Abstract
Objective: Social distancing and hand washing with soap and water have been advocated as the main proactive measures against the spread of coronavirus. We sought to find out what other alternative materials and methods would be used among populations without running water and who may not afford alcohol-based sanitizers. Results: We reviewed studies that reported use of sand, soil, ash, soda ash, seawater, alkaline materials, and sunlight as possible alternatives to handwashing with soap and water. We identified the documented mechanism of actions of these alternative wash methods on both inanimate surfaces and at cellular levels. The consideration of use of these alternative locally available in situations of unavailability of soap and water and alcohol-based sanitizers is timely in the face of coronavirus pandemic. Further randomized studies need to be carried out to evaluate the effectiveness of these alternatives in management of SARS-Cov-2.
Keywords: coronavirus, hand wash, alternatives, sand, ash, soda ash, low-resource settings
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an enveloped strain of coronavirus that causes coronavirus disease 2019 (COVID-19).1 It is known to spread through droplets suspended in the air as well as contact with contaminated surfaces. Contaminated hands are the leading vehicles of transmission through touch on one’s eyes, mouth, and nostrils, thus introducing the virus into the mucosa.1 Viruses, including SARS-Cov-2, are wrapped in lipid membranes and attach onto the hands facilitated by the presence of body oils with both hydrophilic and hydrophobic ends.2
Desperate measures to contain the COVID-19 pandemic have been proposed ranging from hand washing, social distancing, and community containments, among others.1,3 Other public health and community-based strategies imposed by countries such as China, North America, Italy, and South Africa include cancellation of public events, restrictions on human contact games, school closures, and screening of incoming passengers at airports.1,3-5 The impact of these measures, which are majorly informed by lessons learnt from similar outbreaks, are yet to be conclusively outlined.6
Kenya has adopted a number of measures in dealing with COVID-19, including a recommendation that the government should supply the marginalized communities with water and soap for hand washing7 though this may not be sustainable due to economic challenges.
Hand washing with soap and water is now highlighted as a first-line preventive and a hygienic practice in dealing with COVID-19.8 Although this simple, yet effective action is advocated as a first-line measure to prevent the spread of coronavirus, several households from resource-limited settings, and with poor access to water and sanitation may struggle to adhere to this criterion.9 In particular, people living in rural areas and informal urban settlements in developing counties such as Kenya are more likely to be affected compared with the rest of the population.10 In Kenya alone, only 59% of the population have access to clean water services.11 The Ministry of Health organizes workshops and communication campaigns to raise awareness about the importance of hand washing with soap to prevent the spread of disease, however, only 5% of people wash their hands with soap at critical times.11 In the current unprecedented situation of COVID-19, hand washing together with cleaning of surfaces commonly shared by people is recommended to prevent the spread of virus.8 The culture of hand sanitization is foreign practice to many in the community.
In the informal settlements in Kenya, water supply is intermittent, scarce, and unaffordable for most households.12 In cases when water is available, families living in these areas struggle to strike a balance between using the scarce resource for hand hygiene and other competing basic needs such as cooking, livestock watering, and drinking.12
Although alcohol-based hand sanitizers have been suggested as an alternative to hand washing, they remain costly for many households living in the informal settlements. Furthermore, hand sanitizers are not effective in visibly soiled hands.12-14 In their study on alternative strategies for hand hygiene in resource-limited settings Sandhu and Goodnight15 suggested sustainable incremental improvement in hand washing by using available and alternative resources such as ash and soda. Such approaches would translate to the use of what is accessible and possibly effective as the communities work toward the ideal situation of soap and running water for handwashing. It therefore important to explore existing evidence to understand the alternative strategies for hand wash and cleaning of shared surfaces in absence of soap, water, or alcohol-based sanitizers.
Aim of the Study
Our aim was to document alternative, indigenous, and workable solutions in the absence of alcohol-based sanitizers, water, and soap. We reviewed studies that reported the use of locally available products that can be used to decrease virus attachment on surfaces and decontaminate exposed hands and clothes. Some studies hypothesize that viruses can be dislodged from hands and clothes when the content of dissolved organic or inorganic matter is increased to create competition for binding sites with the virus.16 Traditionally soil, ash, and salt have been used as both mechanical and chemical forms of neutralizing contaminants in soiled hands and surfaces.16,17 Dry kitchen ash has previously been recommended as an alternative to soap in hand washing in Kenya.18 The premise of the effectiveness of such materials assumes that households will obtain the soil, ash, and salt from uncontaminated sources. Contaminated soil, ash, or salt may have detrimental effects such as infections with microbes and parasites, among others.16 The availability of these alternative methods may be limited to people living in informal urban settlements areas but not in the rural areas.
Search Method
We searched the literature from PubMed to identify eligible articles. Studies were then mapped, assessed and synthesized for a narrative presentation. We used a combination of the following search terms to identify articles that we included for further assessment. (Coronavirus or COVID-19) AND (MECHANICAL), (coronavirus or COVID-19) AND (SODIUM CHLORIDE), (coronavirus or cOVID-19) AND (SAND), (coronavirus or COVID-19) AND (ALKALINE), (coronavirus or cOVID-19) AND (TEMPERATURE), (coronavirus or COVID-19) AND (SALT), (coronavirus or COVID-19) AND (ash)). A PubMed search was supplemented by a search of articles from Google Scholar and gray literature from the World Health Organization website.
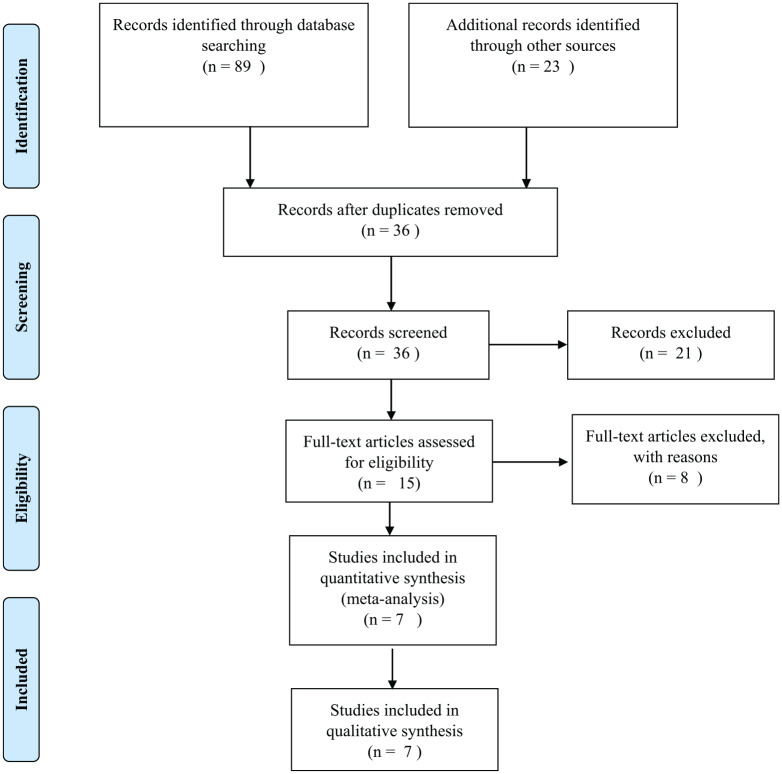
Articles were included if they met the following criteria: (1) article represents a research article (rather than a letter or commentary), (2) the primary focus of the study was to test or evaluate the effectiveness of an alternative strategy for handwashing or cleaning surfaces, (3) the study setting was a community or a resource-limited environment, or (4) studies reported the experiences of communities using the alternative strategy. Out of the 15 full-text articles that were screened at the eligibility stage, 8 were excluded for not meeting the inclusion criteria: did not evaluate the effectiveness of alternative strategy (n = 3); study setting was not a community (n = 3), and the article was not a research article (n = 2). Please see the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram showing the selection of articles (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram showing selection of articles.
Two authors (LK and AC) independently reviewed the full-text articles and where discrepancies were noted they were resolved in consultation with the third and fourth reviewer (PW) and (IN) until a consensus was built.
Results
The search did not yield significant literature that explicitly describes alternative interventions to soap and water and sanitizers for handwashing in low-income settings. This perspective remains silent to most scientists developing strategies for prevention of COVID-19 outbreak but is very crucial in targeting effectiveness of prevention in areas without access to water, the supply of soap, or sanitizers.
Few if any studies have been done specifically on the use of these traditional alternative methods in coronavirus infection. The included studies focused on the cellular level of transmission of coronavirus family,19-21 which we used for possible inferred benefits as the basis of our discussion.
Alternative Decontamination Strategies Reported by the Reviewed Papers
Use of Sea Salt and Salt Gargles
At the cellular level, hypertonic conditions have been known to inhibit coronavirus.20 At the same time, the high osmolality of sodium chloride is known to kill microbes through desiccation and dissolution of fats and oils on the surface, therefore, detaching the contaminants from colonized surfaces, including the hands.22
Gargling with naturally occurring sea water or salt solution containing chloride ions (Cl−) inhibit a number of viruses, including the coronavirus from the throat mucosa resulting in a reduction of the viral infection period with an average of 2.5 days and a reduction in viral shedding.20,21
Use of Sand, Soil, and Ash
Sand, soil, and ash have been used as hand washing agents in low resource setting.23 The act of rubbing of hands with sand generates mechanical force adequate to dislodge any form of matter on the surface of the hands and by default, carry away other types of contaminants, including microbes.17 Although the reviewed studies did not document the mechanism of action against coronavirus specifically, it is implied that these mechanical actions may be of benefit in coronavirus dislodgement. It is noted that the effectiveness of use of these alternative materials is subject to the quality and amount of water concurrently used.24 Studies on use of these materials without water are limited if available. However, an anecdotal note on fresh wood ash highlighted its alkaline nature and its use as a dry agent on surfaces such as floors, handles, and on body wastes such as vomit and blood stains.25
Use of Soda Ash Powder and Other Alkaline Materials
Effect of pH on the fusion of coronavirus with the host cell has been documented26,27 as well as the loss of its infectivity at pH of 8.27 The possibility of decreased attachment to inanimate surfaces covered with fluids of over pH of 8 may be inferred from this observation.28 Ash of any kind creates an alkaline environment that does not support the existence of most pathogens, with possibility of destabilizing coronaviruses that thrive in a pH of between 5.5 and 8.0.29 The effect of highly acidic environment on SARS-CoV-2 needs further investigation. Decreasing the pH of inanimate surfaces by rubbing pH altering acidic fruits such as lemon on hands in the event of unavailability of water need to be explored.
Heat Treatment
Temperatures higher than 27°C have been reported to reduce coronavirus infectivity in surrogate cells and inanimate surfaces.19,27,30 High temperatures and low humidity have been reported to reduce the transmission of COVID-19 by Wang et al.31 Similarly, nursing COVID-19 patients in a warm atmospheric temperature has been reported to contribute to improved survival rates.32
On this basis, it may be necessary to investigate the hypothesis that sun-drying (with temperature of over 27°C) of contaminated items like clothes and other inanimate objects may be desirable to prevent transmission of the coronavirus. This option may apply to households where infected persons have been identified and isolated. Airing personal effects in the open sun may work effectively in places with limited access to water.33 The thermal benefit may be achieved through placing items on dry black soil surfaces that can reach 60°C in tropical sun.25 Sunlight provides natural supplementation of vitamin D, which is known to protect the respiratory system by regulating secretion of pro inflammatory cytokines known to cause lung injury.34 Exposure of family members to sunshine and warmth may be beneficial in the management of COVID-19 infection.
Discussion
Our literature search did not yield much evidence to prove our hypothesis about alternatives strategies that could replace soap and water as practical community-based approaches to prevent the spread of coronavirus. However, a number of studies highlighted several methods used traditionally by local communities for decontamination purposes such as alkaline products (ash), increased temperature, reduced humidity (drying), salt, and sand. These products worked by either mechanically or chemically damaging the microbes. Although this rapid review showed that alkaline environments could potentially reduce the multiplication of the virus, this should not be confused by the myth that alkaline foods could prevent COVID-19 infection.
Application of alkaline products such as seawater, sodium bicarbonate (baking soda), calcium carbonate (limestone), and calcium hydroxide (slaked lime) on inanimate surfaces and to decontaminate hands needs to be explored for use in resource-limited settings.35 Majority of these resources are traditionally known and used by the African communities and some are readily available to rural communities in these regions.36,37 Moreover, in the food industry, alkaline materials have been explored in developing food sanitizers from naturally occurring alkaline salts38 as well as creating a favorable environment in aquatic life.39 Virucidal efficacy of sodium bicarbonate has been documented.40 Analysis of various studies by Bright et al40 postulated possible action of the viricidal effect of food substances against enveloped viruses. The proposed mechanism of action included reduction of the ability of the virus to infect host cells, inhibition of virus replication within the first few hours of contact with the host cells, viral uncoating by reducing acidification and inhibiting viral protein synthesis. Prior application on hands before exposure through outdoor activities may be more explored further to determine the additional benefit compared with post exposure use.
Variation of pH on coronavirus family has resulted in varying effect, including destabilization of the virus at low pH41,42 with the report that COVID-19 is less stable on smooth surfaces.41 The hypothesis that lemon juice could not only create an acidic environment but also contribute to the building of a rough surface hence leading to inactivation of coronavirus needs be explored. Lemon and lime juice has previously been documented to have virucidal effects, leading to the impression that it could contribute to managing COVID-19 challenge, especially in low-resource settings.43 Lemon is a readily available fruit that is stable and can be stored under all conditions.43
The use of soil to neutralize contaminants is a simple and readily available method but was reported in the literature as the least favorable due to potential spread of parasites like hookworms. However, clean sources of soil can be identified by community members and stored in designated locations within the household with ease of access.44,45
Heat or elevated temperatures have been credited as methods with a potential to inactivate viruses within minutes. This is more so in enveloped virus such as SARS-CoV-2.25,46 Marginalized communities may benefit from naturally occurring elevated temperature from the naturally heated soils or the sun.25
Our review has suggested a variety of alternative measures that could be used as stop-gap options in the absence of soap, water, and sanitizers. However, the adverse effects of these materials on humans are barely documented. One report by International Rescue Council shows that alternative methods such as the use of ash may lead to damage of the skin around the hands.25 Further studies are needed to examine how these alternative strategies are affecting communities that are already using them. Due to lack of sufficient evidence to show how the alternative approaches are affecting the communities, we still strongly recommend the use of World Health Organization guideline for social distancing and handwashing with soap and water or alcohol-based commercial sanitizers where applicable.8 This article, however, generates a critical hypothesis that should be examined in the face of COVID-19 especially in the economically developing communities. Additionally, the majority of households in urban settlements in these countries may not observe social distancing due to overcrowding and high poverty levels.47-49 Also due to poverty, the priorities of these communities are likely to be about meeting basic needs such as food and shelter rather than social distancing.
Recommendation
Randomized studies should be carried out to evaluate the effectiveness of these alternative hygiene management methods on coronavirus. The findings of such randomized studies may generate protocols for their use. These local products if proven to be effective, may reduce cost and increase access to decontamination products, especially to disadvantaged communities. The results of such studies could lead to development of policy that could be beneficial especially to the marginalized communities. The proposed alternatives to water, soap, and commercial sanitizers for hygiene and decontamination of surfaces in resource-limited settings are timely in the face of COVID-19 pandemic. These alternative products need, however, to be evaluated in order to derive evidence-based conclusions about the side effects on the skin, when used as hand sanitizers.
Limitations
Few studies have specifically been done to establish the impact of these alternative wash methods on SARS-CoV-2. The studies done at cellular levels involving SARS virus family though with some positive results may not be inferred on external and inanimate surfaces. SARS-CoV-2 may not report similar behavior to the rest of SARS family.
Acknowledgments
We acknowledge our institutions for giving us time during this unprecedented lockdown to do this study.
Footnotes
Authors Contributions: LWK and PW contributed to the conceptualization of the study, LWK, AC and IN contributed to the design and implementation of the research, analysis of the results and to the manuscript.
Declaration of Conflicting Interests: The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Lucy W. Kivuti-Bitok  https://orcid.org/0000-0002-0958-1580
https://orcid.org/0000-0002-0958-1580
Irene Ngune  https://orcid.org/0000-0003-4951-2712
https://orcid.org/0000-0003-4951-2712
References
- 1. Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020;368:m1036. [DOI] [PubMed] [Google Scholar]
- 2. Schijven JF, Hassanizadeh SM. Removal of viruses by soil passage: overview of modeling, processes, and parameters. Crit Rev Environ Sci Technol. 2000;30:49-127. [Google Scholar]
- 3. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:1708-8305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cohen J, Kupferschmidt K. Strategies shift as coronavirus pandemic looms. Science. 2020;367:962-963. [DOI] [PubMed] [Google Scholar]
- 5. Aslam S, Mehra MR. COVID-19: yet another coronavirus challenge in transplantation. J Heart Lung Transpl. 2020;39:408-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anzai A, Kobayashi T, Linton NM, et al. Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19). J Clin Med. 2020;9:601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aluga MA. Coronavirus disease 2019 (COVID-19) in Kenya: preparedness, response and transmissibility. J Microbiol Immunol Infect. Published online April 20, 2020. doi: 10.1016/j.jmii.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Home care for patients with suspected novel coronavirus (nCoV) infection presenting with mild symptoms and management of contacts: interim guidance, 20 January 2020. Accessed June 8, 2020 https://apps.who.int/iris/bitstream/handle/10665/330671/9789240000834-eng.pdf?sequence=1&isAllowed=y
- 9. Cook J, Kimuyu P, Whittington D. The costs of coping with poor water supply in rural Kenya. Water Resour Res. 2016;52:841-859. [Google Scholar]
- 10. Tutu RA, Stoler J. Urban but off the grid: the struggle for water in two urban slums in greater Accra, Ghana. Afr Geogr Rev. 2016;35:212-226. [Google Scholar]
- 11. UNICEF Kenya. Water, sanitation and hygiene. The WASH joint monitoring programme report (2019) by The World Health Organization and UNICEF found that only 59% of Kenyans have access to basic water services and only 29% have access to sanitary services. Accessed April 4, 2020 https://www.unicef.org/kenya/water-sanitation-and-hygiene
- 12. Crow B, Odaba E. Access to water in a Nairobi slum: women’s work and institutional learning. Water Int. 2010;35:733-747. [Google Scholar]
- 13. Osei-Asare C, Eshun Oppong E, Apenteng JA, et al. Managing Vibrio cholerae with a local beverage: preparation of an affordable ethanol based hand sanitizer. Heliyon. 2020;6:e03105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shamian J, Petch T, Lilius F, Shainblum E, Talosi R. What’s the plan? The unique challenges facing the home and community care sector in preparing for a pandemic. Healthc Pap. 2007;8:38-43. [DOI] [PubMed] [Google Scholar]
- 15. Sandhu MP, Goodnight J. Community handwashing guide: utilizing available resources to initiate a handwashing intervention. World Med Health Policy. 2014;6:39-50. [Google Scholar]
- 16. Afroz A, Nasreen S, Unicomb L, et al. Perceptions, practices and barriers of handwashing in rural Bangladesh. Am J Trop Med Hyg. 2010;83:104.20595486 [Google Scholar]
- 17. Bloomfield F, Nath J. Use of ash and mud for handwashing in low income communities. Accessed June 8, 2020 https://www.ifh-homehygiene.org/review-best-practice/use-ash-and-mud-handwashing-low-income-communities
- 18. UNICEF. Consolidated results report (2011. Mtr)—Kenya Programme Cycle : 2009-2013. Accessed June 8, 2020 https://www.unicef.org/about/execboard/files/Kenya_CPD-CRR-2009-2013.pdf
- 19. Belouzard S, Millet JK, Licitra BN, Whittaker GR. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses. 2012;4:1011-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ramalingam S, Graham C, Dove J, Morrice L, Sheikh A. A pilot, open labelled, randomised controlled trial of hypertonic saline nasal irrigation and gargling for the common cold. Sci Rep. 2019;9:1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rousse M, Cucuat N, Janicot C, Shrivastava R. Innovative scientific concept of topical virus glycoprotein inhibitors incorporated in hyperosmotic glycerol revolutionizes future prospects in the treatment of viral and bacterial throat infections. Int J Pharm Sci Drug Res. 2014;6:1-11. [Google Scholar]
- 22. Crassas Y, Blache D. Aqueous saline solutions for the destruction of fatty tissue. Accessed June 8, 2020 https://patents.google.com/patent/US20110262562A1/en
- 23. Nizame FA, Nasreen S, Halder AK, et al. Observed practices and perceived advantages of different hand cleansing agents in rural Bangladesh: ash, soil, and soap. Am J Trop Med Hyg. 2015;92:1111-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hoque BA. Handwashing practices and challenges in Bangladesh. Int J Environ Health Res. 2003;13(suppl 1):S81-S87. [DOI] [PubMed] [Google Scholar]
- 25. Mandal T. Ash as a neglected low-cost alternative for soap for hand washing (and disinfectant) relevant for Ebola prevention—and some more suggestions. Accessed May 20, 2020 https://www.ircwash.org/resources/ash-neglected-low-cost-alternative-soap-hand-washing-and-disinfectant-relevant-ebola
- 26. Chu VC, McElroy LJ, Chu V, Bauman BE, Whittaker GR. The avian coronavirus infectious bronchitis virus undergoes direct low-pH-dependent fusion activation during entry into host cells. J Virol. 2006;80:3180-3188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sturman LS, Ricard CS, Holmes KV. Conformational change of the coronavirus peplomer glycoprotein at pH 8.0 and 37 degrees C correlates with virus aggregation and virus-induced cell fusion. J Virol. 1990;64:3042-3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sattar SA, Springthorpe VS, Karim Y, Loro P. Chemical disinfection of non-porous inanimate surfaces experimentally contaminated with four human pathogenic viruses. Epidemiol Infect. 1989;102:493-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jo SK, Kim HS, Cho SW, Seo SH. Pathogenesis and inflammatory responses of swine H1N2 influenza viruses in pigs. Virus Res. 2007;129:64-70. [DOI] [PubMed] [Google Scholar]
- 30. Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol. 2010;76:2712-2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang J, Tang K, Feng K, Lv W. High temperature and high humidity reduce the transmission of COVID-19. Accessed June 8, 2020 https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3551767
- 32. Cai Y, Huang T, Liu X, Xu G. The effects of “Fangcang, Huoshenshan, and Leishenshan” makeshift hospitals and temperature on the mortality of COVID-19. medRxiv. Published online March 6, 2020. doi: 10.1101/2020.02.26.20028472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thomas PR, Karriker LA, Ramirez A, et al. Evaluation of time and temperature sufficient to inactivate porcine epidemic diarrhea virus in swine feces on metal surfaces. J Swine Health Production. 2015;23:84-90. [Google Scholar]
- 34. Grant WB, Lahore H, McDonnell SL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12:988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Halevy I, Bachan A. The geologic history of seawater pH. Science. 2017;355:1069-1071. [DOI] [PubMed] [Google Scholar]
- 36. Mamiro P, Nyagaya M, Kimani P, et al. Similarities in functional attributes and nutritional effects of Magadi soda and bean debris-ash used in cooking African traditional dishes. Afr J Biotechnol. 2011;10:1181-1185. [Google Scholar]
- 37. Fakhri Y, Amanidaz N, Zandsalimi Y, et al. Association between sodium bicarbonate consumption and human health: a systematic review. Int J Med Res Health Sci. 2016;5:22-29. [Google Scholar]
- 38. Hinton A. Formulating poultry processing sanitizers from alkaline salts of fatty acids. J Food Microbiol Saf Hyg. 2017;1:116-117. [Google Scholar]
- 39. Martins G, Tarouco F, Rosa C, Robaldo R. The utilization of sodium bicarbonate, calcium carbonate or hydroxide in biofloc system: water quality, growth performance and oxidative stress of Nile tilapia (Oreochromis niloticus). Aquaculture. 2017;468:10-17. [Google Scholar]
- 40. Bright KR, Gilling DH. Natural virucidal compounds in foods. In: Goyal SM, Cannon JL, eds. Viruses in Foods. Springer; 2016:449-469. [Google Scholar]
- 41. Chin A, Chu J, Perera M, et al. Stability of SARS-CoV-2 in different environmental conditions. medRxiv. Accessed June 8, 2020 https://www.medrxiv.org/content/10.1101/2020.03.15.20036673v2 [DOI] [PMC free article] [PubMed]
- 42. Rabenau HF, Cinatl J, Morgenstern B, Bauer G, Preiser W, Doerr HW. Stability and inactivation of SARS coronavirus. Med Microbiol Immunol. 2005;194:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Short RV. New ways of preventing HIV infection: thinking simply, simply thinking. Philos Trans R Soc Lond B Biol Sci. 2006;361:811-820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Amoah ID, Singh G, Stenstrom TA, Reddy P. Detection and quantification of soil-transmitted helminths in environmental samples: a review of current state-of-the-art and future perspectives. Acta Trop. 2017;169:187-201. [DOI] [PubMed] [Google Scholar]
- 45. Tchakounte BN, Nkouayep VR, Pone JW. Soil contamination rate, prevalence, intensity of infection of geohelminths and associated risk factors among residents in Bazou (West Cameroon). Ethiop J Health Sci. 2018;28:63-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pinon A, Vialette M. Survival of viruses in water. Intervirology. 2018;61:214-222. [DOI] [PubMed] [Google Scholar]
- 47. Gilbert A. Slums and shanties. In: Orum AM, ed. The Wiley Blackwell Encyclopedia of Urban and Regional Studies. Wiley; 2019:1-9. [Google Scholar]
- 48. Kimani-Murage EW, Muthuri SK, Oti SO, Mutua MK, van de Vijver S, Kyobutungi C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS One. 2015;10:e0129943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kimani-Murage EW, Schofield L, Wekesah F, et al. Vulnerability to food insecurity in urban slums: experiences from Nairobi, Kenya. J Urban Health. 2014;91:1098-1113. [DOI] [PMC free article] [PubMed] [Google Scholar]