Abstract
Individuals increasingly access peer-generated health information (PGHI) through social media, especially online health communities (OHCs). Previous research has documented PGHI topics, credibility assessment strategies, and PGHI’s connection with well-being. However, there is limited evidence on where, when, and why individuals seek PGHI and how they use PGHI in health decisions. We conducted in-person and online focus groups with verified OHC members (n=89)—representing 50 different medical conditions and 77 OHCs—to explore these topics. Two researchers independently coded transcripts with NVivo 9.2 and thematically analyzed responses. Most individuals accidentally discovered PGHI during web searches rather than intentionally seeking it. Individuals valued PGHI primarily as an alternative information source about treatment options, self-care activities, and healthcare provider questions rather than a source of emotional support, and they acknowledged PGHI’s limitation as anecdotal evidence. Individuals used PGHI as a springboard for additional research and patient-provider discussions, ultimately making treatment decisions alongside providers. These findings suggest that individuals use PGHI in much the same way they use traditional online health information and that PGHI facilitates, rather than obstructs, shared decision-making with healthcare providers.
Keywords: Peer-generated health information, social media, online communities, chat rooms, message boards, shared decision-making
Consumers cite the Internet as a popular and useful source of health information, with approximately 60% of U.S. adults regularly seeking health information online (Fox & Duggan, 2013; Manhattan Research, 2005). When individuals have health questions, search engines and medical websites are the first sources consulted (Fox, 2011a; Hesse, Moser, & Rutten, 2010; Levy et al., 2006), and individuals’ seek online health information primarily to research symptoms, understand health conditions, and explore treatment options (Fox, 2011a; Fox & Duggan, 2013; Fox & Jones, 2009; McMullan, 2006; Wald, Dube, & Anthony, 2007).
Research has demonstrated that individuals use online health information to inform treatment decisions, self-care activities, and discussions with healthcare providers (Baker et al., 2003; Fox, 2011b; McMullan, 2006; National Cancer Institute, 2014; Wagner et al., 2004; Wald, Dube, & Anthony, 2007). Many studies suggest that online information has a positive effect, leading to greater knowledge, more active participation in health decisions, and more robust patient-provider discussions without supplanting providers as trusted information sources (Hesse, Moser, & Rutten, 2010; Lee, 2008; Lee, Wang, & Lewis, 2010; Murray et al, 2003; Von Knoop et al., 2003). However, other studies have identified drawbacks to online health information, including the challenge of identifying trustworthy sources, the high volume of information, and the tendency of some individuals to self-diagnose without consulting a physician (Berland et al., 2001; Cline & Haynes, 2001; Fox & Duggan, 2013; Macias & McMillan, 2008).
Despite heavy reliance on traditional (i.e., expert-generated) online health information, individuals increasingly access peer-generated health information (PGHI) through social media sites (Fox, 2011b; Fox & Duggan, 2013). Peer-generated health information typically comprises lay individuals’ personal experiences with diagnosis and treatment, allowing individuals to evaluate the pros and cons of treatment options and to hear others’ perspectives on medical procedures (Author et al., 2014; Bender, Jimenez-Marroquin, & Jadad, 2011; Macias, Lewis, & Smith, 2005). Although individuals can encounter PGHI on standard social media platforms (e.g., Facebook, Twitter), they are most likely to access PGHI in online health communities (OHCs), which are Internet-based discussion forums focused on specific health topics (Bender, Jimenez-Marroquin, & Jadad, 2011; Dutta & Feng, 2007; Eysenbach et al., 2004).
At the same time that individuals are increasingly accessing PGHI, healthcare organizations are increasingly encouraging shared decision-making (SDM) among patients and healthcare providers. SDM has been consistently identified as a gold standard in medical decision-making, and multiple studies have demonstrated that SDM leads to greater patient satisfaction, improved medication adherence, and improved health outcomes (Elwyn et al., 2012; Oshima & Emanuel, 2013). SDM is defined as a collaborative process in which patients and healthcare providers make joint decisions based on both available scientific evidence and patient values/preferences (Briss et al., 2004; Charles, Gafni, & Whelan, 1997; Deber, Kraetschmer, & Irvine, 1996; Informed Medical Decisions Foundation [IMDF], 2012; Rimer et al., 2004). Specifically, SDM includes: (1) Patients and providers discuss available treatment options; (2) Patients understand the pros and cons of treatment options; (3) Patients articulate their values and preferences to providers (e.g., willingness to accept risks); (4) Patients participate in decision-making at their desired level; and (5) Patients and providers make joint treatment decisions that align with patient values/preferences.
Decades of research have examined how offline social networks influence health decisions, demonstrating that networks are strong predictors of health choices, such as the decision to seek screening or treatment (Brunson, 2013; Jackson, Cheater, & Reid, 2008; Kim et al., 2015; Kjos, Worley, & Schommer, 2011; Smith & Christakis, 2008). However, there is considerably less evidence on how individuals use online PGHI, and previous research has focused primarily on three areas. First, content analyses have demonstrated that most PGHI addresses treatment options and prescription drugs, with individuals often recommending specific treatments and medications to others (Macias, Lewis, & Smith, 2005). Second, several studies have found that individuals perceive PGHI as credible when it is specific (Savolainen, 2011), mentioned by multiple users (Metzger, Flanagin, & Medders, 2010), consistent with their own opinions and experiences (Metzger, Flanagin, & Medders, 2010), and delivered by peers whom individuals perceive as similar to themselves (Walther, Slovacek, & Tidwell, 2001; Wang et al., 2008).
Third, studies have presented mixed evidence on how PGHI affects health and well-being. Some studies have found that PGHI and OHC participation can improve social support, increase medical knowledge, promote treatment adherence, and improve clinical discussions. Other studies have found that PGHI does not affect these outcomes and that OHC members are motivated individuals who already seek a great deal of health information (An et al., 2008; Bender, Jimenez-Marroquin, & Jadad, 2011; Dutta & Feng, 2007; Eysenbach et al., 2004; Frost & Massagli, 2008; Jodlowski et al., 2007; Rainie, 2010; Richardson et al., 2010; Setoyama, Nakayama, & Yamazaki, 2011 and 2009; Wicks et al., 2010; Wicks et al., 2012).
Despite this previous research, there are significant gaps in understanding how individuals encounter and use PGHI. First, few studies have examined why and when individuals seek PGHI, with most research assuming that OHCs are social support outlets (Chung, 2014; Wang et al., 2008). Second, there is no documentation of what treatment aspects (e.g., efficacy, side effects) are mentioned in PGHI discussions, what information sources are cited, and the extent to which discussions contain balanced information. Finally, and most importantly, no study has identified how online PGHI influences health and treatment decisions. Given concerns that social media could breed misinformation and disrupt patient-provider relationships (Bosslet et al., 2011; Modahl, Tompsett, & Moorhead, 2011), it is important to address these gaps and understand how individuals use PGHI.
The purpose of this study was to identify how patients and caregivers encounter, interpret, and use online PGHI within OHCs across a broad range of health conditions and how this compares to individuals’ use of traditional online health information. Specifically, we sought to answer the following five research questions:
Platforms and Identification. What types of OHCs do individuals visit when seeking PGHI? How do they find these communities?
Timing and Rationale. When and why do individuals seek PGHI?
Treatment Discussions. What aspects of treatment are discussed within PGHI? How balanced are these discussions?
Information Sources. What sources of information are cited in PGHI?
Role in Health Decisions. How do individuals use PGHI in their health and treatment decisions?
METHODS
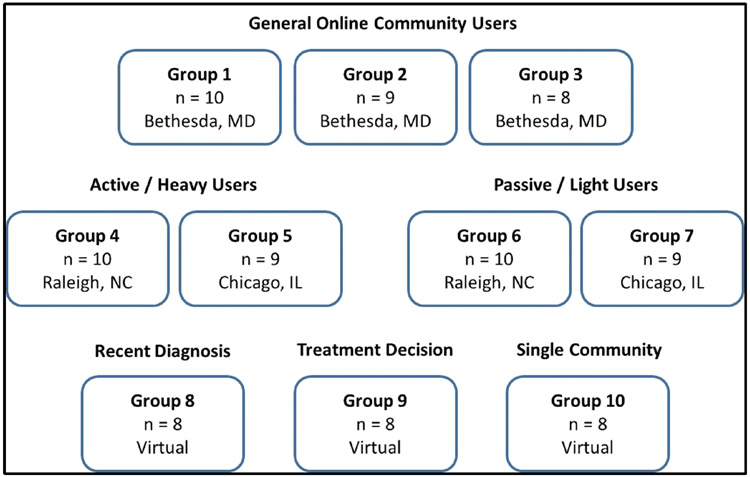
We conducted ten in-person and virtual focus groups with members of verified OHCs to answer the study’s research questions (Figure 1). Focus groups are ideal for exploring individuals’ attitudes and behaviors, and they elicit detailed responses that are difficult to capture on large surveys, especially if response categories are unknown (Morgan, 1998).
Figure 1: Focus Group Populations, Locations, and Sample Sizes1.
1 See Table 1 for group-specific eligibility criteria.
We conducted the first seven groups in person, and we conducted the remaining three groups on a live chat platform to achieve greater geographic diversity, sample sufficient participants with the same illness, and reach individuals who may not be healthy enough to participate in person. Although virtual focus groups are still emerging as a methodology, some studies have documented the advantages of virtual groups and the compatibility of data from in-person and virtual sessions (Banfield et al., 2012; Fox, Morris, & Rumsey, 2007; Poehlman et al., 2015; Popenko et al., 2012; Tates et al., 2009).
Study participants included general OHC users (Groups 1-3); active/heavy users who visited OHCs at least once per week and frequently posted information (Groups 4-5); passive/light users who visited OHCs less than once per week and rarely posted information (Groups 6-7); users recently diagnosed with fibromyalgia (Group 8); users recently engaged in a treatment decision for clinical depression (Group 9); and users who participated in the same multiple sclerosis OHC (Group 10). The criteria for these sub-populations are presented in Table 1.
Table 1.
Participant Eligibility Criteria by Group
| Groups | Population | Eligibility Criteria |
|---|---|---|
| All | All Participants | Aged 18 or older English speaking Visit at least one active online health community focused on an illness or medical condition1 Not employed in healthcare or pharmaceutical industries Community participation is not part of job |
| 1-3 | General Users | Visit community at least once per month |
| 4-5 | Active / Heavy Users | More likely to post information on site than read it Visit community at least once per week |
| 6-7 | Passive / Light Users | More likely to read information on site than post it Visit community at least once per month but less than once per week |
| 8 | Recent Diagnosis (Fibromyalgia) | Diagnosed with fibromyalgia within last 12 months (or family member diagnosed in last 12 months) Visit a community focused on fibromyalgia at least once per month |
| 9 | Recent Treatment Decision (Depression) | Diagnosed with clinical depression (or family member diagnosed) Made a major treatment decision related to depression within last 12 months Visit a community focused on depression at least once per month |
| 10 | Single Community (Multiple Sclerosis) | Diagnosed with multiple sclerosis (or family member diagnosed) Visit the PatientsLikeMe MS community at least once per week |
We verified that OHCs were active and eligible by visiting OHC URLs provided by potential participants. We confirmed that site content was mostly or exclusively member-generated, posted within the last week, and focused on a specific medical condition.
We employed this study design and sub-population strategy to sample different types of OHC users, examine active versus passive users, explore specific topics in depth (e.g., diagnosis, treatment decisions), achieve geographic diversity, and include individuals who may not be able to participate in person. We selected the health conditions in Groups 8-10 to boost illness diversity in the overall sample and ensure topics were relevant to participants (e.g., fibromyalgia patients/caregivers likely struggled with diagnosis given healthcare provider skepticism of the condition). We held the groups during September–December 2011 in Washington, DC; Raleigh, NC; Chicago, IL; and online. Ethics boards at RTI International and the U.S. Food and Drug Administration approved the study.
Recruitment and Screening
We collaborated with three recruitment firms and one OHC to recruit a purposive sample for the study. For Groups 1-9, recruitment firms identified potential participants using databases and advertisements, contacted individuals by telephone, and screened them for eligibility using an 11-item questionnaire. If interested and eligible, individuals were scheduled for focus groups on preselected days.
For Group 10, the community host (PatientsLikeMe.com) posted an advertisement for the study within its multiple sclerosis OHC. (PatientsLikeMe.com was founded in 2004 and is one of the first and longest-running OHCs. It hosts more than 400,000 members representing 2,500 medical conditions and emphasizes sharing health data alongside personal experiences.) Interested individuals contacted the OHC administrator, who conducted a preliminary screening and referred individuals to the study team. A team member then contacted individuals by telephone, screened them for eligibility using the same questionnaire used in Groups 1-9, and scheduled eligible individuals for the focus group on a preselected day.
Eligibility Criteria
Eligible individuals were ages 18 or older, spoke English, and had read or posted content in at least one active OHC for themselves (patients) or a child/parent (caregivers) within the last month. We included caregivers because half of online health research is conducted for someone else (Fox & Duggan, 2013). We excluded individuals who participated in OHCs as part of employment or who worked in the healthcare or pharmaceutical industries. In addition, we established group-specific eligibility criteria to segment participants into sub-populations (Table 1).
We defined OHCs as “websites where individuals gather to learn more about and share health information with one another,” and we shared this definition with potential participants during screening. For all ten groups, we asked potential participants for OHC URLs, and we visited sites to confirm that: (1) site content was mostly or exclusively member generated; (2) content was posted within the last week; and (3) site focused on a medical condition rather than general health/wellness. Individuals who belonged to ineligible or inactive OHCs were excluded.
Data Collection
We developed a semi-structured moderator guide to address the study’s five research questions, including how individuals discovered and engaged with PGHI and what role PGHI played in health decisions. We then tailored the guide into six versions for each of the sub-populations, although most questions were asked in all ten groups.
For Groups 1-7, we conducted two-hour in-person focus groups at market research facilities. Upon arrival, participants were administered written informed consent, and a trained moderator conducted each group using the tailored guide by asking questions, probing for details, and leading an open discussion. We audio recorded all groups and produced verbatim transcripts, and one or two note takers documented themes during the sessions. Participants received a $75 incentive after each group.
For Groups 8-10, we conducted one-hour virtual focus groups on a real-time, live chat platform. We e-mailed consent forms and login credentials to participants in advance. Upon login, participants acknowledged an electronic consent form. A trained moderator posted questions and probes, and participants typed responses visible to the entire group. Three note takers documented themes in each session, and transcripts captured verbatim responses. Participants were mailed a $50 incentive after each group.
Data Analysis
Once all groups were complete, we began reviewing the transcripts/notes and developing a three-tiered coding scheme based on both study research questions and participant responses. The first tier of the coding scheme organized participant responses into pre-determined topics that mapped to the research questions (e.g., first level code = Treatment discussions). The second and third tiers were inductive and contained emergent codes based on participant responses (e.g., second level code = Types of treatment; third level code = Prescription medications).
This coding strategy allowed us to organize participant responses by topic while still ensuring that the data—not research team assumptions—drove the coding. This mix of concept-driven and data-driven codes is a rigorous way to balance a study’s conceptual framework with its raw data (Charmaz, 2003; Gibbs, 2007; Ritchie & Lewis, 2003).
During this process, two team members independently reviewed and coded all transcripts in NVivo 9.2 qualitative analysis software to ensure coding reliability and minimize bias (Denzin, 1970; Gibbs, 2007). Team members examined participant responses, developed second- and third-level codes based on raw data, and coded responses accordingly. The lead author interpreted the few coding discrepancies. Once coding was complete, we conducted thematic analysis by identifying trends in second- and third-level codes across the groups and, when applicable, within sub-populations (Charmaz & Mitchell, 2001; Miles & Huberman, 1994).
RESULTS
Participant Characteristics
We enrolled 89 individuals in the study (Table 2). The majority was female (65%), White (70%), older than 45 years of age (52%), and had at least a college degree (70%). These demographics are consistent with research showing that females, Caucasians, and college graduates are more likely to seek health information online than other demographic groups (Fox & Duggan, 2013).
Table 2.
Participant Demographics
| Characteristic | In-Person Groups (n=65) |
Virtual Groups (n=24) |
Total (n=89) |
|---|---|---|---|
| Sex | |||
| Male | 24 (37%) | 7 (29%) | 31 (35%) |
| Female | 41 (63%) | 17(71%) | 58 (65%) |
| Age (years) | |||
| 18–24 | 6 (9%) | 0 (0%) | 6 (7%) |
| 25–34 | 12 (18%) | 4 (17%) | 16 (18%) |
| 35–44 | 12 (18%) | 8 (33%) | 20 (22%) |
| 45–54 | 19 (29%) | 8 (33%) | 27 (30%) |
| 55–64 | 13 (20%) | 3 (12%) | 16 (18%) |
| 65–74 | 3 (5%) | 1 (4%) | 4 (4%) |
| Ethnic Background | |||
| Caucasian | 43 (66%) | 19 (79%) | 62 (70%) |
| African American | 15 (23%) | 2 (8%) | 17 (19%) |
| American Indian or Alaska Native | 0 (0%) | 0 (0%) | 0 (0%) |
| Hispanic | 1 (2%) | 1 (4%) | 2 (2%) |
| Asian | 1 (2%) | 1 (4%) | 2 (2%) |
| Hawaiian or Pacific Islander | 2 (3%) | 0 (0%) | 2 (2%) |
| Other | 3 (7%) | 1 (4%) | 4 (4%) |
| Education1 | |||
| Less than High School | 1 (2%) | 0 (0%) | 1 (1%) |
| High School | 0 (0%) | 3 (13%) | 3 (3%) |
| Some College or Technical School | 12 (19%) | 10 (42%) | 22 (25%) |
| College Graduate | 33 (52%) | 6 (24%) | 39 (44%) |
| Some Graduate School | 5 (8%) | 1 (4%) | 6 (7%) |
| Graduate School Degree | 13 (20%) | 4 (17%) | 17 (19%) |
Data missing for one participant.
Based on screening data, participants belonged to 77 distinct OHCs representing 50 different medical conditions (Table 3). Because Groups 8-10 were restricted to specific illnesses, participants in Groups 1-7 belonged to a more diverse set of communities. On average, participants belonged to two OHCs (range 1-6) and visited those sites 11 times per month (range 1-40 times per month).
Table 3.
Data based on screening responses (not focus group discussions).
Boldface responses indicate communities visited by more than one participant in the segment.
Platforms and Identification
Participants described encountering PGHI on many different OHC platforms, which we organized into five categories: (1) OHCs that contained multiple illness forums and were hosted by large medical or commercial sponsors (e.g., WebMD.com, Yahoo.com, HealthBoards.com); (2) OHCs focused on a single illness and hosted by medical or non-profit organizations (e.g., American Cancer Society, Crohn’s and Colitis Foundation of America); (3) OHCs focused on a single illness and hosted by health insurers (e.g., BlueCross and BlueShield); (4) standalone OHCs focused on a single illness with no identifiable sponsor (e.g., DiabetesTalkFest.com); and (5) OHCs nested within non-health sites (e.g., depression forum on city website).
The vast majority of participants reported visiting OHCs in the first two categories, especially those with multiple illness forums. The type of platform visited did not seem to differ by demographics, type of illness, or sub-population. Participant engagement (i.e., frequency of visits, active vs. passive usage) also was similar across all five OHC categories. Based on participant descriptions, these platforms varied widely in their size (several hundred members vs. tens of thousands), level of activity (several posts per day vs. hundreds of posts per hour), time in existence (founded one year ago vs. founded in late 1990s), and membership requirements (login required vs. open forum).
Most participants reported finding OHCs through search engines, such as Google. However, instead of deliberately searching for peer communities, participants reported searching for illness or symptom information, and PGHI appeared in the search results. A few participants did report discovering OHCs through other methods, such as family/friend referrals, organization referrals, and product websites.
Group 1: “I usually start with Google, and I’ll do a search on something and then it’ll bring me to a community—like a new community—and then I’ll learn about it.”
Group 1: “My aunt told me about it. When she found out I was diagnosed, she’s like ‘Hey, you should get involved.’”
Timing and Rationale
Participants reported seeking PGHI at two distinct time periods. A small number of participants sought PGHI pre-diagnosis when they suspected an illness. These participants often found OHCs via symptom web searches, and they visited multiple communities to learn what their condition might be. They described seeking PGHI as being spurred by frustration with family and friends who could not understand their health issues and healthcare providers who could not offer diagnoses.
Group 8: “…before I was diagnosed, I pretty much knew by what others were saying in the forum I belonged to [that I had the illness]…The frustration of not knowing what this is drove me to find the community.”
However, most participants sought PGHI soon after a formal diagnosis. These participants searched for PGHI to learn more about their condition, get support, and learn from others’ experiences with the same illness.
Group 3: “I was surprised at the diagnosis…because I thought I was too young to have this problem, and I immediately went into this [community].”
Group 8: “I only really got involved after the diagnosis had been made.”
When asked why they ultimately engaged in OHCs, most participants reported that they wanted to learn more about their (or a loved one’s) health condition. Noticeably fewer participants reported visiting to seek emotional support or because of healthcare provider dissatisfaction (see Author et al., 2014, for more detail).
Group 7: “So it was nice and comforting at a time where I wasn’t exactly comfortable with what was going on. To read what worked for others and kind of try it out and get myself, you know, in shape for it.”
Group 9: “[I wanted] to know that there were other people out there with the same issue.”
Group 1: “Well, for my own knowledge base…To tell my mom a lot of different things since she’s not using the web quite as much as she used to.”
Treatment Discussions
Regardless of illness, participants reported that treatment was one of the most common PGHI discussion topics. Although participants explained that specific treatments varied by community, they reported regularly discussing four treatment categories: (1) prescription and over-the-counter medications, (2) behavioral therapies (e.g., exercise, diet), (3) alternative therapies (e.g., acupuncture), and (4) medical therapies (e.g., surgery). Participants agreed that medication discussions were most prevalent.
Participants explained that treatment discussions comprised multiple elements. Effectiveness and side effects were the most common aspects, with many discussions highlighting others’ positive or negative treatment experiences. Recovery—such as from surgery or chemotherapy—also was discussed frequently, and participants explained that peers often provided day-to-day recovery advice that healthcare providers could not offer. A few participants also reported discussing insurance coverage, medication costs, and—especially in standalone OHCs—illness-related news or drug approvals.
Group 3: “That’s really the bottom line, I think…what are the treatment options, what are the pros, what are the cons.”
Group 2: “I’m like, ‘Hey, does anyone know what’s the best kind of moisturizer after you…had chemo…and your skin starts to dry out?’ So I think you get…some really great feedback of people who have been there, done that.”
Group 6: “There’s a lot of things about complications, too, to the surgery.”
Most participants reported that PGHI treatment discussions were balanced, encompassing both advantages and disadvantages of specific treatments. Participants explained that, although individual posts were typically either positive or negative, the discussion of advantages and disadvantages balanced out within discussion threads.
Group 8: “Usually there is a balance, and you have to appreciate that every case is different.”
Group 6: “Somebody did it, and they didn’t like it; somebody did it, and they loved it. I think it’s just where you get an influx of information and try to delve through it and see what’s applicable for you.”
Nevertheless, participants cautioned that the illness often influenced this balance. For example, some illnesses have limited treatment options and poorer prognoses, and participants explained that PGHI related to these illnesses contained fewer “success stories.”
Information Sources
Almost all participants reported that personal experiences were the most common source of information in treatment discussions. References to factual sources were considerably less common. However, some participants—especially those in Group 10—reported more balance between personal and factual references. Factual references mentioned by participants included links to news articles, scientific papers (e.g., New England Journal of Medicine), and medical websites (e.g., WebMD), and participants who encountered factual references reported occasionally visiting links for more information.
Group 4: “Sometimes…they’ll say, ‘Yeah, I came across this article, follow this link’, but a lot of times it’s personal experience.”
Group 1: “I would say it’s an equal balance depending on what you’re looking for. Because some things pertain to more personal matters, and some things are more broad, so you are really going to go with the facts instead.”
Group 4: “The doctors really don’t know [everything]…They do the surgery but, afterwards at home, they’re not doing the things every day. So it’s to ask other families or the people that have been through this.”
Role in Health Decisions
Participants cited several ways that PGHI influenced their health decisions. First, participants reported using PGHI to identify and evaluate treatment options and self-care activities, both traditional and alternative. Many participants reported that healthcare providers do not have enough time to discuss treatment options in depth, compelling participants to discuss treatment options with individuals who have used them.
Group 4: “I think part of what…draws this whole need for information is that doctors have…less and less time to spend with you.”
Group 10: “I first learned about the current drug that I’m taking by reading about it at [PatientsLikeMe]. When my d[octo]r suggested it, I was already familiar with it and that made things a lot more comfortable.”
Likewise, many participants stated that healthcare providers often emphasized traditional treatments (i.e., medication), and PGHI allowed participants to learn about other options, such as rehabilitation exercises, dietary changes, and home remedies.
Group 6: “They had some exercise for people with osteoarthritis because when you sit in one position you get stiff…I watched the video of what to do, and I started doing that, and it was real helpful.”
Group 2: “Mine’s about how to make different kind of dinners that will help my dad manage his diabetes.”
Second, participants explained that PGHI helped them to prepare for clinical visits. They stated that peer discussions helped them understand medical jargon and learn about treatment options in advance. Thus, when attending clinical appointments, participants reported feeling more prepared and ready to engage with healthcare providers.
Group 4: “I felt like I was educated enough to where I went and had that initial consultation at the doctor, I could ask the appropriate questions and hear what his views were and what he thought.”
Group 3: “Just bringing information to your doctor…and talking it out and possibly coming up with an alternative to what was already set, what your medical path was going to be.”
Finally, participants reported that PGHI helped them to prepare for treatment by learning from others’ experiences. Several participants said reading about others’ treatment experiences helped them to feel less anxious and more prepared for upcoming procedures. Other participants reported learning about financial support for expensive treatments, how to navigate health insurance, and how to balance life and caregiver responsibilities.
Group 2: “You’re more prepared if you understand that this could happen [during treatment], and when it does, you’re not freaking out.”
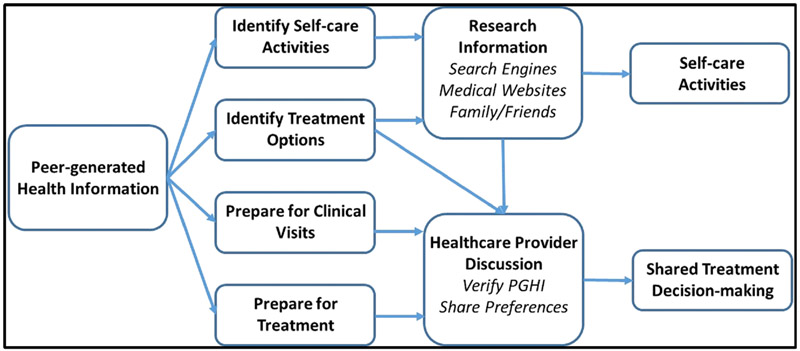
When asked to describe how PGHI fit into their decision-making process, most participants reported using PGHI as a starting point for identifying treatment options, self-care activities, and healthcare provider questions. They described filtering that information through additional research, healthcare provider discussions, and their existing knowledge and then participating in shared decision-making alongside their healthcare provider (Figure 2).
Figure 2.
Role of Peer-generated Health Information in Patient and Caregiver Health Decisions
When they encountered relevant PGHI, most participants reported their first step was to conduct further research to confirm and build on that information. They conducted this research through web searches (e.g., Google), by visiting trusted medical websites (e.g., WebMD, Science Daily), and by talking to family and friends. Next, many participants reported discussing the information with their healthcare provider.
Ultimately, participants explained that they do not make treatment decisions based on PGHI alone, although they may try self-care activities (e.g., exercises, dietary changes) without consulting a provider. Participants consistently reported using PGHI cautiously, describing it as a way to learn new information that they can research more thoroughly, discuss with healthcare providers, and incorporate into their decision-making.
Group 10: “I think you need to use both personal experiences and do your own research before making a decision.”
Group 7: “I mean, you have to use multiple sources to really find out what’s going on. You can’t go to one website and read it and say, ‘Okay, this is how it’s going to be.’”
Group 10: “If I feel it is something I need to look into, I research it on my own and then bring it to my [doctor’s] attention.”
DISCUSSION
Previous research has demonstrated how individuals use traditional online health information and has documented certain aspects of PGHI and online communities (e.g., discussion topics, credibility assessments, advantages and limitations of OHC participation). This study extends that work by identifying where individuals encounter online PGHI, when and why they engage with this information, and how they use PGHI in their health and treatment decisions.
First, we discovered that patients and caregivers use PGHI in much the same way they use traditional online health information. Many studies have established that individuals seek online health information to address unmet information needs and dissatisfaction with their current healthcare (Baker et al., 2003; Lee & Hawkins, 2010; Tustin, 2010; Wald, Dube, & Anthony, 2007). Likewise, this study found that individuals use PGHI to understand new (and potential) diagnoses, explore treatment options, and inform clinical discussions. However, individuals also use PGHI to address needs that cannot be met by traditional online sources or provider discussions, such as hearing about others’ experiences undergoing specific treatments, navigating insurance, and performing self-care activities.
Second, we found that patients and caregivers value PGHI and OHCs primarily as information sources. Although individuals do join OHCs for social support, this motivation appears far less common than the desire to gather information and hear about others’ experiences. This finding aligns with research demonstrating that offline social networks are important sources of factual health information and influence health decisions (Brunson, 2013; Jackson, Cheater, & Reid, 2008; Kim et al., 2015; Kjos, Worley, & Schommer, 2011; Smith & Christakis, 2008), and it challenges the assumption that OHCs are primarily online support groups that should be viewed through a social support lens (Chung, 2014; Wang et al., 2008).
Third, we found that most individuals accidentally discover PGHI in their broader search for online health information, rather than intentionally seeking out PGHI. Although some individuals are referred to OHCs, most patients and caregivers encounter PGHI in search engine results and begin exploring the communities that posted the information. This finding underscores again that individuals who access PGHI are primarily information seekers looking for answers rather than skeptics eschewing clinical guidance.
Finally, we found that patients and caregivers use PGHI to facilitate, rather than sidestep, shared decision-making with healthcare providers. Although individuals value PGHI, they acknowledge it is anecdotal evidence, and they seek to verify it with external resources and clinicians. They also continue to acknowledge healthcare providers as their most trusted source of health information. This suggests a conceptual model in which individuals use PGHI primarily as a starting point to identify treatment options and preparations, self-care activities, and clinical discussion topics and they ultimately consult with healthcare providers to make joint treatment decisions (Figure 2).
Surprisingly, we found few differences by sub-population (e.g., active vs. passive users, recently diagnosed vs. recent treatment decision), and individuals reported similar reasons for using PGHI regardless of activity level or phase of care. One interpretation is that active and passive users seek PGHI for the same reasons and that individuals continue to access online communities even after diagnosis and treatment decisions. Alternatively, this finding might suggest that our eligibility criteria did not effectively distinguish between sub-populations and should be strengthened in future studies.
Theoretical and Practical Implications
The study’s findings have several theoretical implications. First, the findings suggest a conceptual model for how individuals incorporate PGHI into their health decisions (Figure 2). The model suggests that PGHI is a starting point and that individuals use others’ experiences as a stepping stone for shared decision-making with healthcare providers. This model can be used when evaluating programs with PGHI components and refined through future research.
Second, the study’s findings suggest that, despite access to people with the same health condition, healthcare providers continue to be important and trusted information sources. Although individuals may try self-care activities without consulting their provider, they route almost all PGHI—explicitly or implicitly—through providers and make treatment decisions in consultation with them.
The study’s findings also have practical implications. For OHC sponsors, the findings suggest that an active web presence, fresh content, and search engine optimization may be most effective in gaining visitors. Although some individuals intentionally seek PGHI, most discover online communities through search engines. For healthcare providers, the findings suggest that patients and caregivers acknowledge the anecdotal nature of PGHI. Although individuals value others’ experiences, they do not expect identical outcomes, and they try to verify PGHI with other resources, especially healthcare providers. Consequently, providers should understand that PGHI is viewed as a complement to existing online and offline resources and should be open to discussing PGHI with patients and caregivers.
Advantages and Limitations
This study offers multiple advantages over previous research into PGHI and OHCs. First, this study examined PGHI within a broad range of health conditions and online communities, representing more than 50 medical conditions and 77 distinct OHCs. By contrast, almost all previous PGHI studies have focused on a single illness and a few websites. Thus, this study’s findings are considerably more representative of PGHI users. Second, this study sampled current PGHI users and employed qualitative methods to understand their decision-making. Unlike previous content analyses, we investigated not only what information individuals encountered online but also how they used that information in offline decisions.
Third, this study sampled both patients and caregivers. Previous studies have focused almost exclusively on patients, which is problematic given that caregivers conduct half of online health information seeking. Most importantly, this study examined the influence and role of PGHI in patient and caregiver health decisions. This is a topic untouched by previous studies but of high importance to healthcare providers and health communication scholars.
Nevertheless, this study has limitations. First, the findings are based on self-reported experiences at a single time point; a longitudinal or observational study might reveal different results. Second, this is a qualitative study of limited size, demographics, and geography, which restricts the generalizability of the findings. Third, given the eligibility criteria, the findings reflect current OHC users who are relatively active. Individuals who visit infrequently, have become inactive, or seek PGHI on other social media platforms (e.g., Twitter, Facebook) are not represented. Fourth, we did not separate patients and caregivers into different focus groups, which prevents us from identifying differences between these two audiences. Finally, participant responses and engagement may have differed by focus group mode (traditional vs. virtual), although such differences were not apparent during analysis.
Future Research
This study provides a foundation for understanding how PGHI influences health decisions, and we recommend additional research in this area. A large-scale survey of individuals who encounter PGHI could verify the findings on platforms, timing, information sources, and role in health decisions. Likewise, a longitudinal study could provide stronger evidence for how patients and caregivers encounter PGHI over the course of an illness and how they use that information when making health decisions. Finally, future studies should segment participants by role (patient vs. caregiver), medical condition, and type of OHC (e.g., public vs. private) to determine if and how their use of PGHI differs.
CONCLUSION
This study explored how patients and caregivers encounter PGHI and use it in health and treatment decisions. The findings establish that individuals use PGHI in much the same way they use traditional online health information—to learn about illnesses, treatment options, and self-care activities. The findings also demonstrate that PGHI facilitates, rather than obstructs, shared decision-making. In contrast to concerns that PGHI breeds misinformation or circumvents healthcare providers, we found that individuals view PGHI as a starting point for additional research and clinical discussions rather than a substitute for provider advice.
ACKNOWLEDGEMENTS
We would like to acknowledge Kathryn Aikin (U.S. Food and Drug Administration) for her help designing the research and Paul Wicks (PatientsLikeMe) and Dave Clifford (PatientsLikeMe) for their assistance identifying participants and collecting data. We also would like to thank Jeffrey Novey (RTI International) for his help editing the manuscript and Robert Furberg (RTI International) for his feedback on earlier drafts.
FUNDING
This research was funded by a contract from the U.S. Food and Drug Administration (FDA), Office of Prescription Drug Promotion. The findings and conclusions in this article are those of the authors and do not necessarily reflect the opinions of the FDA.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
REFERENCES
- An LC, Schillo BA, Saul JE, Wendling AH, Klatt CM, Berg CJ, Ahulwalia JS, Kavanaugh AM, Christenson M, & Luxenberg MG (2008). Utilization of smoking cessation informational, interactive, and online community resources as predictors of abstinence: Cohort study. Journal of Medical Internet Research, 10(5): e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker L, Wagner TH, Singer S, & Bundorf MK (2003). Use of the Internet and e-mail for health information: Results from a national survey. JAMA, 289(18), 2400–2406. [DOI] [PubMed] [Google Scholar]
- Banfield MA, Barney LJ, Griffiths KM, & Christensen HM (2012). Australian mental health consumers’ priorities for research: Qualitative findings from the SCOPE for Research project. Health Expectations, e-pub, doi: 10.1111/j.1369-7625.2011.00763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender JL, Jimenez-Marroquin M, & Jadad AR (2011). Seeking support groups on Facebook: A content analysis of breast cancer groups. Journal of Medical Internet Research, 13(1), e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berland GK, Elliott MN, Morales LS, Algazy JI, Kravitz RL, Broder MS, et al. (2001). Health information on the Internet: Accessibility, quality, and readability in English and Spanish. JAMA, 285(20), 2612–2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosslet GT, Torke AM, Hickman SE, Terry CL, & Helft PR (2011) The patient-doctor relationship and online social networks: Results of a national survey. Journal of General Internal Medicine, 26(10), 1168–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briss P, Rimer B, Reilley B, et al. (2004). Promoting informed decisions about cancer screening in communities and healthcare systems. American Journal of Preventive Medicine, 26(1), 67–80. [DOI] [PubMed] [Google Scholar]
- Brunson EK (2013). The impact of social networks on parents’ vaccination decisions. Pediatrics, 131(5), e1397–e1404. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, & Whelan T (1997). Shared decision-making in the medical encounter: What does it mean? (Or it takes at least two to tango). Social Science & Medicine, 44(5), 681–692. [DOI] [PubMed] [Google Scholar]
- Charmaz K (2003). Grounded theory In Smith JA (Ed.) Qualitative Psychology: A Practical Guide to Research Methods (pp. 81–110). London: SAGE Publications. [Google Scholar]
- Charmaz K, & Mitchell RG (2001). Grounded theory in ethnography In Atkinson P, Coffey A, Delamont S, Lofland J, & Lofland L (Eds.), Handbook of Ethnography (pp.160–174). London: Sage. [Google Scholar]
- Chung JE (2014). Social networking in online support groups for health: How online social networking benefits patients. Journal of Health Communication, 19(6), 639–659. [DOI] [PubMed] [Google Scholar]
- Cline RJW, & Haynes KM (2001). Consumer health information seeking on the Internet: The state of the art. Health Education Research, 16(6), 671–692. [DOI] [PubMed] [Google Scholar]
- Deber RB, Kraetschmer N, & Irvine J (1996). What role do patients wish to play in treatment decision making? Archives of Internal Medicine, 156(13), 1414–1420. [PubMed] [Google Scholar]
- Denzin NK (1970). The Research Act. Chicago: Aldine. [Google Scholar]
- Dutta MJ, & Feng H (2007). Health orientation and disease state as predictors of online health support group use. Health Communication, 22(2), 181–189. [DOI] [PubMed] [Google Scholar]
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G, Powell J, Englesakis M, Rizo C, & Stern A (2004). Health related virtual communities and electronic support groups: Systematic review of the effects of online peer to peer interactions. British Medical Journal, 328(7449), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S, & Duggan M (2013). Health Online 2013. Washington, DC: Pew Internet & American Life Project; Available from http://www.pewinternet.org/Reports/2013/Health-online.aspx. [Google Scholar]
- Fox FE, Morris M, & Rumsey N (2007). Doing synchronous online focus groups with young people: Methodological reflections. Qualitative Health Research, 17(4), 539–547. [DOI] [PubMed] [Google Scholar]
- Fox S (2011a). Health Topics. Washington, DC: Pew Internet & American Life Project; Available at http://www.pewinternet.org/Reports/2011/HealthTopics.aspx [Google Scholar]
- Fox S (2011b). Peer-to-Peer Healthcare. Washington, DC: Pew Internet & American Life Project; Available at http://www.pewinternet.org/Reports/2011/P2PHealthcare.aspx [Google Scholar]
- Fox S, & Jones S (2009). The Social Life of Health Information. Washington, DC: Pew Internet & American Life Project; Available at http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx [Google Scholar]
- Frost JH, & Massagli MP (2008). Social uses of personal health information within PatientsLikeMe, an online patient community: What can happen when patients have access to one another’s data. Journal of Medical Internet Research, 10(3), e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs G (2007). Analyzing Qualitative Data. London: SAGE Publications. [Google Scholar]
- Hesse BW, Moser RP, & Rutten LJ (2010). Surveys of physicians and electronic health information. New England Journal of Medicine, 362(9), 859–860. [DOI] [PubMed] [Google Scholar]
- Informed Medical Decisions Foundation (2012). Six steps of shared decision making (SDM). Retrieved 15 September 2015, from http://www.slideshare.net/fimdm/six-steps-of-shared-decision-making.
- Jackson C, Cheater FM, & Reid I (2008). A systematic review of decision support needs of parents making child health decisions. Health Expectations, 11(3), 232–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jodlowski D, Sharf BF, Nguyen LC, Haidet P, & Woodard LD (2007). “Screwed for life”: Examining identification and division in addiction narratives. Communication & Medicine, 4(1), 15–26. [DOI] [PubMed] [Google Scholar]
- Kim BH, Wallington SF, Makambi KH, & Adams-Campbell LL (2015). Social networks and physical activity behaviors among cancer survivors: Data From the 2005 Health Information National Trends Survey. Journal of Health Communication, 20(6), 656–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjos AL, Worley MM, & Schommer JC (2011). Medication information seeking behavior in a social context: The role of lay and professional social network contacts. Innovations in Pharmacy, 2(4), 63. [Google Scholar]
- Lee C-J (2008). Does the Internet displace health professionals? Journal of Health Communication, 13(5), 450–464. [DOI] [PubMed] [Google Scholar]
- Lee C, Wang S, & Lewis N (2010). Internet use leads cancer patients to be active health care consumers. Patient Education and Counseling, 8(1S), S63–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SY, Hawkins R (2010). Why do patients seek an alternative channel? The effects of unmet needs on patients' health-related Internet use. Journal of Health Communication, 15(2), 152–166. [DOI] [PubMed] [Google Scholar]
- Levy M, Matiesanu E, Mitskaviets I, Riley M, & Daniels D (2006). Prescription drug advertising: Benchmarking and identifying strategies to increase consumers’ engagement with online ads. Report No. HTH06-C04. New York: Jupiter Research. [Google Scholar]
- Macias W, & McMillan SJ (2008). The return of the house call: The role of Internet-based interactivity in brining health information home to older adults. Health Communication, 23(1), 34–44. [DOI] [PubMed] [Google Scholar]
- Macias W, Lewis LS, & Smith TL (2005). Health-related message boards / chat rooms on the Web: Discussion content and implications for pharmaceutical sponsorships. Journal of Health Communication, 10(3), 209–223. [DOI] [PubMed] [Google Scholar]
- Manhattan Research. (2005). For 31.6 million U.S. adults, the Internet is the first stop for health care decisions. Retrieved 26 June 2012, from http://products.manhattanresearch.com/newsroom/Press_Releases/11212005.aspx
- McMullan M (2006). Patients using the Internet to obtain health information: How this affects the patient-health professional relationship. Patient Education and Counseling, 63(1), 24–28. [DOI] [PubMed] [Google Scholar]
- Metzger MJ, Flanagin AJ, & Medders RB (2010). Social and heuristic approaches to credibility evaluation online. Journal of Communication, 60(3), 413–439. [Google Scholar]
- Miles MB, & Huberman AM (1994). Qualitative Data Analysis. Thousand Oaks, CA: Sage Publication; s. [Google Scholar]
- Modahl M, Tompsett L, & Moorhead T (2011). Doctors, patients, and social media. Retreived 20 September 2015 from http://www.quantiamd.com/q-qcp/doctorspatientsocialmedia.pdf. [Google Scholar]
- Morgan D (1998). The Focus Group Guidebook. Thousand Oaks, CA: SAGE Publications. [Google Scholar]
- Murray E, Lo B, Pollack L, Donelan K, Catania J, White M,et al. (2003). The impact of health information on the Internet on the physician-patient relationship: Patient perceptions. Archives of Internal Medicine, 163(14), 1727–1733. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (2014). Health Information National Trends Survey (HINTS) electronic codebook. Retrieved 18 September 2015 from http://hints.cancer.gov/questions.aspx.
- Oshima LO, & Emanuel EJ (2013). Shared decision making to improve care and reduce costs. New England Journal of Medicine, 368(1), 6–8. [DOI] [PubMed] [Google Scholar]
- Poehlman JA, Rupert DJ, Ray SE, & Moultrie RR (2015). How do virtual and traditional focus groups compare? Cost, recruitment, and participant perceptions. Presented at the National Conference on Health Communication, Marketing, and Media (NCHCMM), Atlanta, GA. [Google Scholar]
- Popenko NA, Devcic Z, Karimi K, & Wong BJ (2012).The virtual focus group: A modern methodology for facial attractiveness rating. Plastic and Reconstructive Surgery, 130(3), 455e–461e. [DOI] [PubMed] [Google Scholar]
- Rainie L (2010). Online Health Seeking: How Social Networks Can Be Healing Communities. Washington, DC: Pew Internet & American Life Project; Available at http://www.pewinternet.org/Presentations/2010/Oct/North-Atlantic-Health-Science-Libraries.aspx [Google Scholar]
- Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, et al. (2010). An online community improves adherence in an Internet-mediated walking program. Part 1: Results of a randomized controlled trial. Journal of Medical Internet Research, 12(4), e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimer BK, Briss PA, Zeller PK, Chan ECY, & Woolf SH (2004). Informed decision making: What is its role in cancer screening? Cancer, 101(5 Suppl), 1214–1228. [DOI] [PubMed] [Google Scholar]
- Ritchie J, & Lewis J (Eds.) (2003). Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications. [Google Scholar]
- Author et al. (2014).
- Savolainen R (2011). Judging the quality and credibility of information in Internet discussion forums. Journal of the American Society for Information Science and Technology, 62(7), 1243–1256. [Google Scholar]
- Setoyama Y, Yamazaki Y, & Nakayama K (2011). Comparing support to breast cancer patients from online communities and face-to-face support groups. Patient Education and Counseling, 85(2), e95–100. [DOI] [PubMed] [Google Scholar]
- Setoyama Y, Nakayama K, & Yamazaki Y (2009). Peer support from online community on the Internet among patients with breast cancer in Japan. Studies in Health Technology and Informatics, 146, 886. [PubMed] [Google Scholar]
- Smith KP, & Christakis NA (2008). Social networks and health. Annual Review of Sociology, 34, 405–418. [Google Scholar]
- Tates K, Zwaanswijk M, Otten R, van Dulmen S, Hoogerbrugge PM, Kamps WA, & Bensing JM (2009). Online focus groups as a tool to collect data in hard-to-include populations: Examples from paediatric oncology. BMC Medical Research Methodology, 9, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tustin N (2010). The role of patient satisfaction in online health information seeking, Journal of Health Communication, 15(1), 3–17. [DOI] [PubMed] [Google Scholar]
- Von Knoop C, Lovich D, Silverstein MB, & Tutty M (2003). Vital signs: E-health in the United States. Retrieved 20 September 2015 from https://www.bcgperspectives.com/content/articles/health_care_ehealth_in_the_united_states/. [Google Scholar]
- Wagner TH, Baker LC, Bundorf MK, & Singer S (2004). Use of the Internet for health information by the chronically ill. Preventing Chronic Disease, 1(4), A13. [PMC free article] [PubMed] [Google Scholar]
- Wald HS, Dube CE, & Anthony DC (2007). Untangling the Web: The impact of Internet use on health care and the physician-patient relationship. Patient Education and Counseling, 68(3), 218–224. [DOI] [PubMed] [Google Scholar]
- Walther JB, Slovacek C, & Tidwell LC (2001). Is a picture worth a thousand words? Photographic images in long term and short term virtual teams. Communication Research, 28(1), 105–134. [Google Scholar]
- Wang Z, Walther JB, Pingree S, & Hawkins RP (2008). Health information, credibility, homophily, and influence via the Internet: Web sites versus discussion groups. Health Communication, 23(4), 358–368. [DOI] [PubMed] [Google Scholar]
- Wicks P, Massagli M, Frost J, Brownstein C, Okun S, Vaughan T et al. (2010). Sharing health data for better outcomes on PatientsLikeMe. Journal of Medical Internet Research, 12(2), e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicks P, Keininger DL, Massagli MP, de la Loge C, Brownstein C, Isojarvi J, et al. (2012). Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy and Behavior, 23(1), 16–23. [DOI] [PubMed] [Google Scholar]