Highlights
-
•
Globally, there was a significant correlation between healthy life expectancy (HALE), non-communicable disease DALYs and mortality, with COVID-19 caseload and deaths.
-
•
There was a positive independent association between HALE and COVID-19 cases.
-
•
The number of tourists was also associated with COVID-19 mortality.
-
•
Our integrated model of global data is valuable for health policymakers, allowing for the implementation of optimal preventative measures at national and global scales.
Key Words: Coronavirus, Stroke, Prevention, Correlation, Mortality, Incidence
Abstract
Background
The interaction between coronavirus disease 2019 (COVID-19) and non-communicable diseases may increase the global burden of disease. We assessed the association of COVID-19 with ageing and non-communicable diseases.
Methods
We extracted data regarding non-communicable disease, particularly cardiovascular disease, deaths, disability-adjusted life years (DALYs), and healthy life expectancy (HALE) from the Global Burden of Disease Study (GBD) 2017. We obtained data of confirmed COVID-19 cases, deaths, and tests from the Our World in Data database as of May 28, 2020. Potential confounders of pandemic outcomes analyzed include institutional lockdown delay, hemispheric geographical location, and number of tourists. We compared all countries according to GBD classification and World Bank income level. We assessed the correlation between independent variables associated with COVID-19 caseload and mortality using Spearman's rank correlation and adjusted mixed model analysis.
Findings
High-income had the highest, and the Southeast Asia, East Asia, and Oceania region had the least cases per million population (3050.60 vs. 63.86). Sub-saharan region has reported the lowest number of COVID-19 mortality (1.9). Median delay to lockdown initiation varied from one day following the first case in Latin America and Caribbean region, to 34 days in Southeast Asia, East Asia, and Oceania. Globally, non-communicable disease DALYs were correlated with COVID-19 cases (r = 0.32, p<0.001) and deaths (r = 0.37, p<0.001). HALE correlated with COVID-19 cases (r = 0.63, p<0.001) and deaths (r = 0.61, p<0.001). HALE was independently associated with COVID-19 case rate and the number of tourists was associated with COVID-19 mortality in the adjusted model.
Interpretation
Preventive measures against COVID-19 should protect the public from the dual burden of communicable and non-communicable diseases, particularly in the elderly. In addition to active COVID-19 surveillance, policymakers should utilize this evidence as a guide for prevention and coordination of health services. This model is timely, as many countries have begun to reduce social isolation.
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a major global crisis.2 , 3 On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic,4 and it has become one of the deadliest pandemics in the last century.5 The burden of COVID-19 extends far beyond that of a contagious disease. COVID-19 affects the entire health system through its direct effect as a communicable disease, as well as its ability to alter the overall mortality and burden of disease through impact on non-communicable diseases.
Globally, non-communicable diseases, including cardiovascular disease, accounted for greater than 70% of all deaths in 2017.6 There is mounting evidence that COVID-19 and non-communicable diseases may be associated on multiple levels, resulting in potentially unexpected effects on health outcomes. On one hand, COVID-19 is associated with cardiovascular diseases, such as acute cardiac injury (e.g. myocarditis), stroke, and exacerbation of subclinical vascular pathology.7, 8, 9 On the other hand, due to worldwide population ageing, many individuals may have multiple chronic medical conditions which can negatively impact the outcome of COVID-19 infection.10 A combination of frailty, ageing, and vascular comorbidities, together with COVID-19, represents a scenario that can exponentially increase hospitalization, intensive care unit admission, and hospital readmissions. This may explain the increased death rates in some countries, particularly among vulnerable patients with non-communicable diseases.11
Governments are urgently attempting to implement national policies and institute an efficient response to the COVID-19 pandemic.12 There are several important public health concerns that need to be addressed at this crucial stage of the pandemic, including the importance of active surveillance, border control, the possible role of tourists, and identification of those at risk. Therefore, collection of accurate and comprehensive global data regarding COVID-19, along with other major causes of disease burden, should be a public health priority. The current study aims to assess the association between the COVID-19 pandemic with the burden of non-communicable diseases and the ageing population worldwide.
Methods
Definitions and classifications
Using the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017, we reported national and regional healthy life expectancy (HALE) and life expectancy (in years). We also obtained data regarding death and disability-adjusted life years (DALYs) per 100000 related to non-communicable diseases, particularly cardiovascular diseases (ischemic heart disease, hypertensive heart disease, and stroke).13
We used the following categories for reporting the results: a) GBD super regions,14 consisting of 1) South Asia (6 countries), 2) Southeast Asia, East Asia & Oceania (23 countries), 3) Central Europe, Eastern Europe & Central Asia (29 countries), 4) North Africa & Middle East (19 countries), 5) Sub-Saharan Africa (56 countries), 6) Latin America & Caribbean (29 countries), and 7) high-income (33 countries); b) World Bank income levels,15 classified as 1) low-income (31 countries), 2) lower middle-income (52 countries), 3) upper middle-income (54 countries), and 4) high-income countries (58 countries);16 and c) hemispheric location including equatorial countries, and northern and southern hemispheres.17 GBD super region classification provides the opportunity to compare major health conditions at the global level. The combination of GBD super regions along with the World Bank classifications provides a suitable model for an ecological study comparing the state of various countries.
Data sources
We used data from the GBD 2017 study, coordinated by the Institute for Health Metrics and Evaluation.13 We used data regarding the number of COVID-19 tests, confirmed cases, and deaths, as well as populations in 2020 from the Our World in Data database.18 The data sources for Our World in Data consist of official websites of ministries of health or other government institutions, and government authorities’ social media accounts.18 We acquired data regarding the date of the first COVID-19 confirmed case in each country from the European Centre for Disease Prevention and Control database.19 We retrieved data regarding national lockdowns from the United Nations Educational, Scientific and Cultural Organization (UNESCO)-COVID-19 Educational Disruption and Response.20 We obtained data regarding total tourist numbers by country from the World Bank database.21
Data analysis
We calculated COVID-19 confirmed cases, deaths, and tests per million population (total number divided by each respective region's population) and 95% confidence intervals (CIs). Using the GBD 2017 database, we reported national and regional rates of non-communicable disease, including cardiovascular disease, mortality and DALYs per 100000 population with their 95% uncertainty intervals (UIs). Also, we reported years of HALE and life expectancy with their 95% UIs. The number of days before instituting lockdowns was calculated as the date of lockdown initiation minus the date of the first COVID-19 confirmed case in each country. We used Kruskal Wallis test to compare days before instituting lockdowns between regions. We used Spearman's rank correlation coefficient (Bonferroni correction) to analyze the association of COVID-19 cases and deaths with 1) non-communicable/cardiovascular disease DALYs, 2) life expectancy, and 3) HALE. We used a mixed model analysis to assess the association of the independent variables with COVID-19 caseload and mortality. We used Z-transform for all variables prior to entering them into the model. We entered the following variables into the fixed effect model: 1) non-communicable/cardiovascular disease DALYs, 2) HALE, 3) delay in national lockdown, 4) tourist number per country in 2018, and 5) hemispheric location. We entered GBD super regions into the random effect model. STATA software (version 13) was used for all statistical analysis. We used adobe Photoshop, Microsoft Excel (2016) and Prism to draw figures. All data used in the study are publicly available in an anonymized format.
Results
General information
Supplemental Table 1S summarizes results of the variables used in this study. We reported the following data: 1) COVID-19 cases (211 countries), deaths (211 countries), and performed tests (84 countries) (Supplemental Table 2S), 2) non-communicable/cardiovascular disease DALYs and deaths (195 countries; Supplemental Table 3S), 3) Population, HALE and life expectancy (195 countries; Supplemental Table 4S), 4) dates of first confirmed cases (211 countries) and dates of national and local lockdown initiation (210 countries; Supplemental Table 5S), and 5) tourist number (210 countries; Supplemental Table 5S).
COVID-19 cases and deaths
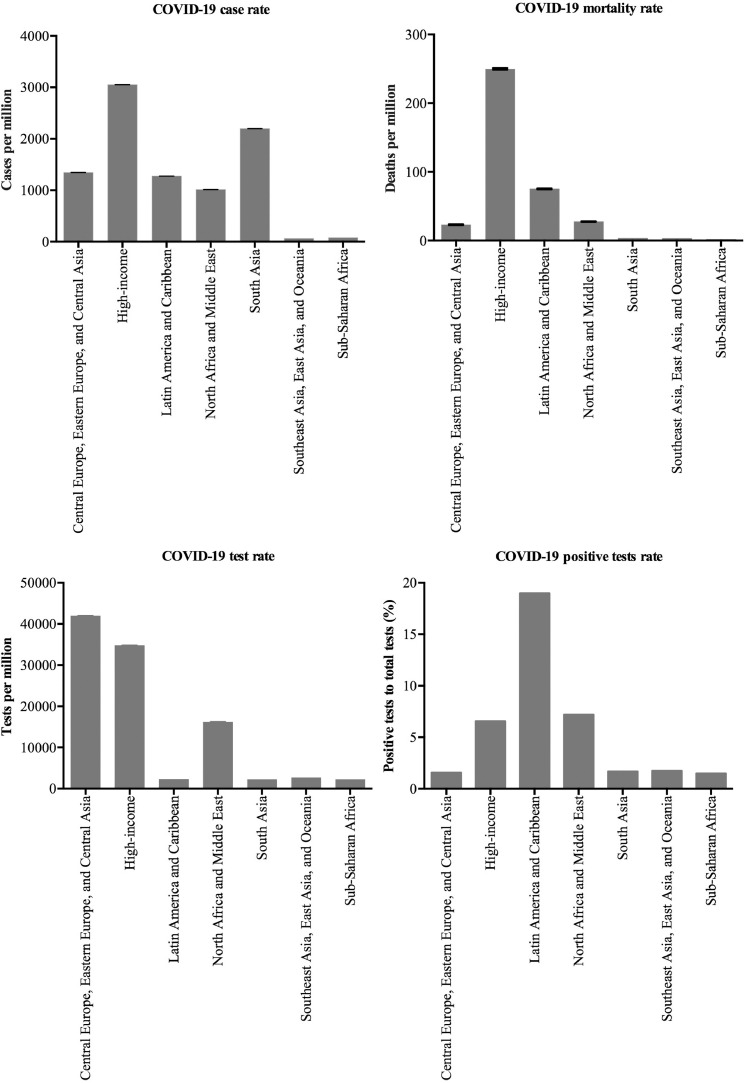
As of May 28, 2020, the highest number of COVID-19 cases were reported in the high-income region (3050.60), followed by Central Europe, Eastern Europe, and Central Asia region (1343.95), Latin America and Caribbean region (1276.58), and North Africa and Middle East (1014.67). Likewise, high-income countries according to World Bank classification, have higher rates of COVID-19 cases (2962.47) and deaths (228.79) compared to low-income countries (cases: 53.17; deaths: 1.23).
Using Our World in Data, we have access to test reports in 84 countries, particularly high-income countries (40 out of 58 high-income countries (69%) vs. 6 out of 31 (19.4%) low-income countries). Additionally, high-income countries had performed substantially more tests per million population in comparison to other countries. Finally, the Latin America and Caribbean region had the highest ratio of confirmed cases to tests performed (18.98%), followed by the North Africa and Middle East region (7.2%). This ratio was also higher in high-income countries according to the World Bank classification as compared to other categories (Figure 1 and Supplemental Table 1S).
Fig. 1.
COVID-19 pandemic: A comparison of (A) confirmed cases, (B) deaths, (C) tests, and (D) positive test rates as of May 28, 2020 according to the seven GBD super regions.
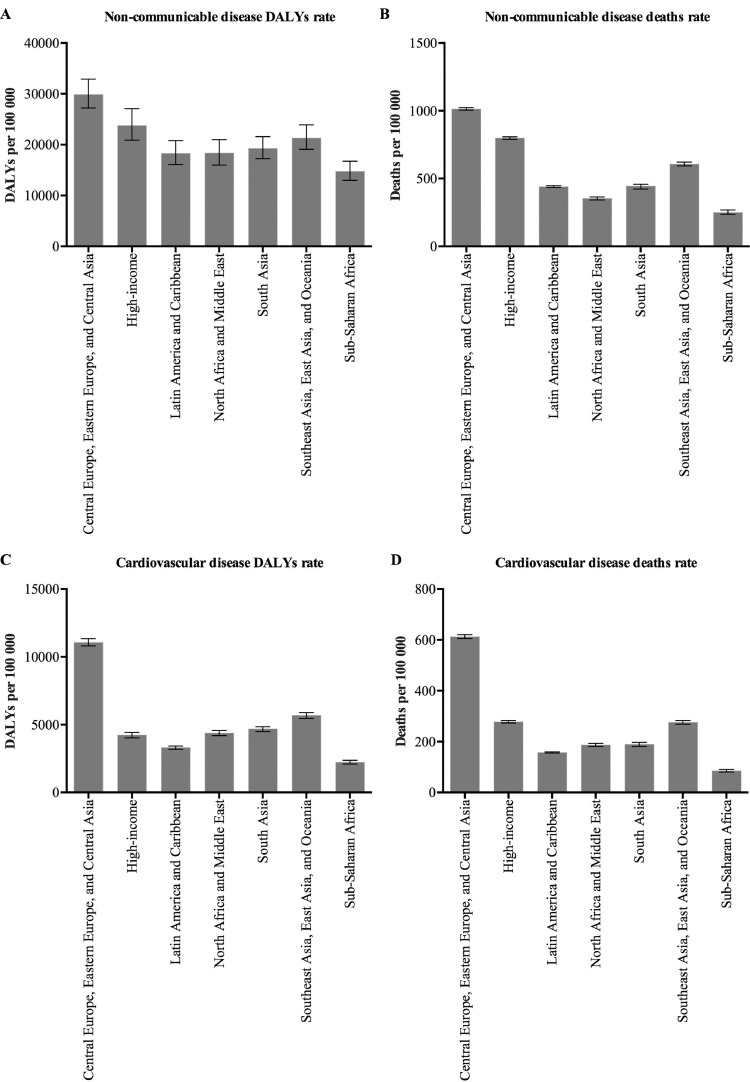
Burden and mortality of non-communicable diseases
In 2017, non-communicable diseases constituted 73% and 62% of all-cause death and DALYs, respectively. Among these, cardiovascular diseases constituted 32% and 15% of all-cause death and DALYs, respectively. The greatest number of non-communicable disease DALYs was observed in Central Europe, Eastern Europe, and Central Asia (29870.3), followed by the high-income region (23778.2; Figure 2 ). A similar pattern was seen for deaths related to non-communicable diseases. Using the World Bank classification, we found higher non-communicable disease DALYs and deaths in high-income countries compared to low- and middle-income countries (Supplementary Tables 1S and 3S).
Fig. 2.
Global burden of (A and B) non-communicable diseases and (C and D) cardiovascular diseases: Results from the GBD 2017 study.
Life expectancy and HALE
High-income countries had approximately 15 more years of life expectancy in 2017 compared to low-income countries. In 2017, the South Asia region had the lowest life expectancy (69.03 years, UI: 68.56 to 69.48) and the high-income region had the highest (81.02 years, UI: 80.88 to 81.16). Likewise, HALE (2017) in high-income countries was higher than low-income countries (69.4 [66.15 to 72.18] vs. 55.66 [53.17 to 57.97]). Among the GBD super regions, HALE ranged from 55.20 (52.68 to 57.58) years in Sub-Saharan Africa to 69.59 (66.35 to 72.36) years in the high-income region (Supplemental Tables 1S and 4S).
Lockdown date
Median (IQR) delay to lockdown initiation varied in different regions, ranging from one day (0 to 10) after the first local confirmed case in Latin America and Caribbean, to 34 days (2 to 52) in Southeast Asia, East Asia, and Oceania (p<0.001). The GBD high-income region instituted their first lockdowns at a median of 19 days (13 to 44) after their first respective cases. Based on the World Bank classification, high-income countries initiated their lockdown 14 days (7.5 to 31.5) later than low-income countries (one day, -1 to 8 days, p<0.001) (Supplemental Table 1S and 5S).
Tourist number
We did not have data on the number of tourist arrivals since the beginning of the pandemic. 2018 data shows the number of tourists (millions) that visited each country: high-income (866.65), upper middle-income (386.7), lower middle-income (152.82), and low-income (29.53) (Supplemental Table 1S and 5S).
Correlation between COVID-19 and non-communicable diseases
Life expectancy (r = 0.65, p<0.001), HALE (r = 0.63, p<0.001), non-communicable disease DALYs (r = 0.32, p<0.001) and ischemic heart disease (r = 0.25, p = 0.01) had a significant correlation with COVID-19 cases. We found a correlation between life expectancy (r = 0.63, p<0.001), HALE (r = 0.61, p<0.001), non-communicable disease DALYs (r = 0.37, p<0.001), ischemic heart disease (r = 0.28, p = 0.002), and ischemic stroke (r = 0.25, p = 0.01) with COVID-19 deaths. We did not find such correlations for total stroke (r = -0.008, p=0.9), cardiovascular disease (r = 0.19, p = 0.2), and hypertensive heart disease (r = -0.06, p = 0.9).
Independent factors associated with COVID-19
In the mixed model analysis of GBD-classified countries, we observed a positive association between HALE (0.49, CI: 0.22 to 0.75) and the number of COVID-19 cases. Among other variables, we only found a positive association between tourist numbers and mortality (0.40, CI: 0.21 to 0.60) (Table 1 A). Hemispheric location did not have a statistically significant correlation with COVID-19 caseload or death. After adjusting for fixed effect variables, there was variability in the number of COVID-19 cases and deaths among super regions.
Table 1.
Variables associated with the COVID-19 pandemic: Results from a mixed model analysis
| COVID-19 cases Estimate (95% CI) |
COVID-19 deaths Estimate (95% CI) |
||
|---|---|---|---|
| GBD super regions classification | |||
| Fixed effect variables | Delay in lockdown (days) | -0.06 (-0.26–0.14) | -0.04 (-0.24–0.14) |
| Healthy life expectancy | 0.49 (0.22–0.75) | 0.15 (-0.10–0.41) | |
| Non-communicable disease DALY | -0.19 (-0.39–0.01) | 0.07 (-0.12–0.28) | |
| Tourist (number per year) | 0.01 (-0.19–0.21) | 0.40 (0.21–0.60) | |
| Geographical locations* | |||
| Equatorial | 0.26 (-0.49–1.02) | 0.36 (-0.35–1.08) | |
| Southern hemisphere | -0.02 (-0.53–0.48) | -0.15 (-0.63–0.32) | |
| Random effect variable | GBD super regions† | 0.94 (0.83–1.06) | 0.89 (0.78–1.01) |
Abbreviations: COVID-19, coronavirus disease 2019; DALY, disability-adjusted life year.
Northern hemisphere considered as a reference category.
GBD super regions: 1) South Asia, 2) Southeast Asia, East Asia & Oceania, 3) Central Europe, Eastern Europe & Central Asia, 4) North Africa & Middle East, 5) Sub-Saharan Africa, 6) Latin America & Caribbean, and 7) high-income.
Note: Data was available in 135 countries.
Discussion
The current study has major public health implications with novel findings regarding the associations between COVID-19 and populations at risk, including the elderly and those with non-communicable diseases. These relationships are more evident in high-income countries, where we found the highest rate of COVID-19 cases and deaths per million when compared to other countries. This could be explained, at least partially, by the greater number of COVID-19 tests, active surveillance models, and ageing populations. Although non-communicable/cardiovascular disease DALYs were not independently associated with COVID-19 cases and deaths, the higher prevalence of non-communicable diseases among the elderly may play a major role in the burden of COVID-19.
COVID-19 is a worldwide health crisis with drastic social, economic, and health consequences. In order to fight against the COVID-19 pandemic, health policymakers require accurate and comprehensive relevant health data. In the current study, we summarized data regarding COVID-19 cases and deaths in 185 countries. High-income countries have the greatest number of COVID-19 cases and deaths. We found a correlation between baseline non-communicable diseases and COVID-19 cases. National and regional burden of all non-communicable diseases, ischemic heart disease, and ischemic stroke had a significant correlation with COVID-19 deaths. Although we did not find an independent association between non-communicable/cardiovascular disease DALYs and COVID-19 cases and deaths, there was a significant association between life expectancy and COVID-19 cases. Life expectancy and HALE in high-income countries are higher than in other countries, and this improved longevity is associated with a higher prevalence of non-communicable disease.1 These findings may explain the increased rates of COVID-19 cases and deaths in high-income countries, where a considerable portion of the community consists of older adults with baseline non-communicable diseases, including cardiovascular diseases. Many COVID-19-related deaths in high-income countries are older individuals and residents of long-term care facilities,22, 23, 24 where a considerable number of people may have concurrent non-communicable diseases. In addition, the difference in affordability and access to long-term care in high-income countries compared to other regions may explain some of the differences between cases and COVID-19-related deaths among high-income countries versus low- and middle-income countries.25 Although the number of COVID-19 cases and deaths is lower in low- and middle-income countries compared to high-income countries, we may observe a potential shift towards a higher mortality rate in low- and middle-income countries due to poorer control of non-communicable diseases, despite the corresponding younger demographic structure.26 This is particularly important after the recent exponential growth in the number of cases in Brazil27 and changes in Africa.28
Elderly individuals, particularly those residing in long-term care, may suffer from frailty syndrome, resulting in a reduced capacity to respond to acute physiological stressors, such as SARS-CoV-2 infection. In this regard, it appears as though many countries have not adequately prepared to prevent communicable diseases of this magnitude. In addition, an increase in the total mortality rate of some countries during the pandemic as compared to the previous years may be due to changes in health care delivery for vulnerable citizens. Between March 13 and April 17 2020, England and Wales reported an additional 11334 deaths compared to their five year average. COVID-19 accounted for 8753 of these deaths.29 Many countries have detrimentally altered the delivery of healthcare to patients suffering from non-communicable diseases during the pandemic, thus it is possible that a significant portion of non-diagnosed COVID-19 additional deaths are due to patients’ lack of control of non-communicable diseases.11 , 30
While differences pertaining to COVID-19 cases and mortality between countries (e.g. low- and middle-income countries versus high-income countries) can be attributed to lower life expectancy in low- and middle-income countries, other factors such as time of initiation of lockdowns, testing per population, active surveillance, and border control may also play a significant role in the discrepancy of COVID-19 cases and deaths in different countries. The COVID-19 pandemic has prompted numerous countries to implement nation-wide lockdowns in order to mitigate the spread of the virus. One possible reason for a higher rate of COVID-19 death in high-income countries may be a delay in the time of lockdown. However, we did not find an independent association between the time of lockdown and the number of COVID-19 cases and deaths. From a public health perspective, it is crucial to implement active surveillance for new cases and enhanced techniques for contact tracing. Successful models have been reported in some South Asian countries.31, 32, 33, 34, 35 This is particularly important in enclosed settings, such as long-term care and cruise ships, where it is crucial to actively monitor for the initial source of the infection, as well as identify potentially infected staff, guests, visitors, and residents.22 We also observed a strong association between the number of tourists and COVID-19 mortality, emphasizing the importance of border control between, and probably within, countries during the COVID-19 pandemic.
During the current pandemic, one of the most important public health and government concerns is when to cease national quarantines. While many countries may change their national isolation policies because of economic factors, at this crucial stage of the COVID-19 pandemic, the convergence of COVID-19 with non-communicable diseases, particularly among the elderly, has yet to be addressed from a public health perspective. Mounting evidence suggests that infectious diseases are prognostic determinants for non-communicable diseases.36 Such associations between non-communicable and communicable diseases emphasize the importance of a comprehensive strategy for integrating infection and non-communicable diseases. Specifically, many outpatient clinics have stopped working, and vulnerable patient populations may have reduced access to their previously established preventive measures. In addition, many patients are reluctant to seek medical care due to fear of exposure to the SARS-CoV-2 virus. The public should be informed that hospitals remain the best place for acute care. Hospital administrators should also ensure patient safety through appropriate preventive measures. For example, many important aspects of patient care, ranging from emergency medical services dispatch to decisions regarding acute vascular interventional therapies, can be performed via telemedicine.37 Early supported discharge services38 should be organized for patients suffering from cardiovascular diseases with or without confirmed COVID-19. In addition, online 24/7 outpatient support with secure cross-platform applications may help fill the gap left by the reduction in traditional face-to-face visits for chronic diseases that require regular follow-up.
Our study has some limitations. We found significant variations between the rates of confirmed cases per number of performed tests in different regions. Differences in the number of COVID-19 cases and deaths in low- and middle-income countries may be related to reduced testing and active screening of suspected cases, affecting the accuracy of reports. Many countries have not reported the number of tests performed; therefore, we do not have access to official reports of COVID-19 testing in several countries. Additionally, we were unable to assess the quality and sensitivity of tests in different countries. Moreover, it is possible that many cases and deaths related to COVID-19 in low- and middle-income countries have been followed only in the community, without hospitalizations. This may affect the total number of both confirmed cases and deaths in these countries. In the current study, we entered GBD super regions as a categorical variable in the mixed effect model. This classification will enable us to compare countries and regions according to their geographic closeness to capture important public health confounders. Although we entered some of the important confounders that may be associated with COVID-19 into our statistical model; e.g. lockdown time, burden of non-communicable disease, geographical locations, HALE (as a snapshot of global health and age), and tourist number (as a marker of international visitors), we were not able to capture many other confounders, such as national and religious ceremonies (e.g. new year celebrations, sport championships, etc) even when using the GBD super region classification. This may explain the instability of our adjusted model with a large variability in confirmed COVID-19 cases and deaths in the mixed effect analysis. In addition, COVID-19 has a dynamic exponential pattern which may affect the results of any adjusted analytic model. As COVID-19 figures are moving targets, and different countries are achieving peak infection at different times, it is likely that some countries still did not reach their peak at the time of analysis. In addition, there is a possibility for a second peak in many countries after reopening business. This would underestimate the correlation between COVID-19 and NCD figures in some countries and regions. Therefore, the results of the adjusted model should be interpreted cautiously. In addition, we used group data in this study which is a subject of ecological fallacy and cannot be interfered with at an individual-based level.39 Nevertheless, the major strength of our study is the reliance on available worldwide data, which provides the opportunity to investigate overlaps of non-communicable diseases and population ageing with COVID-19 on a global scale.
Conclusions
The underlying message of our study is the need for an evidence-based approach to the convergence of the ageing population, non-communicable diseases, and COVID-19. This would facilitate a strategy to develop public health policies and plans for effective risk assessment, surveillance, patient follow-up, health promotion, and prevention, that can protect the population from the dual burden of communicable and non-communicable diseases. The results can subsequently be employed as a reference for public health officials regarding the healthcare system's capacity, and guide decisions during the current pandemic, as well as future global emergencies. Additionally, a model containing our results would allow for coordinated care towards individuals (particularly the elderly) enduring this multi-disease burden, as well as resource allocation towards populations with higher risk of morbidity and mortality. Researchers, health professionals, donor agencies, and politicians should not only focus on a particular health problem, but develop future programs against the aggregated burden of disease.
Acknowledgments
Acknowledgment
The authors have no conflict of interest to declare. We performed this study as a part of the CASCADE initiative. We would like to thank all authors and participant centers that have joined CASCADE shortly after the pandemic to provide global data regarding cerebrovascular and cardiovascular diseases and COVID-19. The current study could have not been done without their encouraging feedback.
Declaration of Competing Interest
Authors and investigators have no conflict of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jstrokecerebrovasdis.2020.105089.
Appendix. Supplementary materials
References
- 1.Monaco A, Palmer K, Marengoni A, Maggi S, Hassan TA, Donde S. Integrated care for the management of ageing-related non-communicable diseases: current gaps and future directions. Aging Clin Exp Res. 2020 doi: 10.1007/s40520-020-01533-z. published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48:155–163. doi: 10.1007/s15010-020-01401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He F, Deng Y, Li W. Coronavirus disease 2019: What we know? J Med Virol. 2020 doi: 10.1002/jmv.25766. published online March 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. WHO Director-general's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020; published online March 11. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed April 23, 2020).
- 5.WHO. WHO/Europe | Past pandemics. 2020. http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/pandemic-influenza/past-pandemics(accessed April 24, 2020).
- 6.Martinez R, Lloyd-Sherlock P, Soliz P. Trends in premature avertable mortality from non-communicable diseases for 195 countries and territories, 1990-2017: a population-based study. Lancet Glob Health. 2020;8:e511–e523. doi: 10.1016/S2214-109X(20)30035-8. [DOI] [PubMed] [Google Scholar]
- 7.Markus HS, Brainin M. COVID-19 and stroke-A global world stroke organization perspective. Int J Stroke. 2020 doi: 10.1177/1747493020923472. 1747493020923472. [DOI] [PubMed] [Google Scholar]
- 8.Aggarwal G, Lippi G, Michael Henry B. Cerebrovascular disease is associated with an increased disease severity in patients with coronavirus disease 2019 (COVID-19): a pooled analysis of published literature. Int J Stroke. 2020 doi: 10.1177/1747493020921664. 1747493020921664. [DOI] [PubMed] [Google Scholar]
- 9.Helms J, Kremer S, Merdji H. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Donovan MR, Sezgin D, Liew A, O'Caoimh R. Burden of disease, disability-adjusted life years and frailty prevalence. QJM. 2019;112:261–267. doi: 10.1093/qjmed/hcy291. [DOI] [PubMed] [Google Scholar]
- 11.Dyer O. Covid-19: Pandemic is having “severe” impact on non-communicable disease care, WHO survey finds. BMJ. 2020;369:m2210. doi: 10.1136/bmj.m2210. [DOI] [PubMed] [Google Scholar]
- 12.Pisano GP, Sadun R, Zanini M. Lessons from Italy's Response to Coronavirus. 2020; published online March 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus(accessed April 21, 2020).
- 13.Global Burden of Disease Collaborative Network . Institute for Health Metrics and Evaluation (IHME); Seattle, United States: 2018. Global Burden of Disease Study 2017 (GBD 2017) Results.http://ghdx.healthdata.org/gbd-results-tool (accessed May 19, 2019) [Google Scholar]
- 14.GBD 2016 Lifetime Risk of Stroke Collaborators. Feigin VL, Nguyen G. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379:2429–2437. doi: 10.1056/NEJMoa1804492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The World Bank Atlas method - detailed methodology – World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/378832-what-is-the-world-bank-atlas-method(accessed April 29, 2020).
- 16.World Bank Country and Lending Groups – World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups(accessed April 29, 2020).
- 17.Southern Hemisphere Countries 2020. https://worldpopulationreview.com/countries/southern-hemisphere-countries/(accessed May 6, 2020).
- 18.Coronavirus pandemic (COVID-19) - statistics and research - our world in data. https://ourworldindata.org/coronavirus(accessed June 9, 2020).
- 19.COVID-19. https://www.ecdc.europa.eu/en/covid-19-pandemic(accessed April 29, 2020).
- 20.UNESCO. COVID-19 impact on education. COVID-19 educational disruption and response. 2020; published online April 17. https://en.unesco.org/sites/default/files/covid_impact_education.csv(accessed April 22, 2020).
- 21.International tourism, number of arrivals | Data. https://data.worldbank.org/indicator/ST.INT.ARVL(accessed May 3, 2020).
- 22.McMichael TM, Currie DW, Clark S. Epidemiology of COVID-19 in a long-term care facility in King county, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arons MM, Hatfield KM, Reddy SC. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020 doi: 10.1056/NEJMoa2008457. published online April 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kimball A, Hatfield KM, Arons M. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - King County, Washington, march 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siegel EO, Backman A, Cai Y. Understanding contextual differences in residential LTC provision for cross-national research: identifying internationally relevant CDEs. Gerontol Geriatr Med. 2019;5 doi: 10.1177/2333721419840591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Checkley W, Ghannem H, Irazola V. Management of NCD in low- and middle-income countries. Glob Heart. 2014;9:431–443. doi: 10.1016/j.gheart.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crokidakis N. COVID-19 spreading in Rio de Janeiro, Brazil: Do the policies of social isolation really work? Chaos Solitons Fractals. 2020;136 doi: 10.1016/j.chaos.2020.109930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adegboye OA, Adekunle AI, Gayawan E. Early transmission dynamics of novel coronavirus (COVID-19) in Nigeria. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17093054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Appleby J. What is happening to non-covid deaths? BMJ. 2020;369:m1607. doi: 10.1136/bmj.m1607. [DOI] [PubMed] [Google Scholar]
- 30.Kluge HHP, Wickramasinghe K, Rippin HL. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020 doi: 10.1016/S0140-6736(20)31067-9. published online May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng H-Y, Li S-Y, Yang C-H. Initial rapid and proactive response for the COVID-19 outbreak - Taiwan's experience. J Formos Med Assoc. 2020;119:771–773. doi: 10.1016/j.jfma.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yen M-Y, Schwartz J, Chen S-Y, King C-C, Yang G-Y, Hsueh P-R. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: Implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.03.011. published online March 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.COVID-19 National Emergency Response Center, Epidemiology & Case Management Team, Korea Centers for Disease Control & Prevention Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect. 2020;11:60–63. doi: 10.24171/j.phrp.2020.11.1.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim YJ, Jeong YJ, Kim SH. Preparedness for COVID-19 infection prevention in Korea: Single-center experience. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.04.018. published online April 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.COVID-19 in Asia: a country-by-country guide – the diplomat. https://thediplomat.com/2020/04/covid-19-in-asia-a-country-by-country-guide/(accessed April 30, 2020).
- 36.Ogoina D, Onyemelukwe GC. The role of infections in the emergence of non-communicable diseases (NCDs): Compelling needs for novel strategies in the developing world. J Infect Public Health. 2009;2:14–29. doi: 10.1016/j.jiph.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corley J. Telestroke: India's solution to a public health-care crisis. Lancet Neurol. 2018;17:115–116. doi: 10.1016/S1474-4422(17)30423-4. [DOI] [PubMed] [Google Scholar]
- 38.Visvanathan V. Early supported discharge services for people with acute stroke: a Cochrane review summary. Int J Nurs Stud. 2019;94:186–187. doi: 10.1016/j.ijnurstu.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 39.Freedman DA. Ecological inference and the ecological fallacy. In: Colton D, editor. Surveys on Solution Methods for Inverse Problems. 1999. https://statistics.berkeley.edu/tech-reports/549 (accessed June 9, 2020) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.