Abstract
Introduction
Existing socioeconomic and racial disparities in healthcare access in New York City have likely impacted the public health response to COVID-19. An ecological study was performed to determine the spatial distribution of COVID-19 testing by ZIP code Tabulation Area and investigate if testing was associated with race or SES.
Methods
Data were obtained from the New York City coronavirus data repository and 2018 American Community Survey 5-year estimates. A combined index of SES was created using principal component analysis and incorporated household income, gross rent, poverty, education, working class status, unemployment, and occupants per room. Multivariable Poisson regressions were performed to predict the number of total tests and the ratio of positive tests to total tests performed, using the SES index, racial composition, and Hispanic composition as predictors.
Results
The number of total tests significantly increased with the increasing proportion of white residents (β=0.004, SE=0.001, p=0.0032) but not with increasing Hispanic composition or SES index score. The ratio of positive tests to total tests significantly decreased with the increasing proportion of white residents in the ZIP code Tabulation Area (β= −0.003, SE=0.000 6, p<0.001) and with increasing SES index score (β= −0.001 6, SE=0.0007, p=0.0159).
Conclusions
In New York City, COVID-19 testing has not been proportional to need; existing socioeconomic and racial disparities in healthcare access have likely impacted public health response. There is urgent need for widespread testing and public health outreach for the most vulnerable communities in New York City.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a rapidly evolving pandemic that emerged at the end of 2019 and has infected more than 8.8 million people and caused more than 450,000 deaths around the world.1 The first official case in New York City (NYC) was confirmed on March 1, 2020, and since then, more than 200,000 cases, 53,000 hospitalizations, and more than 17,500 deaths have affected the city in the brief space of a few weeks.2 COVID-19 testing was implemented relatively late and at a very slow pace in the U.S. Although testing should be performed for contact tracing to prevent COVID-19 spread, it is also a diagnostic tool and remains an important piece in the mitigation phase of a pandemic.
The U.S. has implemented COVID-19 testing in a sporadic and disorganized way, partly because the Centers for Disease Control and Prevention (CDC) guidelines changed several times over a short time span,3 owing in part to the quality and speed of the diagnostic test that was initially very poor. At the beginning of the year, CDC guidelines for testing were restricted to those who recently traveled to China or were in contact with an infected person, and testing performed in state laboratories was halted because of problems with the test itself.4 The test results would require several days to be produced and released, limiting the test's utility for contact tracing, transmission prevention, and disease containment. Currently, CDC acknowledges on their website that it may remain difficult for individuals to be tested.5
Only recently, NYC has released data that minorities are disproportionately affected by COVID-196 and is recognizing the importance of performing widespread testing and surveillance, especially in less affluent neighborhoods.
To study testing rates and positivity in NYC from the onset of COVID-19 and to identify areas of urgent need, this study analyzes existing data provided by the NYC Department of Health. The objectives of this analysis are (1) to study the spatial distribution of the number of COVID-19 tests, of COVID-19 positive tests, and the ratio of positive to total tests according to ZIP code Tabulation Area (ZCTA) and (2) to determine factors associated with testing and with positive testing according to ZCTA. The authors hypothesize that testing is currently not performed according to the metropolitan area's needs, and that the proportion of tests performed relative to the resident population is higher in areas of high SES, whereas the proportion of positive COVID-19 tests is disproportionately high among socioeconomically vulnerable populations.
METHODS
Study Sample
The number of COVID-19 tests performed and the number of positive COVID-19 tests were downloaded from the NYC Coronavirus (COVID-19) data repository hosted by the NYC Department of Health from March 2, 2020 current through April 6, 2020.2 The frequency of positive COVID-19 tests, total COVID-19 tests, and this ratio were mapped in ArcGIS according to quartiles. ZCTAs refer to the location of the person's residence. Cluster analysis was performed using Anselin Local Moran's I to identify high/low clusters of total tests/population of the ZCTA, and high/low clusters of positive tests/total tests.
Measures
ZCTA-level data on median household income in the past 12 months (Table B19013), median gross rent (Table B25064), percentage living <150% of the poverty line (e.g., an annual salary of ≤$26,200 for a 4-person household7; Table C17002), education (Table B15002), percentage working class (Table C24010), percentage unemployed (Table B23025), and more than 1 occupant per room (Table B25014) were downloaded from 2018 American Community Survey 5-year estimates.8 The percentage unemployed and the percentage working class were calculated on the civilian population aged ≥16 years. The education index was calculated on the population aged ≥25 years and is a weighted combination of the percentage high school graduate, high school only, and more than high school, with a greater value indicating higher educational attainment.
These variables were combined into an index of SES using principal component analysis (PCA) similar to Yost et al.9 This PCA differs from that of Yost and colleagues9 because it incorporates the occupants per room measure while removing the median home value to make the index more relevant to this study's area and for modeling COVID-19. The PCA resulted in 1 component being retained based on an eigenvalue >1.0 and the scree plot, which accounted for 72.4% of the variance. Each component of the SES index was ranked, standardized, and applied factor loadings according to the PCA.
A linear combination was then created to obtain an SES index score assigned to each ZCTA, according to:
ZCTAs were classified into quartiles of this SES score, with a score of 1 corresponding to the lowest SES quartile (i.e., lowest resourced) and a score of 4 representing the highest SES quartile.
In addition to the elements included in the SES index, the racial (white alone proportion) and Hispanic composition of each ZCTA were obtained from 2018 American Community Survey 5-year estimates.
Statistical Analysis
Wilcoxon rank sums tests were performed to assess differences in SES index components, racial composition, proportion of Hispanic residents, positive tests, and total tests according to SES quartiles. Mean, median, Quartile 1, Quartile 3, N, minimum, maximum, and SD were calculated for each component of the SES index, racial composition, and proportion of Hispanic residents according to SES quartiles. A multivariable Poisson regression was performed to predict the number of total tests, accounting for the total ZCTA population as an offset, and utilizing the SES index, the racial composition, and the proportion of Hispanic residents at the ZCTA level as predictors (Model 1). Multivariable Poisson regression was performed to predict the ratio of positive tests per total number of tests performed according to the SES index, the racial composition, and the proportion of Hispanic residents of the ZCTA as predictors (Model 2). All analyses were performed in SAS, version 9.4 and ArcGIS, version 10.7.1.
RESULTS
Each component of the SES index, as well as the proportion of white residents, proportion of Hispanic residents, ratio of total tests to population, and ratio of positive to total tests were analyzed according to quartiles of the SES index (Table 1 ). Across SES quartiles representing increasing SES, the median household income (p<0.0001), proportion of residences with more than 1 occupant per room (p<0.0001), percentage unemployed (p<0.0001), proportion living <150% of poverty line (p<0.0001), proportion working class (p<0.0001), education (p<0.0001), proportion of white residents (p<0.0001), the ratio of total tests to population (p=0.2911), and the ratio of positive tests to total tests (p<0.0001) increased. The proportion of Hispanic residents decreased across increasing SES index quartiles (p<0.0001).
Table 1.
SES Index Components, Racial Composition, Positive Tests, and Total Tests According to Quartiles of Increased SES Index
| Variable | Mean | Median | Q1 | Q3 | n | Min | Max | SD |
|---|---|---|---|---|---|---|---|---|
| Quartile 1 | ||||||||
| Median household income (dollars) | 42,114.67 | 39,653 | 28,921 | 51,521 | 45 | 21,149 | 83,240 | 14,256.98 |
| Median rent (dollars) | 1,145.44 | 1,153 | 1,019 | 1,285 | 45 | 690 | 1,591 | 198.6 |
| Unemployed (%) | 10.31 | 10.32 | 8.51 | 12.39 | 45 | 5.2 | 15.75678 | 2.45 |
| Living below 150% poverty line (%) | 39.74 | 39.78 | 30.19 | 49.67 | 45 | 18.7 | 62.49 | 11.79 |
| Working class (%) | 67.13 | 65.49 | 60.24 | 74.17 | 45 | 50.16 | 80.4 | 8.52 |
| Education index | 1,309.29 | 1,315.28 | 1,263.15 | 1,349.38 | 45 | 1,189.91 | 1,397.24 | 52.72 |
| >1 occupants per room | 2,228.38 | 1,910 | 996 | 2,882 | 45 | 218 | 6,329 | 1,549.98 |
| White residents (%) | 23.89 | 17.73 | 12.49 | 36.1 | 45 | 3.512 | 63.27 | 15.44 |
| Hispanic residents (%) | 45.7 | 47.53 | 25.62 | 66.57 | 45 | 12.43 | 75.77 | 20.32 |
| Total tests/population (%) | 0.87 | 0.83 | 0.77 | 0.97 | 45 | 0.57 | 1.42 | 0.18 |
| Positive tests/total tests (%) | 0.55 | 0.55 | 0.53 | 0.58 | 45 | 0.39 | 0.66 | 0.61 |
| Quartile 2 | ||||||||
| Median household income (dollars) | 60,041.11 | 60,076.5 | 51,345.00 | 69,099.00 | 44 | 35,859 | 85,707 | 11,846.73 |
| Median rent (dollars) | 1,401.07 | 1,403 | 1,312.00 | 1,508.50 | 44 | 963 | 1,746 | 166.83 |
| Unemployed (%) | 6.84 | 6.94 | 5.92 | 7.74 | 44 | 4.2 | 10.08 | 1.38 |
| Living below 150% poverty line (%) | 28.29 | 27.23 | 21.96 | 33.94 | 44 | 13.89 | 52.84 | 8.63 |
| Working class (%) | 60.77 | 63.11 | 53.65 | 67.49 | 44 | 38.68 | 77.14 | 9.19 |
| Education index | 1,352.4 | 1,357.72 | 1,313.92 | 1,397.16 | 44 | 1,188.21 | 1,473.17 | 57.84 |
| >1 occupants per room | 1,720.86 | 1,269.5 | 811.50 | 2,114.50 | 44 | 256 | 6,532 | 1,465.32 |
| White residents (%) | 37.24 | 34.6 | 21.61 | 57.27 | 44 | 1.76 | 73.7 | 20.11959 |
| Hispanic residents (%) | 27.06 | 24.6 | 16.17 | 36.43 | 44 | 5.1 | 63.06 | 15.52 |
| Total tests/population (%) | 0.86 | 0.82 | 0.69 | 1.04 | 44 | 0.48 | 1.36 | 0.25 |
| Positive tests/total tests (%) | 0.56 | 0.57 | 0.48 | 0.62 | 44 | 0.35 | 0.73 | 0.09 |
| Quartile 3 | ||||||||
| Median household income (dollars) | 76,926.23 | 71,648 | 61,548.00 | 86,058.00 | 43 | 39,207 | 250,001 | 30,767.51 |
| Median rent (dollars) | 1,620.84 | 1,550 | 1,392.00 | 1,700.00 | 43 | 1,186 | 3,501 | 395.04 |
| Unemployed (%) | 5.39 | 5.43 | 4.42 | 6.18 | 43 | 3.15 | 8.04 | 1.07 |
| Living below 150% poverty line (%) | 20.43 | 19.95 | 13.92 | 25.63 | 43 | 5.49 | 39.13 | 8.02 |
| Working class (%) | 54.25 | 56.09 | 48.97 | 61.50 | 43 | 24.87 | 86.58 | 13.17 |
| Education index | 1,399.53 | 1,406.12 | 1,376.73 | 1,437.56 | 43 | 1,211.08 | 1,564.23 | 66.88 |
| >1 occupants per room | 1,649.23 | 868 | 440.00 | 2,376.00 | 43 | 34 | 8,451 | 1,835.46 |
| White residents (%) | 51.84 | 52.71 | 37.66 | 70.92 | 43 | 2.32 | 93.78 | 24.28 |
| Hispanic residents (%) | 18.99 | 14.91 | 9.58 | 22.70 | 43 | 4.9 | 75.49 | 13.55 |
| Total tests/population (%) | 0.95 | 0.94 | 0.73 | 1.14 | 43 | 0.45 | 2.39 | 0.33 |
| Positive tests/total tests (%) | 0.53 | 0.51 | 0.47 | 0.58 | 43 | 0.38 | 0.77 | 0.08 |
| Quartile 4 | ||||||||
| Median household income (dollars) | 115,455.7 | 110,625 | 91,936.00 | 127,506.00 | 45 | 71,225 | 246,813 | 33,086.37 |
| Median rent (dollars) | 2,194.69 | 2,174 | 1,730.00 | 2,472.00 | 45 | 607.14 | 3,394 | 630.37 |
| Unemployed (%) | 4.01 | 4 | 3.29 | 4.79 | 45 | 0.61 | 6.68 | 1.27 |
| Living below 150% poverty line (%) | 13.16 | 11.93 | 8.96 | 17.38 | 45 | 3.14 | 36.91 | 6.18 |
| Working class (%) | 34.06 | 28.72 | 26.16 | 41.11 | 45 | 19.98 | 68.31 | 11.37 |
| Education index | 1,508.14 | 1,522.96 | 1,476.59 | 1,561.51 | 45 | 1,353.02 | 1,591.87 | 63.14 |
| >1 occupants per room | 834.64 | 665 | 334.00 | 1,064.00 | 45 | 25 | 4,071 | 747.75 |
| White residents (%) | 72 | 73.94 | 63.14 | 81.67 | 45 | 38.86 | 95.42 | 13.09 |
| Hispanic residents (%) | 12.18 | 10.9 | 6.94 | 15.12 | 45 | 1.12 | 44.27 | 7.26 |
| Total tests/population (%)a | 0.96 | 0.94 | 0.75 | 1.08 | 45 | 0.53 | 1.75 | 0.28 |
| Positive tests/total tests (%) | 0.42 | 0.42 | 0.37 | 0.46 | 45 | 0.25 | 0.63 | 0.08 |
Note: The education index was calculated on the population ≥25 years and is a weighted combination of the percentage of high school graduates, high school only, and more than high school, with a greater value indicating higher educational attainment.
Total tests/population (%): Test per 100 persons.
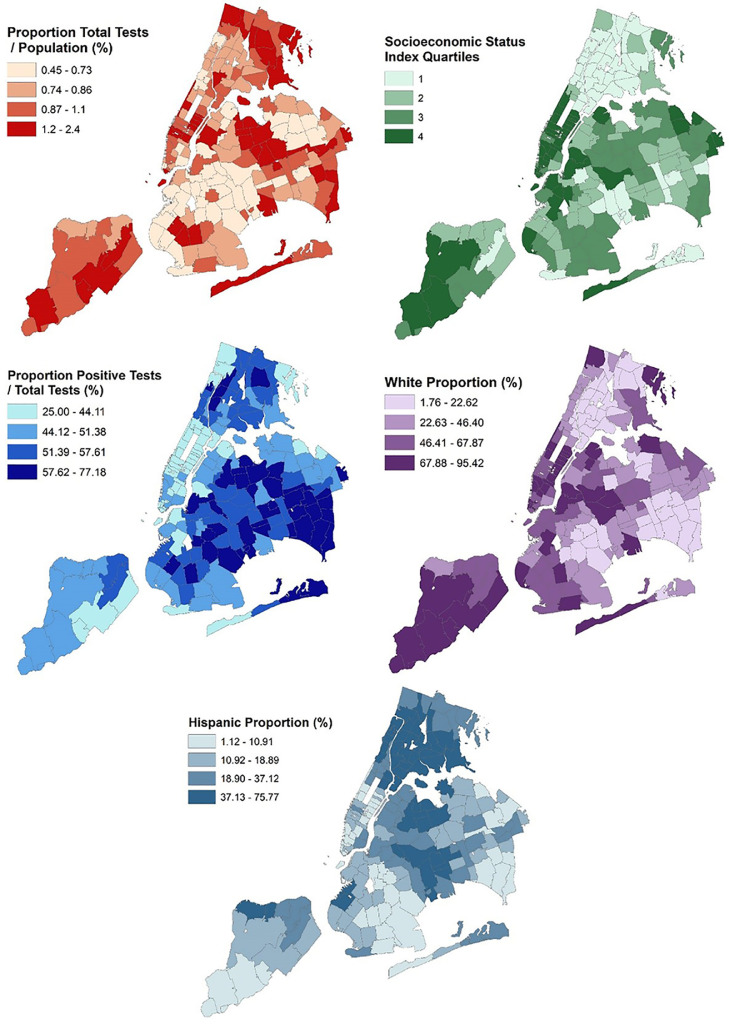
There are 177 ZCTAs in NYC. The ratio of total tests to population and positive tests to total tests performed were mapped according to each ZCTA (Figure 1 ). Clusters of a low proportion of total tests/population were present in areas of northern Brooklyn, and clusters of a high ratio of total tests relative to population were identified throughout midtown Manhattan and an area in central Queens (Appendix Figure 1, available online). Cluster and outlier analysis using local Moran's I revealed clusters of a high ratio of positive tests to total tests in areas of Brooklyn and Queens and clusters of a low ratio of positive tests to total tests throughout Manhattan and the waterfront of Queens and Brooklyn adjacent to Manhattan.
Figure 1.
Spatial distribution of the proportion of total tests/population (%) (top-left), positive tests/total tests (%) (middle-left), SES index (top-right), proportion white race alone (bottom-right), and Hispanic proportion (bottom-middle) across NYC. Proportion total tests/population (%) displayed in hundreds of residents.
NYC, New York City.
The number of total tests significantly increased with the increasing proportion of white residents in the ZCTA (β=0.004, SE=0.001, p=0.0032), whereas the proportion of Hispanic residents (β=0.0008, SE=0.001, p=0.5617) and the SES index score (β= −0.0007, SE=0.001, p=0.6077) were not statistically significant (Table 2 ). The ratio of positive tests to total tests significantly decreased with the increasing proportion of white residents in the ZCTA (β= −0.003, SE=0.0006, p<0.001) and the increasing SES index score (β= −0.0016, SE=0.0007, p=0.0159).
Table 2.
Predictors of Total Number of Tests and Positive Tests
| Outcome | Total testsa |
Positive tests/total testsb |
||||
|---|---|---|---|---|---|---|
| β | SE | p-value | β | SE | p-value | |
| Intercept | ‒4.92 | 0.06 | <0.0001 | 58.94 | 0.05 | <0.0001 |
| White alone proportion | 0.004 | 0.001 | 0.0032 | ‒0.003 | 0.0006 | <0.001 |
| Hispanic proportion | 0.0008 | 0.001 | 0.5617 | ‒0.00001 | 0.0007 | 0.9482 |
| SES indexc | ‒0.0007 | 0.001 | 0.6077 | ‒0.0016 | 0.0007 | 0.0159 |
Note: Models were adjusted for all variables listed.
Poisson regression performed, adjusted with a Pearson scaling factor to correct for overdispersion, log(population) used as an offset.
Poisson regression performed.
The SES index was constructed from principal component analysis of 2018 American Community Survey estimates of median household income in the past 12 months, median gross rent, percent living below 150% of the poverty line, education, percent working class, percent unemployed, >1 occupants per room. The education index was calculated on the population ≥25 years and is a weighted combination of the percentage high school graduate, high school only, and more than high school, with a greater value indicating higher educational attainment.
DISCUSSION
Both the number of tests for COVID-19, accounting for the ZCTA population, and the proportion of positive testing vary by ZCTA within NYC, with racial composition and SES being significant predictors of testing volume and positivity. These results show that more tests were performed in areas with an increasingly white racial composition. Conversely, the highest proportion of positive tests were recorded in nonwhite neighborhoods and in areas defined by a lower SES.
NYC has quickly become the epicenter of the COVID-19 pandemic, and the staggering number of infected residents, along with the complete shutdown of all services, have exacerbated existing social and racial disparities in healthcare access and utilization. This analysis integrates with data showing racial disparities in COVID-19 cases and deaths, both nationally and within NYC.6 Although mortality data from COVID-19 have not been released to date by ZCTA in NYC, data have been released by borough of residence.10 Among confirmed COVID-19 cases, mortality rates are higher in Queens (31.9%), Brooklyn (28.4%), and the Bronx (22.9%) than in Manhattan (11.5%) and Staten Island (5.3%). These patterns of higher mortality correspond to areas that were shown to have proportionately more positive test results and less testing in general. This analysis shows that working-class populations in lower-SES areas are less likely to receive tests and more likely to be positive when tested. This population inherently includes essential workers, municipal transportation workers, factory workers, and those working in healthcare settings, all of which are especially vulnerable to COVID-19. One explanation is that residents of low-SES metropolitan areas are more likely to be tested when symptomatic given that they were more likely to have a positive test result. Symptomatic testing may identify more advanced cases, thus contributing to the high mortality rates, while at the same time not mitigating the diffusion of the infection in the community. This phenomenon has serious implications in areas such as Queens and Brooklyn, where a large number of healthcare and service workers work and reside. Additionally, low-SES residents may be essential workers, with limited time to devote to be tested or limited access to transportation to testing sites. Similar barriers have been observed in other settings such as cancer screening.11, 12, 13
Widespread COVID-19 testing has been identified as a crucial step in reopening the economy.14 , 15 In fact, testing is necessary to track positive cases, identify asymptomatic transmitters, and trace contacts in the community. When widely available, saliva-based testing offers an alternative to nasopharyngeal swabs that may be more practical and more sensitive (Wyllie AL, PhD, unpublished data, January 2020). However, additional barriers to testing include access and cost. To remove barriers to testing, New York State prohibited cost sharing on private insurance companies for COVID-19 testing on March 2, 2020.16 Additionally, House Resolution (HR) 6201 dated March 18, 2020 enacted free COVID-19 testing and removed costs for traveling to be tested.17 However, this bill does not prevent against surprise charges. Still, the number of people who need to be tested outnumbers the available test kits, nasal swabs, and other necessary equipment for conducting the test. Despite recommendations for widespread testing and the potential option for free testing, this does not ensure that the entire population will be tested, nor does it guarantee the quantity and quality of testing kits necessary for widespread testing.18 If the disparities identified in this analysis continue to persist, this necessary testing may not be administered to an adequate degree in all ZCTAs within NYC, hindering overall efforts to prevent a second outbreak of COVID-19 while putting thousands at risk of infection.
Limitations
One limitation of this analysis is that Census data potentially under represent noncitizens, which would influence the SES index measures and the racial composition of each ZCTA. This highlights the fact that the provisions of HR 6201 do not extend to noncitizens, and thus an already vulnerable population would not have access to free testing. There are no assurances that undocumented immigrants would have any protections if they seek to be tested. In addition, it is important to consider that the data used in these analyses are not individual-level but instead aggregate ZCTA-level data, which limits the ability to draw individual-level conclusions. For instance, the authors cannot comment on the interaction between being nonwhite and of low SES on the likelihood of testing or of a positive test, knowledge that would help to identify the most vulnerable populations. This study was ecological in nature and there are more individual-level factors that may influence COVID-19 testing that could not be taken into account here. Taken together, these results suggest that testing was not planned or implemented according to needs in NYC, and that testing policies may need to be revisited and more resources devoted to lower-SES communities to minimize loss of life, retain the ability of essential working-class individuals to provide vital services and contribute to the economy, and eventually stop this pandemic.
CONCLUSIONS
This analysis identifies disparities in those being tested and suggests a gap in COVID-19 response policy, as well as the need for widespread testing and public health outreach to the most vulnerable populations of NYC. This is essential to stop the pandemic and reopen the economy in NYC. Future studies should focus on the reasons why these disparities in testing occurred; focus groups among residents of low-SES areas could help define if barriers to testing exist and generate suggestions on how to address such obstacles.
ACKNOWLEDGMENTS
No funding was received for this work. The corresponding author had full access to all the data in the study.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2020.06.005.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.WHO. Coronavirus disease (COVID-19) Situation Report - 154. Geneva, Switzerland: WHO.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200622-covid-19-sitrep-154.pdf?sfvrsn=d0249d8d_2. Published June 22, 2020. Accessed June 22, 2020.
- 2.NYC coronavirus disease 2019 (COVID-19) data. New York City Department of Health. https://github.com/nychealth/coronavirus-data. Updated daily. Accessed June 22, 2020.
- 3.Overview of testing for SARS-CoV-2. Centers for Disease Control and Prevention (CDC). www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html. Updated July 2, 2020. Accessed April 13, 2020.
- 4.Shear MD, Goodnough A, Kaplan S, Fink S, Thomas K, Weiland N. The lost month: how a failure to test blinded the U.S. to Covid-19. New York Times. March 28, 2020 www.nytimes.com/2020/03/28/us/testing-coronavirus-pandemic.html. Updated April 1, 2020. Accessed April 13, 2020. [Google Scholar]
- 5.Testing for COVID-19. Centers for Disease Control and Prevention (CDC).www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html. Updated June 24, 2020. Accessed April 13, 2020.
- 6.New York City Department of Health. Age adjusted rate of fatal lab confirmed COVID-19 cases per 100,000 by race/ethnicity group. New York, NY: New York City Department of Health.www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-04082020-1.pdf. Published April 6, 2020. Accessed April 13, 2020.
- 7.2020 poverty guidelines for the 48 contiguous states and the District of Columbia. HHS.https://aspe.hhs.gov/poverty-guidelines. Updated January 8, 2020. Accessed May 27, 2020.
- 8.American Community Survey. 2018 American Community Survey 5-Year estimates. U.S. Census Bureau. https://data.census.gov/cedsci/. Updated January 23, 2020. Accessed April 28, 2020.
- 9.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–711. doi: 10.1023/a:1011240019516. [DOI] [PubMed] [Google Scholar]
- 10.New York City Department of Health. Confirmed and probable COVID-19 deaths. New York, NY: New York City Department of Health.www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-confirmed-probable-daily-04142020.pdf. Published April 13, 2020. Accessed April 14, 2020.
- 11.Liss DT, Baker DW. Understanding current racial/ethnic disparities in colorectal cancer screening in the United States: the contribution of socioeconomic status and access to care. Am J Prev Med. 2014;46(3):228–236. doi: 10.1016/j.amepre.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Jadav S, Rajan SS, Abughosh S, Sansgiry SS. The role of socioeconomic status and health care access in breast cancer screening compliance among Hispanics. J Public Health Manag Pract. 2015;21(5):467–476. doi: 10.1097/PHH.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 13.Fang CY, Ragin CC. Addressing disparities in cancer screening among U.S. immigrants: progress and opportunities. Cancer Prev Res (Phila) 2020;13(3):253–260. doi: 10.1158/1940-6207.CAPR-19-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gottlieb S, Rivers C, McClellan MB, Silvis L, Watson C. National coronavirus response: a road map to reopening. Washington, DC: American Enterprise Institute.www.aei.org/wp-content/uploads/2020/03/National-Coronavirus-Response-a-Road-Map-to-Recovering-2.pdf. Published March 28, 2020. Accessed April 10, 2020.
- 15.Studdert DM, Hall MA. Disease control, civil liberties, and mass testing - calibrating restrictions during the Covid-19 pandemic. N Engl J Med. 2020;382(2):102–104. doi: 10.1056/nejmp2007637. [DOI] [PubMed] [Google Scholar]
- 16.Governor's Press Office Governor Cuomo announces new directive requiring New York insurers to waive cost-sharing for coronavirus testing. New York State Governor's Press Office. March 2, 2020 www.governor.ny.gov/news/governor-cuomo-announces-new-directive-requiring-new-york-insurers-waive-cost-sharing [Google Scholar]
- 17.House resolution 6201. Families First Coronavirus Response Act. Congress.gov. www.congress.gov/bill/116th-congress/house-bill/6201. Updated March 18, 2020. Accessed April 13, 2020.
- 18.Parmet WE, Sinha MS. Covid-19—the law and limits of quarantine. N Engl J Med. 2020;382(15):e28. doi: 10.1056/NEJMp2004211. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.