Abstract
This study uses Medicare’s Nursing Home Compare and a university long-term care database to compare census, admissions, discharges, and mortality at skilled nursing facilities (SNFs) in 3 metropolitan areas during March-May 2020 vs March-May 2019.
Mortality from coronavirus disease 2019 (COVID-19) is disproportionately concentrated in skilled nursing facilities (SNFs). As of June 18, 2020, 50 185 residents died of COVID-19 in the 41 states reporting deaths at SNFs, accounting for 45% of their total COVID-19 deaths statewide.1 In addition to long-term care, SNFs provide short-term care after elective surgeries and hospitalizations. With the decreases in hospital volume for elective surgeries and other services during the pandemic, SNF admissions may also be declining.2
Little peer-reviewed evidence on COVID-19 in SNFs exists beyond single centers.3 Therefore, we examined outcomes at SNFs in 3 metropolitan areas from March to May 2020.
Methods
We assessed outcomes from January 1, 2019, to May 26, 2020, aggregated by CarePort Health, a health technology company that provides data for care coordination to hospitals and postacute care providers via SNF electronic health records. Outcomes included weekly rates for all-cause mortality, admissions, and patient census at SNFs in Cleveland, Ohio; Detroit, Michigan; and New York City, New York; along with weekly total COVID-19 death counts for these areas.4
We compared the characteristics of the SNF sample with all other SNFs in the 3 cities using data on quality, staffing, and patient characteristics from Medicare’s Nursing Home Compare database and Brown University’s LTCFocus.org database.5
To quantify changes in weekly mortality and admissions, we estimated adjusted incidence rate ratios (IRRs) and 95% CIs comparing March-May 2020 with the same weeks in 2019 using Poisson regression at the week level and adjusted for SNF-level fixed effects. Analyses were performed using SAS version 9.4 (SAS Institute Inc). The Harvard Medical School institutional review board exempted this study from review.
Results
The study sample consisted of 189 SNFs, which accounts for 34% of the 559 SNFs in the 3 cities. The sample SNFs differed from other regional SNFs. In Cleveland, the sample SNFs had higher Medicare star ratings than all SNFs in the area (mean, 3.8 vs 3.3, respectively; Table). There were 3853 all-cause in-facility deaths in the sample SNFs from March-May 2020 vs 1765 during March-May 2019, with excess mortality that followed a similar pattern to overall COVID-19 deaths regionally (Figure).
Table. Characteristics of Sample Skilled Nursing Facilities (SNFs) vs All SNFs in 3 Metropolitan Areas.
| Characteristics | SNFs by metropolitan area | |||||
|---|---|---|---|---|---|---|
| Cleveland | Detroit | New York City | ||||
| Sample | All | Sample | All | Sample | All | |
| Facilities | ||||||
| Total No. | 65 | 182 | 59 | 134 | 65 | 243 |
| Medicare star rating for 2020, %a | ||||||
| Mean | 3.8 | 3.3 | 2.6 | 2.9 | 3.8 | 3.7 |
| 1 | 6.2 | 14.8 | 27.1 | 22.4 | 4.6 | 5.8 |
| 2-3 | 26.2 | 35.2 | 45.8 | 38.8 | 33.8 | 37.0 |
| 4-5 | 67.7 | 49.5 | 27.1 | 38.8 | 61.5 | 56.8 |
| For-profit institution, %a | 73.8 | 80.8 | 88.1 | 82.8 | 73.8 | 72.8 |
| No. of beds, meana | 116 | 108 | 146 | 126 | 308 | 239 |
| Occupancy, %a | 85.2 | 82.5 | 86.5 | 84.8 | 93.6 | 92.6 |
| Staffing during third quarter of 2019, h/resident/da,b | ||||||
| Registered nurses | 0.7 | 0.6 | 0.5 | 0.5 | 0.7 | 0.7 |
| Nursing aides | 2.2 | 2.0 | 2.0 | 2.1 | 2.3 | 2.2 |
| Total staff | 3.8 | 3.6 | 3.7 | 3.8 | 3.6 | 3.6 |
| Quality measures in 2020a | ||||||
| Rate of potentially preventable readmission 30 d after discharge, %c | 7.5 | 7.4 | 7.5 | 7.5 | 7.1 | 7.2 |
| Rate of successful discharge without complication to home or community, %c | 59.9 | 55.8 | 50.0 | 51.2 | 48.2 | 44.6 |
| Medicare spending/beneficiary vs national Medicare beneficiary spending, mean | 1.0 | 1.0 | 1.1 | 1.1 | 1.3 | 1.3 |
| Part of a chain vs an independent facility, % | 52.3 | 58.2 | 61.0 | 53.0 | 6.2 | 3.7 |
| Residents in 2017d | ||||||
| Mean age, y | 80.6 | 77.7 | 77.1 | 77.4 | 78.9 | 76.9 |
| Female, % | 60.7 | 57.0 | 55.9 | 55.2 | 55.1 | 53.8 |
| Race/ethnicity, %e | ||||||
| Black | 27.4 | 33.9 | 42.8 | 42.5 | 27.1 | 29.8 |
| Hispanic | 1.5 | 1.1 | 0.1 | 0 | 16.6 | 16.2 |
| White | 79.6 | 71.6 | 57.3 | 58.2 | 49.7 | 47.2 |
| Insurance coverage, % | ||||||
| Medicare | 14.6 | 10.6 | 15.2 | 17.0 | 16.6 | 14.8 |
| Medicaid | 53.0 | 59.9 | 63.8 | 60.5 | 60.3 | 62.8 |
Data extracted from the publicly available Nursing Home Compare database.
Based on payroll-based staffing data from the Centers for Medicare & Medicaid Services.
Among Medicare fee-for-service short-stay patients.
Extracted from publicly available data at LTCFocus.org.5
Extracted from the federally mandated Minimum Data Set for all residents on admission using the categories defined by the Medicare-based collection instrument. Self-reported by patients or family members. These data are reported in this study to understand the differences in population characteristics between the sample SNFs and all SNFs regionally.
Figure. Weekly Mortality, Admissions, and Patient Census From Skilled Nursing Facilities (SNFs) and Overall COVID-19 Deaths in 3 Metropolitan Areas.
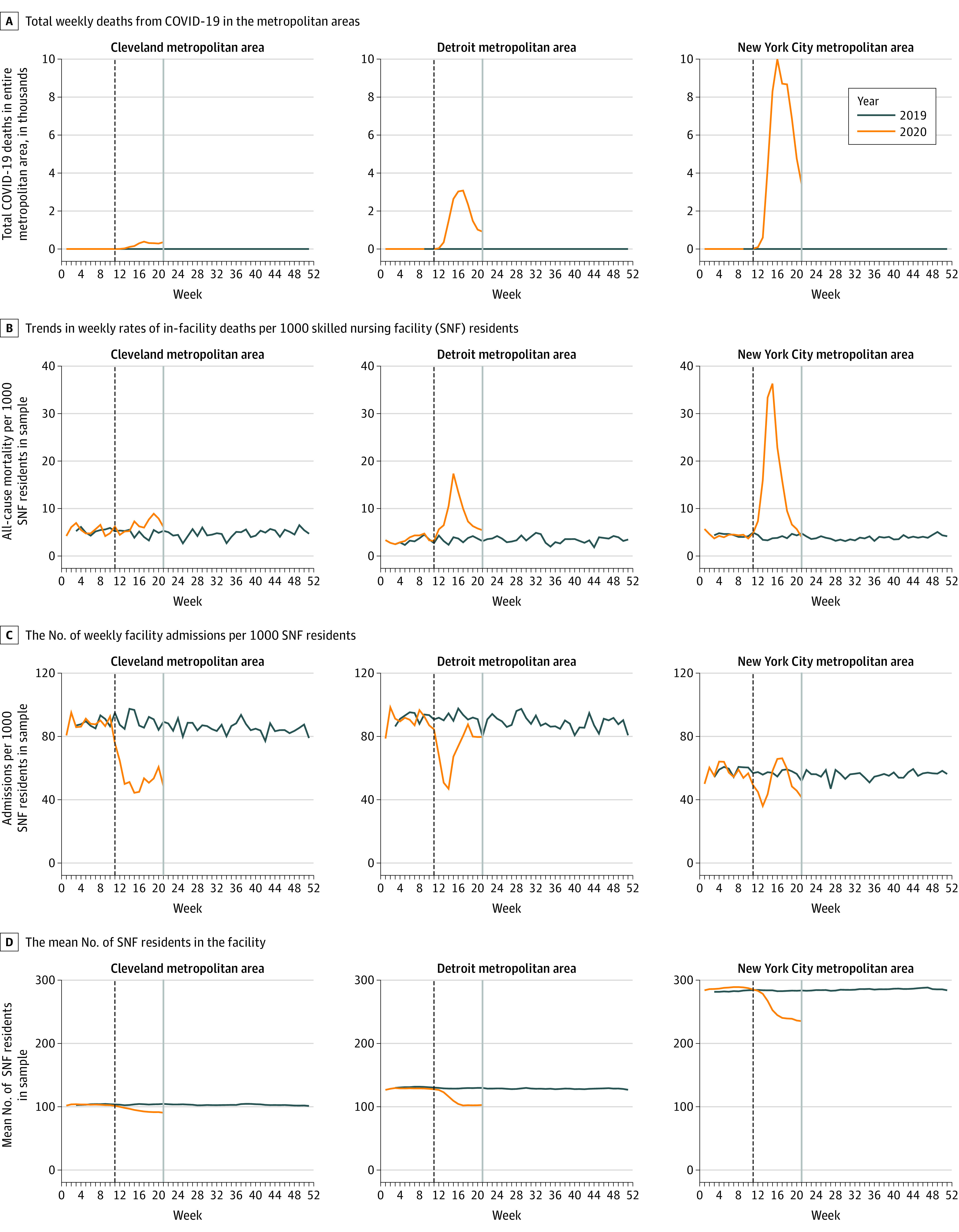
The panels show the weekly rates for 2019 (blue) and 2020 (orange) that were superimposed to show contrast. The dashed vertical lines mark when Medicare directed all SNFs to disallow visitors and discontinue communal activities (week of March 13, 2020) due to coronavirus disease 2019 (COVID-19). The gray vertical lines mark the last week of data (May 20, 2020).1
In Cleveland, there was higher mortality at SNFs in 2020 vs 2019 (mean, 6.3 and 4.9, respectively, per 1000 residents per week during March-May), but the difference was not statistically significant (adjusted IRR, 1.02; 95% CI, 0.94-1.11). Similarly, in Detroit, there was higher mortality at SNFs in 2020 vs in 2019 (mean, 7.9 and 3.5, respectively, per 1000 residents per week during March-May; adjusted IRR, 2.18; 95% CI, 2.01-2.37) and in New York City (mean, 13.8 vs 4.1, respectively, per 1000 residents per week during March-May; adjusted IRR, 4.13; 95% CI, 3.95-4.33). During the peak week in April 2020, mortality at SNFs in Detroit was 17.4 per 1000 residents per week vs 4.0 during the same week in April 2019 (adjusted IRR, 6.74; 95% CI, 5.57-8.15); and in New York City, mortality was 36.3 vs 3.7, respectively, per 1000 residents per week (adjusted IRR, 8.79; 95% CI, 7.75-9.98).
Weekly admissions declined in sample SNFs during March-May 2020 compared with 2019 in Cleveland (adjusted IRR, 0.59; 95% CI, 0.51-0.68), Detroit (adjusted IRR, 0.63; 95% CI, 0.62-0.74), and New York City (adjusted IRR, 0.75; 95% CI, 0.74-0.76) (Figure). The patient census was also lower in sample SNFs in March-May 2020 vs 2019 in Cleveland (mean, 90.6 vs 104.5), Detroit (mean, 102.7 vs 129.7), and New York City (mean, 235.2 vs 283.6).
Discussion
From March to May 2020, there was a spike in overall mortality among residents at SNFs in Detroit and New York City, which were 2 cities with substantial COVID-19 burden, and a lower increase in mortality in Cleveland, which was a city with fewer COVID-19 cases. Regardless of mortality, admissions and patient census decreased in all 3 cities.
This analysis may not necessarily generalize to other regions in the US, and the study sample differed from other regional SNFs. Also, these results do not include the causes of death and do not capture deaths occurring outside SNFs.
These results suggest that SNFs experienced substantial clinical challenges during the COVID-19 pandemic. Mortality increased quickly, raising concerns about the capacity of SNFs to respond to outbreaks. Compounding the challenge, decreased patient census may lead to reductions in revenue at a time when SNFs have the greatest need for additional resources to manage and prevent future outbreaks.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Henry J. Kaiser Family Foundation State data and policy actions to address coronavirus. Published June 18, 2020. Accessed June 18, 2020. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/
- 2.Baum A, Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. Published online June 5, 2020. doi: 10.1001/jama.2020.9972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMichael TM, Currie DW, Clark S, et al. ; Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team . Epidemiology of COVID-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. doi: 10.1056/NEJMoa2005412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.New York Times COVID-19 data. Accessed June 2, 2020. https://github.com/nytimes/covid-19-data
- 5.Brown University School of Public Health LTCfocus—long-term care: facts on care in the US. Accessed June 2, 2020. http://ltcfocus.org/2/faq


