Abstract
Background
As Covid-19 evolved into a world-wide pandemic, hospitals reported marked declines in strokes, only to be followed by reports of increased numbers of young people presenting with large-vessel occlusions. We reviewed our patient data-base to determine if similar or other novel trends were present.
Results
Our Thrombectomy Stroke Center experienced marked declines in ED visits from 2,349 in early March to 1,178 in late April, stroke alerts dropped from 34 to 14 during the same period. Average monthly stroke admissions dropped from 34 in 2019 to 23 in 2020. Nonetheless, in March, we had 12 patients eligible for tPA, which is twice the typical caseload and was unexpected given the low overall stroke presentations. Although the neurointervention caseload was low, the patients were significantly younger. Of the acute intervention patients in March, 5 of the 12 patients were ≤ 60 years old, and two were in their 30’s. These trends are similar to those reported elsewhere but were highly unusual for our center as our catchment area is predominantly Caucasian with 34 % of the population > 65 years of age.
Conclusions
Even in low risk centers Covid-19 will likely impart unique stroke presentations. It will be imperative to determine the mechanisms responsible for these changes so we can institute effective strategies for optimal stroke prevention as well as maintain timely acute interventions.
Key Words: Acute stroke, Covid-19, Thrombectomy, IV tPA, Thromboembolic
As COVID19 evolved into a world-wide pandemic, there seemed to be an inexplicable decline in stroke presentations both in the US and abroad.1 Then within weeks, some of the hardest hit hospitals began to report more strokes, particularly in young patients with no apparent risks.2 In light of these reports, we reviewed our stroke program data to determine if similar or other novel patterns were present in our patient population.
Results
Our hospital is a Thrombectomy Stroke Center (TSC) in south Florida whose county ranked second in COVID 19 cases and deaths. There was a profound drop in ED (emergency department) visits from 2,349 in the first two weeks of March to 1,178 in the final two weeks of April. Stroke alerts dropped from 34 to 14 during the same period (Table 1 ). The total number of patients admitted with an acute stroke in March and April of 2020 was 46, compared to 68 in 2019. There were only seven stroke neurointervention cases during the same period compared to 14 in 2019.
Table 1.
Decline in Patient Presentations in Early Covid-19 Pandemic
| DATE | EMERGENCY ROOM VISITS |
STROKE ALERTS | |
|---|---|---|---|
| “Walk-in” Arrivals | EMS Arrivals | ||
| MARCH | |||
| Week 1 & 2 | 2,024 | 325 | 34 |
| Week 3 & 4 | 1,446 | 267 | 21 |
| APRIL | |||
| Week 1 & 2 | 1,074 | 177 | 9 |
| Week 3 & 4 | 990 | 188 | 14 |
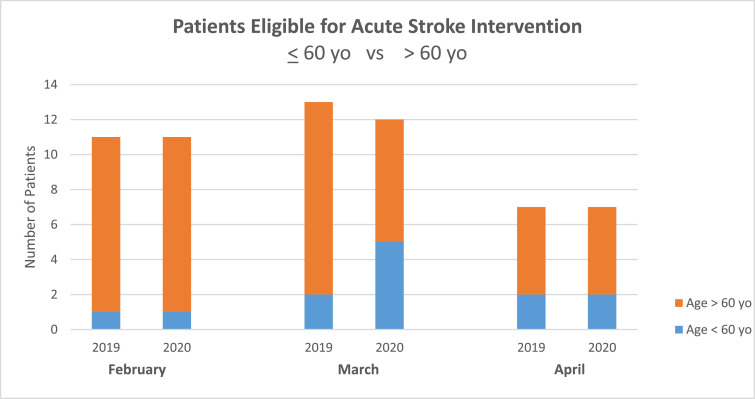
Despite these declines, we had 12 tissue plasminogen activator (tPA) eligible patients in March 2020, and typically we average six/month. There were significantly more patients ≤ 60 years of age who underwent any acute stroke intervention (tPA and/or neurointervention). In March, 5 of 12 were ≤ 60 years of age, compared to only two of 13 in 2019 (Graph 1 ). Amongst the thrombectomy cases, two were very young, 31 and 35 years old and both were African American.
Graph 1.
Age of patients eligible for acute stroke interventions in 2020 compared to 2019.
Discussion
Our TSC's ED visits, stroke alerts, stroke admissions and neurointervention cases did indeed drop precipitously in the first few months of the Covid-19 pandemic in keeping with some of the earliest reports. But in spite of these dramatic declines, we had twice the number of patients who were tPA-eligible in March, the month that coincided with our region's onset of coronavirus presentations. Whether directly related to coronavirus infection is difficult to prove as testing was not yet widespread and other risk factors that may have been exacerbated by the pandemic such as medication non-compliance, lifestyle changes or difficulty accessing health care, cannot be excluded. Nonetheless, as the thromboembolic risks associated with Covid-19 infection become increasingly apparent,3 , 4 the brief uptick in tPA cases we saw may have been a “red flag” and a unique pattern to remember as we face the coming months of possible viral surges. Another concern was raised by noting the overall lower stroke admissions to the hospital. Were only the patients with more severe or obvious deficits coming to the ED? Were people with mild symptoms simply avoiding the hospital giving the false impression of an overall lower stroke incidence? The answer remains unclear however our center has instituted community stroke education to remind people of the benefit of early intervention and we remain vigilant to look for “missed strokes” so that proper secondary prevention can be instituted.
Similar to the earlier reports from New York and Philadelphia, our center also encountered younger patients with large vessel occlusions. Although the neurointervention caseload was uncharacteristically low in March and April, four of the seven patients were ≤ 60 years old, and two of those were African American women in their 30’s. This trend of younger stroke patients was also present in the candidates for tPA. This was a novel finding and quite unexpected at our TSC, as our surrounding community is predominantly Caucasian with 34% of the population ≥ 65 years of age, no recent changes in the catchment area, physician staffing or proximity of other stroke centers that might have affected our hospital's population.
In conclusion, our findings support the notion that Covid-19 has surely impacted stroke presentations, even in presumed low risk communities such as ours, and physicians caring for acute stroke patients may need to recognize and anticipate these unique patterns. As we move forward in this pandemic, it will also be imperative that we determine what mechanisms underlie these changes so that we can implement both preventative strategies and continue the most effective acute stroke treatments.
Authors contributed equally to the patient data collection, review and preparation of the manuscript.
Declaration of Competing Interest
There are no known financial or personal conflicts of interest.
References
- 1.Morelli N., Rota E., Terracciano C. The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur Neurol. 2020 Apr 14:1–3. doi: 10.1159/000507666. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oxley T.J., Mocco J., Majidi S. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med. 2020 Apr 28 doi: 10.1056/NEJMc2009787. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hess D.C., Eldahshan W., Rutkowski E. COVID-19-Related Stroke. Transl Stroke Res. 2020;11(3):322–325. doi: 10.1007/s12975-020-00818-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M. Incidence of Thrombotic Complications in Critically Ill ICU Patients with COVID-19. Thromb Res. 2020 Apr 10 doi: 10.1016/jthromres.2020.04.013. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]