Approximately 6–20% of patients on IMV support fail weaning and place themselves in a high mortality and morbidity group44, 45 (see Ch. 31). Numerous criteria have been proposed to assess the capacity of the patient to wean;52 however, the predictive value of any of these individual criteria is limited. The simple criterion of patient respiration rate/tidal volume <100 breaths/min per litre had the best predictive value for weaning success, but the advantage of this overly simple clinical assessment during weaning is uncertain. Other indications to extubate COPD patients safely include  < 40%;
< 40%;  /
/ > 200, PEEP 5 cmH2O, cardiovascular stability, afebrile, pH > 7.35,
> 200, PEEP 5 cmH2O, cardiovascular stability, afebrile, pH > 7.35,  < 50 mmHg (6.5 kPa), GCS > 10 and, if available to be measured, static compliance >25 mL/cmH2O.44 Some patients unable to achieve these criteria may require weaning with
< 50 mmHg (6.5 kPa), GCS > 10 and, if available to be measured, static compliance >25 mL/cmH2O.44 Some patients unable to achieve these criteria may require weaning with  50–65 mmHg (6.5–8.45 kPa) with a bicarbonate level of >30 mmol/L allowed or encouraged to reduce the work of breathing and achieve a less abnormal pH. Following extubation, weaning can be continued with immediate placement upon NIV, which is associated with reduced re-intubation rates, lower ICU and hospital length of stay and mortality and morbidity.44, 45 Synchronisation of NIV, especially during sleep, is crucial and may require polysomnography.53
50–65 mmHg (6.5–8.45 kPa) with a bicarbonate level of >30 mmol/L allowed or encouraged to reduce the work of breathing and achieve a less abnormal pH. Following extubation, weaning can be continued with immediate placement upon NIV, which is associated with reduced re-intubation rates, lower ICU and hospital length of stay and mortality and morbidity.44, 45 Synchronisation of NIV, especially during sleep, is crucial and may require polysomnography.53
Tracheostomy
Tracheostomy may be beneficial in a small group of patients who have failed extubation despite NIV, or who have successfully weaned but are unable to adequately clear secretions, or who have required long-term ventilatory support. After 10 days of endotracheal intubation, the risk of laryngeal trauma and sepsis increases.
A tracheostomy allows long-term ventilatory support, sputum clearance, protection of the upper airway from oral secretions and, off mechanical ventilation, reduced dead space and upper-airway resistance. Compared with naso/orotracheal intubation, tracheostomy is much less intrusive and therefore less sedation is required. Also, it allows direct access to the large airways for the purpose of suctioning and bronchoscopy. However, patients are unable to generate sufficient upper-airway seal to cough, and as such may have ongoing atelectasis until tracheostomy removal and the development of an effective cough. Usually a nasoenteric feeding tube is required. Consider percutaneous endoscopic gastrostomy (PEG) tube feeding if long-term tracheostomy is being considered to avoid nasal trauma and infection and to reduce oesophagitis. Minimal occlusion tracheostomy cuff pressures (usually <20 cmH2O) should be checked 8-hourly. Adequate humidification and the use of tracheostomies with an inner cannula is recommended to allow for inner tube cleaning or replacement to avoid occlusion by dried secretions.
Consider removing the tracheostomy when:
-
•
the oxygenation requirement is low (e.g.
 < 40%)
< 40%) -
•
the patient does not require ventilatory support or requires only intermittent low-level ventilatory support and non-invasive ventilatory support is available
-
•
the patient is cooperative and has a good capacity to cough and can, for example, clear secretions via the tracheostomy tube
-
•
the patient has a low suction frequency requirement (<2–4-hourly).
Before tracheostomy removal, always ensure the patient is able to protect the upper airway from aspiration and can swallow safely and there is an absence of upper-airway obstruction (e.g. no granulation tissue or tracheal stenosis).
Post-intensive-unit care
Reassessment of potential precipating causes
COPD is commonly associated with cardiovascular disease, depression (and social isolation), and occult malignancy – all of which may need further management following an admission. Lung function assessment is crucial post admission and regular follow-up.3, 4
Assessment for long-term oxygen therapy should be undertaken ( < 55 mmHg (7.15 kPa), or <60 mmHg (7.8 kPa) with cor pulmonale) as there are two trials indicating a survival benefit.54, 55 Current smoking is a contraindication to domiciliary oxygen therapy due to the risk of fire. This can be checked by assessing carboxyhaemoglobin values on ABG (>2% suggests smoking) or urinary cotinine levels.
< 55 mmHg (7.15 kPa), or <60 mmHg (7.8 kPa) with cor pulmonale) as there are two trials indicating a survival benefit.54, 55 Current smoking is a contraindication to domiciliary oxygen therapy due to the risk of fire. This can be checked by assessing carboxyhaemoglobin values on ABG (>2% suggests smoking) or urinary cotinine levels.
Assessment of underlying obstructive sleep apnoea (COPD and OSA = overlap syndrome) should be considered. Treatment of this combination with CPAP is associated with an improved survival and exacerbation-free survival over a 9.5-year period according to a large, although uncontrolled, Spanish trial.56 Habitual snoring, witnessed apnoeas, obesity (BMI > 30), large neck size (>45 cm) and crowded oropharynx (Mallampati grade 3–4) provide clues of the possibility of underlying OSA.
Domiciliary nocturnal non-invasive ventilatory support
In COPD patients with chronic hypercapnia, avoidance of excessive domiciliary oxygen therapy is advised. Whether long-term domiciliary nocturnal NIV is required in this group is less clear. In the two largest studies,57, 58 improved physiology (sleep quality and ABG) were noted overnight without changes in FEV1 and a borderline improvement in survival. Long-term NIV has also been associated with improved ventilation perfusion matching.29 Patients may benefit from domiciliary NIV if they have the following: (a) confirmed COPD diagnosis with optimal medical treatment and reversal of coexistent medical problems, (b) chronic hypercapnia, (c) at least two admissions with acute acidotic hypercapnia that responded to NIV, (d) demonstration of sleep-related hypoventilation (e.g. total sleep time hypoxic ( < 90%) >30% plus a rise in
< 90%) >30% plus a rise in  of >5 mmHg (0.65 kPa)), (e) 1-month trial of domiciliary NIV with objective adherence and improved quality of life and (f) an improvement in physiological markers (e.g. awake
of >5 mmHg (0.65 kPa)), (e) 1-month trial of domiciliary NIV with objective adherence and improved quality of life and (f) an improvement in physiological markers (e.g. awake  or 6-minute walk distance).
or 6-minute walk distance).
Rehabilitation
Rehabilitation should be considered for all patients with COPD, particularly those following ARF. There are numerous randomised controlled trials showing improvements in exercise physiology, lung function, quality of life and reduced hospitalisation rates.59 The change in 6-minute walk distance with rehabilitation is a powerful predictor of improved survival and significant patient motivator.60
Vaccination and antibiotics
Two large trials have recently advocated the use of macrolide antibiotics (erythromycin16 or azithromycin17) for stable COPD. Both studies, conducted over a 12-month period, indicated a significant reduction in exacerbations, probably via anti-inflammatory and antibacterial effects. However, this benefit needed to be offset against potential for greater long-term microbiological resistance and side effects such as hearing loss. Vaccination should be considered in all patients with COPD when stable. Annual influenza and 5-yearly pneumococcal vaccination are recommended.4
Domiciliary oxygen
Based upon two studies conducted in the 1970s–80s indicating a mortality benefit,54, 55 supplemental oxygen should be provided to patients with advanced COPD who: (a) are optimally controlled medically, (b) do not smoke, and (c) have  < 55 mmHg (7.15 kPa) or
< 55 mmHg (7.15 kPa) or  < 60 mmHg (7.8 kPa) with cor pulmonale. Great caution should be undertaken to avoid excessive oxygen at home when stable (aim for overnight oximetry of 88–92%) and during acute exacerbations.8, 22, 23
< 60 mmHg (7.8 kPa) with cor pulmonale. Great caution should be undertaken to avoid excessive oxygen at home when stable (aim for overnight oximetry of 88–92%) and during acute exacerbations.8, 22, 23
Lung transplantation
Lung transplantation is another palliative surgical procedure for patients with advanced disabling COPD who are aged <65 years, are not ventilator dependent, are on less than 10 mg prednisolone/day and are free of significant coexistent disease.61 The current 1-, 2- and 5-year international survival figures are 75, 66 and 50% respectively. Common complications are systemic hypertension, bronchiolitis obliterans, acute rejection, viral infection with cytomegalovirus and neoplasms.
Prognosis
Patients with sufficiently severe COPD to warrant hospital admission incur an inpatient mortality of 8%, and 90-day mortality of 15% in the UK.8, 9 Predictors of mortality were performance status, age and admission urea, albumin, pH,  and
and  plus the presence of respiratory physicians involved in the care.62Although in-hospital mortality for hypercapnic COPD patients may reach 62%,63 in an Australian report in-hospital mortality for hypercapnic COPD patients treated with NIV was 11% and all deaths were with palliative intent, which followed time to allow for patient and family discussions.43 In Hong Kong, acute hypercapnic COPD patients have a 12-month re-admission rate of 80% and a 49% 1-year mortality.7 The body–mass index, air-flow obstruction, dyspnoea and exercise capacity (BODE) index is a 10-point scale made up from the following four variables: (1) body mass index, (2) air-flow obstruction, (3) severity of dyspnoea, and (4) exercise capacity, and has been found to be very useful in predicting survival in ambulatory patients with COPD6 (see Table 30.2).
plus the presence of respiratory physicians involved in the care.62Although in-hospital mortality for hypercapnic COPD patients may reach 62%,63 in an Australian report in-hospital mortality for hypercapnic COPD patients treated with NIV was 11% and all deaths were with palliative intent, which followed time to allow for patient and family discussions.43 In Hong Kong, acute hypercapnic COPD patients have a 12-month re-admission rate of 80% and a 49% 1-year mortality.7 The body–mass index, air-flow obstruction, dyspnoea and exercise capacity (BODE) index is a 10-point scale made up from the following four variables: (1) body mass index, (2) air-flow obstruction, (3) severity of dyspnoea, and (4) exercise capacity, and has been found to be very useful in predicting survival in ambulatory patients with COPD6 (see Table 30.2).
![]() Access the complete references list online at http://www.expertconsult.com
Access the complete references list online at http://www.expertconsult.com
References
- 4.Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi: 10.1016/S0140-6736(07)61382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pauwels RA, Buist AS, Calverley PM. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 8.Roberts CM, Stone RA, Buckingham RJ. Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations. Thorax. 2010;66(1):43–48. doi: 10.1136/thx.2010.153114. [DOI] [PubMed] [Google Scholar]
- 9.Chandra D, Stamm JA, Taylor B. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998-2008. Am J Respir Crit Care Med. 2012;185(2):152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malhotra A, Schwartz DR, Ayas N. Treatment of oxygen-induced hypercapnia. Lancet. 2001;357(9259):884–885. doi: 10.1016/s0140-6736(05)71817-1. [DOI] [PubMed] [Google Scholar]
- 38.Elliott MW, Nava S. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease: ‘Don't think twice, it's alright!’. Am J Respir Crit Care Med. 2012;185(2):121–123. doi: 10.1164/rccm.201111-1933ED. [DOI] [PubMed] [Google Scholar]
References
- 1.Buist AS, McBurnie MA, Vollmer WM. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 2.Devereux G. ABC of chronic obstructive pulmonary disease. Definition, epidemiology, and risk factors. BMJ (Clinical research edn) 2006;332(7550):1142–1144. doi: 10.1136/bmj.332.7550.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niewoehner DE. Clinical practice. Outpatient management of severe COPD. New Engl J Med. 2010;362(15):1407–1416. doi: 10.1056/NEJMcp0912556. [DOI] [PubMed] [Google Scholar]
- 4.Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi: 10.1016/S0140-6736(07)61382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pauwels RA, Buist AS, Calverley PM. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 6.Celli BR, Cote CG, Marin JM. The body–mass index, air flow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. New Engl J Med. 2004;350(10):1005–1012. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 7.Chu CM, Chan VL, Lin AW. Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax. 2004;59(12):1020–1025. doi: 10.1136/thx.2004.024307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roberts CM, Stone RA, Buckingham RJ. Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations. Thorax. 2010;66(1):43–48. doi: 10.1136/thx.2010.153114. [DOI] [PubMed] [Google Scholar]
- 9.Chandra D, Stamm JA, Taylor B. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998-2008. Am J Respir Crit Care Med. 2012;185(2):152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Britton JR, Pavord ID, Richards KA. Dietary antioxidant vitamin intake and lung function in the general population. Am J Respir Crit Care Med. 1995;151(5):1383–1387. doi: 10.1164/ajrccm.151.5.7735589. [DOI] [PubMed] [Google Scholar]
- 11.Abroug F, Ouanes-Besbes L, Nciri N. Association of left-heart dysfunction with severe exacerbation of chronic obstructive pulmonary disease: diagnostic performance of cardiac biomarkers. Am J Respir Crit Care Med. 2006;174(9):990–996. doi: 10.1164/rccm.200603-380OC. [DOI] [PubMed] [Google Scholar]
- 12.Tuxen DV, Lane S. The effects of ventilatory pattern on hyperinflation, airway pressures, and circulation in mechanical ventilation of patients with severe air-flow obstruction. Am Rev Respir Dis. 1987;136(4):872–879. doi: 10.1164/ajrccm/136.4.872. [DOI] [PubMed] [Google Scholar]
- 13.Aubier M, Murciano D, Lecocguic Y. Effect of hypophosphatemia on diaphragmatic contractility in patients with acute respiratory failure. New Engl J Med. 1985;313(7):420–424. doi: 10.1056/NEJM198508153130705. [DOI] [PubMed] [Google Scholar]
- 14.Aubier M, Viires N, Piquet J. Effects of hypocalcemia on diaphragmatic strength generation. J Appl Physiol. 1985;58(6):2054–2061. doi: 10.1152/jappl.1985.58.6.2054. [DOI] [PubMed] [Google Scholar]
- 15.Seemungal TA, Wilkinson TM, Hurst JR. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2008;178(11):1139–1147. doi: 10.1164/rccm.200801-145OC. [DOI] [PubMed] [Google Scholar]
- 16.Albert RK, Connett J, Bailey WC. Azithromycin for prevention of exacerbations of COPD. New Engl J Med. 2011;365(8):689–698. doi: 10.1056/NEJMoa1104623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barr RG, Bluemke DA, Ahmed FS. Percent emphysema, air flow obstruction, and impaired left ventricular filling. New Engl J Med. 2010;362(3):217–227. doi: 10.1056/NEJMoa0808836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum GL, Schwartz A, Llamas R. Left ventricular function in chronic obstructive lung disease. New Engl J Med. 1971;285(7):361–365. doi: 10.1056/NEJM197108122850701. [DOI] [PubMed] [Google Scholar]
- 19.Robertson CH, Jr, Pagel MA, Johnson RL., Jr The distribution of blood flow, oxygen consumption, and work output among the respiratory muscles during unobstructed hyperventilation. J Clin Invest. 1977;59(1):43–50. doi: 10.1172/JCI108620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malhotra A, Schwartz DR, Ayas N. Treatment of oxygen-induced hypercapnia. Lancet. 2001;357(9259):884–885. doi: 10.1016/s0140-6736(05)71817-1. [DOI] [PubMed] [Google Scholar]
- 21.Austin MA, Wills KE, Blizzard L. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ (Clinical research edn) 2010;341:c5462. doi: 10.1136/bmj.c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joosten SA, Koh MS, Bu X. The effects of oxygen therapy in patients presenting to an emergency department with exacerbation of chronic obstructive pulmonary disease. Med J Austral. 2007;186(5):235–238. doi: 10.5694/j.1326-5377.2007.tb00879.x. [DOI] [PubMed] [Google Scholar]
- 23.Fahey PJ, Hyde RW. ‘Won't breathe’ vs ‘can't breathe’. Detection of depressed ventilatory drive in patients with obstructive pulmonary disease. Chest. 1983;84(1):19–25. doi: 10.1378/chest.84.1.19. [DOI] [PubMed] [Google Scholar]
- 24.Kato S, Nakamoto T, Iizuka M. Early diagnosis and estimation of pulmonary congestion and edema in patients with left-sided heart diseases from histogram of pulmonary CT number. Chest. 1996;109(6):1439–1445. doi: 10.1378/chest.109.6.1439. [DOI] [PubMed] [Google Scholar]
- 25.Schneider HG, Lam L, Lokuge A. B-type natriuretic peptide testing, clinical outcomes, and health services use in emergency department patients with dyspnea: a randomised trial. Ann Intern Med. 2009;150(6):365–371. doi: 10.7326/0003-4819-150-6-200903170-00004. [DOI] [PubMed] [Google Scholar]
- 26.Lim BL, Kelly AM. A meta-analysis on the utility of peripheral venous blood gas analyses in exacerbations of chronic obstructive pulmonary disease in the emergency department. Eur J Emerg Med. 2010;17(5):246–248. doi: 10.1097/MEJ.0b013e328335622a. [DOI] [PubMed] [Google Scholar]
- 27.Bone RC, Pierce AK, Johnson RL., Jr Controlled oxygen administration in acute respiratory failure in chronic obstructive pulmonary disease: a reappraisal. Am J Med. 1978;65(6):896–902. doi: 10.1016/0002-9343(78)90740-4. [DOI] [PubMed] [Google Scholar]
- 28.Salpeter SR, Buckley NS, Salpeter EE. Meta-analysis: anticholinergics, but not beta-agonists, reduce severe exacerbations and respiratory mortality in COPD. Gen Intern Med. 2006;21(10):1011–1019. doi: 10.1111/j.1525-1497.2006.00507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Backer L, Vos W, Dieriks B. The effects of long-term noninvasive ventilation in hypercapnic COPD patients: a randomized controlled pilot study. Int J Chron Obstruct Pulmon Dis. 2011;6:615–624. doi: 10.2147/COPD.S22823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Albert RK, Martin TR, Lewis SW. Controlled clinical trial of methylprednisolone in patients with chronic bronchitis and acute respiratory insufficiency. Ann Intern Med. 1980;92(6):753–758. doi: 10.7326/0003-4819-92-6-753. [DOI] [PubMed] [Google Scholar]
- 31.Rubini F, Rampulla C, Nava S. Acute effect of corticosteroids on respiratory mechanics in mechanically ventilated patients with chronic air flow obstruction and acute respiratory failure. Am J Respir Crit Care Med. 1994;149(2 Pt 1):306–310. doi: 10.1164/ajrccm.149.2.8306023. [DOI] [PubMed] [Google Scholar]
- 32.Aubier M, De Troyer A, Sampson M. Aminophylline improves diaphragmatic contractility. New Engl J Med. 1981;305(5):249–252. doi: 10.1056/NEJM198107303050503. [DOI] [PubMed] [Google Scholar]
- 33.Berry RB, Desa MM, Branum JP. Effect of theophylline on sleep and sleep-disordered breathing in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1991;143(2):245–250. doi: 10.1164/ajrccm/143.2.245. [DOI] [PubMed] [Google Scholar]
- 34.Rice KL, Leatherman JW, Duane PG. Aminophylline for acute exacerbations of chronic obstructive pulmonary disease. A controlled trial. Ann Intern Med. 1987;107(3):305–309. doi: 10.7326/0003-4819-107-2-305. [DOI] [PubMed] [Google Scholar]
- 35.Guyatt GH, Townsend M, Pugsley SO. Bronchodilators in chronic air-flow limitation. Effects on airway function, exercise capacity, and quality of life. Am Rev Respir Dis. 1987;135(5):1069–1074. doi: 10.1164/arrd.1987.135.5.1069. [DOI] [PubMed] [Google Scholar]
- 36.Dhingra S, Solven F, Wilson A. Hypomagnesemia and respiratory muscle power. Am Rev Respir Dis. 1984;129(3):497–498. doi: 10.1164/arrd.1984.129.3.497. [DOI] [PubMed] [Google Scholar]
- 37.Petty TL. The National Mucolytic Study. Results of a randomized, double-blind, placebo-controlled study of iodinated glycerol in chronic obstructive bronchitis. Chest. 1990;97(1):75–83. doi: 10.1378/chest.97.1.75. [DOI] [PubMed] [Google Scholar]
- 38.Elliott MW, Nava S. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease: ‘Don't think twice, it's alright!’. Am J Respir Crit Care Med. 2012;185(2):121–123. doi: 10.1164/rccm.201111-1933ED. [DOI] [PubMed] [Google Scholar]
- 39.Brochard L, Mancebo J, Wysocki M. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. New Engl J Med. 1995;333(13):817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 40.Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355(9219):1931–1935. doi: 10.1016/s0140-6736(00)02323-0. [DOI] [PubMed] [Google Scholar]
- 41.Lightowler JV, Wedzicha JA, Elliott MW. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ (Clinical research edn) 2003;326(7382):185. doi: 10.1136/bmj.326.7382.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keenan SP, Sinuff T, Cook DJ. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive-pressure ventilation? A systematic review of the literature. Ann Intern Med. 2003;138(11):861–870. doi: 10.7326/0003-4819-138-11-200306030-00007. [DOI] [PubMed] [Google Scholar]
- 43.Crummy F, Buchan C, Miller B. The use of noninvasive mechanical ventilation in COPD with severe hypercapnic acidosis. Respir Med. 2007;101(1):53–61. doi: 10.1016/j.rmed.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 44.Ferrer M, Sellares J, Valencia M. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. 2009;374(9695):1082–1088. doi: 10.1016/S0140-6736(09)61038-2. [DOI] [PubMed] [Google Scholar]
- 45.Burns KE, Adhikari NK, Keenan SP. Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. BMJ (Clinical research edn) 2009;338:b1574. doi: 10.1136/bmj.b1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Antonelli M, Conti G, Rocco M. A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. New Engl J Med. 1998;339(7):429–435. doi: 10.1056/NEJM199808133390703. [DOI] [PubMed] [Google Scholar]
- 47.Mehta S, Hill NS. Noninvasive ventilation. Am J Respir Crit Care Med. 2001;163(2):540–577. doi: 10.1164/ajrccm.163.2.9906116. [DOI] [PubMed] [Google Scholar]
- 48.Menzies R, Gibbons W, Goldberg P. Determinants of weaning and survival among patients with COPD who require mechanical ventilation for acute respiratory failure. Chest. 1989;95(2):398–405. doi: 10.1378/chest.95.2.398. [DOI] [PubMed] [Google Scholar]
- 49.Connors AF, Jr, McCaffree DR, Gray BA. Effect of inspiratory flow rate on gas exchange during mechanical ventilation. Am Rev Respir Dis. 1981;124(5):537–543. doi: 10.1164/arrd.1981.124.5.537. [DOI] [PubMed] [Google Scholar]
- 50.Tuxen DV. Detrimental effects of positive end-expiratory pressure during controlled mechanical ventilation of patients with severe air flow obstruction. Am Rev Respir Dis. 1989;140(1):5–9. doi: 10.1164/ajrccm/140.1.5. [DOI] [PubMed] [Google Scholar]
- 51.Baigorri F, de Monte A, Blanch L. Hemodynamic responses to external counterbalancing of auto-positive end-expiratory pressure in mechanically ventilated patients with chronic obstructive pulmonary disease. Crit Care Med. 1994;22(11):1782–1791. [PubMed] [Google Scholar]
- 52.Esteban A, Frutos F, Tobin MJ. A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. New Engl J Med. 1995;332(6):345–350. doi: 10.1056/NEJM199502093320601. [DOI] [PubMed] [Google Scholar]
- 53.Vignaux L, Vargas F, Roeseler J. Patient-ventilator asynchrony during non-invasive ventilation for acute respiratory failure: a multicenter study. Intensive Care Med. 2009;35(5):840–846. doi: 10.1007/s00134-009-1416-5. [DOI] [PubMed] [Google Scholar]
- 54.Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Nocturnal Oxygen Therapy Trial Group. Ann Intern Med. 1980;93(3):391–398. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 55.[No authors listed] Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet. 1981;1(8222):681–686. [PubMed] [Google Scholar]
- 56.Marin JM, Soriano JB, Carrizo SJ. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325–331. doi: 10.1164/rccm.200912-1869OC. [DOI] [PubMed] [Google Scholar]
- 57.Clini E, Sturani C, Rossi A. The Italian multicentre study on noninvasive ventilation in chronic obstructive pulmonary disease patients. Eur Respir J. 2002;20(3):529–538. doi: 10.1183/09031936.02.02162001. [DOI] [PubMed] [Google Scholar]
- 58.McEvoy RD, Pierce RJ, Hillman D. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax. 2009;64(7):561–566. doi: 10.1136/thx.2008.108274. [DOI] [PubMed] [Google Scholar]
- 59.Goldstein RS, Gort EH, Stubbing D. Randomised controlled trial of respiratory rehabilitation. Lancet. 1994;344(8934):1394–1397. doi: 10.1016/s0140-6736(94)90568-1. [DOI] [PubMed] [Google Scholar]
- 60.Rasekaba T, Lee AL, Naughton MT. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39(8):495–501. doi: 10.1111/j.1445-5994.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- 61.Orens JB, Estenne M, Arcasoy S. International guidelines for the selection of lung transplant candidates: 2006 update – a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006;25(7):745–755. doi: 10.1016/j.healun.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 62.Price LC, Lowe D, Hosker HS. UK National COPD Audit 2003: Impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax. 2006;61(10):837–842. doi: 10.1136/thx.2005.049940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Squadrone E, Frigerio P, Fogliati C. Noninvasive vs invasive ventilation in COPD patients with severe acute respiratory failure deemed to require ventilatory assistance. Intensive Care Med. 2004;30(7):1303–1310. doi: 10.1007/s00134-004-2320-7. [DOI] [PubMed] [Google Scholar]


