Abstract
The purpose of this descriptive study was to, from the perspective of adult people with epilepsy (PWE) and caregivers of PWE, explore the effects of the current pandemic and resulting societal changes on epilepsy self-management. Ninety-four respondents completed a mixed-methods quantitative and qualitative survey focused on their epilepsy self-management experiences during the coronavirus disease-19 (COVID-19) pandemic.
Respondents noted significant disruption in epilepsy self-management. Lack of ability to obtain medications or see epilepsy providers, as well as increased stress, social isolation, and changes in routine were all reported as troublesome, and more than one-third of the sample reported an increase in seizure frequency since the onset of the pandemic. Suggestions are given regarding how to support PWE during future COVID-19 outbreaks and to better prepare PWE and their caregivers for any life-altering events, such as a pandemic, with robust self-management skills that will allow them to maintain the highest level of function possible.
Keywords: Epilepsy self-management, COVID-19, Pandemic, Nursing research
Highlights
-
•
The COVID-19 pandemic puts people with epilepsy at risk because of lack of normal access to healthcare.
-
•
People with epilepsy and caregivers report significant disruptions in epilepsy self-management.
-
•
Obtaining medications, communicating with doctors, and routine changes are problematic.
-
•
Any major change in daily life can threaten to decay self-management.
-
•
Robust self-management skills should be prioritized for people with epilepsy.
1. Introduction
The 2020 novel coronavirus SARS-CoV-2 and subsequent coronavirus disease-19 (COVID-19) pandemic has caused unprecedented societal disruption worldwide. Social distancing mandates combined with extreme stress on the United States (US) healthcare system have rendered daily life in the US nearly unrecognizable. While most Americans' daily lives and routines have markedly changed during the pandemic, Americans with chronic disease, including epilepsy, are at unique risk for health-related disruptions. Both Federal and state mandates put in place to quell the spread of COVID-19, and the risk of contracting the virus, have potentially created unique barriers for those with epilepsy.
First reported in China, COVID-19 is caused by a novel virus that leads to respiratory illness in varying degrees of severity, from asymptomatic to respiratory failure and death. Nearly 3 million cases of COVID-19 have been confirmed globally, with the US currently having the most at nearly 1 million confirmed cases; nearly 200,000 people [1], including more than 50,000 Americans [2], have died from COVID-19. Given its novelty, COVID-19 has been especially difficult to contain, with public health experts scrambling to determine details about the virus' spread and ability to live on surfaces. The unknown aspects of the highly contagious virus' spread and effective treatment have caused Federal- and state-level government action on a scale not seen since some states enacted social distancing during the 1918 Spanish Flu pandemic [3].
President Trump has ordered the nation to follow drastic social distancing guidelines, which include staying at least six feet apart from others outside of family, only leaving the house for essential purposes, and working from home whenever possible. Universities and schools across the nation have halted in-person classes, transitioning to online learning, and 80% of Americans are under governor-enacted lockdown orders. A majority of states have restricted gatherings and prohibited all but essential travel outside the home; some states have formal “shelter-in-place” orders in effect [4]. Even in states beginning to open, daily environments are far from normal.
In the midst of a personal protective equipment and ventilator shortage, governors have halted nonemergent surgeries and procedures, and many health clinics are closed or only seeing patients in the event of an emergency [5]. These necessary precautions have resulted in not only economic collapse but also extreme alterations in a healthcare system on which 3 million Americans rely for treatment and management of their epilepsy, a condition which the Centers for Disease Control and Prevention (CDC) has indicated increases the risk for serious COVID-19 infection [6]. In the midst of a healthcare crisis focused on preventing and treating COVID-19, another question arises—how does the pandemic affect the health of patients not affected by COVID-19, and especially those managing chronic diseases like epilepsy? This question is especially important to consider given that the nation will likely have to engage in additional rounds of social distancing until a vaccine for COVID-19 is available [7].
Epilepsy self-management is key to achievement of epilepsy-related outcomes [8] and refers to a patient managing the treatments and day-to-day lifestyle changes associated with epilepsy. Specifically, epilepsy self-management is the process during which patients incorporate multidimensional strategies that meet their self-identified needs to manage and cope with epilepsy within the context of their daily living; successful management of both functioning in day-to-day life along with management of chronic illness requires the individual to continually monitor health and functional status and take appropriate actions during acute phases, and this management often involves a familial caregiver [9]. The COVID-19 pandemic creates a rare opportunity to explore how epilepsy self-management is altered when societal, economic, and healthcare structures do not exist in their usual forms in the US. The purpose of this descriptive study was to, from the perspective of adult people with epilepsy (PWE) and caregivers of PWE, explore the effects of the current pandemic and resulting societal changes on epilepsy self-management. Specifically, we sought to explore how mandated isolation, social distancing orders, closure of many businesses, and COVID-19 infections have affected PWE and their caregivers' ability to self-manage (control seizures, access medications, manage triggers, and communicate with providers). Further, we explored the frequency and severity of affective symptoms, as well as other PWE- and caregiver-identified difficulties that have arisen during the pandemic.
2. Materials and methods
The study was submitted to the Indiana University IRB and deemed exempt. Using social media, an advertisement for the survey was shared via various epilepsy-related Facebook pages and via Twitter with the appropriate hashtags to render it searchable (#COVID-19, #epilepsy, #pandemic, and #research). Organic sharing of the advertisement from members of these groups also occurred. All participants self-referred to the study via the link embedded in the online advertisement.
Inclusion criteria were the following: age 18 years or older, a person diagnosed with epilepsy taking antiseizure medication OR the caregiver of a child/loved one with epilepsy currently taking antiseizure medication for epilepsy, fluent in English, reliable access to the Internet, and currently living in the US. Participants lacking these criteria were excluded and automatically directed to the end of the survey. The survey included a total of 65 questions, 50 of which were relevant to this manuscript, and included questions related to demographics, perceived changes in epilepsy self-management, social distancing, and affective symptoms since the pandemic began. The data were collected over a three-day period, from March 27 to March 30, 2020. During this three day period, 31 states were under some version of stay-at-home orders.
Using SPSS version 26, descriptive statistics were run on all quantitative variables. Paired t-tests were used to detect statistically significant differences on items that involved respondents providing a pre- and postpandemic score. Qualitative comments were analyzed using traditional content analysis.
3. Results
3.1. Demographics
The survey was accessed by 112 people. Five surveys were discarded because of high recaptcha scores on Qualtrics, indicating high likelihood of bot completion. These five surveys were manually reviewed and found to contain unreliable data. Thus, 107 completed the survey, and 94 participants completed every single survey item. The final sample size was thus 94. Table 1 displays the demographics of the sample. The gender of the sample was equally split, with 47 men and 47 women. The average age of respondents was 36 years (range: 19 to 88). There were 78 PWE and 16 caregivers. Participants were White (80%), African American (9%), American Indian/Alaskan Native (4%), Native Hawaiian or Pacific Islander (4%), Asian (2%), or Other (1%). Participants resided in the Midwest (30%), Northeast (19%), Mid-Atlantic (18%), West (17%), Northwest (7%), Southeast (6%), and Southwest (3%) regions of the US. Sixty respondents indicated that they or their loved ones with epilepsy had not been tested for COVID-19, 16 of whom reported that they had current symptoms (fever, cough, or shortness of breath) that they believed could have been contributed to COVID-19. Thirty-one participants reported that they or their loved ones with epilepsy had been tested for COVID-19; of these, 7 reported that they (or their loved one with epilepsy) were COVID-19 positive, while 24 reported negative COVID-19 testing results. Sixty-nine percent of the sample (n = 65) indicated that they were aware that the CDC has named PWE as high risk for serious COVID-19 infections, and the majority (82%) learned this from the Epilepsy Foundation social media accounts. No demographic variables were statistically significantly correlated with other measures.
Table 1.
Demographic information, N = 94.
| Sex | – Male n = 47 (50%) – Female n = 47 (50%) |
| Age | Mean = 36, range: 19–88 |
| Caregiver/PWE | – Caregiver n = 16 (17%) – PWE n = 78 (83%) |
| Ethnicity | – White n = 75 (80%) – African American n = 9 (9%) – American Indian/Alaskan native n = 4 (4%) – Native Hawaiian/Pacific Islander n = 3 (4%) – Asian n = 2 (2%) – Other n = 1 (1%) |
| Area of United States | – Midwest n = 28 (30%) – Northeast n = 18 (19%) – Mid-Atlantic n = 17 (18%) – West n = 16 (17%) – Northwest n = 6 (7%) – Southeast n = 6 (6%) – Southwest n = 3 (3%) |
| Annual income | – <$10,000 n = 5 (5%) – $10K–$19,999 n = 6 (6%) – $20K–$29,999 n = 2 (3%) – $30K–$39,999 n = 10 (11%) – $40K–$49,999 n = 15 (16%) – $50K–$59,999 n = 12 (13%) – $60K–$69,999 n = 7 (7%) – $70K–$79,999 n = 13 (14%) – $80K–$89,999 n = 7 (7%) – $90K–$99,999 n = 3 (3%) – $100K–$149,999 n = 11(12%) – >$150,000 n = 3 (3%) |
| Employment status | – Employed full-time n = 72 (77%) – Employed part-time n = 13 (14%) – Unemployed/looking for work n = 2 (2%) – Unemployed/not looking for work n = 2 (2%) – Student n = 3 (3%) – Disability n = 2 (2%) |
| Education | – High school graduate n = 4 (4%) – Some college n = 7 (7%) – 2-Year college degree n = 10 (10%) – 4-Year college degree n = 60 (65%) – Master's degree n = 12 (13%) – Doctoral degree n = 1 (1%) |
| Relationship status | – Married n = 70 (74%) – Widowed n = 3 (3%) – Divorced n = 10 (10%) – Separated n = 1 (1%) – Single/never married n = 5 (6%) – Partnered or dating but not married n = 5 (6%) |
| Seizure frequency | – Well-controlled, periods of seizure freedom one year or greater n = 28 (30%) – Somewhat well-controlled, with periods of seizure freedom six months to one year n = 47 (50%) – Uncontrolled, with periods of seizure freedom three to six months n = 10 (11%) – Very uncontrolled, with periods of seizure freedom less than three months n = 6 (6%) – Extremely uncontrolled, with period of seizure freedom less than one week n = 3 (3%) |
3.2. Social distancing
Respondents were asked to describe the degree to which they have been practicing social distancing. On a scale of 0–10, with 0 being not practicing social distancing at all and 10 practicing social distancing very much, respondents' ratings averaged 8.03 (standard deviation (SD): 1.28, range: 4–10). Seventy-seven respondents indicated that they were struggling to practice social distancing; 40 participants reported that having to report to work for an essential job interfered with their ability to practice social distancing. Other interferences with social distances included having to work in order to make ends meet (n = 26), caring for others outside the home (n = 22), and having social engagements they were unable or unwilling to miss (n = 14). Table 2 includes additional results related to respondents' experiences with social distancing.
Table 2.
Additional social distancing questions, N = 94.
| To what degree does epilepsy affect your decision to social distance? (scale 1–10) | Mean: 7.48, SD 1.99, range: 1–10 |
| Compared to other people you know, would you say that you began to engage in social distancing early on in this pandemic or later? (scale 1–10, 1 = much earlier, 10 = much later) | Mean: 5.83, SD 2.89, range: 1–10 |
| Compared to other people you know, would you say you are social distancing more or less than they are? (scale 1–10, 1 = much less, 10 = much more) | Mean: 7.37, SD 1.34, range: 4–10 |
| How likely are you to continue to follow lockdown and social distancing orders for the duration of the pandemic, even if it lasts for months? (scale 1–10, 1 = not at all likely, 10 = very likely) | Mean: 7.58, SD 1.42, range: 2–10 |
3.3. Epilepsy- and self-management-related changes
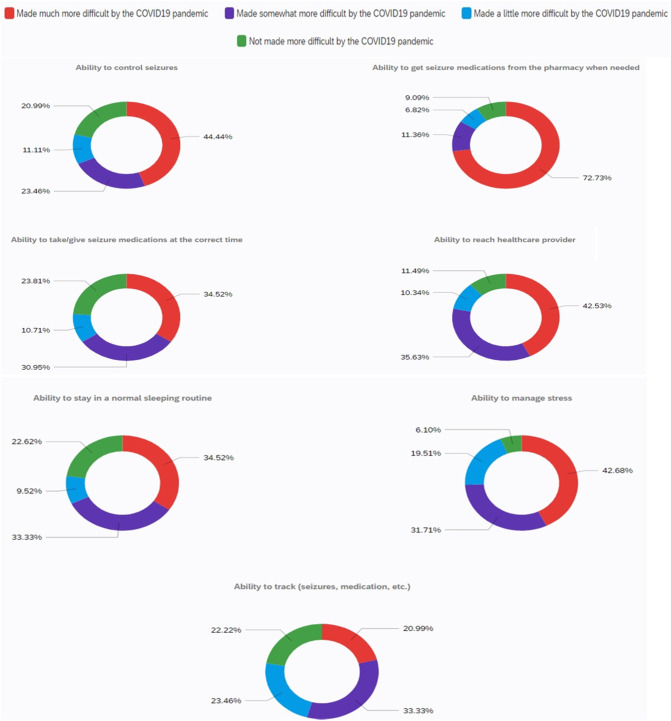
We asked various questions aimed at determining how respondents' epilepsy and epilepsy self-management have been affected by the pandemic. More than one-third (35%, n = 33) of respondents indicated that they or their loved ones have experienced increased seizure frequency since pandemic onset. Of those who indicated worsening seizures during the pandemic, on a scale of 0–10 with 0 being seizure frequency has not increased at all and 10 being seizure frequency has increased very much, the mean score was 6.88 (SD: 0.98, range: 3–8). Respondents were asked to rank the degree to which several epilepsy self-management-related activities (ability to control seizures, ability to get seizure medication from pharmacy when needed, ability to reach healthcare provider, ability to take/give seizure medication at the correct time, ability to manage stress, ability to stay in a normal sleeping routine, and ability to track seizures and medication) were affected by the pandemic. Ability to get medications from the pharmacy was most affected by the pandemic, with 73% of the sample indicating that this area of epilepsy self-management was made “much more difficult” by the pandemic. More than 40% of the sample indicated that managing seizures, managing stress, and reaching their epilepsy healthcare provider were made “much more difficult” by the pandemic. Fig. 1 displays more detailed results of respondents' rankings in response to this question.
Fig. 1.
Self-management difficulty rankings.
Respondents were asked to rate the degree to which they feel confident that they could get timely help from their/their loved one's epilepsy provider, hospital, and pharmacy using a 0–10 scale, with 0 being not at all confident and 10 being very confident. Respondents were least confident in their ability to get timely help for epilepsy at a hospital (mean = 5.19, SD: 2.69), followed by their confidence in receiving help from pharmacies (mean = 5.89, SD: 2.65). Respondents had the highest level of confidence in receiving help from epilepsy providers (mean = 5.91, SD: 2.44), resulting in the highest level of confidence being just above “somewhat confident.”
3.4. Affective symptoms
Participants were asked to describe the degree to which their support networks, feelings of isolation, and anxiety had changed as compared with before the pandemic. Respondents rated the strength of their social support networks using a 10-point Likert scale (0 = not at all strong, 10 = very strong) before and after the pandemic, and there was a statistically significant difference in pre- and postpandemic social support network strength (mean score pre = 7.52; mean score post = 7.41; t = 3.02, p < .003). The same was true for perceived isolation pre- and postpandemic (mean score pre = 6.27; mean score post = 7.18; t = 4.12, p = .000). Using the PROMIS anxiety scale [10], respondents reported statistically significant higher levels of anxiety postpandemic than prepandemic (mean score pre = 22.2; mean score post = 26.7; t = − 6.86; p = .000). Asked to rate how they were coping with the current pandemic on a scale of 0–10, with 0 being not at all and 10 being very well, the mean score was 7.08 (SD: 1.89; range: 0–10).
3.5. Qualitative comments
Respondents were asked to write free text regarding any other thoughts they had about how the COVID-19 pandemic was affecting their or their loved one's epilepsy. Forty-five respondents (35 PWE and 10 caregivers) left remarks.
3.5.1. Difficulties with social distancing
Many (n = 23) respondents described how current responsibilities interfered with social distancing. One participant stated, “I live alone, so grocery shopping and pharmacy are all on me.” Others reported having to continue to report to work or other volunteer duties, which threatened their ability to social distance. “I work at a post office, and sometimes we are not six feet apart” wrote one participant, while another stated, “I work part time at a church with a food pantry which is essential… While a lot of practices have been put in place to help social distance while doing this, there is still some interaction. I also do not drive due to my seizures so I need to rely on others for transportation, which has limited my ability to social distance.” Another participant remarked, “I have to report to work where 50 people are daily.” Others noted that the ability to work from home has been very helpful in social distancing, “With the ability to telework 100%… we were able to prepare early by stocking food supplies to limit trips out of the house and obtain 90 day supplies of antiseizure meds, and critical vitamins and minerals for health stability. If we were not able to telework we would suffer with caring for our daughter and providing a safe situation for seizure monitoring.”
3.5.2. Impact on seizure frequency and severity
Nine of 33 respondents who indicated a worsening of seizure frequency and/or severity left comments about how the pandemic has directly affected their seizure frequency and severity. According to one respondent, “I'm having a lot more complex partial seizures. This week I had one every day, they usually only occur 1 to 3 times per month. And I had a tonic clonic that was almost 8 minutes & the vns didn't seem to help like it usually does.” Caregivers reported similar seizure increases, with one stating, “He has had more seizures in the past week…since all this started.” Others responded with the exact numbers of seizures they have experienced since the onset of the pandemic, with respondents reporting an increase by 3 (two respondents), 4 (two respondents), 5, and 10 (three respondents), seizures beyond their normal seizure frequency since pandemic onset.
3.5.3. Changes in routine affecting self-management
Some respondents reported changes that directly affected their ability to self-manage their epilepsy or that of their loved ones. Respondents reported difficulty with maintaining a normal sleep routine, managing stress, obtaining prescriptions, and reaching healthcare providers. As one respondent explained, “It is more difficult to obtain medications from the pharmacy due to reduced hours, living alone and not having adequate transportation without ride sharing (which has been greatly reduced in this area currently). Doctors are not accepting appointments except for sick patients, so follow ups are nonexistent currently. There is added stress from work, which also makes a normal sleep routine more difficult. All of these things ultimately lead to poor seizure control over time.” Another respondent noted, “With social distancing it has been more difficult to get the medications when needed. Stress has also been a factor just worrying about if you were to have a seizure that we would need to go to the hospital and being exposed there.” Another respondent found that family members being home most of the time also affected self-management. “It's changed my daily routine & that of the people I live with (for instance my brother being out of school) so my sleep has changed. He's a teen & sees this as a longer summer vacation, so he's staying up late & keeping me up. Stress has been the hardest.” One respondent explained the inability to get epilepsy-related questions answered during this time, stating “You cannot get help for things that are not life or death right now, including small seizures or questions about medications…it's not clear when or if I am allowed to call them with a question if it's not an emergency.” Similarly, a caregiver shared, “I feel guilty calling to ask anything…we have only been dealing with this about 7 months and I still have tons of questions but am afraid to ask right now because I know everyone else has it far worse.”
3.5.4. Fear
Several respondents spoke of being fearful of contracting COVID-19 or having care rationed in the event they or their loved ones needed hospitalization related to seizures. As one respondent explained, “I dare not go to the hospital for regular testing because I am worried that the hospital will take in many patients infected with the virus. I also dare not go to the pharmacy, which makes me feel panic.” One respondent with epilepsy explained fear regarding COVID-19's effect on epilepsy, stating, “[I have] fear of getting the virus. I have seizure clusters with fevers so I'm worried what will happen if I get it. Hearing some kind of comforting word from a neuro, that I won't die if I get it would be helpful.” A caregiver of a child with epilepsy noted being concerned about rationing of ventilators, stating, “Worried that if she needs any kind of hospital care she will be less likely to receive a ventilator — not likely if she get Co-Vid to get a vent…her cognitive function is greatly delayed and if care is rationed she is in a group that will be at the bottom of the list. That worries me greatly.”
4. Discussion
Our results indicate that the ongoing COVID-19 pandemic has affected the ability of PWE and caregivers of PWE to effectively self-manage epilepsy in many ways. While there is no prior pandemic literature to which we can compare our results, it is not surprising that, in a time during which our typical social structure and healthcare system are upended, PWE are especially affected.
A large portion of the sample reported difficulties following social distancing guidelines. While there is no published survey of the general public's difficulties with social distancing, these things making social distancing difficult to achieve (need to go to work, caring for others outside home) for this sample are likely not specific to PWE or their caregivers. However, respondents also reported that they felt they began engaging in social distancing earlier than others they know, and that they were practicing social distancing more than others around them (Table 2). The sample's early adoption and more strict adherence to social distancing guidelines may be due to the presence of epilepsy, as respondents indicated that their or their loved one's epilepsy was a major factor in their decision to social distance, and nearly 70% of respondents indicated that they knew that the CDC has named PWE as a high-risk group for serious COVID-19 infection. This is an encouraging result—the CDC's classifications of high-risk groups appears to have been well-disseminated to this sample, and they are also taking steps (social distancing) to prevent COVID-19 given their or their loved one's high-risk COVID-19 infection status. Most respondents (82%) learned of the CDC classification via the Epilepsy Foundation's social media, indicating that sharing of CDC guidelines in this manner is effective and should be repeated, and even amplified, in the event of future COVID-19 outbreaks. Because some respondents knew this information but were unsure of its full meaning (worry about COVID-19 meaning automatic death for someone with epilepsy), it is important to consider addressing details of what it means to be on the CDC's high-risk list.
Our results demonstrate a clear disruption in epilepsy self-management during the pandemic, in many cases leading to increased seizure frequency or a deterioration in self-management that puts PWE at higher-than-normal risk for seizures. In response to both quantitative and qualitative questions, respondents indicated problems managing epilepsy in large part due to difficulty obtaining medications from pharmacies, securing appointments with epilepsy providers, and disruption in normal routine. These results suggest that the necessary changes accompanying a pandemic like COVID-19 threaten the management of epilepsy, and likely other conditions as well. Ahead of the next round of social distancing or a new pandemic entirely, it is important to put in place structures that will ease patients' ability to access medications and providers. Physicians and other providers caring for PWE should consider 3-month prescriptions for antiseizure drugs, at least until a vaccine is widely available. From a more system-level perspective, there is a need to devise a system that will allow people who require medication for chronic diseases, including epilepsy, to access their medications in the event of more social distancing or another outbreak. Prescription mail delivery (especially for PWE who lack transportation) and no contact drive-thru service are potential options, though respondents in this sample also noted that restricted pharmacy hours contributed to their difficulty in getting their medications, while others who cannot drive may struggle to find transportation to the pharmacy in a lockdown. State and Federal funding may need to be considered to allow pharmacies to continue to offer services that will prevent disruption of medications for PWE and others with chronic conditions. Regarding lack of access to epilepsy providers, the use of robust video health visit platforms will be most helpful and will hopefully already exist during subsequent outbreaks; the providers of respondents in this sample required time to set up these systems. As the pandemic wanes, epilepsy clinics should consider prioritizing the maintenance of these virtual visit platforms, including helping patients and caregivers to feel comfortable using them in preparation for the next wave. A downside of virtual video visits is that a strong internet connection is required. Given that virtual health visits have led to higher satisfaction and lower no-show rates, this may be an opportunity to make them more mainstream for maintenance epilepsy care [11].
However, those in rural communities who may have inferior internet, or none at all, may not be able to participate in virtual visits. While Internet companies have offered to connect low-income families with free Internet during the pandemic [12], some live in areas where broadband is not available. In these cases, the use of telehealth (visits by telephone) could be a more appropriate and reliable option. Most importantly, practices must communicate clearly with patients and caregivers regarding the plan for scheduling a visit, getting questions answered, etc., as in our sample, a lack of understanding of how to reach providers, and whether a question was “urgent enough” to call appeared to contribute to issues with provider communication.
Respondents' reports of altered and poorer quality of sleep since the onset of the pandemic is concerning given that lack of sleep is a known seizure trigger for many PWE [[13], [14], [15], [16]]. In preparation for more COVID-19 outbreaks and subsequent social distancing and changes in the healthcare system, epilepsy physicians and other providers should prioritize self-management skill-building, particularly regarding sleep, with their patients and caregivers, which could be done via nurses, including Advanced Practice Nurses. Web-based self-management interventions, such as WebEASE [17], which provides training in sleep-related management, could also be used leading up to and during the next outbreak of COVID-19 or in a similar situation. It is also imperative that PWE and their caregivers have a reliable way to communicate with epilepsy providers in the event that a subsequent outbreak results in changes in routine, such as altered sleep, that increase their seizure risk.
Our sample's reports of increased isolation, anxiety, and stress during the pandemic are also troubling. During normal circumstances, PWE, as well as family caregivers, tend to be socially isolated when compared with the general public [18]. In fact, this sample had a significant level of social isolation prepandemic (mean: 6.27 on a 0–10 scale). This isolation puts them at risk of depressive symptoms, anxiety, and lower quality of life [19]. The significant increase in the social isolation seen in both PWE and caregivers during the pandemic is concerning, as it puts them at risk for an exacerbation of existing isolation-related problems. Further, the significant decrease in respondents' perceived levels of social support after pandemic onset suggests that members of our sample, socially isolated at baseline, are even more isolated now but with less social support. In anticipation of more social distancing in the future, PWE and caregivers should be educated on how to mitigate social isolation. Those PWE who have existing mental healthcare practitioners should be encouraged to reach out to them for virtual visits. Those without such existing practitioners should be encouraged to visit the CDC and Epilepsy Foundation websites, where resources regarding social isolation, including virtual support groups, can be found, and those who continue to struggle with social isolation can be referred to an appropriate mental healthcare provider, even in the midst of a pandemic.
Our sample's significant increase in anxiety and stress from pre- to postpandemic onset is not surprising but is concerning in that it could put them at higher risk for seizures [20]. While some of these increased anxiety and stress was related to the pandemic in general, some was specific to epilepsy: concern about what would happen if they did contract the virus (e.g., were they more likely to die given the presence of epilepsy), worry about not being able to access medications or healthcare provider, and fear of not receiving needed care due to rationing. Thus, epilepsy providers or their liaisons should be sure to communicate to patients and caregivers about how they could be more or less affected by COVID-19 given their epilepsy, and explain truths about care rationing, and its potential to affect PWE. As stated earlier, counseling PWE and caregivers on ways in which to secure medications will also help to allay fears in this area.
The overall findings of the current study also underscore that any major change in routine—pandemic-related or not—can put a person's epilepsy self-management and associated outcomes at risk. Prior studies have indicated that epilepsy self-management is a complex process that changes based on a person's perceived health and all levels of his or her environment, from interpersonal to societal. In short, epilepsy self-management is not a stagnant concept, and can be destabilized when a person's environment changes [9]. Development of robust self-management skills for PWE should thus be prioritized, including for very disruptive instances, such as another pandemic, periods of social distancing, or any life-altering event.
4.1. Limitations
This study is not without limitations. First, we were not able to collect data on important variables (affective symptoms, for example) prior to the pandemic. Rather, we had to rely on respondents' memories, asking them to answer questions considering both normal and present (pandemic) circumstances. Second, our sample represents mostly White, middle-class people with college degrees. It is important to recognize that our results may not be as generalizable to populations less well-represented in our sample. Finally, our sample of 94 is somewhat small; if possible, similar research should be repeated with a larger, more diverse sample in the event of a similar situation.
5. Conclusions
The COVID-19 pandemic has upended normal life, and current findings demonstrate that it has also disrupted epilepsy self-management for PWE and their caregivers. During this unusual time, most medical care is understandably directed at managing COVID-19 and saving lives of those affected. While there has been and will be a future need to put off “nonurgent” healthcare during subsequent local and state shut downs, those citizens with chronic diseases, including epilepsy, have daily management needs that do not go away during a pandemic or other life-altering change; conversely, these needs are heightened. Physicians and nurses who provide care to PWE should prioritize making plans with PWE and caregivers in the event of significant disruptions. Members of our sample would have benefitted greatly from clear-cut guidance from epilepsy providers regarding how to communicate with them and that they were allowed to do so. In light of current results, the professional epilepsy community should consider treatment and management guidelines for pandemic-like societal and health system disruptions. In addition, prioritization of robust self-management skills upon epilepsy diagnosis and continuing throughout the disease course remains necessary for PWE and the caregivers who assist them.
Declaration of competing interest
The authors declare that they have no known competing interest.
References
- 1.University JH. COVI-19 dashboard 2020 [Available from: https://coronavirus.jhu.edu/map.html accessed 4/25 2020.
- 2.Prevention CfDCa . 2020. Cases of coronavirus disease (COVID-19) in the U.S. [Google Scholar]
- 3.Prevention CfDCa . 2020. 1918 pandemic (H1N1 virus) [Google Scholar]
- 4.The White House CfDCaP, and the Federeal Emergency Management Adjacency Coronavirus (COVID-19) 2020 [Available from: https://www.coronavirus.gov/ accessed 4/25 2020.
- 5.Prevention CfDCa. Healthcare facilities: preparing for community transmission 2020 [Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html accessed 4/25 2020.
- 6.Prevention CfDCa. People who are at higher risk for severe illness 2020 [Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html accessed 4/20 2020.
- 7.Kissler S.M., Tedijanto C., Goldstein E., Grad Y., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020 doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tarver T. Epilepsy across the spectrum: promoting health and understanding edited by Mary Jane England, Catharyn T. Liverman, Andrea M. Schultz, and Larisa M. Strawbridge. J Consum Health Internet. 2013;17(2):238–239. [Google Scholar]
- 9.Miller W.R., Lasiter S., Bartlett Ellis R., Buelow J.M. Chronic disease self-management: a hybrid concept analysis. Nurs Outlook. 2015;63(2):154–161. doi: 10.1016/j.outlook.2014.07.005. published Online First: 2014/09/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cella D., Yount S., Rothrock N., Gershon R., Cook K., Reeve B. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. published Online First: 2007/04/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Appireddy R., Khan S., Leaver C., Martin C., Jin A., Durafourt B.A. Home virtual visits for outpatient follow-up stroke care: cross-sectional study. J Med Internet Res. 2019;21(10):e13734. doi: 10.2196/13734. published Online First: 2019/10/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Armstrong R.L. Your guide to internet service during new coronavirus (COVID-19) outbreak 2020. https://www.highspeedinternet.com/resources/internet-guide-during-coronavirus-outbreak Available from:
- 13.van Diessen E., Otte W.M., Braun K.P., Stam C.J., Jansen F.E. Does sleep deprivation alter functional EEG networks in children with focal epilepsy? Front Syst Neurosci. 2014;8:67. doi: 10.3389/fnsys.2014.00067. published Online First: 2014/05/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manganotti P., Bongiovanni L.G., Fuggetta G., Zanette G., Fiaschi A. Effects of sleep deprivation on cortical excitability in patients affected by juvenile myoclonic epilepsy: a combined transcranial magnetic stimulation and EEG study. J Neurol Neurosurg Psychiatry. 2006;77(1):56–60. doi: 10.1136/jnnp.2004.041137. published Online First: 2005/12/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malow B.A. Sleep deprivation and epilepsy. Epilepsy Curr. 2004;4(5):193–195. doi: 10.1111/j.1535-7597.2004.04509.x. published Online First: 2005/08/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller W.R., Otte J.L., Pleuger M. Perceived changes in sleep in adults with epilepsy. J Neurosci Nurs. 2016;48(4):179–184. doi: 10.1097/JNN.0000000000000214. published Online First: 2016/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dilorio C., Escoffery C., Yeager K.A., McCarty F., Henry T.R., Koganti A. WebEase: development of a Web-based epilepsy self-management intervention. Prev Chronic Dis. 2009;6(1):A28. published Online First: 2008/12/17. [PMC free article] [PubMed] [Google Scholar]
- 18.Mlinar S, Petek, D., Cotic, Z., Ceplak, M., & Zaletel, M. Persons with epilepsy: between social inclusion and marginalisation. Behav Neurol 2016 doi: https://dx.doi.org/10.1155%2F2016%2F2018509 [DOI] [PMC free article] [PubMed]
- 19.Mula M., Sander J.W. Psychosocial aspects of epilepsy: a wider approach. BJPsych Open. 2016;2(4):270–274. doi: 10.1192/bjpo.bp.115.002345. published Online First: 2016/10/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKee H.R., Privitera M.D. Stress as a seizure precipitant: identification, associated factors, and treatment options. Seizure. 2017;44:5. doi: 10.1016/j.seizure.2016.12.009. [DOI] [PubMed] [Google Scholar]