Purpose of review
The novel coronavirus-2019 disease (COVID-19) pandemic has had devastating consequences on healthcare systems globally. The effect this has on urologists and the patients they care for is not fully understood and presents the challenge of prioritizing the most urgent cases. We aim to review the impact on urology services and evaluate strategies to minimize disruption.
Recent findings
Various healthcare systems have been forced to postpone treatment for many urological conditions as resources are dedicated to the treatment of COVID-19. Training has been postponed as staff are reallocated to areas of need. Face-to-face contact is largely minimized and innovative, virtual communication methods are used in the outpatient setting and multidisciplinary team meetings. Surgical practice is changing because of the risks posed by COVID-19 and procedures can be prioritized in a nonurgent, low priority, high priority or emergency category.
Summary
Although the COVID-19 pandemic will inevitably affect urological services, steps can be taken to mitigate the impact and prioritize the patients most in need of urgent care. Similarly, in future; simulation, e-learning and webinars will allow interaction to share, discuss and debate focused training and education.
Keywords: anaesthesia, coronavirus, novel coronavirus-2019 disease, endourology, laparoscopy, training, urology, ventilation
KEY POINTS
Covid-19 has had an unprecedented effect on global healthcare.
It has severely struck the urological services leading to delay in treatment.
Patient suffering and oncological consequences of delayed treatment could worsen clinical outcomes.
There will be severe impact on surgical training, potentially affecting trainee progression.
INTRODUCTION
Since the first cases were identified in Hubei Province, China, in December 2019, the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has relentlessly spread around the world affecting all inhabited continents [1]. As of the 7th April 2020, more than 1.2 million people have been infected with approximately 67 000 deaths globally. The WHO declared novel coronavirus-2019 disease (COVID-19), caused by SARS-CoV-2, to be a public health emergency and a pandemic on 11th March 2020 [2].
SARS-CoV-2 causes a wide range of clinical manifestations from asymptomatic infection to death [3]. The majority of patients develop a mild upper respiratory tract infection with fever that does not require hospitalization in most cases. However, a significant proportion of patients develop severe viral-pneumonia, which can result in respiratory failure requiring mechanical ventilation. Overall, the fatality rate due to COVID-19 is currently estimated to be between 1 and 5% [4]. However, this is higher in older patients and those with comorbidities including hypertension, diabetes, cancer and coronary heart disease [3].
The key initial management for all suspected cases is infection control and prevention by isolation into a separate area and adequate protective personal equipment (PPE) [5]. Diagnosis will require laboratory confirmation. Nasopharyngeal swabs and sputum are widely tested using the real-time transcription polymerase chain reaction. Radiological imaging of the chest including x-ray and computed tomography can be used to aid diagnosis. Currently, serology testing is under development aiming to identify antibodies to SARS-CoV-2 [6].
The rapid, overwhelming surge of COVID-19 cases has resulted in unprecedented numbers of critically unwell patients requiring ICU treatment, straining health systems globally. As ICU and hospitals are overwhelmed by the impact of COVID-19, the progressive cancellation of elective services is widely enacted.
IMPLICATIONS TO CLINICAL PRACTICE
The significant increase in demand on critical care facilities in health systems throughout the world has had extensive implications on the urological service provision [7▪–9▪]. The number of patients requiring intubation and ventilation to manage respiratory failure from COVID-19 has resulted in the redeployment of anaesthetists to ICUs. In many cases, ventilators and theatres are being repurposed to ICUs as existing facilities are overburdened by the number of cases requiring admission. Furthermore, the number of acutely unwell patients requiring admission to the hospital has meant that wards have been allocated for the care of those with COVID-19, reducing availability of bed space for non-COVID-19 patients. Medical staff are at particular risk of developing COVID-19 from increased exposure to the virus, especially in areas where there is reduced availability of adequate PPE [10]. This can result in staff shortages throughout hospitals, necessitating redeployment to areas most in need such as ICU and the emergency department. Many organizations and governments have ordered a suspension of elective surgeries as a consequence of this. The impact on individual centres will vary in intensity and timing; however, the urologist should be prepared to work outside of their usual range of practice in the depths of the crisis.
As a speciality, urology provides a variety of services to the local population. This ranges from lower priority surgical procedures including circumcision and vasectomy to emergency procedures for testicular torsion or infected obstructed kidneys. Urology services must focus on continuing to provide an emergency service, while postponing lower priority procedures to allow capacity for COVID-19 cases. The challenge for urology departments is managing cases that lie somewhere between these two categories including those with malignancy or awaiting renal transplantation for end-stage renal failure.
NON-ONCOLOGICAL DISEASES
Renal stone disease
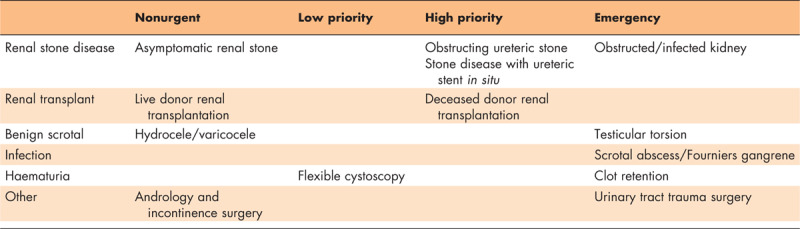
Although a benign condition, many cases of renal stones present a serious threat to health if associated with renal impairment and/or infection Table 1. Cases awaiting surgery should be carefully evaluated to determine their priority. Renal stone treatment may need to be postponed and only ureteric stones treated actively. Preferential cases would be those with a solitary kidney, renal impairment, associated with sepsis or with a ureteric stent in situ for a prolonged period. Ureteric stents can increase the risk of infection and stent encrustations, making their removal challenging. Stent encrustation can be seen in 76.3% of cases when left in situ for more than 12 weeks [11]. In patients where stents have been left in situ for over six months, complications can arise from longer procedural time or the need for multistep invasive procedures [12].
Table 1.
Showing prioritization for nononcological disease
Alternatives to ureteroscopy or percutaneous nephrolithotomy such as shockwave lithotripsy should be utilized where possible as these can be performed as an outpatient procedure and reduce the need for a general anaesthetic [13]. When stone surgery is performed and ureteric stenting is required, stent-on-strings should be considered to avoid further hospital attendance for removal. Although there is a 10% risk of premature stent dislodgement with string use, this was not associated with adverse outcomes [14].
Renal transplant
Decisions regarding renal transplantation can be particularly challenging with many patients dying on the waiting list which is usually long, yet transplantation can lead to increased risk of exposure to COVID-19 and mortality [15].
Patients with chronic kidney disease are at an increased risk of mortality from COVID-19 [16]. Those requiring haemodialysis will still need attend a healthcare setting regularly, which increases the potential exposure to the virus [17].
Renal transplant patients are on life-long immunosuppression leaving them more susceptible to infectious diseases, which is particularly relevant in the immediate postoperative period when on a high-dose induction regimen [18]. Although at a higher risk of developing severe disease in COVID-19, early recognition and appropriate treatment can improve prognosis [19].
Some may require intensive or high dependency care postoperatively which may not be possible during the COVID-19 pandemic [20]. In-depth counselling with the patient about the risks is essential. To reduce transmission risk, while addressing the current demand of transplantation, deceased donors should be prioritized but live donors should be delayed.
Other benign urological diseases
Bladder outflow obstruction secondary to benign prostatic enlargement (BPH) can be managed conservatively with a urethral catheter or suprapubic catheter and surgical management deferred until the pandemic has eased. Similarly, surgery for urinary incontinence and andrology or infertility procedures should be suspended to reduce burden on theatres and staffing. Benign scrotal procedures for disease such as epididymal cyst or hydrocoele are usually performed for mild symptoms and can therefore be deferred [21]. Although usually performed as a day-case procedure, prolonged length of stay or readmission may be required from haematoma or infection in the postoperative period.
ONCOLOGICAL DISEASES
Renal cancer and upper urinary tract cancer
Renal cell carcinoma (RCC) usually presents late with up to 30% having metastatic disease on initial diagnosis and is therefore associated with high mortality [22]Table 2. However, if diagnosed early, active surveillance and delaying treatment up to three months in stage T1 RCC does not worsen prognostic outcomes. Ablative treatments could be considered for cT1a tumours rather than surgical intervention [23]. Stage T2 RCC with scheduled nephrectomy could be considered to be postponed for one month with considerations of patient and tumour characteristics [23]. Stage T3 and above RCC, especially those extending into the inferior vena cava are aggressive tumours requiring prompt treatment. They may be more technically challenging, associated with a longer length of stay and higher risk of postoperative complications like requiring haemodialysis and ICU admission [24]. Hence, treatment need not be delayed for Stage T3+ RCC but careful counselling of risks are required.
Table 2.
Showing prioritization for oncological disease
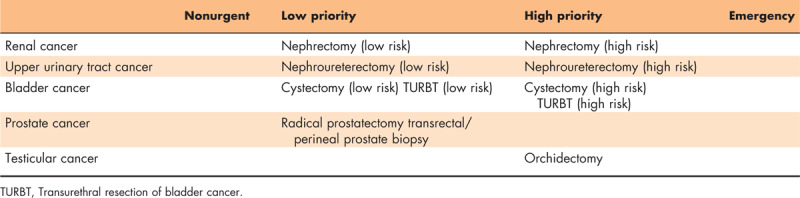
Delaying surgery in low-grade nonmuscle-invasive uppertract urothelial carcinoma (UTUC) for up to three months does not affect survival outcome [25,26]. However, delaying radical nephroureterectomy in high-grade invasive UTUC is associated with a significant progression of disease [27].
Bladder cancer
Two-thirds of bladder cancer cases are nonmuscle-invasive bladder cancer (carcinoma in situ, Ta and T1) [28]. High-grade T1 bladder cancer is associated with a high risk of recurrence and understaging at transurethral resection of bladder cancer (TURBT) [29]. Cases that are clinically deemed to be T1 should be prioritized for TURBT because of the risk of muscle-invasive bladder cancer (MIBC). Delaying treatment of MIBC by three months is associated with worse overall survival rates [30]. Similarly, delaying radical cystectomy by more than 10 weeks after neoadjuvant chemotherapy is associated with worse overall survival [31]. However, radical cystectomy is a major operation and the median length of stay is seven days even on an enhanced recovery after surgery pathway and ICU admission may be required [32,33]. The stage and grade of tumour and the availability of postoperative high-care bed should guide cystectomy procedures. Patients who are cisplatin-eligible should be offered this even more actively than before. Cisplatin ineligible MIBC should be offered a radical cystectomy within 12 weeks.
Prostate cancer
A watch and wait approach is often adopted for many patients with prostate cancer. Postponing radical prostatectomy has not been associated with increased risk of biochemical or clinical recurrence of prostate cancer in those with low or intermediate-risk groups [34]. Even in high-risk disease, the risk of recurrence increased only after 12 months, suggesting radical prostatectomy can be considered to be postponed [34,35]. Other treatment modalities including radiotherapy and androgen deprivation therapy should be considered with the multidisciplinary team [36]. Some centres have stopped performing prostate biopsies during the outbreak [37]. Additional consideration should be given to performing transperineal prostate biopsy under fusion MRI guidance scan as opposed to transrectal prostate biopsies for diagnostic purposes as SARS-CoV-2 RNA has been identified in 29% of faecal samples in patients with COVID-19 and may be a potential route for transmission of infection [38].
Testicular cancer
Delayed presentation, diagnosis and orchidectomy of testicular cancer is associated with higher rates of mortality from testicular cancer [39,40]. Orchidectomy also serves the purpose of providing tissue for diagnosis and risk stratification to determine further management including chemotherapy [41]. Inguinal orchidectomy for testicular cancer can be performed as a day case procedure, reducing pressure on beds [42]. Therefore, radical orchidectomy is high priority and should be performed whenever possible.
Emergency urology service
In the event that pressures on hospital resources by the COVID-19 pandemic are so great that high-priority malignancy operations have to be delayed, an emergency service must be maintained to provide surgery for ‘life-or-limb’ cases. This may mean that more innovative management options are pursued. In certain situations, surgery is mandated, such as debridement of Fournier's gangrene, exploration and fixation of testicular torsion or drainage of urosepsis.
In urinary retention as a result of BPH for example, a urethral catheter should be used to relieve the obstruction. Similarly, renal colic should be managed conservatively wherever possible. However, in cases of an infected and obstructed kidney, decompression and intravenous antibiotics are indicated. Urosepsis associated with nephrolithiasis can be associated with severe illness and even death with ICU admission required in as many as 18% of patients [43] Decompression can be facilitated with either ureteric stenting or percutaneous nephrostomy. Careful consideration should be given to which procedure is chosen as nephrostomy under local anaesthetic can spare a ventilator [44]. In centres with suitable experience, ureteric stenting under local anaesthetic in the outpatient setting can be considered [45]. Definitive stone surgery can then be postponed for a few weeks.
Laparoscopic procedures
The Royal College of Surgeons [46] and Society of American Gastrointestinal and Endoscopic Surgeons [47] advise caution when performing laparoscopic surgery due to limited evidence of the risk posed by COVID-19. The potential exposure to aerosolized biological fluid carried within surgical smoke or while removing trocars or surgical specimens can result in an explosive release of smoke, risking COVID-19 aerosol exposure. Although it can potentially be mitigated by the use of smoke filters, smoke extraction devices and use of PPE.
OUTPATIENT
‘Telemedicine’ and ‘Telehealth’ are consultations using electronic devices, for example, telephone or video call. Since the COVID-19 outbreak, it is much more widely used in different countries to reduce face-to-face contact, while addressing a patient's medical concerns. Video calls should be the preferential option as it provides visual cues to help gain better rapport [48,49].
In the cases where face to face contact is necessary, further stratification is required. All appointments requiring attendance should be screened, ensuring the patient is well and COVID-19 infection risk is low. Clinicians should be wearing adequate PPE including eye protection, gloves, fluid repellent surgical masks and fluid resistant aprons [5,8▪].
Routine appointments for elective procedures should be postponed. Postoperative follow-up could be initially addressed via telephone or video consultation and assessed for the need of a face to face appointment. Urgent appointments for suspected malignancy or obstructive uropathy should still proceed with screening [8▪].
FUTURE IMPLICATIONS
The long-term impact of the pandemic is difficult to fully appreciate, while still in the midst of the crisis and the effects are likely to have long-lasting implications. The toll on mental health and training progression of medical staff should not be overlooked and colleagues may be in need of support. The effects of delaying procedures and diagnosis may have far-reaching effects that will not be understood for many years. It might also mean testing of all patients on wards and in theatres.
TRAINING
All trainees have been greatly impacted in the COVID-19 outbreak. In several countries, trainees are no longer rotating as per their scheduled training program with many being redeployed to areas of need like emergency department, medicine or ICU. The focus is service provision and training opportunities have subsequently suffered. Routine procedures are no longer being performed, prioritizing emergency or cancer surgeries. Only experienced surgeons will perform these procedures to ensure efficiency with minimal staffing. Exams and training courses essential for progression are being cancelled. This combined with the lack of training opportunities could be detrimental to trainee progression [8▪,50]. However, these might lead to development of online courses and journal clubs. It will also allow for more online training and simulation as an emerging field and a solution for urologists to address those and similar situations. Simulation training would allow a safe environment for trainees to acquire and enhance surgical skills [51]. Similarly, in future, e-learning and webinars will allow interaction to share, discuss and debate focused training and education.
MENTAL HEALTH
Deterioration of mental health could be a major issue amongst all clinicians. During the unprecedented crisis, clinicians will be faced with more stress than ever before, personally and professionally. Workload may have significantly increased and some clinicians may be working in areas outside the remit of their expertise. The simple fear of spreading the virus to their closest and especially in those living with vulnerable members brings a large amount of psychological burden. Mental health support will be paramount to ensure the wellbeing of clinicians during and following the pandemic [52].
Outpatient and surgical waiting time
Waiting lists for outpatient appointments and surgical procedure has been an issue prior to the pandemic. With the additional cancellations and rescheduling, the backlog will be a major issue that will need addressing in due course.
As the surgical waiting time further lengthens, patients may present with more advanced disease leading to increasingly complex procedures. As procedures become complex, more senior, experienced surgeons will be required to perform these and training opportunities may be further impeded.
The use of ‘telemedicine’ could be more widely used in the outpatient settings following the pandemic, to help with efficiency and guide prioritization according to clinical need. The future following the pandemic remains uncertain but issues addressed above expresses the necessity of careful planning to minimize the negative implications.
CONCLUSION
Various healthcare systems have been forced to postpone treatment for many urological conditions as resources are dedicated to the treatment of COVID-19. Training has been postponed as staff are reallocated to areas of need. Face-to-face contact is largely minimized and innovative, virtual communication methods are used in the outpatient setting and multidisciplinary team meetings. Surgical practice is changing because of the risks posed by COVID-19 and procedures can be prioritized in a nonurgent, low priority, high priority or emergency category. Although the COVID-19 pandemic will inevitably affect urological services, steps can be taken to mitigate the impact and prioritize the patients most in need of urgent care.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus [Internet]. World Health Organization; 2020. [cited 2020 April 7]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rajgor D, Lee M, Archuleta S, et al. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis 2020; doi: 10.1016/S1473-3099(20)30244-9. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Infection prevention and control during health- care when novel coronavirus (nCoV) infection is suspected [Internet]. World Health Organization; 2020 March 19 [cited April 5, 2020]. 5 p. Available from: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125.
- 6.BMJ Best Practice. Coronavirus disease 2019 (COVID-19): symptoms, diagnosis and treatment [Internet]. BMJ Best Practice; 2020 April [cited 2020 April 5]. 132 p. Available from: https://bestpractice.bmj.com/topics/en-gb/3000168/treatment-algorithm#patientGroup-0-0.
- 7▪.Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol 2020; doi:10.23736/S0393-2249.20.03846-1. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]; Italy was the first European country to be severely affected by COVID-19 and this article discusses the way in which their urological practice has changed and recommendations to minimize future disruption.
- 8▪.Chan M, Yeo S, Chong Y, Lee Y. Stepping forward: urologists’ efforts during the COVID-19 outbreak in Singapore. Eur Urol 2020; 10.1016/j.eururo.2020.03.004 10.1016/j.eururo.2020.03.004. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; Singapore was one of the first countries outside of China to be affected by COVID-19 and they discuss the change role of the urologist and implications on training in the pandemic.
- 9▪.Stensland KD, Morgan TM, Moinzadeh A, et al. Considerations in the triage of urologic surgeries during the COVID-19 pandemic [Internet]. Eur Urol 2020; Available from: https://els-jbs-prod-cdn.literatumonline.com/pb/assets/raw/Health%20Advance/journals/eururo/EURUROL-D-20-00380-1584548684213.pdf [cited April 7, 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article summarizes the prioritization of urological procedures, considering the long-term effects of delaying treatment.
- 10.Liu J, Ouyang L, Guo P, et al. Epidemiological, clinical characteristics and outcome of medical staff infected with COVID-19 in Wuhan, China: a retrospective case series analysis. medRxiv 2020. [Google Scholar]
- 11.El-Faqih SR, Shamsuddin AB, Chakrabarti A, et al. Polyurethane internal ureteral stents in treatment of stone patients: Morbidity related to indwelling times. J Urol 1991; 146:1487–1491. [DOI] [PubMed] [Google Scholar]
- 12.Adanur S, Ozkaya F. Challenges in treatment and diagnosis of forgotten/encrusted double-J ureteral stents: the largest single-center experience. Renal Fail 2016; 38:920–926. [DOI] [PubMed] [Google Scholar]
- 13.Junuzovic D, Prstojevic J, Hasanbegovic M, Lepara Z. Evaluation of extracorporeal shock wave lithotripsy (ESWL): efficacy in treatment of urinary system stones. Acta Inform Med 2014; 22:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliver R, Wells H, Traxer O, et al. Ureteric stents on extraction strings: a systematic review of literature. Urolithiasis 2016; 46:129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.OPTN. Organ Procurement and Transplantation Network [Internet]. Human Resources and Services Administration; 2020 [updated 2020 March 4; cited 2020 April 5]. Available from: https://optn.transplant.hrsa.gov/.
- 16.Henry B, Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol 2020; doi: 10.1007/s11255-020-02451-9. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao Y, Qian K, Luo Y, et al. SARS-CoV-2 infection in renal failure patients: a potential covert source of infection. Eur Urol. 2020. doi: 10.1016/j.eururo.2020.03.025 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 18.Hardinger K, Brennan D, Klein C. Selection of induction therapy in kidney transplantation. Transplant Int 2012; 26:662–672. [DOI] [PubMed] [Google Scholar]
- 19.Zhu L, Gong N, Liu B, et al Coronavirus disease 2019 pneumonia in immunosuppressed renal transplant recipients: a summary of 10 confirmed cases in Wuhan, China. Eur Urol; 2020. doi: 10.1016/j.eururo.2020.03.039 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 20.Freitas F, Lombardi F, Pacheco E, et al. Clinical features of kidney transplant recipients admitted to the intensive care unit. Progr Transplant 2017; 28:56–62. [DOI] [PubMed] [Google Scholar]
- 21.Menon V, Sheridan W. Benign scrotal pathology: should all patients undergo surgery? BJU Int 2001; 88:251–254. [DOI] [PubMed] [Google Scholar]
- 22.Lam JS, Leppert JT, Figlin RA, et al. Surveillance following radical or partial nephrectomy for renal cell carcinoma. Curr Urol Rep 2005; 6:7–18. [DOI] [PubMed] [Google Scholar]
- 23.Tan W, Trinh Q, Hayn M, et al. Delayed nephrectomy has comparable long-term overall survival to immediate nephrectomy for CT1A renal cell carcinoma: a retrospective cohort study. Urol Oncol-Semin Ori 2019; 38:74. [DOI] [PubMed] [Google Scholar]
- 24.Tang Q, Song Y, Li X, et al. Prognostic outcomes and risk factors for patients with renal cell carcinoma and venous tumor thrombus after radical nephrectomy and thrombectomy: the prognostic significance of venous tumor thrombus level. BioMed Res Int 2015; 2015:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gadzinski AJ, Roberts WW, Faerber GJ, et al. Long term outcomes of immediate versus delayed nephroureterectomy for upper tract urothelial carcinoma. J Endourol 2012; 26:566–573. [DOI] [PubMed] [Google Scholar]
- 26.Nison L, Rouprêt M, Bozzini G, et al. The oncologic impact of a delay between diagnosis and radical nephroureterectomy due to diagnostic ureteroscopy in upper urinary tract urothelial carcinomas: results from a large collaborative database. World J Urol 2013; 31:69–76. [DOI] [PubMed] [Google Scholar]
- 27.Waldert M, Karakiewicz PI, Raman JD, et al. A delay in radical nephroureterectomy can lead to upstaging. BJU Int 2010; 105:812–817. [DOI] [PubMed] [Google Scholar]
- 28.Nepple K, O’Donnell M. The optimal management of T1 high-grade bladder cancer. Can Urol Assoc J 2013; 3 (6-S4):188. [PMC free article] [PubMed] [Google Scholar]
- 29.Ark J, Keegan K, Barocas D, et al. Incidence and predictors of understaging in patients with clinical T1 urothelial carcinoma undergoing radical cystectomy. BJU Int 2014; 113:894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chu A, Holt S, Wright J, et al. Delays in radical cystectomy for muscle-invasive bladder cancer. Cancer 2019; 125:2011–2017. [DOI] [PubMed] [Google Scholar]
- 31.Boeri L, Soligo M, Frank I, et al. Delaying radical cystectomy after neoadjuvant chemotherapy for muscle-invasive bladder cancer is associated with adverse survival outcomes. Eur Urol Oncol 2019; 2:390–396. [DOI] [PubMed] [Google Scholar]
- 32.Dunkman W, Manning M, Whittle J, et al. Impact of an enhanced recovery pathway on length of stay and complications in elective radical cystectomy: a before and after cohort study. Perioper Med 2019; 8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brassetti A, Möller A, Laurin O, et al. Evolution of cystectomy care over an 11-year period in a high-volume tertiary referral centre. BJU Int 2018; 121:752–757. [DOI] [PubMed] [Google Scholar]
- 34.Fossati N, Rossi M, Cucchiara V, et al. Evaluating the effect of time from prostate cancer diagnosis to radical prostatectomy on cancer control: Can surgery be postponed safely? Urol Oncol: Semin Orig Investig 2017; 35:150.e9–150.e15. [DOI] [PubMed] [Google Scholar]
- 35.Boorjian S, Bianco F, Scardino P, Eastham J. Urological oncology: does the time from biopsy to surgery affect biochemical recurrence after radical prostatectomy? BJU Int 2005; 96:773–776. [DOI] [PubMed] [Google Scholar]
- 36.Wang Z, Ni Y, Chen J, et al. The efficacy and safety of radical prostatectomy and radiotherapy in high-risk prostate cancer: a systematic review and meta-analysis. World J Surg Oncol 2020; 18:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Naspro R, Da Pozzo L. Urology in the time of corona. Nat Rev Urol 2020; 17:251–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020; doi:10.1001/jama.2020.3786. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Neal R, Tharmanathan P, France B, et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer 2015; 112 (S1):S92–S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wishnow K, Johnson D, Preston W, et al. Prompt orchiectomy reduces morbidity and mortal from testicular carcinoma. Br J Urol 1990; 65:629–633. [DOI] [PubMed] [Google Scholar]
- 41.Reddy BV, Sivakanth A, Naveen Babu G, et al. Role of chemotherapy prior to orchiectomy in metastatic testicular cancer-is testis really a sanctuary site? Ecancermedicalscience 2014; 8:407.doi:10.3332/ecancer.2014.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vetterlein M, Seisen T, Löppenberg B, et al. Resident involvement in radical inguinal orchiectomy for testicular cancer does not adversely impact perioperative outcomes: a retrospective study. Urol Int 2016; 98:472–477. [DOI] [PubMed] [Google Scholar]
- 43.Fukushima H, Kobayashi M, Kawano K, Morimoto S. Performance of quick sequential (sepsis related) and sequential (sepsis related) organ failure assessment to predict mortality in patients with acute pyelonephritis associated with upper urinary tract calculi. J Urol 2018; 199:1526–1533. [DOI] [PubMed] [Google Scholar]
- 44.Bayne D, Taylor E, Hampson L, et al. Determinants of nephrostomy tube dislodgment after percutaneous nephrolithotomy. J Endourol 2015; 29:289–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nourparvar P, Leung A, Shrewsberry A, et al. Safety and efficacy of ureteral stent placement at the bedside using local anesthesia. J Urol 2016; 195:1886–1890. [DOI] [PubMed] [Google Scholar]
- 46.Updated intercollegiate general surgery guidance on COVID-19 [Internet]. R Coll Surg; 2020 [cited 2020 May 5]. 3 p. Available from: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/
- 47.Pryor A. SAGES and EAES recommendations regarding surgical response to COVID-19 crisis [Internet]. Soc Am Gastrointest Endosc Surg; 2020 [cited 2020 May 5]. Available from: https://www.sages.org/recommendations-surgical-response-covid-19/.
- 48.Hollander J, Carr B. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 49.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020; 6:e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rimmer A. Trainees and Covid-19: your questions answered. BMJ 2020; 368:m1059. [DOI] [PubMed] [Google Scholar]
- 51.Sarmah P, Voss J, Ho A, et al. Low vs high fidelity: the importance of ‘realism’ in the simulation of a stone procedure. Curr Op Urol 2017; 27:316–322. [DOI] [PubMed] [Google Scholar]
- 52.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among healthcare workers exposed to coronavirus disease. JAMA Network Open 2020; 3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]


