Abstract
The novel RNA betacoronavirus SARS-CoV-2 is driving great efforts in clinical and basic research and several studies of the epidemiology, risk factors, clinical and virological features of this infection are already available. However COVID-19 is a totally new pathological entity, and many gray areas regarding associated diseases still need to be elucidated, especially in the group of patients who suffer from preexistent gastrointestinal disease. The aim of this review is to summarize the published data on the correlation between chronic gastrointestinal disorders and COVID-19.
Keywords: COVID-19, SARS-CoV-2, chronic gastrointestinal disorders, inflammatory bowel disease
The high number of infected and deceased patients during the global pandemic of the novel RNA betacoronavirus, also called SARS-CoV-2, is driving great efforts in clinical and basic research [1]. Since the discovery of SARS-CoV-2 at the end of 2019, several studies of the epidemiology, risk factors, clinical findings, therapy and virological features of this infection have become available and are totally free to clinicians via a PubMed search [1,2].
In the great Italian epidemic area, the fight against this infection is showing the first signs of improvement due to the rapid spread of knowledge and the more severe social restrictions adopted. During the first days of April 2020, a better understanding of the mechanisms of diffusion and pathogenesis of SARS-CoV-2 infection led to a decrease in newly infected subjects and in patients’ hospitalization, in both regular wards and ICU recovery, and a progressive flattening in the daily number of deaths [3]. However COVID-19 is a totally new pathological entity and many gray areas regarding associated diseases still need to be elucidated. In particular, several risk factors that are involved in acquiring the infection and that affect the clinical course and severity of COVID-19-related diseases have been identified (Figure 1), but conclusive data are still lacking [2,4].
Figure 1.
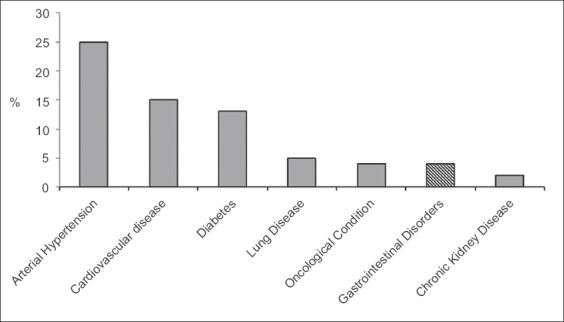
Rate (%) of underlying comorbidities in COVID-19 patients
There is growing evidence, recently summarized in a systematic review [5], that cardiovascular diseases, particularly arterial hypertension, diabetes and advanced age are the major negative prognostic factors for both contagion and disease severity [5]. Similarly, chronic pneumopathy, chronic kidney diseases, immunosuppression, and oncological conditions were found to be highly prevalent in COVID-19 patients, especially in those who progress to SARS and require intensive care [4-6].
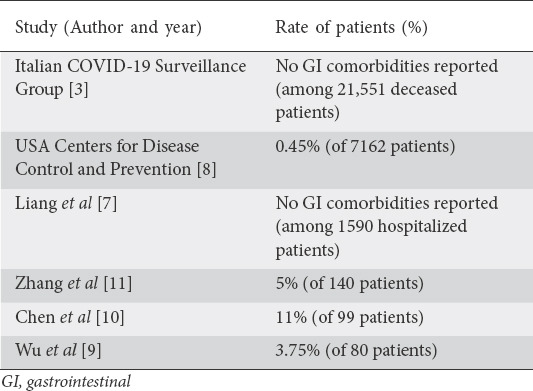
In contrast, there remain very few published reports about SARS-CoV-2 infection in the setting of chronic gastrointestinal (GI) disorders (Table 1). A retrospective analysis of data from 1590 hospitalized COVID-19 patients in epicentral and non-epicentral areas of China did not show a high prevalence of preexistent chronic GI comorbidities in these patients [7]. Preliminary data from the USA’s Centers for Disease Control and Prevention regarding 7162 COVID-19 patients demonstrated a negligible (32 cases; 0.45%) prevalence of underlying GI diseases [8]. Current epidemiological data from deceased patients in Italy also did not report a significant rate of GI comorbidity in these patients [3]. However, data from a multicenter Chinese study found that GI diseases were the third most common comorbidity, being present in 3.75% of 80 hospitalized COVID-19 patients [9]. A higher rate (11%) of preexistent GI disorders was also reported for 99 COVID-19 patients in Wuhan [10]. Unfortunately, neither of these studies specified which conditions were reported as chronic GI disorders. Only one study specifically described a 5% rate of chronic gastritis and gastric ulcer in 140 COVID-19 patients in Wuhan [11]. Moreover, none of the abovementioned studies evaluated a possible correlation between these comorbidities and the course of COVID-19-related diseases.
Table 1.
Chronic gastrointestinal comorbidities in COVID-19 patients
As far as inflammatory bowel disease (IBD) is concerned, there are no data to suggest a higher risk of SARS-CoV-2 infection or a higher severity of related diseases in these patients, compared to the general population. To date, only one of the IBD patients in the 7 largest IBD referral centers of China has tested positive for COVID-19 [12,13]. Current data from the SECURE IBD database show that worldwide barely 700 cases of around 2,400,000 identified COVID-19 patients had underlying IBD [13].
Notably, in vitro studies suggest that a soluble form of angiotensin converting enzyme (ACE) 2, over-expressed in both inflamed intestine and blood of IBD patients, may be a competitive ligand for SARS-CoV-2, reducing full-length virus binding to cell surface and possibly limiting infection spread in these subjects [14]. However, a fatal case of COVID-19 pneumonia has recently been reported in an 80-year-old Italian female patient, admitted during recovery from left-side ulcerative colitis reactivation treated with systemic steroid therapy [15]. World Health Organization recommendations discourage steroid use in COVID-19, because of the risk of viral spreading, but rapid steroid tapering or discontinuation is notoriously dangerous in IBD patients with active, severe disease. Therefore, in the absence of clear SARS-CoV-2 infection symptoms, it is reasonable to maintain the scheduled steroid treatment until its ending [12,16].
With regard to pediatric IBD patients, only 8 children have had COVID-19 globally, all with mild infection and no need for hospitalization, despite therapy with immunomodulators and/or biologics. No cases have been reported in China and South Korea, but in 79 pediatric patients biological treatment was preventively delayed, and 17 (22%) of them showed IBD reactivation [17]. At present, there is no evidence that would justify stopping biological and immunosuppressive treatments in epidemic areas, taking into account the high risk of IBD reactivation and hospitalization, especially in a pediatric setting. However, starting a new treatment with these drugs is not recommended in epidemic areas [12]. Based on these considerations, accurate surveillance is required in IBD patients receiving steroid, immunosuppressive or biological therapy, including strict social isolation [12,16]. As suggested by Chinese and European IBD associations, patients need to be remotely managed with telephone contacts and minimal access to the hospital structure, whenever possible [12,18].
Regarding the liver, it has been observed that chronic liver diseases (cirrhosis, nonalcoholic fatty liver disease, etc.) were present in 2-11% of patients with COVID-19. On the other hand, alteration of liver enzymes, albumin reduction and increased bilirubin may occur in as many as 14-53% of patients, more frequently in the severe form of the disease. Therefore, liver function should be properly monitored during the disease so as to promptly detect any worsening. It is unclear whether the alterations of liver function depend on the viral infection or the hepatotoxicity of drugs used [19].
Mild acute pancreatitis was reported in 17% of 52 patients during COVID-19 pneumonia, and it was supposed that high ACE2 expression in pancreatic β-cells may be a possible viral target [20,21]. β-cell injury causes an alteration of glycemic control and a worsening of preexisting diabetes in these patients. It is thus conceivable that patients affected by underlying chronic pancreatitis may have a more severe course regarding these COVID-19-related complications during the infection. Therefore, patients with chronic pancreatitis should be appropriately informed by clinicians about this risk.
At present, no data are available on SARS-CoV-2 infection in patients with celiac disease or other chronic GI diseases.
In conclusion, during the new COVID-19 pandemic emergency, the efforts of gastroenterologists should be aimed towards a better understanding of COVID-19-related diseases in the setting of chronic GI disorders. More specifically, prospective studies to analyze the risk of the infection and its possible course in patients with IBD, pancreatitis and liver diseases are needed in order to improve care for these patients.
Biography
Santa Maria Hospital of Orvieto; Apuane Hospital of Massa; General Hospital of Perugia; Riuniti Hospital, Foggia; Nuovo Regina Margherita Hospital, Rome, Italy
Footnotes
Conflict of Interest: None
References
- 1.Ren LL, Wang YM, Wu ZQ, et al. Identification of a novel coronavirus causing severe pneumonia in human:a descriptive study. Chin Med J (Engl) 2020;133:1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun Y, Koh V, Marimuthu K, et al. Epidemiological and clinical predictors of COVID-19. Clin Infect Dis. 2020 Mar 25; doi: 10.1093/cid/ciaa322. [Epub ahead of print]. doi:10.1093/cid/ciaa322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Italian COVID-19 surveillance group. Characteristics of COVID-19 patients dying in Italy. Report based on available data on April 6th. 2020. [Accessed 6 May 2020]. Available from:https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_6_april_2020.pdf .
- 4.Wynants L, Van Calster B, Bonten MMJ, et al. Prediction models for diagnosis and prognosis of Covid-19 infection:systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19:a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 6.Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2:a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang WH, Guan WJ, Li CC, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicenter) and outside Hubei (non-epicenter):A Nationwide Analysis of China. Eur Respir J. 2020;55:2000562. doi: 10.1183/13993003.00562-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Service/Centers for Disease Control and Prevention:Covid-19 response team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus disease 2019 —United States, February 12–March 28 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu province:a multicenter descriptive study. Clin Infect Dis. 2020 Feb 29; doi: 10.1093/cid/ciaa199. [Epub ahead of print]. doi:10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China:a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 Feb 19; doi: 10.1111/all.14238. [Epub ahead of print]. doi:10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 12.Mao R, Liang J, Shen J, et al. Society of IBD Chinese Elite IBD Union;Chinese IBD Quality Care Evaluation Center Committee. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol. 2020;5:30076–30085. doi: 10.1016/S2468-1253(20)30076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SECURE IBD database. [Accessed 6 May 2020]. Available from:https://covidibd.org/current-data/
- 14.Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J Crohns Colitis. 2020 Mar 26; doi: 10.1093/ecco-jcc/jjaa061. [Epub ahead of print] doi:10.1093/ecco-jcc/jjaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mazza S, Sorce A, Peyvandi F, Vecchi M, Caprioli F. A fatal case of COVID-19 pneumonia occurring in a patient with severe acute ulcerative colitis. Gut. 2020;69:1148–1149. doi: 10.1136/gutjnl-2020-321183. [DOI] [PubMed] [Google Scholar]
- 16.Rubin DT, Abreu MT, Rai V, Siegel CA International Organization for the Study of Inflammatory Bowel Disease. Management of patients with Crohn's disease and ulcerative colitis during the COVID-19 pandemic:results of an International Meeting. Gastroenterology. 2020 Apr 6; [Epub ahead of print]. doi:10.1053/j.gastro.2020.04.002. [Google Scholar]
- 17.Turner D, Huang Y, Martín-de-Carpi J, et al. Paediatric IBD Porto group of ESPGHAN. COVID-19 and paediatric inflammatory bowel diseases:Global experience and provisional guidance (March 2020) from the Paediatric IBD Porto group of ESPGHAN. J Pediatr Gastroenterol Nutr. 2020;70:727–733. doi: 10.1097/MPG.0000000000002729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.IOIBD Update on COVID19 for patients with Crohn's disease and ulcerative colitis. [Accessed 6 May 2020]. Available from:https://www.ioibd.org/ioibd-update-on-covid19-for-patients-with-crohns-disease-and ulcerative-colitis/
- 19.Zhang C, Shi L, Wang F. Liver injury in COVID-19:management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang F, Wang H, Fan J, Zhang Y, Wang H, Zhao Q. Pancreatic injury patterns in patients with COVID-19 pneumonia. Gastroenterology. 2020 Apr 1; doi: 10.1053/j.gastro.2020.03.055. [Epub ahead of print]. doi:10.1053/j.gastro.2020.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maddaloni E, Buzzetti R. Covid-19 and diabetes mellitus:unveiling the interaction of two pandemics. Diabetes Metab Res Rev. 2020 Mar 31; doi: 10.1002/dmrr.3321. [Epub ahead of print]. doi:10.1002/dmrr.3321. [DOI] [PMC free article] [PubMed] [Google Scholar]


