Abstract
Objective
Explore the impact of the Great Recession on domestic violence (DV) related hospitalizations and emergency department (ED) visits in California.
Methods
Hospital and ED data were drawn from California's Office of Statewide Health Planning and Development (OSHPD). DV-related hospitalizations and ED visits in California were analyzed between January 2000 and September 2015 (53,596), along with total medical costs. Time series were divided into pre-recession (Jan 2000-Nov 2007) and recession/post-recession (Dec 2007-Sept 2015) periods.
Results
The medical cost of DV-related hospitalizations alone was estimated as $1,136,165,861. A dramatic increase in DV episodes was found potentially associated with the Great Recession. The number of ED visits per month tripled from pre- to post-recession (104.9 vs. 290.6), along with an increased number of hospitalizations (77.1 vs. 95.6); African Americans and Native Americans were disproportionally impacted. In addition, psychiatric comorbidities, severe DV episodes, in-hospital mortality and charge per hospitalization escalated. The rise in DV hospitalizations and ED visits beginning in December 2007 was mainly attributable to physical abuse episodes in adults; minors had no change in DV trends.
Discussion
Recessions are frequent in modern economies and are repeated cyclically. Our study provides critical information on the effects of the 2007 financial crisis on DV-related healthcare service utilization in California. Given the current financial crisis associated with COVID-19, which expert predict could extend for years, the results from this study shine a spotlight on the importance of DV-related screening, prevention and response.
Keywords: Domestic violence, Hospitalizations, Social determinants
Highlights
-
•
We corroborated a correlation between financial stress and DV-related events.
-
•
Number of DV episodes dramatically increased during the 2007 financial crisis.
-
•
African American and Native American persons were disproportionally impacted.
-
•
Co-existing psychiatric conditions and in-hospital mortality also increased.
-
•
In addition, charges per hospitalization escalated during the economic recession.
1. Background
Domestic violence (DV) is a national public health problem, affecting 10 million people in the U.S. annually (Huecker and Smock, 2019). The scope and effects of DV cross the lifespan. One in seven U.S. children suffers from child abuse and/or neglect annually (Finkelhor et al., 2009); one in four U.S. women will experience physical, sexual, and/or stalking violence by an intimate partner during their lifetime (Smith et al., 2018); and nearly one in ten older adults in the U.S. will experience abuse in domestic settings (Pillemer et al., 2016). The combined economic impact from healthcare costs and lost wages surpasses three trillion dollars in the U.S. (Peterson et al., 2018a; Peterson et al., 2018b)
DV is strongly associated with financial stress and financial dependence on family members (Pillemer et al., 2016; Renzetti, 2009; Schneider et al., 2016; Schneider et al., 2017; Berger et al., 2011). Moreover, the most vulnerable groups in society (non-white, low-income and low-educated) are disproportionally affected by DV (Office of Women's Health, 2012); for example, the 2007 Great Recession disproportionately impacted women and the most vulnerable populations in this manner (Margerison-Zilko et al., 2016). Moreover, many California families were adversely affected by the mortgage market crisis (the majority of subprime loans were issued in California) before the technical beginning of the 2007 Great Recession (Irons, 2009; DHUD, 2010); therefore, California residents were highly vulnerable to DV.
Recessions are frequent in modern economies and are cyclical. Repeated periods during which economic growth falls are called recessions and depressions, whether mild or more severe, respectively. One of the most well-known is the Great Depression, which occurred during the 1930s. The U.S. has experienced 11 recessions during the post-World War II era (including the recessions of 1949, 1953, 1958, 1960, 1969, 1973, 1980, 1981–1982, the early 1990s and 2000s recessions and the Great Recession in 2007), and the novel coronavirus (COVID-19) is leading to widespread financial crisis which experts predict could extend for years (Semuels, 2020; RT, 2020; Menickella, 2020). The Great Recession began with a crisis in the mortgage market during which remarkable increases in foreclosure numbers were reported beginning in the second quarter of 2006; California, Arizona, Nevada and Florida experienced the sharpest rise in foreclosures (DHUD, 2010). While the Great Recession officially lasted less than two years, from December 2007 to June 2009, during which the GDP contracted, the economic crisis produced long-lasting consequences for individuals as well as society as a whole (Irons, 2009).
Studies suggest that the scale and effects of DV worsen in children (Schneider et al., 2017; Berger et al., 2011) and adults (Renzetti, 2009; Schneider et al., 2016) during economic recessions, and yet, the impact of economic recessions on DV in the U.S. is poorly understood. The present study explores the extent to which the Great Recession impacted the number of reported DV hospitalizations and emergency department (ED) visits in California across various domains.
Victims of DV frequently interact with healthcare services (Huecker and Smock, 2019). Therefore, healthcare data is a unique resource that can be used to identify and study DV trends (Schafer et al., 2008). However, few studies on DV hospitalization trends and risks factors have been published, especially in relation to recessions. In the present paper, we describe the impact of the Great Recession on DV-related hospitalizations and ED visits in California from 2000 to 2015 (pre-recession through post-recession). Our study sample comprised 53,596 DV-related episodes, which encompassed intimate partner violence (IPV), as well as violence against elders and children. Data were drawn from California's Office of Statewide Health Planning and Development (OSHPD), which provides a large representative dataset that includes all DV-related hospitalizations and ED visits in California. DV-related hospitalizations and visits to EDs represent the most dramatic and severe violence episodes in domestic settings.
2. Methods
2.1. Data source
DV-related hospital and ED morbidity rates in California were examined. Data on service utilization were drawn from the OSHPD hospital dataset, a government-sponsored healthcare register that includes records from all licensed hospitals and EDs in California. The OSHPD data provides anonymized information from hospitals and EDs, including patient characteristics (residential ZIP code, sex, age, ethnicity/race), expenses and source of payment, principal diagnosis (the condition established to be the chief cause of the admission or ED encounter) and up to 24 coexisting diagnoses (comorbidities). Not all patients' comorbidities are coded; rather, only chief cause of service and contributing condition for the hospitalization or ED admission are reported. Therefore, co-existing conditions that did not contribute to the cause of the service are not included in the dataset. The International Classification of Diseases, 9th version (ICD9) was used to code service utilization between January 2000 and September 2015, while the ICD10 was used to code service utilization records between October 2015 and December 2017; the transition from ICD9 to ICD10 codes, which allows reporting for both suspected/confirmed cases, in October 1st, 2015, abruptly increased the number of reported DV episodes. Therefore, the ICD10 code period (October 2015 to December 2017) was excluded from analysis.
The term DV refers to physical, sexual and emotional/psychological violence in a domestic setting and includes a range of behaviors, from intimate partner violence (IPV) to violence against elders and children. The study sample comprised all records (53,596) for which DV-related codes (ICD9 codes 995.5, 995.8) were established as chief cause or contributing condition for hospitalizations and ED encounters from January 2000 to September 2015. ICD9 codes for DV defined in previous studies (Schafer et al., 2008; Rudman, 2000) include: Adult (ICD9 codes 995.80–995.85) and Child (ICD9 code 995.5) abuse/maltreatment. Sub-categories identify five types of abuse: emotional/psychological, sexual, physical abuse, neglected (nutritional) and other/unspecified abuse. E-Codes and Y07 codes, which identify who committed the act of violence, were not available in the dataset. V-Codes were not used to identify patients with a history of DV, as only episodes for on-going abuse were analyzed. For comparability, all hospital charge data were inflation-adjusted using the medical care consumer price index (Bureau of Labor Statistics, 2020) to 2015 dollars, representing the dollar value at the end of the study period.
2.2. Data analysis
Descriptive and time series analysis were conducted to analyze trends in DV episodes. Descriptive statistics for the analyzed sample (Table 1 ) were examined for the pre-recession period (January 2000 to November 2007) and the recession and post-recession period (December 2007 to September 2015). This was done to identify possible changes in DV-hospitalization characteristics in different time periods, including in-hospital mortality ratio, hospital charge, scope of injuries and co-existing conditions (including psychiatric conditions) associated with DV-related episodes. In addition, racial categories included in the OSHPD dataset were used to estimated age-adjusted rates for five races/ethnicities (White, Hispanic, African American, American Indian/Alaska Native, Asian and Native Hawaiian/other Pacific Islander), and the “2000 US standard population” was used for calculating age-adjusted rates (Klein and Schoenborn, 2001). Age-adjusted rates are rates we would have obtained if the study population had the same age distribution as the standard population. Age-adjusted rates are usually estimated when comparing populations with different age structures (for example, White and Hispanic populations) to eliminate differences in crude rates that result from differences in the populations' age distributions (Klein and Schoenborn, 2001). Time series analysis comprises methods to extract meaningful statistics of the data involving temporal measurements. A given time series consists of four systematic components including level (average value in the series), trend (long term direction), noise (unsystematic, short term fluctuations) and seasonality (systematic, calendar related movements). Noise and seasonality can obscure the impact of events and changes in level and temporal trend. Seasonal adjustment, usually done in trend analysis, is a statistical method for removing noise and the seasonal component of a time series from level and trend (Length, 2016; Shumway and Stoffer, 2010). Seasonally adjusted time series were estimated to identify changes in level or trend and analyze the number of DV hospitalizations and ED visits and the overall number of DV episodes as well as the overall number of DV episodes in minors and adults separately and by type of abuse (physical, sexual, emotional, neglect and unspecified). Differences in slope and mean values were assessed using t-ratio and t-test, respectively, to compare trends and level in time series. Microsoft Excel 2016 and R statistical software (“lsmeans”, and “zoo” R packages) (Length, 2016) were used to generate the graphs and conduct all analyses.
Table 1.
Descriptive statistics on domestic violence (DV) variables for two time periods: pre-recession (January 2000–November 2007), recession and post-recession (December 2007–September 2015).
| Pre-recession: Jan 2000 – Nov 2007 |
Recession and post-recession: Dec 2007–Sept 2015 |
||||
|---|---|---|---|---|---|
| Number (column %) | Number (column %) | Diff | |||
| Emergency department visits | Admissions per month | 104.9 | 290.6 | 185.7; p < 0.001 | |
| Abuse type | Physical | 5471 (54.9%) | 16,843 (61.7%) | 6.8%; p < 0.001 | |
| Emotional psychological | 99 (1%) | 562 (2.1%) | 1.1%; p < 0.001 | ||
| Neglect | 540 (5.4%) | 882 (3.2%) | −2.2%; p < 0.001 | ||
| Sexual | 2741 (27.5%) | 6499 (23.8%) | −3.7%; p < 0.001 | ||
| Unspecified/others | 1188 (11.9%) | 2843 (10.4%) | −1.5%; p < 0.001 | ||
| Causes of healthcare assistance for DV-related episodes | Injuries or psychiatric conditions | 6361 (63.8%) | 20,702 (75.8%) | ||
| Injuries | 5206 (52.2%) | 13,505 (49.4%) | −2.8%; p < 0.001 | ||
| Psychiatric conditions | 412 (4.1%) | 2789 (10.2%) | 6.1%; p < 0.001 | ||
| Injuries and psychiatric cond. | 743 (7.5%) | 4408 (16.1%) | 8.6%; p < 0.001 | ||
| Other diseases and health cond. | 3609 (36.2%) | 6616 (24.2%) | −12%; p < 0.001 | ||
| Average number of co-existing condition | 1.9 | 2.9 | 1; p < 0.001 | ||
| Mortality | 6 (0.06%) | 21 (0.08%) | 0.02%; p = 0.596 | ||
| Sex: female | 7951 (80.1%) | 22,088 (80.9%) | 0.8%; p = 0.088 | ||
| Average age | 25.9 | 29.9 | 4%; p < 0.001 | ||
| Age groups | Minors | 3366 (33.8%) | 6523 (23.9%) | −9.9%; p < 0.001 | |
| 0–4 | 1288 (12.9%) | 2264 (8.3%) | −4.6%; p < 0.001 | ||
| 5–17 | 2078 (20.8%) | 4259 (15.6%) | −5.2%; p < 0.001 | ||
| Adults | 6604 (66.2%) | 20,795 (76.1%) | +9.9%; p < 0.001 | ||
| 18–34 | 3572 (35.8%) | 11,089 (40.6%) | 4.8%; p < 0.001 | ||
| 35–64 | 2803 (28.1%) | 8592 (31.5%) | 3.4%; p < 0.001 | ||
| 65+ | 229 (2.3%) | 1114 (4.1%) | 1.8%; p < 0.001 | ||
| Total | 9970 (100%) | 27,318 (100%) | 0%; p < 0.001 | ||
| Hospitalizations | Admissions per month | 77.1 | 95.6 | 18.5; p < 0.001 | |
| Abuse type | Physical | 3566 (48.7%) | 4011 (44.6%) | −4.1%; p < 0.001 | |
| Emotional psychological | 333 (4.5%) | 527 (5.9%) | 1.4%; p < 0.001 | ||
| Neglect | 1636 (22.3%) | 2358 (26.2%) | 3.9%; p < 0.001 | ||
| Sexual | 549 (7.5%) | 725 (8.1%) | 0.6%; p = 0.187 | ||
| Unspecified/others | 1472 (20.1%) | 1715 (19.1%) | −1%; p0.099 | ||
| Cause of healthcare assistance for DV-related episodes | Injuries or psychiatric conditions | 6032 (82.4%) | 7657 (85.2%) | ||
| Injuries | 2630 (35.9%) | 2692 (29.9%) | −6%; p < 0.001 | ||
| Psychiatric conditions | 1809 (24.7%) | 2559 (28.5%) | 3.8%; p < 0.001 | ||
| Injuries and psychiatric cond. | 1593 (21.8%) | 2406 (26.8%) | 5%; p < 0.001 | ||
| Other diseases and health cond. | 1288 (17.6%) | 1332 (14.8%) | −2.8%; p < 0.001 | ||
| Average number of co-existing condition | 6.8 | 10.2 | 3.4; p < 0.001 | ||
| Mortality | 0 (0%) | 21 (0.23%) | 0.2%; p < 0.001 | ||
| Length of stays | 7.6 | 8.3 | 0.7; p < 0.001 | ||
| Charge per admission | $56,534 | $77,092 | $20,557; p < 0.001 | ||
| Total charge | $415,157,884 | $721,007,977 | N/A | ||
| Payment category | Invalid/blank | 1 (0%) | 1 (0%) | 0%; p = 1 | |
| Medicare | 1927 (26.3%) | 2654 (29.5%) | 3.2%; p < 0.001 | ||
| Medi-Cal | 3085 (42.1%) | 3752 (41.7%) | −0.4%; p = 0.602 | ||
| Private coverage | 1257 (17.2%) | 1399 (15.6%) | −1.6%; p = 0.006 | ||
| Workers' compensation | 3 (0%) | 5 (0.1%) | 0.1%; p = 0.738 | ||
| County indigent programs | 266 (3.6%) | 248 (2.8%) | −0.8%; p = 0.002 | ||
| Other government | 299 (4.1%) | 457 (5.1%) | 1%; p = 0.003 | ||
| Other indigent | 39 (0.5%) | 35 (0.4%) | −0.1%; p = 0.197 | ||
| Self-pay | 417 (5.7%) | 400 (4.4%) | −1.3%; p < 0.001 | ||
| Other payer | 26 (0.4%) | 38 (0.4%) | 0%; p = 0.529 | ||
| Sex: female | 4878 (66.6%) | 6106 (67.9%) | 1.3%; p = 0.084 | ||
| Average age | 35.2 | 38.0 | 2.8; p < 0.001 | ||
| Age groups | Minors | 3009 (41.1%) | 3378 (37.6%) | −3.5; p < 0.001 | |
| 0–4 | 2231 (29.7%) | 2392 (26.6%) | −3%; p < 0.001 | ||
| 5–17 | 855 (11.4%) | 986 (11%) | −0.5%; p = 0.33 | ||
| Adults | 4310 (58.9%) | 5611 (62.4%) | +3.5; p < 0.001 | ||
| 18–34 | 978 (13%) | 1127 (12.5%) | −0.6%; p = 0.289 | ||
| 35–64 | 1476 (19.7%) | 1990 (22.1%) | 2.3%; p = 0.014 | ||
| 65+ | 1960 (26.1%) | 2494 (27.7%) | 1.7%; p < 0.001 | ||
| Total | 7319 (100%) | 8989 (100%) | |||
3. Results
All DV-related hospitalizations and visits to EDs in California between January 2000 and September 2015 (53,596), including IPV, child and elder abuse, were analyzed. Table 1 reports descriptive statistics for DV variables for the pre-recession (January 2000 to November 2007) and the recession/post-recession period (December 2007 to September 2015). The number of ED visits substantially exceed the number of hospitalizations during the recession/post-recession period (75.2%, 27,318 out of 8989) and to a lesser extent during the pre-recession (57.7%, 9970 out of 7319).
The number of ED visits per month for all-forms of DV nearly tripled during the recession/post-recession period as compared to the pre-recession period (290.6 vs. 104.9, respectively); a less pronounced increase in DV episodes per month was found in DV-related hospitalizations (95.6 vs. 77.1). The average number of co-existing conditions per ED patient also increased in both, EDs (1.9 vs. 2.9 during the pre-recession, and recession/post-recession period, respectively) and hospitals (6.8 vs. 10.2). This included the percent of episodes associated with psychiatric conditions (psychiatric conditions alone or together with injuries and fractures). In-hospital mortality increased during the recession/post-recession period as compared to the pre-recession period (0.23% vs. 0%, respectively). There was no increase in mortality in EDs (0.06% vs. 0.08%, p = 0.596). The percent of DV-related patients that were adults, rather than minors, increased in the recession/post-recession period as compared to the pre-recession period in the ED (76.1% vs. 66.2%) and hospitals (62.4% vs. 58.9%). Similar percentages of female patients were found over time in EDs (80.1% vs. 80.9% during the pre-recession, and recession/post-recession period, respectively; p = 0.088) and hospitals (66.6% vs. 67.9%; p = 0.084).
The estimated total cost for all DV hospitalizations for January 2000 to September 2015 was $1,136,165,861. We found a relative slight increase in hospital length of stay during the recession/post-recession as compared to the pre-recession period (7.6 vs. 8.3; p < 0.001) (Table 1). However, the inflation-adjusted charge per hospitalization increased dramatically over time ($56,534 vs. $77,092). Together, the percent of “private coverage” and “self-pay” hospital payment slightly decreased for the recession/post-recession compared to the pre-recession (22.9% vs. 20.0%, respectively), while the combination of “Medicare”, “Medi-Cal” and “Other Government” slightly increased (72.6% vs. 76.3%, respectively). No data on length of stay, cost or payment was available for ED visits.
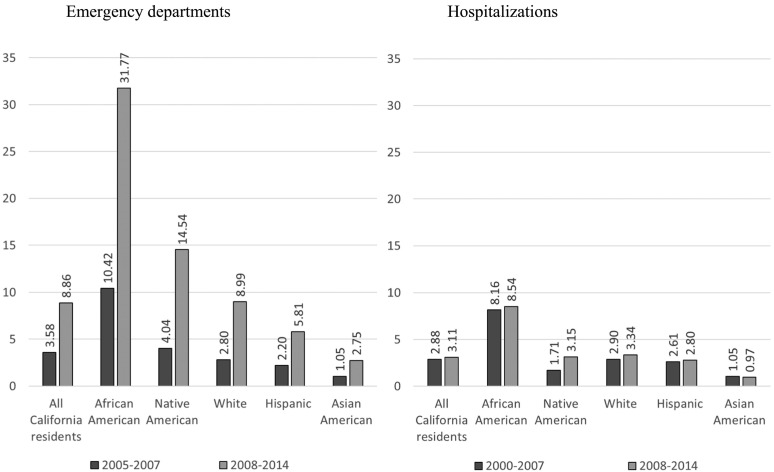
Fig. 1 displays DV-related visits to the ED and hospitalizations as an age-adjusted rate per 100,000 California residents estimated for all Californians and five ethnic/race groups in the two analyzed time periods. The rates of DV-related visits among African Americans is over three times the rates for all California residents in EDs (3.58 vs. 10.42 ED visits per 100,000 in all California residents and African Americans, respectively, during the pre-recession period; 8.86 vs. 31.77 during the recession/post-recession period) and hospitals (2.88 vs. 8.16 during the pre-recession period; 3.11 vs. 8.54 during the recession/post-recession period). ED rates increased for all Californians in the recession/post-recession period compared to the pre-recession; however, Native Americans were disproportionately affected. Hospitalization rates remained fairly similar from the pre-recession as compared to the recession/post-recession period except for Native Americans, which nearly doubled.
Fig. 1.
Domestic violence-related hospitalizations and visits to emergency departments (ED). Ethnic/race age-adjusted rates per 100,000 inhabitants.
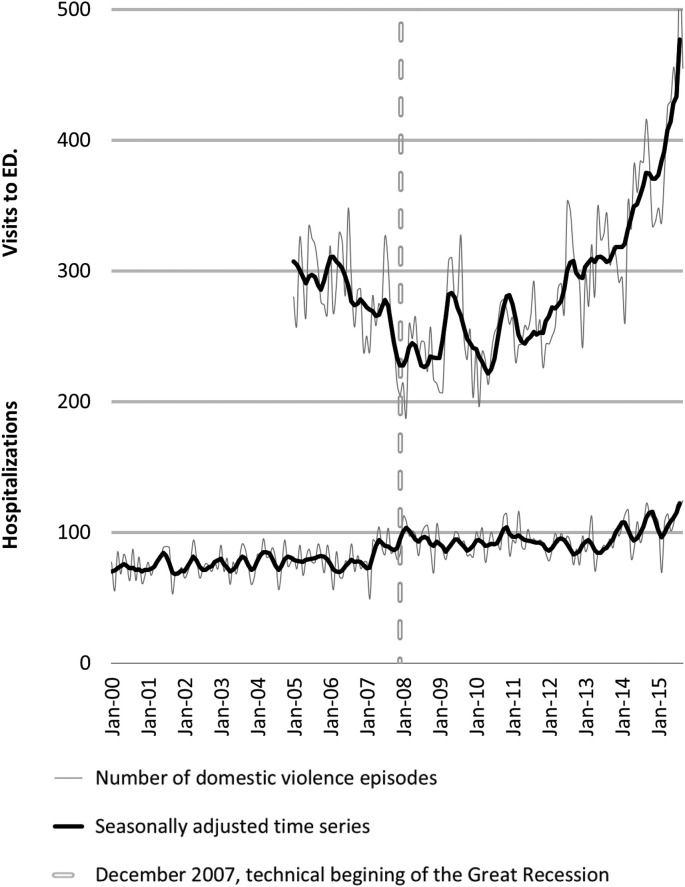
Fig. 2 shows the monthly number of DV episodes in hospitals and EDs. An abrupt turning point was found for ED visits in December 2007, during the technical beginning of the Great Recession; ED visits decreased 1.48 episodes per month during the pre-recession period and then increased 0.35 episodes per month during the recession/post-recession period (slope increase 1.83 (−1.48 vs. +0.35), df = 66, t-ratio = −5.35, p < 0.0001). The number of DV-related hospitalizations per month began a slow but steady step increase in April 2007 [mean difference = 15.5 (77.5 vs. 93.0); df = 114, t-test = −13.9, p < 0.0001], during the mortgage market crisis.
Fig. 2.
Domestic violence-related visits to emergency departments (ED) and hospitalizations in California, January 2000 – Sept 2015.
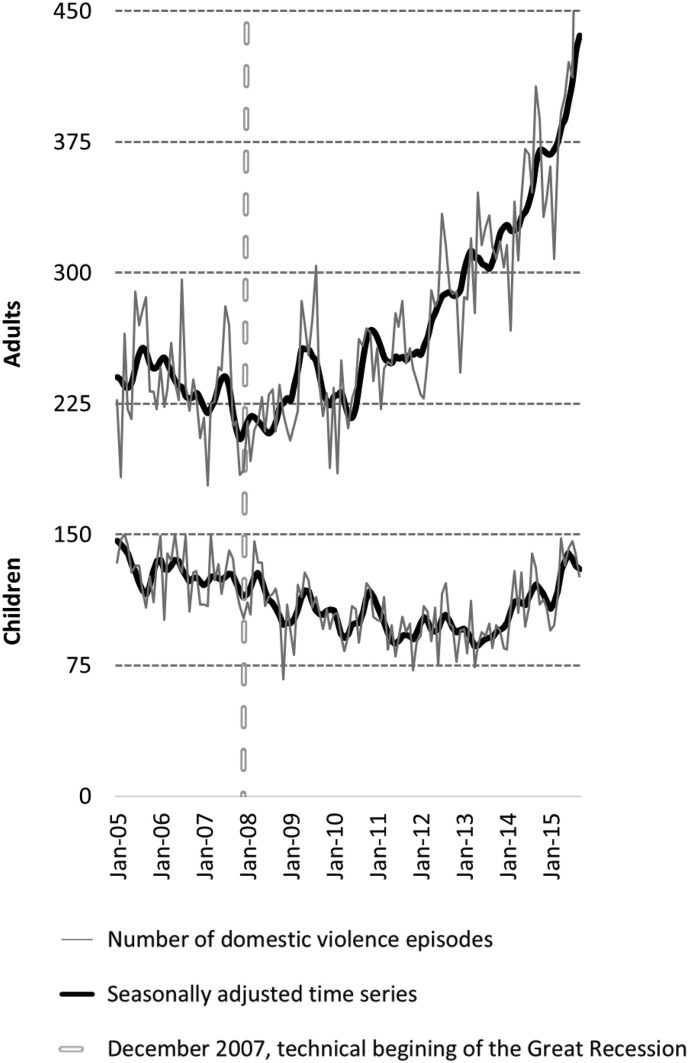
Fig. 3 displays the monthly overall number of DV episodes (services in hospitals and EDs combined) for adults and minors between January 2005 and September 2015 (no available ED data prior to January 2005). There was no statistically significant change for minors between the pre-recession and recession/post-recession time periods. However, DV-related episodes in the adult population began to rise starting December 2007, the technical beginning of the Great Recession [slope increase 1.57 (−0.80 vs. 0.77); df = 66, t.ratio = −15.249, p = 0.0001].
Fig. 3.
Domestic violence-related episodes in adults and children in California, January 2005 – Sept 2015.
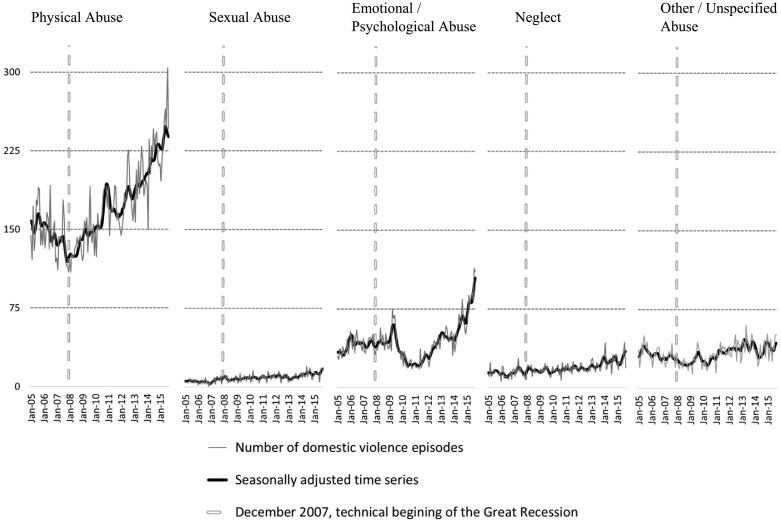
The monthly number of DV episodes in the adult population by type of abuse is displayed in Fig. 4 . Both neglect (nutritional) and emotional/psychological abuse began to increase pre-recession ([June 2006; slope increase 0.38 (−1.2 vs. -0.82); df = 32, t.ratio = −2.91, p = 0.0065] and [December 2006; slope increase 0.17 (−0.08 vs. +0.09); df = 44, t.ratio = −3.995, p = 0.0002]), respectively. Physical abuse increased beginning December 2007 [slope increase 2.234 (−0.9 vs. +1.33); df = 66, t.ratio = −15.249, p = 0.0001], and other/unspecified abuse began to rise December 2008 [slope increase 0.62 (−0.31 vs. +0.32); df = 90, t.ratio = −13.987, p = 0.0001]. Adult sexual abuse remained unchanged until the beginning of February 2014 [slope increase 2.5 (+0.12 vs. +2.62); df = 34, t.ratio = −9.725, p = 0.0001]. This time point was also associated with an uptick in cases of minor abuse (Fig. 3, [slope increase 1.41 (−0.01 vs. +1.4); df = 34, t.ratio = −3.773, p = 0.0006]).
Fig. 4.
Domestic violence-related episodes in the adult population (18+) by type of abuse in California, January 2005 – Sept 2015.
4. Discussion
We conducted one of the first studies, to date, to examine the impact of a modern recession on DV rates and hospital and ED visits. Our findings show that the number of DV episodes per month dramatically increased from 182.0 to 386.2 between the pre- and post-recession and was mainly attributable to physical abuse episodes in adults, with African American and Native American persons disproportionally impacted. Co-existing psychiatric conditions and in-hospital mortality ratios also increased over time, along with charges per hospitalization. Our findings corroborate existing studies showing a correlation between financial stress and DV-related events (Pillemer et al., 2016; Renzetti, 2009; Schneider et al., 2016; Schneider et al., 2017; Berger et al., 2011).
For the period analyzed (2000–2015), the estimated total charge for all analyzed DV hospitalizations (data not available for EDs) was over one billion dollars ($1,136,165,861). Length of hospital stays slightly increased during the recession/post-recession period as compared to the pre-recession period, yet the inflation-adjusted charge per hospitalization dramatically increased over time. It is important to note that the described increase in DV-related hospitalizations during the recession does not correspond to a general trend in healthcare in California. For example, California cancer hospital rates dropped during the recession (OSHPD, 2020; Gomez et al., 2017). However, an increasing demand for emergency care during the recession and post-recession period has been reported and may reflect limitations in accessing care in other parts of the healthcare system (Hsia et al., 2018). The number of co-existing conditions and in-hospital mortality ratios increased over time, suggesting a rise in the number of more severe DV episodes during the recession/post-recession period. Increases were also seen in the number of DV-related hotline calls during the recession (Renzetti, 2009) and police reports (Becerra, 2018; Harris, 2009). Moreover, the number of California police calls for weapon-involved DV episodes steadily increased from 2008 to 2014 (65,219 vs. 75,102, respectively); the percentage of murders that involved DV with respect to the total murders committed in California was relative stable between 2000 and 2007 (8.4% vs. 8.3%, respectively), but abruptly increased from 2008 to 2010 (8.1% vs. 12.3%, respectively) (Becerra, 2018; Harris, 2009). An increasing number of co-existing psychiatric conditions was found in both ED and hospital admissions. Psychiatric comorbidity, including substance abuse, was found in approximately 50% of DV patient. Importantly, the true number of co-existing conditions, including psychiatric conditions, could be much higher because not all coexisting conditions are reported; as a standard rule only those that contribute to explaining the health care service must be reported.
DV is among the most underreported crimes worldwide (Strong et al., 2010), and DV-related hospitalizations and visits to EDs represent particularly severe cases. Therefore, DV-related health services are generally considered to be only the tip of the epidemiologic iceberg, with minoritized people and populations highly impacted (Office of Women's Health, 2012). Our study findings showed that ED visits and hospitalizations were disproportionately higher in African American and Native American persons as compared to others.
Our findings bear important information for health care providers and systems in preparing for future recessions. Screening for DV in health care settings is important and can be done successfully (O'Doherty et al., 2015; Feltner et al., 2018). Drawing from our early learning in the novel coronavirus (COVID-19) era – which has had widespread economic ramifications (Semuels, 2020; RT, 2020; Menickella, 2020) – health care providers and systems should establish systematic partnerships with community-based partners specializing in DV service provision and should implement safe, proactive outreach to persons experiencing domestic violence and/or at high risk for domestic violence. Bonomi and Martin (2020) recently described professional advocacy models that involve safely and proactively connecting with DV victims via text message to buffer against abusers' manipulation strategies. Viveiros and Bonomi (2020) suggest such safe, proactive outreach is especially needed for minoritized people, who may be especially isolated, experiencing disconnections from services, and facing extreme financial stress.
In line with our results, intimate partner violence increased during the 2007 Great Recession in the U.S. (Schneider et al., 2016). We found an abrupt turning-point for the overall number of DV episodes that began in December 2007, mainly attributable to physical abuse in the adult population. There is also scientific evidence that child abuse increased during the 2007 Great Recession in the U.S (Schneider et al., 2017; Berger et al., 2011). However, we found no significant increasing trends for the overall number of DV episodes in minors in California during the economic recession. We do not have a plausible reason that can explain why the recession had a dramatic impact on hospitalizations and visits to EDs by adults while no impact on services utilization was found for minors.
Many of the DV hospital episodes studied here involved emotional abuse, and neglect, among others, rather than physical abuse. One-third of U.S. women experience intimate partner emotional/psychological abuse during their lifetime (Smith et al., 2018). While the links between economic insecurity and economic abuse are emerging, the need to include financial abuse (often hidden and invisible) as a form of DV has garnered great attention in the scientific literature (Postmus et al., 2020). Importantly, the Trump administration made significant changes to the definition of DV and sexual assault in April 2019. The new definition only considers physical harm that constitutes a felony to be DV. Therefore, those experiencing psychological/emotional or economic harms may no longer fall under the U.S. Department of Justice's definition of DV. Narrowing the definition of DV is inconsistent with scientific knowledge (Postmus et al., 2020). According to experts, the new definition will have significant repercussions for millions of victims of DV; narrowing the definition will lead to victims not being able to access protection and DV services and the number of trials for domestic and sexual violence will be reduced (Oppenheim, 2019; Nanasi, 2019).
Our study has strengths and limitations. The main strength is the use of a large representative dataset. A core limitation is that the study design precluded establishing causal relationships between the recession and DV-related service use. A second limitation is the potential for omitted variables bias; we did not have access to data representing the full range of variables that could influence DV-related correlates. Finally, many health settings fail to screen for domestic violence adequately (Schafer et al., 2008; Rudman, 2000). Therefore, a significant portion of DV-hospitalizations could be missed. On the other hand, there has been a significant effort over the past decades to expand and improve DV evidence-based screening processes in healthcare settings, which could explain the increase in DV observed over time in California.
Our findings provide evidence for the impact of economic recessions on DV episodes, and DV-related ED visits and hospitalizations. Given the impending economic recession due to the novel coronavirus, and future recessions, we urge improving DV screening, prevention and response and expanding research. Such research should focus on the most economically and socially vulnerable populations, including systematic strategies for proactive outreach (Bonomi and Martin, 2020; Viveiros and Bonomi, 2020).
CRediT authorship contribution statement
Alvaro Medel-Herrero: Conceptualization, Data curation, Funding acquisition, Methodology, Formal analysis, Writing - original draft. Martha Shumway: Data curation, Funding acquisition, Methodology, Writing - review & editing. Suzette Smiley-Jewell: Data curation, Funding acquisition, Methodology, Writing - review & editing. Amy Bonomi: Data curation, Funding acquisition, Methodology, Writing - review & editing. Dennis Reidy: Data curation, Funding acquisition, Methodology, Writing - review & editing.
Acknowledgments
Acknowledgments
We thank the National Coalition Against Domestic Violence (NCADV), National Center on Domestic and Sexual Violence (NCDSV), California Partnership to End Domestic Violence (CPEDV), Futures Without Violence (FWV), Healthy Relationships California (HRC) and the California Coalition Against Sexual Assault (CALCASA) for supporting this project.
Funding
This research was supported by the Feminist Research Institute (FRI) Seed Grant, 2018–2019.
Declaration of competing interest
We have no conflicts of interest to declare.
References
- Becerra X. California Homicide Statistics for 2017. California Department of Justice; 2018. Homicide in California 2017. [Google Scholar]
- Berger R.P., Fromkin J.B., Stutz H., Makoroff K., Scribano P.V., Feldman K., Tu L.C., Fabio A. Abusive head trauma during a time of increased unemployment: a multicenter analysis. Pediatrics. 2011;128(4) doi: 10.1542/peds.2010-2185. [DOI] [PubMed] [Google Scholar]
- Bonomi A.E., Martin D. Domestic abusers: expert triangulators, new victim advocacy models to buffer against it. J. Fam. Violence. 2020 doi: 10.1007/s10896-020-00156-2. [DOI] [Google Scholar]
- Department of Housing and Urban Development (DHUD) Office of Policy Development and Research; 2010. Report to Congress on the Root Causes of the Foreclosure Crisis US. [Google Scholar]
- Feltner C., Wallace I., Berkman N. Screening for intimate partner violence, elder abuse, and abuse of vulnerable adults: evidence report and systematic review for the US preventive services task force. JAMA. 2018;320(16):1688–1701. doi: 10.1001/jama.2018.13212. [DOI] [PubMed] [Google Scholar]
- Finkelhor D., Turner H., Ormrod H., Hamby S., Kracke K. Juvenile Justice Bulletin. 2009. Children’s exposure to violence: a comprehensive National Survey. [Google Scholar]
- Gomez S.L., Canchola A.J., Nelson D.O., Keegan T.H., Clarke C.A., Cheng I., Shariff-Marco S., DeRouen M., Catalano R., Satariano W.A., Davidson-Allen K., Glaser S.L. Recent declines in cancer incidence: related to the Great Recession? Cancer Causes Control. 2017;28(2):145–154. doi: 10.1007/s10552-016-0846-y. [DOI] [PubMed] [Google Scholar]
- Harris K.D. California Homicide Statistics for 2010. California Department of Justice; 2009. Homicide in California 2010. [Google Scholar]
- Hsia R.Y., Sabbagh S.H., Guo J., Nuckton T.J., Niedzwiecki M.J. Trends in the utilization of emergency departments in California, 2005–2015: a retrospective analysis. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-021392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huecker M.R., Smock W. StatPearls. 2019. Kentucky domestic violence. [Google Scholar]
- Irons J. Briefing Paper #243. September 30. Economic Policy Institute; 2009. Economic scarring. The long-term impacts of the recession. [Google Scholar]
- Klein RJ, Schoenborn CA. (2001) Age adjustment using the 2000 Projected U.S. Population. Statistical Notes. CDC, National Center for Health Statistics. Number 20. [PubMed]
- Length R.V. Least-squares means: the R package lsmeans. J. Stat. Softw. 2016;69(1) [Google Scholar]
- Margerison-Zilko C., Goldman-Mellor S., Falconi A., Downing J. Health impacts of the Great Recession: a critical review. Curr Epidemiol Rep. 2016;3(1):81–91. doi: 10.1007/s40471-016-0068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menickella B. COVID-19 worldwide: the Pandemic’s impact on the economy and markets. Forbes. 2020;(Apr 8) [Google Scholar]
- Nanasi N. The trump administration quietly changed the definition of domestic violence and we have no idea what for. Jurisprudence. 2019;(Jan 21) [Google Scholar]
- O’Doherty L., Hegarty K., Ramsay J., Davidson L.L., Feder G., Taft A. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst. Rev. 2015;7 doi: 10.1002/14651858.CD007007.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Women’’s Health (OWH) Results from the 2009 California Women’s Health Survey. Issue 8, Summer, Num. 21. 2012. California Department of Health Care Services and California Department of Public Health. Data Points. [Google Scholar]
- Oppenheim M. Trump administration ‘rolling back women’s rights by 50 years’ by changing definitions of domestic violence and sexual assault. Independent. 2019;(January 24) [Google Scholar]
- OSHPD Data and reports/healthcare utilization, inpatient ICD-9/ICD-10-CM code frequencies. 2020. https://oshpd.ca.gov Retrieved from.
- Peterson C., Florence C., Klevens J. The economic burden of child maltreatment in the United States, 2015. Child Abuse Negl. 2018;86:178–183. doi: 10.1016/j.chiabu.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C., Kearns M.C., McIntosh W.L., Estefan L.F., Nicolaidis C., McCollister K.E.…Florence C. Lifetime economic burden of intimate partner violence among US adults. American Journal of Preventive Medicine. 2018;55(4):433–444. doi: 10.1016/j.amepre.2018.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillemer K., Burnes D., Riffin C., Lachs M.S. Elder abuse: global situation, risk factors, and prevention strategies. Gerontologist. 2016;56(Suppl. 2):S194–S205. doi: 10.1093/geront/gnw004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postmus J.L., Hoge G.L., Breckenridge J., Sharp-Jeffs N., Chung D. Economic abuse as an invisible form of domestic violence: a multicountry review. Trauma Violence Abuse. 2020 Apr;21(2):261–283. doi: 10.1177/1524838018764160. [DOI] [PubMed] [Google Scholar]
- Renzetti C.M. CRVAW Faculty Research Reports and Papers. 2009. Economic stress and domestic violence; p. 1. [Google Scholar]
- RT Covid-19 may cause deepest economic crisis ‘of our lifetimes’ — WTO chief. RT.com 8 Apr, 2020. 2020. https://www.rt.com/business/485313-wto-covid19-deepest-economic-crisis/ Retrieved from.
- Rudman W.J. Family Violence Prevention Fund. 2000. Coding and documentation of domestic violence.https://www.futureswithoutviolence.org/userfiles/file/HealthCare/codingpaper.pdf Retrieved from: [Google Scholar]
- Schafer S.D., Drach L., Hedberg K., Kohn M.A. Using diagnostic codes to screen for intimate partner violence in Oregon emergency departments and hospitals. Public Health Rep. 2008;123(5):628–635. doi: 10.1177/003335490812300513. Sep-Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider D., Harknett K., McLanahan S. Intimate partner violence in the Great Recession. Demography. 2016;53(2):471–505. doi: 10.1007/s13524-016-0462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider W., Waldfogel J., Brooks-Gunnc J. The Great Recession and risk for child abuse and neglect. Child Youth Serv. Rev. 2017;72:71–81. doi: 10.1016/j.childyouth.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semuels A. As COVID-19 crashes the economy, workers and business owners wonder if anything can save them from financial ruin. TIME. Business. 2020 https://time.com/5805526/coronavirus-economy-layoffs/ March 18, 2020. Retrieved from. [Google Scholar]
- Shumway R.H., Stoffer D.S. Third edition. Springer Texts in Statistics, LLC; NY: 2010. Time Series Analysis and its Applications with R Examples. [Google Scholar]
- Smith S.G., Zhang X., Basile K.C., Merrick M.T., Wang J., Kresnow M., Chen J. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; Atlanta, GA: 2018. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief – Updated Release. [Google Scholar]
- Strong Bryan, DeVault Christine, Cohen Theodore. Cengage Learning. 2010. The marriage and family experience: intimate relationships in a changing society; p. 447. Archived from the original on January 10, 2017. [Google Scholar]
- Viveiros N., Bonomi A. Novel Coronavirus (COVID-19): Violence, Reproductive Rights and Related Health Risks for Women, Opportunities for Practice Innovation. J Fam Violence. 2020:1–5. doi: 10.1007/s10896-020-00169-x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7275128/ [DOI] [PMC free article] [PubMed] [Google Scholar]