Abstract
Immune-related (IR)-pneumonitis is a rare and potentially fatal toxicity of anti-PD(L)1 immunotherapy. Expert guidelines for the diagnosis and management of IR-pneumonitis include multidisciplinary input from medical oncology, pulmonary medicine, infectious disease, and radiology specialists. Severe acute respiratory syndrome coronavirus 2 is a recently recognized respiratory virus that is responsible for causing the COVID-19 global pandemic. Symptoms and imaging findings from IR-pneumonitis and COVID-19 pneumonia can be similar, and early COVID-19 viral testing may yield false negative results, complicating the diagnosis and management of both entities. Herein, we present a set of multidisciplinary consensus recommendations for the diagnosis and management of IR-pneumonitis in the setting of COVID-19 including: (1) isolation procedures, (2) recommended imaging and interpretation, (3) adaptations to invasive testing, (4) adaptations to the management of IR-pneumonitis, (5) immunosuppression for steroid-refractory IR-pneumonitis, and (6) management of suspected concurrent IR-pneumonitis and COVID-19 infection. There is an emerging need for the adaptation of expert guidelines for IR-pneumonitis in the setting of the global COVID-19 pandemic. We propose a multidisciplinary consensus on this topic, in this position paper.
Keywords: guidelines as topic, immunotherapy, autoimmunity
Background
Immune-related (IR)-pneumonitis is an uncommon but potentially fatal toxicity that occurs in 5%–10% of patients treated with anti-PD(L)1 immunotherapy, and is defined as a focal or diffuse inflammation of the lung parenchyma.1 Patients with IR-pneumonitis most commonly present clinically with non-productive cough and shortness of breath, and less commonly with fever and chest pain.2 The diagnosis of IR-pneumonitis is one of exclusion, and involves completion of a standard institutional evaluation to rule out respiratory infection inclusive of laboratory testing, chest CT imaging, and in selected symptomatic cases, bronchoscopy with bronchoalveolar lavage (BAL), with the goal of ruling out alternative diagnoses such as infection and malignant lung infiltration.3–5
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a newly recognized respiratory virus responsible for the COVID-19 global pandemic. Since its declaration as a global pandemic by the WHO on March 11, 2020, over five million cases of documented COVID-19 have been diagnosed worldwide, resulting in over 330,000 deaths.6 Importantly, patients with comorbidities such as cancer appear to have higher case-fatality rates from COVID-19.7–9 Retrospective studies suggest patients with hematologic malignancies, lung cancer, and metastatic cancer are at particularly high risk of severe disease.10 Interestingly, receipt of programmed-death 1 (PD-1) pathway blockade does not appear to impact the severity of COVID-19 in patients with cancer.11 That said, the diagnosis and management of toxicities related to immune checkpoint blockade in the era of COVID-19 poses several challenges. Similar to patients who develop IR-pneumonitis, those with COVID-19 infection tend to present clinically with fever, cough, myalgia, fatigue, and shortness of breath.12–14 Unlike IR-pneumonitis, however, COVID-19 is a viral illness transmissible via droplet, human contact, and possibly airborne transmission, and thus requires infection prevention measures to limit transmission. Across the world, testing and triage algorithms have been developed in order to identify patients most suitable for COVID-19 testing via viral PCR assay of nasopharyngeal samples. In general, patients who develop fever, respiratory changes, or other symptoms consistent with COVID-19 are considered for testing. Although widespread testing of asymptomatic individuals is not currently recommended, institutions may opt to test select asymptomatic populations such as residents of long-term care facilities or patients undergoing operative interventions. For symptomatic patients, diagnostic evaluation with chest imaging (chest X-ray, CT) and other laboratory tests (ferritin, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, interleukin (IL)-6) are completed according to institutional algorithms to assist in identifying cases that may clinically worsen,15 but have yet to be validated for their associations with clinical outcome.
Since patients with cancer have a COVID-19-related fatality rate of up to 25%,7 the timely diagnosis and management of this infection has rapidly risen to a level of equal importance as the management of these patients’ underlying cancers, and the complications of their treatment. Thus, the ability to effectively discern and appropriately manage IR-pneumonitis in the context of COVID-19 is a question of increasing clinical relevance in patients with cancer, since anti-PD(L) immunotherapy is approved in 15 different cancer indications, with over 40% of patients with cancer in the USA now being eligible to receive immunotherapy in a standard of care setting.16
Methods
Recommendations: group representation and input
In response to the need for clear and concise recommendations for the management of IR-pneumonitis in the setting of the global COVID-19 pandemic, these recommendations were drafted with multidisciplinary cross-institutional input from medical oncology, infectious diseases including hospital epidemiology and infection control, pulmonary medicine and radiology subspecialists with expertise in IR-pneumonitis and COVID-19. The most pressing clinically-relevant questions and recommendations were discussed using an iterative, modified Delphi methodology.
Recommendation objectives
The primary objectives of this position paper are to outline diagnostic evaluation and management principles for IR-pneumonitis in the setting of COVID-19. This includes emerging issues related to appropriate: (1) isolation procedures, (2) imaging and interpretation, (3) adaptations to invasive testing for IR-pneumonitis, (4) adaptations to current medical management of IR-pneumonitis, (5) immunosuppressive therapy for steroid-refractory IR-pneumonitis, and (6) management of suspected concurrent IR-pneumonitis and COVID-19 infection.
Strengths and limitations of recommendations
The recommendations in this clinical guidance document represent expert opinion that is based on limited and primarily retrospective data. Recommendations are subject to change as new data become available.
Clinical considerations and recommendations
Previous to the COVID-19 pandemic, published consensus guidelines for the diagnosis and management of IR-pneumonitis had been developed by multiple oncologic societies.3 4 17 18 We propose that selected recommendations within these guidelines be adapted in the context of COVID-19, and outline these changes in table 1. These recommendations provide overall guidance in common clinical scenarios, however specific management decisions should be made on a case-by-case basis, weighing individual risks/benefits in the context of patient goals, comorbidities, disease status, and provider safety. In addition, wherever possible, multi-specialty input should be sought.19
Table 1.
Pneumonitis diagnostic evaluation and management considerations in setting of COVID-19
| Pneumonitis grading* | Diagnostic evaluation, safety procedures and management | Treatment | |
| COVID-19 negative | COVID-19 positive | ||
| G1†: clinically asymptomatic with radiographic changes ONLY |
|
|
|
| G2: clinically symptomatic, restricting instrumental activities of daily living |
|
|
|
| G3: severe symptoms limiting activities of daily living, oxygen indicated G4: life-threatening respiratory compromise |
|
|
|
*Grade by Common Terminology Criteria for Adverse Events (CTCAE) criteria version 4.03.
†For G1 pneumonitis, a chest CT with contrast should be obtained if not already performed. Guidelines also suggest obtaining pulmonary function testing (PFTs) but in the setting of COVID-19 and risk of virus transmission with PFTs, we do not recommend obtaining routine PFTs if there is any suspicion for COVID-19.
‡Follow-up preferable by virtual telemedicine visit or telephone.
§Practitioner should wear contact personal protective equipment with eye protection (PAPR or N95 with face shield/goggles), gown, and gloves.
G, grade; IVIG, intravenous immunoglobulin; PAPR, powered air purifying respirator; RVP, respiratory viral panel.
Isolation procedures
The WHO and other groups have established guidelines for the appropriate screening and triage of patients with suspected COVID-19.20–22 When possible, routine patient visits and monitoring of otherwise clinically asymptomatic individuals receiving cancer treatments should be conducted via telemedicine.21 22 If in-person clinical evaluation is required, we recommend screening for the new onset of symptoms concerning for COVID-19 by phone prior to the scheduled visit, and again at in-person registration, to ensure patients are seen in a setting where appropriate infection prevention practices can be instituted such as a dedicated COVID-19 assessment area.
For patients who screen positive for symptoms concerning for IR-pneumonitis and/or COVID-19 when in the oncology clinic, such patients should be isolated in a separate dedicated COVID-19 screening/testing area to limit exposure to other patients and healthcare workers. Specifically, this includes ensuring that the patient immediately dons a face mask, and is placed in a private room (ideally with negative-pressure capabilities) with the door closed. Staff assessing these patients should be trained on optimal infection prevention practices including appropriate donning and safe doffing of personal protective equipment (PPE) which may include a fit-tested N95 or other respirator, protective eyewear, gown and gloves. Due to nationwide PPE shortages we recognize many facilities may not have sufficient respirators for all healthcare workers evaluating patients with COVID-19, and may preserve respirators for those undergoing aerosol generating procedures. On vacating the clinic room, it is vital to clean, disinfect, and await adequate air exchange, as directed by institutional guidance from infection control specialists. These measures are important in order to prevent potential onward transmission from a patient with suspected IR-pneumonitis and/or COVID-19 to ensure patients are seen in a setting where appropriate infection prevention practices can be instituted, such as a dedicated COVID-19 assessment area including mobile drive-through testing.
Imaging of IR-pneumonitis and COVID-19
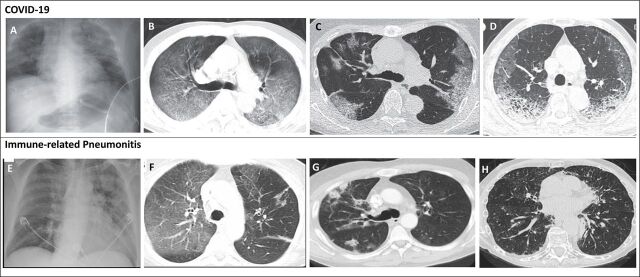
The most common appearances of IR-pneumonitis and COVID-19 infection on chest X-ray and chest CT imaging are depicted in figure 1. Since interstitial lung changes are poorly appreciated on chest X-ray, diagnostic chest CT is the recommended imaging modality for the evaluation of IR-pneumonitis.4 The spectrum of imaging findings of IR-pneumonitis on chest CT are described using radiographic patterns according to American Thoracic Society and European Respiratory Society classifications of interstitial pneumonias and related conditions including (1) acute interstitial pneumonia/acute respiratory distress syndrome (ARDS) pattern; (2) cryptogenic organizing pneumonia (COP) pattern; (3) non-specific interstitial pneumonia pattern; and (4) hypersensitivity pneumonitis pattern.1 23–27 Among these, the most common pattern is the COP pattern, characterized by multifocal bilateral parenchymal consolidations and ground glass opacities (GGOs) in a peripheral and lower lung distribution on chest CT.23 In addition, many patients frequently have diffuse bilateral lung involvement and the distribution is often independent from that of tumor involvement of the lung.2
Figure 1.
Representative images for COVID-19 (A–D) and immune-related (IR) pneumonitis (E–H). (A) Radiograph with opacities in bilateral upper and mid-lung fields. (B) Axial chest CT with diffuse bilateral ground-glass opacities (GGOs) with areas of consolidative opacities. (C) Axial chest CT with predominantly peripheral GGOs associated with interlobular septal thickening. (D) Axial chest CT with bilateral peripheral interstitial opacities with GGOs, reticular opacities, consolidation and interlobular septal thickening. (E) Radiograph of patient with immune-related pneumonitis, demonstrating left upper lobe predominant airspace opacities. (F) Axial chest CT of same patient demonstrates bilateral GGOs with interlobular septal thickening. (G) Axial chest CT demonstrating cryptogenic organizing pneumonia pattern of IR-pneumonitis with multifocal discrete areas of consolidation and bilateral GGOs. (H) Axial chest CT demonstrating a non-specific interstitial pneumonia pattern of IR-pneumonitis with increased interstitial markings, interlobular septal thickening, subpleural GGOs and reticular opacities. (A–D) images abstracted from Zu et al, 33 Shi et al 35 (E–F) images abstracted fromNaidoo et al,1 Al-Shamsi et al,22 Licenses to reproduce images obtained for22 and,33 licenses for1 and 35 in process.
Similar to IR-pneumonitis, chest X-ray appears to be less sensitive in detecting lung pathology for COVID-19 compared with CT imaging. In the largest single retrospective compilation of patient data from 1099 patients from 552 hospitals in 30 municipalities in mainland China, 59% of patients with COVID-19 had abnormal chest radiograph findings, whereas 86% had abnormal chest CT findings.28 The imaging manifestations of COVID-19 pneumonia are also variable, and have a wide spectrum ranging from normal chest CT in PCR-positive patients to fulminant and extensive bilateral interstitial opacities29–37 (figure 1). Evolving knowledge indicates that the typical CT imaging features of COVID-19 pneumonia include peripheral, bilateral GGOs or multifocal rounded GGOs that are noted with or without consolidation, or other findings suggestive of organizing pneumonia.38 Therefore, the radiographic pattern of typical COVID-19 pneumonia certainly overlaps with a COP pattern of IR-pneumonitis, which is the most frequently observed pattern. Similarly, the most fulminant cases from both entities result in the manifestations of ARDS characterized by diffuse or multifocal extensive GGOs and consolidations on imaging. In both entities, imaging manifestations reflect the lung’s response to injury, and the lung’s response patterns are often limited to several types as previously described.26 Thus, overlap is inevitable, making it difficult to distinguish between entities based on imaging alone.
Further complicating the diagnosis, abnormalities on chest CT may precede positive COVID-19 testing in some patients.32 35 Several studies have shown that completely asymptomatic infection may have imaging abnormalities (which tend to be less severe than in symptomatic patients).35 Conversely, a substantial percentage of patients with confirmed COVID-19 may initially present with normal CT imaging.30 The optimal approach to the longitudinal management of these patients has not been elucidated. Relevant to these cases, the WHO recommends symptomatic treatment and self-isolation only for patients with mild symptoms not requiring hospitalization.20 39 Therefore, in patients in whom grade 1 IR-pneumonitis is suspected, asymptomatic COVID-19 should now be considered in the differential diagnosis. Specific management recommendations for grade 1 IR-pneumonitis are outlined in the management section below.
Invasive diagnostic testing for IR-pneumonitis
The standard evaluation for IR-pneumonitis involves completion of a broad assessment of common respiratory pathogens via laboratory and non-invasive testing including but not limited to a respiratory viral panel, testing for atypical lung infections (eg, Mycoplasma, Aspergillus, Pneumocystis jiroveci), sputum culture and blood culture. In addition, a contrast-enhanced chest CT scan is recommended to assess lung tumor progression, and may require CT angiography technique if pulmonary embolism is suspected. Other common pulmonary comorbidities, particularly in patients with lung cancers, such as exacerbations of chronic obstructive pulmonary disease or congestive heart failure, should also be considered. Evaluation in symptomatic and critically ill cases may also include bronchoscopy with bronchoalveolar lavage (BAL) ±lung biopsy in order to assess for respiratory pathogens that may have been missed on non-invasive testing, as well as for malignant lung infiltration.
However, performing a bronchoscopy to diagnose suspected IR-pneumonitis may increase viral transmission risk of COVID-19 through aerosolization and may precipitate respiratory failure in patients with a tenuous clinical status. Precautions to minimize coughing and aerosolization, such as elective intubation, and the use of disposable bronchoscopes (if available) should be considered. Overall, we recommend that bronchoscopy for suspected IR-pneumonitis should be avoided or only completed in selected cases in which appropriate airborne precautions have been taken, and in consultation with both pulmonary medicine and infectious disease specialists. In selected cases in which this is needed, this procedure should ideally be performed in a negative pressure room with full COVID-19 precautions including appropriate donning of PPE. These recommendations align with those laid out by the Surviving Sepsis Campaign guidelines on the management of critically ill adults with COVID-19.40
Management of IR-pneumonitis in the setting of COVID-19
Grade 1 IR-pneumonitis
The management of patients who develop grade 1 IR-pneumonitis (radiographic abnormalities but otherwise asymptomatic) is a contentious area in clinical practice. Published guidelines recommend either holding immunotherapy, or cautiously continuing treatment.3 4 17 18 While imaging findings consistent with COVID-19 may appear in otherwise asymptomatic individuals, the decision to pursue COVID-19 testing for these patients is controversial, and likely will be affected by the availability of tests and region-specific risks of COVID-19. Thus, testing for COVID-19 in the setting of suspected grade 1 pneumonitis should be made on a case-by-case basis in consultation with institutional infectious disease and infection control specialists. Given this, we recommend that those with suspected grade 1 IR-pneumonitis continue to be monitored at 3–7 days after initial diagnosis in order to assess for potential development of either symptomatic pneumonitis or COVID-19. In addition, because radiographic changes of COVID-19 may appear before symptoms develop or PCR testing is warranted, we recommend withholding of anti-PD(L)1 immunotherapy in this scenario (table 1). The duration of immune checkpoint inhibitor (ICI) withholding should be made on a case-by-case basis, depending on subsequent development of symptoms, and further clinical assessments.
Grade 2 and higher IR-pneumonitis
High-dose corticosteroid therapy is the cornerstone of treatment for patients who develop symptomatic (grade ≥2) IR-pneumonitis. Due to the potential fatality risk from this immune-related adverse event (irAE), and guided by its severity by Common Toxicity Criteria for Adverse Events,41 corticosteroids are often commenced prior to completion of a full diagnostic evaluation, and may be co-prescribed with empiric antimicrobials.
The role for corticosteroids in the management of COVID-19 infection is controversial. Several retrospective studies suggest a potential role for corticosteroids in the management of severe COVID-19 infection with ARDS. In a single-center retrospective analysis from Wuhan Jinyintan Hospital in China, methylprednisolone use in patients with COVID-19 with ARDS was associated with a reduced risk of death (HR, 0.38; 95% CI, 0.20 to 0.73).42 In a separate published but not peer-reviewed single-center study, methylprednisolone given at a dose of 1–2 mg/kg/day for 5–7 days in patients hospitalized for severe COVID-19 pneumonia was associated with a shorter duration of supplemental oxygen use.43 Other studies have shown that a greater percentage of patients requiring ICU admission have received corticosteroids than those not needing ICU-level care,13 and demonstrated that more non-survivors of severe COVID-19 infection received corticosteroids compared with survivors.44 45 However, these data are likely to represent confounding by indication in the setting of critical illness.
In other viral ARDS syndromes, data have been mixed on the utility of corticosteroids. Large-scale meta-analyses suggest corticosteroid use may be associated with increased risk of mortality and hospital-acquired infection in patients with influenza.46 However, the quality of this data was poor and a subsequent analysis found no association between corticosteroid use and risk of death.47 In critically-ill patients infected with Middle East Respiratory Syndrome coronovirus (MERS-CoV) or SARS-CoV, corticosteroid treatment was not associated with increased mortality, but was associated with a delay in viral RNA clearance.48 49 In the treatment of ARDS as a whole, corticosteroid use has been shown to be associated with a reduced duration of mechanical ventilation, but its effect on all-cause mortality is uncertain.50 51
Taking the above data into account, the surviving sepsis guidelines on the management of critically ill adults with COVID-19 makes a weak recommendation against the routine use of systemic corticosteroids in mechanically ventilated adults with COVID-19 without ARDS. However, they make a weak recommendation for systemic corticosteroid use in mechanically ventilated patients with COVID-19 with ARDS.40 Other guidelines similarly recommend prudent corticosteroid use for selected critically ill patients with COVID-19 only,52 or routine avoidance of corticosteroids unless indicated for another reason.39 Multiple clinical trials (NCT04244591, NCT04323592, NCT04273321) are currently ongoing to clarify the role for corticosteroids in critically-ill patients with COVID-19.
Based on the clear benefit for corticosteroids in IR-pneumonitis, and the conflicting evidence for corticosteroids in COVID-19 with limited evidence in non-critically ill patients, we recommend confirmation of COVID-19 status before proceeding with corticosteroid therapy in patients with suspected grade 2 IR-pneumonitis.
For patients with grade 3 or higher IR-pneumonitis, in whom expedited treatment is critical, we recommend empiric corticosteroids while awaiting results of COVID-19 testing (table 1). Corticosteroids can then be discontinued in the setting of a positive COVID-19 PCR test result. In the setting of a negative COVID-19 PCR with ongoing high level of clinical suspicion for COVID-19, it is reasonable to reassess for concurrent COVID-19 infection with repeat PCR testing within 5–7 days of corticosteroid initiation.
Immunosuppression for steroid-refractory IR-pneumonitis in the context of COVID-19
While the majority of cases of IR-pneumonitis will improve with high-dose corticosteroids, steroid-refractory pneumonitis is not uncommon.2 In the event of IR-pneumonitis that does not clinically improve after ≥48 hours of high-dose steroids, multiple guidelines recommend consideration of alternative immunomodulating agents including infliximab, cyclophosphamide, mycophenolate mofetil, or intravenous immunoglobulin.3 4 17 18 However, prospective data in support of these strategies are lacking, and are based largely on case series and case reports.53 54
One attractive potential treatment for steroid-refractory IR-pneumonitis is anti-IL-6 therapy. IL-6 is a prominent cytokine implicated in acute inflammation, particularly in phenomena such as cytokine release syndrome (CRS) secondary to chimeric antigen receptor (CAR)-T cell therapy.55 Anti-IL-6 agents such as tocilizumab and sarilumab are standard-of-care treatments for CRS from CAR-T.18 This treatment may also be an effective strategy for irAEs. In a single-center retrospective study of 34 patients with steroid-refractory irAEs, including 12 with IR-pneumonitis, 79.4% of patients demonstrated clinical improvement following tocilizumab treatment.56 A prospective study of tocilizumab for the treatment of gastrointestinal (GI) and rheumatologic irAEs is ongoing (NCT03601611), but additional prospective studies are warranted to further evaluate the efficacy of anti-IL-6 therapy in the treatment of IR-pneumonitis.
Cytokine release and severe systemic inflammation also appear to play a prominent role in severe ARDS secondary to COVID-19 infection. Multiple retrospective studies suggest COVID-19 infected patients requiring ICU-level care have higher levels of markers of systemic inflammation including D-dimer, multiple interleukins and tumor necrosis factor alpha (TNFα).12 13 Furthermore, higher levels of inflammatory markers including CRP, ferritin, IL-6 and D-dimer have been observed in non-survivors compared with survivors of COVID-19.42 44 45 57 Thus anti-inflammatory treatments, such as anti-IL-6 therapy, are mechanistically appealing for the treatment of COVID-19. Early data have been encouraging, with multiple case reports supporting the efficacy of tocilizumab in the treatment of severe COVID-19 infection.58–60 In addition, a prospective Chinese trial showed improved oxygenation in patients treated with tocilizumab,61 resulting in the approval of this therapy for the treatment of severe COVID-19 in China. These encouraging data have led to the development of multiple ongoing prospective clinical trials for anti-IL-6 therapy in patients with severe COVID-19, of which there are >40 trials enrolling patients worldwide at the time of this publication. Furthermore, the Society for Immunotherapy of Cancer recently published a consensus statement on IL-6 targeted therapies for COVID-19, advocating for maximal expeditious effort to make available anti-IL-6 agents for compassionate use, as well as suggesting monitoring of FiO2, PaO2/FiO2, CRP, and IL-6 in patients with COVID-19 receiving anti-IL-6 agents.62
Concurrent IR-pneumonitis and COVID-19 infection
Since there are published data in support of the potential benefit of anti-IL-6 therapy for both steroid-refractory IR-pneumonitis and severe COVID-19 infection, anti-IL-6 may be a reasonable treatment option for immunotherapy-treated patients with steroid-refractory IR-pneumonitis in the era of COVID-19 infection, as well as in the setting of possible concurrent IR-pneumonitis and COVID-19 infection. Anti-IL-6 therapy should not, however, replace initial management with corticosteroids in these patients. Rather, early implementation (≤48 hours of high-dose steroids if no clinical improvement or sooner if further deterioration) of anti-IL-6 therapy should be considered in an effort to limit prolonged exposure to high-dose corticosteroids.
Conclusions
With the escalation of the COVID-19 crisis, there is a critical need for guidelines outlining management strategies for patients with cancer. With Food and Drug Administration (FDA)-approvals in multiple cancer indications for anti-PD(L)1 immunotherapy, immunotherapy-treated patients with cancer represent a distinct subset of patients who may experience IR-pneumonitis, a challenging clinical situation to manage during the COVID-19 crisis. The multidisciplinary recommendations provided herein are intended to serve as a starting point for addressing the critical issues for diagnosis and management of IR-pneumonitis in the setting of COVID-19. We highlight the requirement for isolation procedures while COVID-19 rule out is conducted in those with IR-pneumonitis, the need to forgo bronchoscopy except in selected or exceptional cases, adaptation of corticosteroid treatment in the context of COVID-19, and recommendations for additional immunosuppressive options such as anti-IL-6 in steroid-refractory IR-pneumonitis or when concurrent COVID-19 infection is suspected. Crucially, these preliminary recommendations are made in light of the current immediate need for guidance, but should be refined as prospective data emerge.
Acknowledgments
Patients with cancers, those who are suffering from COVID-19, frontline healthcare workers caring for patients with COVID-19, and the many researchers who have gone to great lengths to publish vital data on this global crisis.
Footnotes
Twitter: @DrJNaidoo
Contributions: Manuscript writing: JN, JER; manuscript editing: JN, JER, KS, DF-K, PMF, SMS, CR, DBJ, MN, JRB; development of figures: JN, JER, MN. Study concept and design: JN, PMF, CR, JRB; recommendations: JN, JER, KS, DF-K, PMF, SMS, CR, DBJ, MN, JRB.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: JN: research funding: Merck, AstraZeneca; consulting/advisory board: Bristol-Myers Squibb, AstraZeneca, Roche/Genentech; honoraria: Bristol-Myers Squibb, Merck, AstraZeneca. DBJ: advisory boards/consulting: Array Biopharma, BMS, Jansen, Merck, Novartis; research funding: BMS, Incyte. JRB: advisory boards/consulting: Amgen, BMS, Genentech/Roche, Eli Lilly, GlaxoSmithKline, Merck, Sanofi; research funding: AstraZeneca, BMS, Genentech/Roche, Merck, RAPT Therapeutics Inc., Revolution Medicines; data and safety monitoring board/committees: GlaxoSmithKline, Sanofi. MN: advisory boards/consulting: Daiichi Sankyo, AstraZeneca; research funding: Merck, Canon Medical Systems, AstraZeneca, Daiichi Sankyo; honorarium: Roche. PMF: advisory boards/consulting: Abbvie, AstraZeneca, BMS; research funding: AstraZeneca, BMS, Kyowa, Novartis, Corvus.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with Anti-Programmed Death-1/Programmed death ligand 1 therapy. J Clin Oncol 2017;35:709–17. 10.1200/JCO.2016.68.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Suresh K, Voong KR, Shankar B, et al. Pneumonitis in non-small cell lung cancer patients receiving immune checkpoint immunotherapy: incidence and risk factors. J Thorac Oncol 2018;13:1930–9. 10.1016/j.jtho.2018.08.2035 [DOI] [PubMed] [Google Scholar]
- 3. Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of clinical oncology clinical practice guideline. J Clin Oncol 2018;36:1714–68. 10.1200/JCO.2017.77.6385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for immunotherapy of cancer (SITC) toxicity management Working group. J Immunother Cancer 2017;5:95. 10.1186/s40425-017-0300-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thompson JA. New NCCN guidelines: recognition and management of Immunotherapy-Related toxicity. J Natl Compr Canc Netw 2018;16:594–6. 10.6004/jnccn.2018.0047 [DOI] [PubMed] [Google Scholar]
- 6. University JH . Coronavirus resource center, 2020. Available: https://coronavirus.jhu.edu/map.html
- 7. Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335–7. 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314Cases from the Chinese center for disease control and prevention. JAMA 2020. [Epub ahead of print: 24 Feb 2020]. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 9. Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol 2020. 10.1016/j.annonc.2020.03.296. [Epub ahead of print: 26 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov 2020. 10.1158/2159-8290.CD-20-0422. [Epub ahead of print: 28 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Luo J, Rizvi H, Egger JV, et al. Impact of PD-1 blockade on severity of COVID-19 in patients with lung cancers. Cancer Discov 2020. 10.1158/2159-8290.CD-20-0596. [Epub ahead of print: 12 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. 10.1001/jama.2020.1585. [Epub ahead of print: 07 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. University JH . COVID-19 adult clinical management recommendations for Non-ICU patients (v.2020-04-01), 2020. Available: https://livejohnshopkins.sharepoint.com/sites/COVID-ED/Shared%20Documents/AgileMD%20_%20COVID-19%20Adult%20Inpatient%20Clinical%20Management%20Recommendations%20for%20Non-ICU%20Patients%20DRAFT%202020-04-01.pdf?csf=1&e=jHPgAY&cid=600254b9-2939-405d-9cd7-9be2a37fe98d [Accessed 1 Apr 2020].
- 16. Haslam A, Prasad V. Estimation of the percentage of US patients with cancer who are eligible for and respond to checkpoint inhibitor immunotherapy drugs. JAMA Netw Open 2019;2:e192535. 10.1001/jamanetworkopen.2019.2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haanen JBAG, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018;29:iv264–6. 10.1093/annonc/mdy162 [DOI] [PubMed] [Google Scholar]
- 18. Thompson JA, Schneider BJ, Brahmer J, et al. NCCN guidelines insights: management of Immunotherapy-Related toxicities, version 1.2020. J Natl Compr Canc Netw 2020;18:230–41. 10.6004/jnccn.2020.0012 [DOI] [PubMed] [Google Scholar]
- 19. Naidoo J, Zhang J, Lipson EJ, et al. A multidisciplinary toxicity team for cancer Immunotherapy-Related adverse events. J Natl Compr Canc Netw 2019;17:712–20. 10.6004/jnccn.2018.7268 [DOI] [PubMed] [Google Scholar]
- 20. World Health O . Operational considerations for case management of COVID-19 in health facility and community: interim guidance, 19 March 2020. Geneva: World Health Organization, 2020. 2020. Contract No.: WHO/2019-nCoV/HCF_operations/2020.1. [Google Scholar]
- 21. Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID-19 pandemic: Agility and collaboration toward a common goal. J Natl Compr Canc Netw 2020:1–4. 10.6004/jnccn.2020.7560 [DOI] [PubMed] [Google Scholar]
- 22. Al‐Shamsi HO, Alhazzani W, Alhuraiji A, et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID ‐19) Pandemic: An International Collaborative Group. Oncologist 2020. 10.1634/theoncologist.2020-0213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nishino M, Ramaiya NH, Awad MM, et al. Pd-1 Inhibitor-Related pneumonitis in advanced cancer patients: radiographic patterns and clinical course. Clin Cancer Res 2016;22:6051–60. 10.1158/1078-0432.CCR-16-1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Andruska N, Mahapatra L, Hebbard C, et al. Severe pneumonitis refractory to steroids following anti-PD-1 immunotherapy. BMJ Case Rep 2018;2018:bcr2018225937. 10.1136/bcr-2018-225937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nishino M, Sholl LM, Hodi FS, et al. Anti-PD-1-Related pneumonitis during cancer immunotherapy. N Engl J Med 2015;373:288–90. 10.1056/NEJMc1505197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nishino M, Hatabu H, Sholl LM, et al. Thoracic complications of precision cancer therapies: a practical guide for radiologists in the new era of cancer care. Radiographics 2017;37:1371–87. 10.1148/rg.2017170015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sears CR, Peikert T, Possick JD, et al. Knowledge gaps and research priorities in immune checkpoint Inhibitor-related pneumonitis. An official American thoracic Society research statement. Am J Respir Crit Care Med 2019;200:e31–43. 10.1164/rccm.201906-1202ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Guan W-jie, Ni Z-yi, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med Overseas Ed 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lei J, Li J, Li X, et al. Ct imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020;295:18. 10.1148/radiol.2020200236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bernheim A, Mei X, Huang M, et al. Chest CT findings in coronavirus Disease-19 (COVID-19): relationship to duration of infection. Radiology 2020;295:200463. 10.1148/radiol.2020200463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shi H, Han X, Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology 2020;295:20. 10.1148/radiol.2020200269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xie X, Zhong Z, Zhao W, et al. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 2020;200343:200343. 10.1148/radiol.2020200343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. ZY Z, Jiang MD, PP X, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology 2020;200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhao W, Zhong Z, Xie X, et al. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol 2020;214:1072–7. 10.2214/AJR.20.22976 [DOI] [PubMed] [Google Scholar]
- 35. Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020;20:425–34. 10.1016/S1473-3099(20)30086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wang K, Kang S, Tian R, et al. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin Radiol 2020;75:341–7. 10.1016/j.crad.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med 2020;382:2012–22. 10.1056/NEJMoa2004500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America expert consensus statement on reporting chest CT findings related to COVID-19. endorsed by the Society of thoracic radiology, the American College of radiology, and Rsn. Radiology: Cardiothoracic Imaging 2020;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Organization WH . Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected (version 1.2): World Health organization department of communications, 2020. Available: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected [Accessed 13 Mar 2020].
- 40. Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med 2020;48:e440–69. 10.1097/CCM.0000000000004363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang DY, Salem J-E, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 2018;4:1721–8. 10.1001/jamaoncol.2018.3923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020. 10.1001/jamainternmed.2020.0994. [Epub ahead of print: 13 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang Y, Jiang W, He Q, et al. Early, low-dose and short-term application of corticosteroid treatment in patients with severe COVID-19 pneumonia: single-center experience from Wuhan, China. medRxiv 2020. [Google Scholar]
- 44. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Deng Y, Liu W, Liu K, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J 2020. 10.1097/CM9.0000000000000824. [Epub ahead of print: 20 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lansbury LE, Rodrigo C, Leonardi-Bee J, et al. Corticosteroids as adjunctive therapy in the treatment of influenza: an updated Cochrane systematic review and meta-analysis. Crit Care Med 2020;48:e98–106. 10.1097/CCM.0000000000004093 [DOI] [PubMed] [Google Scholar]
- 47. Delaney JW, Pinto R, Long J, et al. The influence of corticosteroid treatment on the outcome of influenza A(H1N1pdm09)-related critical illness. Crit Care 2016;20:75. 10.1186/s13054-016-1230-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Arabi YM, Mandourah Y, Al-Hameed F, et al. Corticosteroid therapy for critically ill patients with middle East respiratory syndrome. Am J Respir Crit Care Med 2018;197:757–67. 10.1164/rccm.201706-1172OC [DOI] [PubMed] [Google Scholar]
- 49. Lee N, Allen Chan KC, Hui DS, et al. Effects of early corticosteroid treatment on plasma SARS-associated coronavirus RNA concentrations in adult patients. J Clin Virol 2004;31:304–9. 10.1016/j.jcv.2004.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Villar J, Ferrando C, Martínez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med 2020;8:267–76. 10.1016/S2213-2600(19)30417-5 [DOI] [PubMed] [Google Scholar]
- 51. Lewis SR, Pritchard MW, Thomas CM, et al. Pharmacological agents for adults with acute respiratory distress syndrome. Cochrane Database Syst Rev 2019;7:Cd004477. 10.1002/14651858.CD004477.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zhao JP, Hu Y, Du RH, et al. [Expert consensus on the use of corticosteroid in patients with 2019-nCoV pneumonia]. Zhonghua Jie He He Hu Xi Za Zhi 2020;43:183–4. 10.3760/cma.j.issn.1001-0939.2020.03.008 [DOI] [PubMed] [Google Scholar]
- 53. Ortega Sanchez G, Jahn K, Savic S, et al. Treatment of mycophenolate-resistant immune-related organizing pneumonia with infliximab. J Immunother Cancer 2018;6:85. 10.1186/s40425-018-0400-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Petri CR, Patell R, Batalini F, et al. Severe pulmonary toxicity from immune checkpoint inhibitor treated successfully with intravenous immunoglobulin: case report and review of the literature. Respir Med Case Rep 2019;27:100834. 10.1016/j.rmcr.2019.100834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Teachey DT, Lacey SF, Shaw PA, et al. Identification of predictive biomarkers for cytokine release syndrome after chimeric antigen receptor T-cell therapy for acute lymphoblastic leukemia. Cancer Discov 2016;6:664–79. 10.1158/2159-8290.CD-16-0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Stroud CR, Hegde A, Cherry C, et al. Tocilizumab for the management of immune mediated adverse events secondary to PD-1 blockade. J Oncol Pharm Pract 2019;25:551–7. 10.1177/1078155217745144 [DOI] [PubMed] [Google Scholar]
- 57. Ruan Q, Yang K, Wang W, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846–8. 10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Michot J-M, Albiges L, Chaput N, et al. Tocilizumab, an anti-IL-6 receptor antibody, to treat COVID-19-related respiratory failure: a case report. Ann Oncol 2020. 10.1016/j.annonc.2020.03.300. [Epub ahead of print: 02 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhang X, Song K, Tong F, et al. First case of COVID-19 in a patient with multiple myeloma successfully treated with tocilizumab. Blood Adv 2020;4:1307–10. 10.1182/bloodadvances.2020001907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mihai C, Dobrota R, Schröder M, et al. COVID-19 in a patient with systemic sclerosis treated with tocilizumab for SSc-ILD. Ann Rheum Dis 2020;79:668–9. 10.1136/annrheumdis-2020-217442 [DOI] [PubMed] [Google Scholar]
- 61. Zhang C, Wu Z, Li J-W, et al. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents 2020;55:105954. 10.1016/j.ijantimicag.2020.105954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Paolo Ascierto A A, Urba WJ, Anderson AC, et al. SITC statement on anti-IL-6/IL-6R for COVID-19, 2020. Available: https://www.sitcancer.org/research/covid-19-resources/il-6-editorial [Accessed updated April 2, 2020].