This cross-sectional study assesses cardiac structure and function in elite female basketball players.
Key Points
Question
What is the spectrum of cardiac remodeling in elite female basketball players?
Findings
In this cross-sectional echocardiographic study of 140 Women's National Basketball Association athletes with mean body surface area of 2.02 m2, left ventricular enlargement was present in 26.0% and right ventricular enlargement in 42.2% of athlete and maximal left ventricular wall thickness was 1.0 cm or greater in 55.7% and greater than 1.3 cm in 0.7% of athletes; 16.0% of athletes met criteria for left ventricular hypertrophy, mean aortic root diameter was 3.1 cm, and only 1.4% of athletes had guideline-defined aortic enlargement.
Meaning
In this study, increased cardiac dimensions except for aortic root were frequently present in Women’s National Basketball Association athletes.
Abstract
Importance
There is a paucity of data detailing cardiac remodeling in female athletes compared with male athletes. The lack of reference cardiac data for elite female basketball players or female athletes of similar size makes it difficult to differentiate athletic remodeling from potential underlying cardiac disorders in this population of athletes.
Objective
To assess cardiac structure and function in elite female basketball players.
Design, Setting, and Participants
This cross-sectional echocardiographic study included 140 Women's National Basketball Association (WNBA) athletes on active rosters for the 2017 season. The WNBA mandates annual preseason stress echocardiograms for each athlete. The WNBA has partnered with Columbia University to annually perform a review of these studies. Data analysis was performed from June 7, 2017, to October 5, 2017.
Main Outcomes and Measures
Echocardiographic variables included left ventricular (LV) dimensions, wall thickness, mass, prevalence of LV hypertrophy, aortic dimensions, right ventricular (RV) dimension, and right and left atrial size. Linear regression was used to assess the associations between cardiac structure and function with body size quantified as body surface area (BSA) in the primary analysis.
Results
A total of 140 female athletes (mean [SD] age, 26.8 [3.9] years; 105 [75.0%] African American) participated in the study. Mean (SD) athlete height was 183.4 (9.0) cm, and mean (SD) BSA was 2.02 (0.18) m2. Compared with guideline-defined normal values, LV enlargement was present in 36 athletes (26.0%) and 57 athletes (42.2%) had RV enlargement. There was a linear correlation between LV and RV cavity sizes and BSA extending to the uppermost biometrics (LV cavity size: r, 0.48; RV cavity size: r, 0.32; P < .001 for both). Maximal left ventricular wall thickness (LVWT) ranged from 0.6 to 1.4 cm, with 78 athletes (55.7%) having LVWT of 1.0 cm or greater and only 1 athlete (0.7%) having LVWT greater than 1.3 cm. Twenty-three athletes (16.4%) met the criteria for left ventricular hypertrophy (LVH) (>95 g/m2). Eccentric LVH was present in 16 athletes (69.6%), concentric LVH in 7 athletes (30.4%), and concentric remodeling in 27 athletes (19.3%). Mean aortic root diameter was 3.1 cm (95% CI, 3.0-3.2). Only 2 athletes (1.4%) had guideline-defined aortic enlargement compared with a range of 18% to 42% for left and right ventricular and atrial enlargement.
Conclusions and Relevance
In this study, increased cardiac dimensions were frequently observed in WNBA athletes. Both BSA and physiologic remodeling affected cardiac morphologic findings. This study may provide a framework to define the range of athletic cardiac remodeling exhibited by elite female basketball players.
Introduction
Cardiac remodeling frequently develops in response to the hemodynamic demands of intensive athletic training. Increased left ventricular (LV) mass caused by mild LV chamber enlargement and/or increased wall thickness has been consistently described in athletes engaged in a wide variety of sporting disciplines.1,2,3,4 A study by Engel et al5 reported the findings of an echocardiographic analysis in a large cohort of male professional basketball players. A detailed description of athletic cardiac remodeling in this athlete group is important because basketball is a leading sport globally and youth and collegiate basketball players have been reported to have a higher incidence of sudden cardiac death compared with other athlete groups.6,7 Hypertrophic cardiomyopathy is a prominent cause of exercise-triggered sudden cardiac death. Thus, reference data that help to differentiate cardiac remodeling due to intensive athletic training from similar cardiac structural changes associated with hypertrophic cardiomyopathy and other cardiomyopathies are clinically important in basketball players.6,7
Women are underrepresented in the echocardiographic studies that assess the cardiac morphologic changes associated with athletic training. They comprise a smaller proportion of competitive athletes, which may partially account for a smaller number of sport-related sudden cardiac death events.6,7 However, the increasing participation of women in sports previously dominated by men has heightened the need to understand and distinguish physiologic remodeling from potential underlying cardiac disorders in female athletes. Few large-scale echocardiographic analyses4,8,9 of large numbers of female athletes have been performed. These studies4,8,9 collectively examined female athletes participating in a wide variety of sporting disciplines. Basketball players and other female athletes of similar size comprise only a small proportion of the population of athletes examined. Thus, no large-scale or sport-specific reference echocardiographic data are currently available for female basketball players. We assessed the phenotypic characterization of cardiac structure and function associated with athletic training in a large cohort of female professional basketball players in the Women's National Basketball Association (WNBA).
Methods
Study Participants
This cross-sectional echocardiographic study included WNBA athletes on active rosters for the 2017 season. The policies of the WNBA mandate that each athlete on a team roster undergo an annual rest and exercise stress echocardiogram as part of the annual cardiac screening examination requirement. The review and analysis of the echocardiograms for this study were approved by the WNBA, the Women's National Basketball Players Association, and the institutional review board of Columbia University Irving Medical Center. All echocardiographic data were deidentified. Pursuant to approval from the institutional review board of Columbia University Irving Medical Center, informed consent was not required for this study because echocardiograms were obtained as part of the routine evaluation of all athletes, anonymized, and analyzed retrospectively.
The 2017 preseason echocardiograms performed by WNBA team–affiliated physicians were sent in digital format to Columbia University Irving Medical Center for core laboratory review and analysis via a league-wide electronic medical records system. Among the 144 athletes on active rosters during the 2017 WNBA season, 140 athletes with adequate echocardiographic images for research analysis were included in this study. Race/ethnicity of athletes was determined by the investigators.
Echocardiographic Analysis
Transthoracic echocardiograms were performed using commercially available systems. All 2-dimensional measurements were completed in accordance with the American Society of Echocardiography (ASE) and European Association of Cardiovascular Imaging (EACI) guidelines on chamber quantification.10 Left ventricular end-diastolic diameter (LVEDD), interventricular septum and inferolateral wall thickness (LVWT), left atrial (LA) anteroposterior diameter, and aortic root diameter were measured from the parasternal long axis view. Aortic dimensions were measured using leading edge to leading edge technique. Left atrial volume was calculated using the biplane area-length method. Right atrial volume was calculated using a single-plane measurement in the apical 4 chambers. The left ventricular ejection fraction (LVEF) was calculated using the modified Simpson biplane method in 128 athletes (91.4%) with technically adequate views and was visually estimated in 12 patients (8.6%). Right ventricular (RV) basal and midventricular diameter were measured in an apical 4-chamber RV-focused view. In accordance with guideline recommendations, chamber dimensions and LV mass were indexed to body surface area (BSA) (square root [height (cm) × weight (kg)]/3600). Left ventricular hypertrophy (LVH) was defined as left ventricular mass index (LVMI) greater than 95 g/m.2,10 Left ventricular relative wall thickness (RWT) was calculated as [2 × (inferolateral wall thickness)/LVEDD]. Diastolic function was assessed using the ASE and EACI algorithm.11
A single reader (S.S.) analyzed all echocardiograms in this study. Reproducibility was assessed using 20 echocardiograms in which core dimensions were measured and intraclass correlation coefficients were calculated for each measure. The intraclass correlation coefficients were 99% for LVEDD, 96% for aortic root diameter, and 91% for RV basal dimension. The mean intraobserver difference was 0.15 mm for LVEDD, 0.35 mm for aortic root diameter, and 0.7 mm for RV basal dimension. A second reader (D.J.E.) independently analyzed a random subset of 20 echocardiograms to quantify interreader variability. The intraclass correlation coefficients were 96% for LVEDD, 97% for aortic root diameter, and 95% for RV basal diameter (eFigures 1-3 in the Supplement).
Statistical Analysis
Continuous variables are presented as mean (SD) and mean (95% CI). Categorical variables are presented as number (percentage). Kolmogorov-Smirnov tests were performed to assess the normality of all variables. Skewed data were log transformed, and the transformed data were used for all analyses. To allow for the most flexible possible associations between measures of cardiac structure and body size, cubic spline models were applied, and Wald tests were used to assess the overall associations and whether the associations deviated from linearity. Linear regression was used to assess the associations between cardiac structure and function with body size quantified as BSA in the primary analysis. In secondary analyses, the associations with height (in centimeters, square centimeters, and centimeters to 2.7 power) were also examined. We tested for interactions among all 4 cardiac chamber dimensions, LV mass, and aortic root dimension with race/ethnicity. This subgroup analysis was confined to African American and white athletes given well-established data characterizing differences in cardiac athletic remodeling in male African American and white athletes12,13 and the small number of nonwhite or non–African American athletes (5 [3.5%]). Scatterplots with a Pearson product-moment correlation were performed to quantify the associations between cardiac structure and body size.
A 2-sided P < .05 was the threshold for statistical significance. Statistical analyses were performed using STATA/MP, version 15.1 (StataCorp LLC). Data analysis was performed from June 7, 2017, to October 5, 2017.
Results
Characterization of the Study Population
A total of 140 female athletes (mean [SD] age, 26.8 [3.9] years; 105 [75.0%] African American) participated in the study. Table 1 gives the baseline characteristics of the study population. The mean (SD) athlete height was 183.4 (9.0) cm, mean (SD) weight was 79.6 (11.8) kg, and mean (SD) BSA was 2.02 (0.18) m2. Mean (SD) resting blood pressures were 116 (11)/70 (8) mm Hg, and mean (SD) heart rate was 56/min (9/min).
Table 1. Characteristics of WNBA Athletes Overall and Stratified by Race/Ethnicity.
| Characteristic | Overall, mean (SD) [range] (N = 140) | Mean (SD) | P valuea | |
|---|---|---|---|---|
| African American (n = 105) | White (n = 30) | |||
| Age, y | 26.8 (3.9) [21-37] | 26.9 (3.7) | 26.7 (4.3) | .81 |
| Height, cm | 183.4 (9.0) [147-201] | 183.4 (8.8) | 183.5 (9.7) | .98 |
| Weight, kg | 79.6 (11.8) [54.9-127.0] | 80.0 (12.2) | 79.1 (10.6) | .73 |
| BSA, m2 | 2.02 (0.18) [1.62-2.51] | 2.02 (0.18) | 2.01 (0.17) | .68 |
| Heart rate, /min | 56.4 (8.6) [40-90] | 57.3 (9.0) | 53.6 (6.4) | .04 |
| Blood pressure, mm Hg | ||||
| Systolic | 115.6 (10.7) [96-147] | 115.4 (11.4) | 115.1 (7.9) | .92 |
| Diastolic | 70.3 (8.0) [49-92] | 70.2 (8.5) | 70.8 (6.8) | .76 |
Abbreviations: BSA, body surface area (calculated as the square root of [height in centimeters × weight in kilograms]/3600); WNBA, Women’s National Basketball Association.
P value is for the comparison between African American and white athlete groups.
Ventricular and Atrial Dimensions in WNBA Athletes
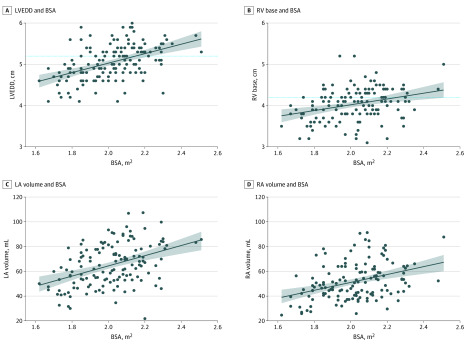
Ventricular and atrial dimensions in the WNBA athletes are presented in Table 2. The LVEDD ranged from 4.1 to 6.0 cm (mean LVEDD, 5.0 cm; 95% CI, 5.0-5.1 cm), and 36 players (26.0%) had LV dilation defined as LVEDD greater than 5.2 cm by ASE guidelines. Although a significant number of players had LV dilation, LV cavity sizes were predominately normal compared with reference female adult sizes when adjusted for BSA except for in 1 player who had an indexed LVEDD of 3.2 cm/m2 (3.1 cm/m2 being the upper range of normal).10 We found a positive linear association between LVEDD and BSA in the athlete group (r, 0.48; P < .001) (Figure 1A). The RV basal dimension was measured in 135 athletes and ranged from 3.1 to 5.2 cm (mean RV basal diameter, 4.0 cm; 95% CI, 4.0-4.1 cm). Fifty-seven athletes (42.2%) had an enlarged basal RV dimension greater than 4.1 cm, and the linear association between the RV basal dimension and BSA was weakly correlated (r, 0.32; P < .001) (Figure 1B).
Table 2. Distribution of Echocardiographic Findings in WNBA Athletes.
| Variable | Mean (95% CI) | Percentile | ||||
|---|---|---|---|---|---|---|
| 10% | 25% | 50% | 75% | 90% | ||
| Left ventricle | ||||||
| LVEDD, cm | 5.0 (5.0-5.1) | 4.6 | 4.8 | 5.0 | 5.4 | 5.6 |
| LVESD, cm | 3.4 (3.3-3.4) | 2.9 | 3.1 | 3.3 | 3.7 | 3.9 |
| Maximum LVWT, cm | 0.99 (0.97-1.01) | |||||
| LVM, g | 170.2 (164.3-176.0) | 123.9 | 148.1 | 167.7 | 192.2 | 212 |
| LVMI, g/m2 | 84.1 (81.7-86.5) | 66.2 | 75.1 | 84.3 | 93.4 | 100.4 |
| RWT, cm | 0.39 (0.38-0.40) | 0.32 | 0.35 | 0.38 | 0.42 | 0.48 |
| LVEF, % | 55.7 (55.1-56.3) | 0.51 | 0.53 | 0.56 | 0.58 | 0.60 |
| Normal geometry, No./total No. (%) | 90/140 (64.3) | |||||
| Concentric, No./total No. (%) | ||||||
| Remodeling | 27/140 (19.3) | NA | NA | NA | NA | NA |
| Hypertrophy | 7/140 (5.0) | NA | NA | NA | NA | NA |
| Eccentric hypertrophy, No./total No. (%) | 16/140 (11.4) | NA | NA | NA | NA | NA |
| Right ventricle | ||||||
| RV basal diameter, cm | 4.0 (4.0-4.1) | 3.5 | 3.8 | 4.1 | 4.3 | 4.5 |
| Atria | ||||||
| Left atrium | ||||||
| Diameter, cm | 3.4 (3.3-3.5) | 2.9 | 3.1 | 3.4 | 3.7 | 4.0 |
| Volume, mL | 65.1 (62.2-67.9) | 43.9 | 53.2 | 64.4 | 78.2 | 86.4 |
| Volume index, mL/m2 | 32.6 (31.2-33.9) | 23.0 | 26.4 | 31.5 | 37.5 | 43.4 |
| Right atrium | ||||||
| Volume, mL | 51.6 (49.0-54.1) | 35.74 | 40.72 | 48.80 | 61.76 | 74.16 |
| Volume index, mL/m2 | 25.5 (24.4-26.7) | 17.74 | 20.26 | 24.92 | 28.88 | 35.16 |
| Aorta | ||||||
| Root, cm | 3.1 (3.0-3.2) | 2.7 | 2.9 | 3.1 | 3.3 | 3.6 |
| Ascending, cm | 2.8 (2.8-2.9) | 2.5 | 2.6 | 2.8 | 3.0 | 3.2 |
| Transverse, cm | 2.5 (2.5-2.6) | 2.1 | 2.3 | 2.5 | 2.8 | 2.9 |
Abbreviations: LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic diameter; LVM, left ventricular mass; LVMI, left ventricular mass indexed to body surface area; LVWT, left ventricular wall thickness; NA, not applicable; RV, right ventricle; RWT, relative wall thickness; WNBA, Women’s National Basketball Association.
Figure 1. Associations Between Cardiac Chamber Size and Body Surface Area (BSA).
Solid lines represent the fitted mean values of cardiac dimensions compared with BSA, shaded areas representing 95% CIs. Dotted lines represent the American Society of Echocardiography (ASE) cutoffs for normal ventricular dimensions. A, The ASE cutoff for left ventricular end-diastolic diameter (LVEDD) was 5.2 cm. B, The ASE cutoff for right ventricular (RV) basal diameter was 4.2 cm. LA indicates left atrial; RA, right atrial.
The LA diameter ranged from 1.7 to 4.6 cm (mean LA diameter, 3.4 cm; 95% CI, 3.3-3.5), and there was a correlation between LA volume and BSA (r, 0.43; P < .001) (Figure 1C). The mean LA volume index was 32.6 mL/m2 (95% CI, 31.2-33.9 mL/m2); LA enlargement (LA volume index >34.0 mL/m2) was present in 57 athletes (40.7%). The mean RA volume index was 25.5 mL/m2 (95% CI, 24.4-26.7 mL/m2) and was correlated with BSA (r, 0.38; P < .001) (Figure 1D). The RA enlargement (defined as RA volume index >33 mL/m2) was present in 25 athletes (18.2%).
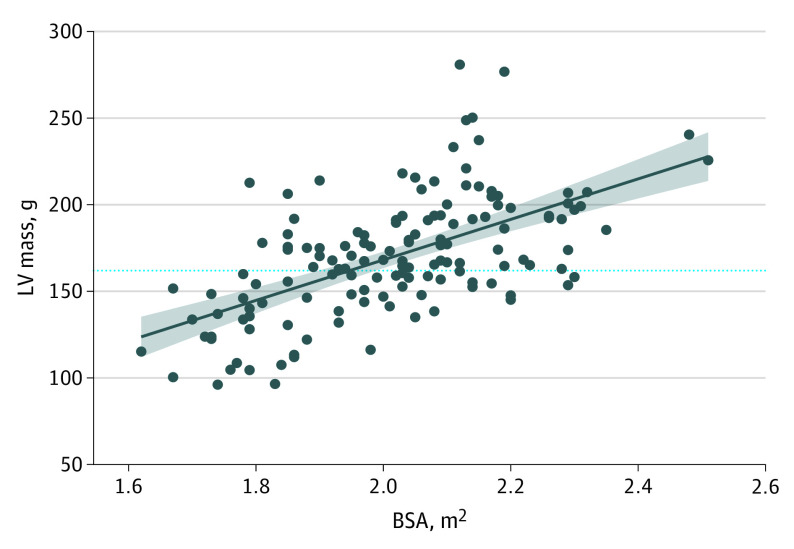
LV Remodeling
Maximal LV wall thickness (LVWT) ranged from 0.7 to 1.4 cm, with a mean (SD) interventricular septal thickness of 0.9 (0.1) and a mean (SD) posterior wall thickness of 1.0 (0.1) cm, with 78 athletes (55.7%) having an LVWT of 1.0 cm or greater and only 1 athlete (0.7%) having an LVWT greater than 1.3 cm. There was a linear association of LV mass with BSA (r, 0.59; P < .001) (Figure 2). Mean LVMI was 84.1 g/m2 (95% CI, 81.7-86.5 g/m2), with 23 athletes (16.4%) meeting the ASE criteria for LVH (>95 g/m2). Of the athletes with LVH, 16 (69.6%) had eccentric LVH and 7 (30.4%) had concentric LVH. Of the remaining athletes with normal LV mass, 27 (23.1%) had concentric remodeling and 90 (76.9%) had normal LV geometry.
Figure 2. Association Between Left Ventricular (LV) Mass and Body Surface Area (BSA).
Solid line represents the fitted mean value for LV mass compared with BSA, with shaded areas representing 95% CIs. The dotted line represents the American Society of Echocardiography cutoff for normal LV mass of 162 g.
LV Function
The LVEF in WNBA athletes ranged from 44% to 65%, with a mean LVEF of 55.7% (95% CI, 55.1%-56.3%). Twenty-one athletes (15.0%) had resting LVEF less than 52%, and 4 (2.9%) had LVEF less than 50%; all of these athletes demonstrated normal augmentation of LV systolic function after exercise stress testing. The LV diastolic function was normal at rest in all athletes.
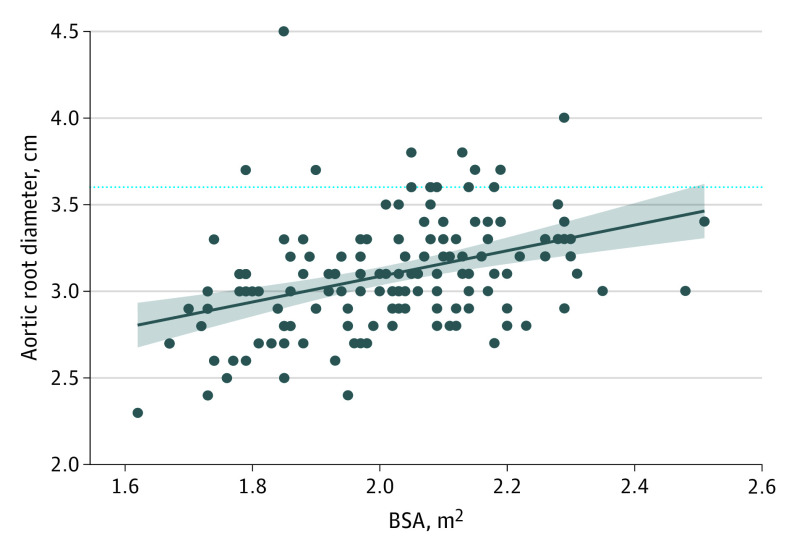
Aortic Dimensions
The aortic root diameter ranged from 2.3 to 4.5 cm (mean aortic root diameter, 3.1 cm; 95% CI, 3.0-3.2), with 9 athletes (6.4%) meeting the criteria for aortic root enlargement by ASE criteria (aortic root diameter >3.7 cm). Only 2 athletes (1.4%) had an aortic root diameter of 4.0 cm or greater, and 1 athlete had a bicuspid aortic valve with borderline normal aortic root dimension (3.7 cm). The aortic root had a positive association with BSA (r, 0.41; P < .001) (Figure 3). In contrast to our findings for ventricular size and mass, the fitted mean and 95% CI for aortic root diameter remained within the ASE guideline reference range across the spectrum of BSA for WNBA athletes (Figure 3).
Figure 3. Association Between Aortic Root Diameter and Body Surface Area (BSA).
Solid line represents the fitted mean value for aortic root diameter compared with BSA, with shaded areas representing 95% CIs. The dotted line represents the American Society of Echocardiography cutoff for normal aortic root diameter of 3.6 cm for women.
Associations Between Cardiac Structure and Function and Body Size
In accordance with ASE guidelines, all cardiac dimensions were indexed to BSA. In sensitivity analyses, we additionally examined the associations between cardiac dimensions and height. In this group of female athletes, we found that BSA compared with alternative indexing methods that account exclusively for height correlated best with all cardiac chamber and aortic sizes.
Racial/Ethnic Variation in the Associations Between Cardiac Structure and Function
In comparing cardiac dimensions by race/ethnicity, white athletes had larger LVEDD (mean LVEDD, 5.2 cm [95% CI, 5.1-5.4 cm] vs 5.0 [95% CI, 5.0-5.1 cm] cm; P = .03) and aortic root diameter (mean aortic root diameter, 3.2 cm [95% CI, 3.1-3.4 cm] vs 3.1 cm [95% CI, 3.0-3.1 cm]; P = .02). The eTable in the Supplement gives the other echocardiographic findings of the study participants.
Discussion
This is the first study, to our knowledge, to assess the cardiac adaptations associated with intense physical training among elite female basketball players. Our study differs from the few previously published echocardiographic examinations of female athlete groups in that the athletes in the current study were predominately African American (75.0%) and had significantly larger heights and BSA. In addition, because the study focused on a single-sport study rather than being a pooled analysis of athletes engaged in multiple sports, the cardiac data represent adaptation to similar physiologic demands. The results provide important additive cardiac reference data for female athletes and, to our knowledge, are the only such reference data for female basketball players.
We observed that LV cavity sizes in WNBA athletes were similar to those previously reported in mixed-sport, white female athletes studied at the Institute of Sports Science in Rome8 and elite mixed-sport, white female athletes studied in the UK.4 After LV chamber size was indexed to body size (BSA), however, we observed differences in the WNBA group compared with these other female athlete groups. Only 0.7% of WNBA players had an enlarged LV cavity size when indexed to BSA compared with 18% of the female athletes studied in the UK.4 Although we found less LV dilation in WNBA athletes compared with other female athlete groups, we observed greater increases in LVWT and indexes of concentric geometry. A total of 55% of WNBA athletes had an LVWT of 1.0 cm or greater compared with 9% of previously studied elite Italian female athletes.8 In addition, relative wall thickness was higher in WNBA players than previously reported in mixed-sport female athletes in the UK (0.39 in WNBA athletes compared with 0.35 in UK athletes).4 Eccentric LVH was more prevalent in the UK athletes than in WNBA athletes (21% vs 11.4%), whereas concentric geometry (concentric remodeling and concentric hypertrophy) was significantly more prevalent in WNBA athletes (24.2% vs 7.7%). Of note, most athletes with normal LV mass had normal LV geometry, consistent with a prior study.4
Within the WNBA cohort, we did not observe differences with respect to race/ethnicity in LVWT, LV mass index, or relative wall thickness. This finding differs from a prior study9 examining racial/ethnic differences in cardiac athletic remodeling in mixed-sport female athletes, which found that these indexes were increased in African American compared with white athletes. There are many reasons why our results may differ from those of Rawlins et al,9 including a lack of power to examine racial/ethnic differences in the current study because of the small number of white athletes and selection bias at this highest level of professional athletic competition. However, our overall findings highlight the importance of recognizing sport-specific differences in cardiac adaptation to training and suggest that concentric remodeling is a more prominent feature of athletic cardiac remodeling in female basketball players irrespective of race/ethnicity than has been reported in other studies that have included women engaged in a cross-section of sports.
The findings regarding athletic remodeling in WNBA players have important similarities and differences to those found in elite male basketball players in the National Basketball Association (NBA).5 We observed that LV size and mass in WNBA players were proportional to BSA, extending to the uppermost biometrics of the group, as was similarly demonstrated in male basketball players.5 However, the development of LV hypertrophy was less prevalent in WNBA players than in NBA players; 16.4% of WNBA players met sex-specific ASE criteria for LVH compared with 27.4% of male NBA players. Furthermore, only 1 WNBA athlete (0.7%) had an LVWT greater than 1.3 cm compared with 12% of NBA players. Our results are consistent with previously published data that, unlike in the male athletic counterparts, increased wall thickness beyond 12 mm was uncommon in female athletes and warrants investigation for a potential underlying cardiac disorder.4,8,12
In addition to our findings regarding athletic remodeling of the LV, the results of our study further support the finding that the RV chamber is enlarged in athletes and frequently exceeds the normal reference values proposed by the ASE.14,15 We observed that 42.2% of WNBA athletes had RV enlargement based on ASE criteria.10 Similar findings were observed in a previous study16 of 1016 white Olympic athletes, of whom 36% were women and 23% of all athletes exceeded the criteria for normal RV size based on RV outflow tract diameter. When RV basal diameter measurements were compared, mixed isometric and isotonic sports (which includes basketball) were associated with more RV enlargement than skill or power sports but with less RV enlargement than endurance sports. In that study, RV remodeling differed by sex. Although absolute RV outflow tract and RV basal diameters were larger in male than female athletes, BSA-indexed dimensions were larger in female athletes. Furthermore, a correlation between basal RV diameter and LVEDD was observed, highlighting that the RV may adapt similarly to the LV in association with athletic training. Current ASE guidelines do not provide sex-specific reference ranges for RV dimensions, and the ASE does not recommend indexing to BSA. In the current study, RV basal dimension correlated with BSA, supporting the importance of considering athlete’s size when assessing RV size. That weaker correlation of RV basal dimension than that of LVEDD and BSA may reflect the variability in measurement introduced by the lack of clear landmarks to ensure that the ASE-recommended optimal view (RV-focused view) is obtained when assessing RV basal dimension. Nonetheless, these data suggest that sex and size should be considered when assessing the RV and that perhaps a larger reference range should be accepted when assessing the RV in female athletes.
Aortic root diameter is another important cardiac dimension that is assessed in the evaluation of athletes, especially in tall athletes for whom there is potential for overlap with individuals who may have Marfan syndrome. The importance of correlating aortic root diameter with body size has been well documented and is reflected in the ASE recommendations to use nomograms that incorporate age, sex, and BSA in consideration of aortic root size.10 In male NBA basketball players, aortic root diameters reach a plateau at the highest extremes of athlete height and BSA.5 The findings in our cohort of female basketball athletes differed from what has been observed in male basketball athletes. In the WNBA group, a linear correlation was found between the aortic root and BSA. Given that the range of height and BSA in female athletes did not reach the same, higher dimensions as were seen in male athletes, we cannot currently estimate whether a similar plateau would have occurred. However, despite the larger size of female NBA athletes (mean BSA, 2.02 m2) compared with reference female adults, aortic root diameters rarely exceeded upper limit parameters as defined by the ASE (2 women [1.4%]), in contrast with our findings for left and right atrial and ventricular dimensions for which 18% to 42% of the athlete cohort demonstrated ASE-defined enlargement. This lack of aortic remodeling beyond the ASE-recommended criteria despite the larger body size is consistent with previously made observations by Engel et al5 and Pelliccia et al17 that dilation of aortic root greater than 40 mm in male athletes and greater than 34 mm in female athletes participating in a variety of sports disciplines was uncommon and requires investigation for a possible pathologic condition.5,17
Limitations
Some limitations to our results should be recognized. The demonstration of the associations between cardiac structure and geometry as well as aortic dimensions with body size in this female athlete group leads to the question of how to determine the relative contributions of physical training and body size to cardiac remodeling. We were not able to compare our findings with a group of sedentary controls of similar height and BSA as the athletes in our study. Some insight, however, can be gleaned from the study8 of Italian female athletes in which a group of 65 sedentary controls, matched by height and BSA, were compared with 600 athletes. A small but statistically significant difference was found, with athletes having larger LVEDD, LV mass, and LV wall thickness than the sedentary controls. Thus, this study further suggests that although athlete size may be a significant determinant of LV size and mass, athletic training represents an additional factor for which the association will vary depending on the type of training and physiologic demands required in the sport.
The optimal size index for cardiac chambers is debated in the literature, with studies examining height in centimeters, square centimeters, and centimeters to 2.7 power. We observed that in this elite female athlete population, all the cardiac chamber measurements had the strongest correlation with BSA, supporting the ASE recommendation of adjusting to BSA as an index of size in lean individuals.
Conclusions
In this study, increased cardiac dimensions were frequently observed in WNBA athletes. Both BSA and physiologic remodeling affected cardiac morphologic findings. The data presented here for female professional basketball players may provide a framework to help define the upper limits of athletic cardiac remodeling in this important athlete group. The findings provide new reference data in this athletic population and will perhaps act as a stimulus to investigate sex-specific cardiac changes in other athletic disciplines.
eTable. Echocardiographic Findings in WNBA Athletes Stratified by Race/Ethnicity
eFigure 1. Interobserver Variability for Left ventricular End-Diastolic Diameter
eFigure 2. Interobserver Variability for Aortic Root Diameter
eFigure 3. Interobserver Variability for Right Ventricular Basal Diameter
References
- 1.Maron BJ. Structural features of the athlete heart as defined by echocardiography. J Am Coll Cardiol. 1986;7(1):190-203. doi: 10.1016/S0735-1097(86)80282-0 [DOI] [PubMed] [Google Scholar]
- 2.Pelliccia A, Maron BJ, Spataro A, Proschan MA, Spirito P. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N Engl J Med. 1991;324(5):295-301. doi: 10.1056/NEJM199101313240504 [DOI] [PubMed] [Google Scholar]
- 3.Spirito P, Pelliccia A, Proschan MA, et al. Morphology of the “athlete’s heart” assessed by echocardiography in 947 elite athletes representing 27 sports. Am J Cardiol. 1994;74(8):802-806. doi: 10.1016/0002-9149(94)90439-1 [DOI] [PubMed] [Google Scholar]
- 4.Finocchiaro G, Dhutia H, D’Silva A, et al. Effect of sex and sporting discipline on LV adaptation to exercise. JACC Cardiovasc Imaging. 2017;10(9):965-972. doi: 10.1016/j.jcmg.2016.08.011 [DOI] [PubMed] [Google Scholar]
- 5.Engel DJ, Schwartz A, Homma S. Athletic cardiac remodeling in us professional basketball players. JAMA Cardiol. 2016;1(1):80-87. doi: 10.1001/jamacardio.2015.0252 [DOI] [PubMed] [Google Scholar]
- 6.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085-1092. doi: 10.1161/CIRCULATIONAHA.108.804617 [DOI] [PubMed] [Google Scholar]
- 7.Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in U.S. college athletes. J Am Coll Cardiol. 2014;63(16):1636-1643. doi: 10.1016/j.jacc.2014.01.041 [DOI] [PubMed] [Google Scholar]
- 8.Pelliccia A, Maron BJ, Culasso F, Spataro A, Caselli G. Athlete’s heart in women: echocardiographic characterization of highly trained elite female athletes. JAMA. 1996;276(3):211-215. doi: 10.1001/jama.1996.03540030045030 [DOI] [PubMed] [Google Scholar]
- 9.Rawlins J, Carre F, Kervio G, et al. Ethnic differences in physiological cardiac adaptation to intense physical exercise in highly trained female athletes. Circulation. 2010;121(9):1078-1085. doi: 10.1161/CIRCULATIONAHA.109.917211 [DOI] [PubMed] [Google Scholar]
- 10.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14. doi: 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 11.Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(4):277-314. doi: 10.1016/j.echo.2016.01.011 [DOI] [PubMed] [Google Scholar]
- 12.Basavarajaiah S, Boraita A, Whyte G, et al. Ethnic differences in left ventricular remodeling in highly-trained athletes relevance to differentiating physiologic left ventricular hypertrophy from hypertrophic cardiomyopathy. J Am Coll Cardiol. 2008;51(23):2256-2262. doi: 10.1016/j.jacc.2007.12.061 [DOI] [PubMed] [Google Scholar]
- 13.Di Paolo FM, Schmied C, Zerguini YA, et al. The athlete’s heart in adolescent Africans: an electrocardiographic and echocardiographic study. J Am Coll Cardiol. 2012;59(11):1029-1036. doi: 10.1016/j.jacc.2011.12.008 [DOI] [PubMed] [Google Scholar]
- 14.Zaidi A, Ghani S, Sharma R, et al. Physiological right ventricular adaptation in elite athletes of African and Afro-Caribbean origin. Circulation. 2013;127(17):1783-1792. doi: 10.1161/CIRCULATIONAHA.112.000270 [DOI] [PubMed] [Google Scholar]
- 15.Oxborough D, Sharma S, Shave R, et al. The right ventricle of the endurance athlete: the relationship between morphology and deformation. J Am Soc Echocardiogr. 2012;25(3):263-271. doi: 10.1016/j.echo.2011.11.017 [DOI] [PubMed] [Google Scholar]
- 16.D’Ascenzi F, Pisicchio C, Caselli S, Di Paolo FM, Spataro A, Pelliccia A. RV remodeling in Olympic athletes. JACC Cardiovasc Imaging. 2017;10(4):385-393. doi: 10.1016/j.jcmg.2016.03.017 [DOI] [PubMed] [Google Scholar]
- 17.Pelliccia A, Di Paolo FM, De Blasiis E, et al. Prevalence and clinical significance of aortic root dilation in highly trained competitive athletes. Circulation. 2010;122(7):698-706. doi: 10.1161/CIRCULATIONAHA.109.901074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Echocardiographic Findings in WNBA Athletes Stratified by Race/Ethnicity
eFigure 1. Interobserver Variability for Left ventricular End-Diastolic Diameter
eFigure 2. Interobserver Variability for Aortic Root Diameter
eFigure 3. Interobserver Variability for Right Ventricular Basal Diameter