Abstract
Background
COVID-19 pandemic is presenting serious challenges to the world’s healthcare systems. The high communicability of the COVID-19 necessitates robust medical preparedness and vigilance.
Objective
To report on the simulation-based training and test preparedness activities to prepare healthcare workers (HCWs) for effective and safe handling of patients with COVID-19.
Methodology
Two activities were conducted: simulation-based training to all HCWs and a full-scale unannounced simulation-based disaster exercise at King Fahad Medical City (KFMC). The online module was designed to enhance the knowledge on COVID-19. This module was available to all KFMC staff. The five hands-on practical part of the course was available to frontliner HCWs. The unannounced undercover simulated patients’ full-scale COVID-19 simulation-based disaster exercise took place in the emergency department over 3 hours. Six scenarios were executed to test the existing plan in providing care of suspected COVID-19 cases.
Results
2620 HCWs took the online module, 17 courses were conducted and 337 frontliner HCWs were trained. 94% of learners were satisfied and recommended the activity to others. The overall compliance rate of the full-scale COVID-19 disaster drill with infection control guidelines was 90%. Post-drill debriefing sessions recommended reinforcing PPE training, ensuring availability of different sizes of PPEs and developing an algorithm to transfer patients to designated quarantine areas.
Conclusion
Simulation-based training and preparedness testing activities are vital in identifying gaps to apply corrective actions immediately. In the presence of a highly hazardous contagious disease like COVID-19, such exercises are a necessity to any healthcare institution.
Keywords: simulation based Education, quality improvement, disaster simulation, emergency department, COVID-19
What is already known in this subject.
Performance evaluation in disasters is a major challenge to healthcare administrators.
Personal protective equipment are needed for protecting healthcare workers against COVID-19.
System integration is used to bridge gaps and improve performance.
What this study adds.
COVID-19 presented serious challenges to the world’s healthcare systems.
Our study enforces the benefits of using simulation -based training and drills to prepare healthcare workers for effective and safe handling of patients with COVID-19 patients.
Three areas worth of testing for COVID-19 preparedness: triage system, infection control measures and flow of patients.
Introduction
The novel coronavirus pandemic has presented serious challenges to the world’s healthcare systems’ infrastructure.1 The high communicability of the COVID-19 disease necessitates robust medical preparedness and vigilance.2 Detailed practices and precautions need to be applied throughout the spectrum of care of patients with COVID-19.3 Routine testing of preparedness remains an integral step in assuring effective and safe handling and treatment of patients with highly hazardous contagious disease. The Center of Research, Education and Simulation Enhanced Training (CRESENT) at King Fahad Medical City (KFMC) in Riyadh, Saudi Arabia, has been conducting simulation exercises for performance improvement and to test operational preparedness for many years. CRESENT conducted simulation training exercises for mock codes, bed sores in intensive care unit,4 Ebola virus disease preparedness, speaking up as well as operational preparedness of new emergency department (ED) and bronchoscopy suite.5
This article reports on the simulation-based training and test preparedness activities to prepare KFMC healthcare workers (HCWs) for effective and safe handling of patients with COVID-19.
Methods
KFMC is the largest tertiary care medical centre under the Ministry of Health (MOH) in Saudi Arabia. The KFMC campus includes four hospitals with 1200-bed capacity and nine apartment towers for nursing staff and more than 400 living quarters. The higher administration of KFMC approved the initiative from the Infection Control Department (ICD), Disaster Management Department and CRESENT to train and test preparedness for COVID-19. A multidisciplinary committee composed of nurses, physicians, paramedics, simulationists and experts in system integration, quality control and disaster management were actively involved in developing and executing the training programme. The COVID-19 preparedness committee identified a specific goal for training and testing of KFMC HCWs: to increase awareness and preparedness of KFMC HCWs as per Saudi MOH, WHO and Centers for Disease Control and Prevention guidelines regarding COVID-19.6 7 The committee followed system integration methodology by reviewing and analysing current policies and practices related to the subject matter, identifying the gaps, exploring opportunities and composing a simulation-based training to bridge the previously identified gaps.8 Three main system domains were identified: triage system, infection control measures and flow of patients. Using structured electronic questionnaire, a representative sample from targeted departments was surveyed to identify their top needed skills and attitude objectives, preferred teaching methodology, target audience and ideal duration and timing of the training programme without affecting patient care. To accomplish these needs, the committee decided on two separate initiatives: a simulation-based training to all HCWs at KFMC who may get in contact with COVID-19 cases and a full-scale unannounced simulation-based disaster exercise at KFMC. Accordingly, two task forces were formed to develop the curriculum for the simulation-based education exercises.
The COVID-19 training task force objectives were:
To understand definition, epidemiology, symptoms and transmission of COVID-19.
To demonstrate competency in donning and doffing of personal protective equipment (PPE) including N95 mask.
To learn proper use of powered air-purifying respirators (PAPRs).
To perform medical equipment cleaning after a suspected case of COVID-19.
To recognise the importance of speaking up regarding infection control measures.
The course followed the blended learning approach. The online self-learning module was designed to enhance the knowledge of the learners on COVID-19 definition, epidemiology, signs, symptoms and transmission as per Saudi MOH. This module was made available to all KFMC staff (around 4500 HCWs) and was followed by an online examination. An electronic certificate was generated indicating completion of the theoretical part. The practical part of the course was made available to front-line staff (around 950 HCWs). It consisted of five hands-on skill stations: donning and doffing of PPE, PAPR, equipment cleaning, nasopharyngeal swab and one group discussion session on speaking up (table 1).
Table 1.
Characteristics of skill stations
| Skill station | Category | Elements | Description |
| PPE donning and doffing | Orientation | Simulator | Participants were oriented to PPE: N95 masks, surgical masks, gowns |
| Environment | Location | Multipurpose room | |
| Equipment | Gloves, gowns, face shield, N95 mask, hand sanitizer, cleaning wipes | ||
| Instructional design | Duration | 30 min (five learners) | |
| Structure | Demonstration by facilitator and each learner performs donning and doffing | ||
| Assessment | Direct observation | ||
| Feedback | Source | Facilitator | |
| Duration | During demonstration | ||
| Facilitator | Infection control nurse | ||
| Structure | Immediate feedback | ||
| Timing | Concurrent | ||
| PAPR | Orientation | Simulator | Participants were oriented to PAPR and Airway Larry (Nasco) |
| Environment | Location | Skills training room | |
| Equipment | PAPRs, cleaning spray and wipes, Airway Larry (Nasco) task trainer | ||
| Instructional design | Duration | 30 min (five learners) | |
| Structure | Demonstration by facilitator and assembly on manikin by learners | ||
| Assessment | Direct observation | ||
| Feedback | Source | Facilitator | |
| Duration | During demonstration | ||
| Facilitator | Infection control nurse | ||
| Structure | Immediate feedback | ||
| Timing | Concurrent | ||
| Cleaning of medical equipment | Orientation | Simulator | Participants were oriented to the vital signs monitor and room furniture |
| Environment | Location | ER examination clinic in simulation centre | |
| Equipment | Vital signs monitor (Carescape V100), crash cart, hospital bed, wipes | ||
| Instructional design | Duration | 30 min (five learners) | |
| Structure | Participants work together to clean equipment and surfaces | ||
| Assessment | Direct observation | ||
| Feedback | Source | Facilitator | |
| Duration | During demonstration | ||
| Facilitator | Environmental Services Instructor | ||
| Structure | Immediate feedback | ||
| Timing | Concurrent | ||
| Obtaining a nasopharyngeal swab | Orientation | Simulator | Participants were oriented to nasogastric tube model (3B Scientific) |
| Environment | Location | Skills training room | |
| Equipment | Nasogastric tube simulator, universal transport medium kit, blue top viral transfer, biohazard bag, labels, requisition form | ||
| Instructional design | Duration | 30 min (five learners) | |
| Structure | Demonstration by facilitator then each learner performs task | ||
| Assessment | Direct observation | ||
| Feedback | Source | Facilitator | |
| Duration | During demonstration | ||
| Facilitator | Nursing educator | ||
| Structure | Immediate feedback | ||
| Timing | Concurrent | ||
| Speaking up group discussion | Orientation | Simulator | Participants were oriented to group discussion format |
| Environment | Location | Classroom | |
| Equipment | Computer, LCD screen, flip chart | ||
| Simulation scenario | Event | Each group will watch the video: ‘We stand alone together, moments in China’s coronavirus battle’, followed by group discussion | |
| Format | Group discussion | ||
| Instructional design | Duration | 30 min | |
| Structure | Participants divided into four groups (five learners per group). In each station, they will watch a video for 3 min and then have group discussion | ||
| Assessment | Learner’s participation | ||
| Feedback | Source | Facilitator | |
| Duration | PC, LCD, chairs, flip chart, markers | ||
| Facilitator | Simulationist with expertise in debriefing | ||
| Structure | Advocacy inquiry debriefing | ||
| Timing | 20–25 min |
ER, emergency room; LCD, liquid crystal display; PAPR, powered air-purifying respirator; PC, personal computer; PPE, personal protective equipment.
On the other hand, the full-scale COVID-19 simulation-based disaster exercise objectives were the following:
To test Emergency Medical Services (EMS) response in a prehospital setting as per KFMC epidemic protocol.
To evaluate ED response dealing with suspected COVID-19 cases as per newly developed algorithms.
To assess infection control measures when dealing with COVID-19 cases.
Ancillary hospital departments at KFMC whose services were critical to the success of caring for patients with COVID-19 were involved in the unannounced exercise. These were: ED, EMS, patient affairs, security staff and Nursing Administration. The full-scale COVID-19 simulation-based disaster exercise took place in the ED over 3 hours with participation of around 70 staff from those departments. A total of six scenarios, using six standardised patients (SP) and one full body manikin, were executed to test the existing plan in providing care of the six patients with suspected COVID-19 disease (table 2). Compliance with infection control procedures was measured by computing the rate of fulfilments of the ‘expected actions’ from table 2. Plus-delta debriefing methodology was used for postexercise debriefing (table 2). The cited information and/or identifiable in table 2 are not from an actual patient. Any resemblance to real person living or deceased will be coincidence. In one hybrid scenario, the SP was switched to a manikin after he asked for a urinal and the HCW left the room.
Table 2.
Scenarios of full-scale COVID-19 simulation exercise
| No | Scenario | Expected action |
| 1 | A 35-year-old HCW living in the hospital housing calls hospital dispatch centre and tells them: he has high fever and cough and came from Egypt 2 days ago. Vital signs: BP=140/90 mm Hg, temperature=38.6°C, RR=28/min, HR=100/min, O2 Sat=91% (room air). After a few hours, the COVID-19 result is negative. |
|
| 2 | A 40-year-old HCW came from South Korea (Daegu City) asymptomatic and came to ED to check herself. Vital signs: BP=135/85 mm Hg, temperature=36.5°C, RR=18/min, HR=80/min, O2 Sat=96% (room air). |
|
| 3 | A 41-year-old Lebanese HCW, asymptomatic came to ER to check himself. Vital signs: BP=130/80 mm Hg, temperature=37°C, RR=16/min, HR=75/min, O2 Sat=97% (room air). |
|
| 4 | A 35-year-old nurse arrived 5 days back from India presented to the ED with cough, fever, fatigue and runny nose. Vital signs: BP=135/75 mm Hg, temperature=39°C, RR=20/min, HR=105/min, O2 Sat=95% (room air). CXR and laboratories: normal. |
|
| 5 | A 60-year-old man with diabetes, hypertension, complaining of cough, fever and shortness of breath came from Eastern Province in Saudi Arabia to the ED and has a contact with positive COVID-19 case. After triage and admission to a room in the ED Critical Area, a SimMan 3G is placed on the stretcher instead of the patient. Vital signs: BP=110/65 mm Hg, temperature=38.5°C, RR=28/min, HR=135/min, O2 Sat=85% (room air). |
|
| 6 | A 22-year-old college student comes from Eastern Province of Saudi Arabia to ED with fever, runny nose, sore throat and fatigue. Vital signs: BP=125/80 mm Hg, temperature=38.5°C, RR=18/min, HR=100/min, O2 Sat=96% (room air). |
|
BP, blood pressure; CXR, chest X-ray; ED, emergency department; EMS, Emergency Medical Services; ER, emergency room; HCW, healthcare worker; HR, heart rate; ICD, Infection Control Department; ICU, intensive care unit; MOH, Ministry of Health; O2 Sat, oxygen saturation; RR, respiratory rate.
Results
A total of 2620 HCWs at KFMC took the online module. Until the writing of this manuscript, a total of 17 courses were conducted with a total of 337 frontliner HCWs trained (table 3). Post-course evaluations were collected and presented in table 4. Around 94% of learners were satisfied or highly satisfied and recommended the simulation-based educational activity to the others.
Table 3.
Characteristics of healthcare providers who participated in COVID-19 training
| Characteristics | n (%) |
| Total | 337 (100) |
| Females | 292 (87) |
| Males | 45 (13) |
| Physicians | 9 (2.5) |
| Nurses | 317 (94) |
| Paramedics | 9 (2.5) |
| Allied health | 2 (1) |
Table 4.
COVID-19 course evaluation
| Item | Percentage |
| Educational perspective | |
| Content of this course related to my practice | 92 |
| Objectives of the course are clearly defined | 88 |
| Course has enough hands-on practice | 66 |
| Course duration was adequate for the content | 84 |
| Course information was up-to-date | 88 |
| Course objectives | |
| Understand the definition, epidemiology, symptoms and transmission of COVID-19 | 82 |
| Recognise the WHO and MOH guidelines and policy of COVID-19 outbreak preparedness | 80 |
| Follow the proper steps and guidelines when exposed to confirmed/ suspected patient with COVID-19 | 88 |
| Demonstrate competency in donning and doffing the PPE | 92 |
| Use PAPR effectively when dealing with suspected or confirmed cases | 88 |
| Recognise importance of speaking up when dealing with breaching of proper infection control guidelines | 90 |
MOH, Ministry of Health; PAPR, powered air-purifying respirator; PPE, personal protective equipment.
A total of 14 members from Disaster Management, ICD, Nursing Administration and CRESENT, 6 evaluators and 6 SPs conducted the full-scale COVID-19 simulation-based disaster exercise on the 11 March 2020. The overall compliance rate of the HCWs with infection control guidelines was 90%. Post-drill debriefing sessions with all participating departments/administrations were conducted to empower the strength points and identify the gaps in the triage system, infection control and flow of patients (table 5).
Table 5.
Strengths and challenges of the full-scale COVID-19 simulation-based disaster exercise
| Strengths |
|
| Challenges |
|
ED, emergency department; EMS, Emergency Medical Services; ER, emergency room; HCWs, healthcare workers; IC, infection control; ICD, Infection Control Department; PPE, personal protective equipment.
Triage system
The Nursing Administration at KFMC developed a robust algorithm for screening and triage of all patients arriving to ED (figure 1). Two main strengths of this full-scale COVID-19 simulation-based disaster drill worth mentioning. First was the identification of all undercovered (mystery) simulated patients as possible COVID-19 cases early on at arrival to the main door and namely by the so-called ‘visual nurse’. Second, the integration of Canadian Triage and Acuity Scale9 and the Visual Triage Checklist for Acute Respiratory Illness (figure 2) in the screening and triage process. No challenges reported under this domain.
Figure 1.
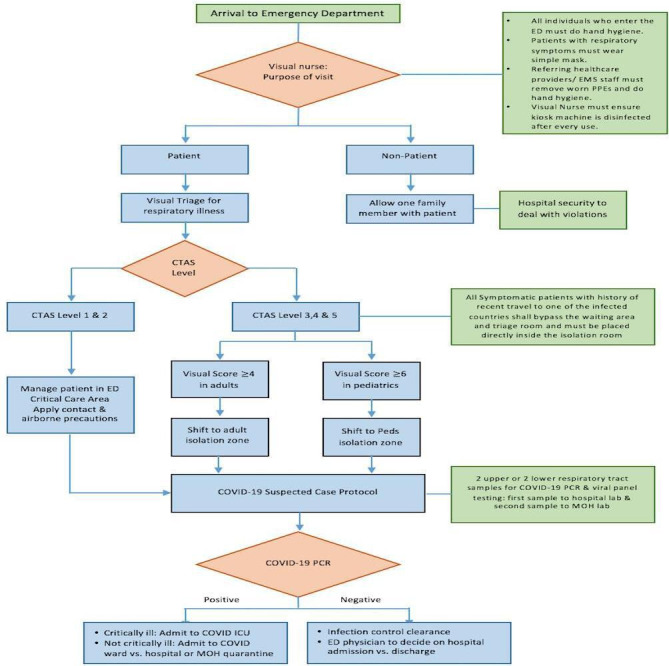
COVID-19 algorithm for screening and triage of patients arriving to emergency department (ED). CTAS, Canadian Triage and Acuity Scale; EMS, Emergency Medical Services; ICU, intensive care unit; MOH, Ministry of Health; PPEs, personal protective equipments.
Figure 2.
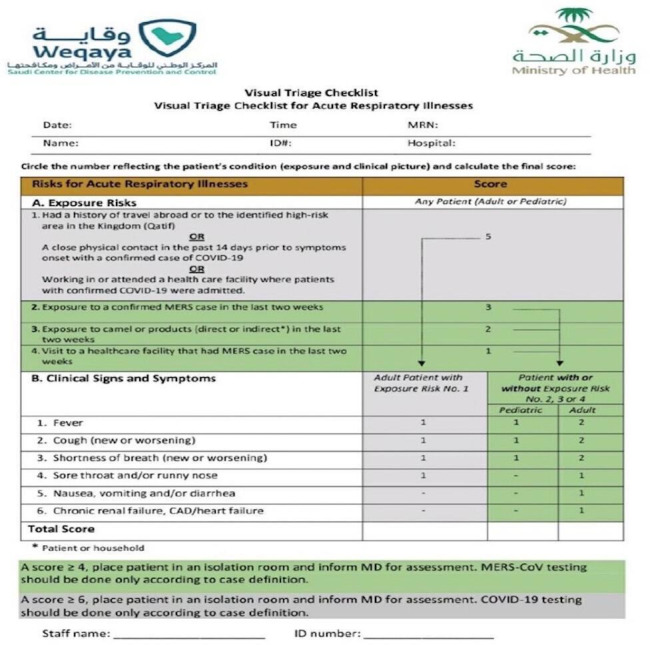
Visual triage checklist for acute respiratory illness. CAD, coronary artery disease; MERS-CoV, Middle East respiratory syndrome coronavirus; MRN, medical record number.
Infection control
All HCWs who participated in the full-scale COVID-19 simulation-based disaster drill practised strict infection control measures. Many strengths were described by the observation team. Hand hygiene was universally applied by all HCWs. There was limited access to the ED and hospital security played a noticeable role to achieve it. The challenges included: one nurse was not wearing the proper PPE, no proper cleaning of the queuing machine and linen used by EMS was taken back to the ambulance.
Flow of patients
The prehospital transfer of symptomatic HCWs from their living quarters to ED was adequate. The flow of patients within the ED was well controlled by hospital security and triage nurses. As for the confirmed patients with COVID-19 who require hospitalisation, they were transferred by EMS to the MOH-designated COVID-19 hospital outside KFMC as per protocol. Undercovered simulated HCWs with COVID-19 were supposed to be transferred to one of the KFMC housing towers that was designated by the ICD for home quarantine. Three challenges were identified: lack of written instructions for home isolation, no designated party to transfer back quarantined HCWs and lack of training of security staff in HCWs’ quarantine areas on infection control measures.
The major recommendations that were included in the final report: reinforcing PPE training regularly and registration in the COVID-19 course, ensuring availability of different sizes of PPEs and developing a clear algorithm to transfer patients to designated quarantine areas.
Discussion
Evaluating healthcare facilities performance in disasters remains a major challenge to healthcare administrators. Advanced healthcare systems, such as Italy, Spain and China, were overwhelmed with patients with COVID-19.10–12 Full-scale exercises and drills have been widely used to assess hospital readiness for effective and safe performance during highly contagious outbreaks.13–16 Violations of infection control practices by HCWs can be a major factor in facilitating the transmission of pathogens and outbreak.17 Infection control measures like hand hygiene require relentless efforts to secure a high level of awareness and compliance among HCWs.18 This study showed very high compliance of KFMC HCWs in applying written protocols when dealing with suspected cases of COVID-19. It also discovered gaps that were remediated immediately. The high compliance rate we encountered is due to the high awareness level of the KFMC HCWs as well as the unprecedented global effect of COVID-19. People around the world are exercising extreme measures like social distancing, disinfection of belongings and home quarantine to limit the spread of this highly communicable disease.
A key element in the success of any quality improvement and system integration project is the support from higher administration.19 The CRESENT System Integration Committee at KFMC, formed from leaders in high positions, has the mission to apply consistent, planned, collaborative and integrated interventions, in conjunction with systems engineering and risk management, to address KFMC healthcare system issues and needs and achieve excellent clinical care, enhanced patient safety and improved outcome metrics across the healthcare system. It represents an organised bidirectional feedback loop between CRESENT and the healthcare system at KFMC to integrate simulation programmes within the whole KFMC healthcare system.20 Many accelerated precautions decisions were taken at higher levels during the period of conducting the course, like stopping all training activities which might increase the risk of disease outbreak. The COVID-19 training course was excluded and precautions were arranged with the ICD to provide safe training to attendees and instructors. These precautions included reducing the number of participants per session, spacing the skill stations and frequent hand washing.
Protecting HCWs from getting infected remains an essential weapon in defeating COVID-19. Physicians, nurses, respiratory therapists, EMS personnel, environmental services personnel are all vulnerable and need to be protected both physically21 and psychologically.22 By the end of February 2020, China reported more than 3000 infected HCWs in Hubei alone.23 In a single designated hospital in Wuhan, 28 physicians and nurses contracted COVID-19.24 The figures from Italy have been more alarming given the difference in population and healthcare workforce. Around 9% (2609) of the COVID-19 cases are among HCWs.25 We included HCWs in four out of the six scenarios in the full-scale COVID-19 simulation-based disaster exercise with various risks to COVID-19.
The full-scale COVID-19 simulation-based disaster drill was unannounced with injected undercovered simulated patients. Unannounced or no-notice drills provide added realism and produce more realistic data when compared with scheduled drills. In Ebola preparedness no-notice drills, 40% of hospitals failed to ask patients about travel history, occupation, contact history and cluster information compared with 90% compliance rate during regular inspection.26 Furthermore, 49 New York City EDs were evaluated regarding their response to communicable diseases through unannounced undercovered simulated patient drills.27 These drills generated valuable information to the hospitals to improve on identifying and isolating patients with a potentially highly infectious disease.27
During this experience, we faced a few challenges. The main challenge was related to limited time in planning and execution of training and exercise. The COVID-19 has been spreading fast all over the world and immediate training and preparedness testing is of utmost importance. Another challenge is the balance of using PPE for training and saving hospital resources like N95 masks for the real pandemic. Such decisions need to be discussed properly with the institution’s supply chain and may affect course design and execution. The drills were carried out by members of Disaster Management, CRESENT and ICDs. Most of them are known by the hospital staff and this can affect performance and evaluation.
Simulation-based training and preparedness testing activities are vital in identifying gaps to apply corrective actions immediately. In the presence of a highly hazardous contagious disease like COVID-19, such exercise is a necessity to any healthcare institution. It identifies gaps and improves the HCWs’ preparedness. The main three areas worth of emphasising for COVID-19 preparedness simulation training include triage system, infection control measures and flow of patients.
Footnotes
Contributors: Study conception and design: UA, AAAl, WA, AAAr, MAA, BYM, SSA, YIA. Acquisition of data: YIA, BYM, SSA, MA, WA, AAAr, MAM, HAMA. Analysis and interpretation of data: HMSL, MA, WA, AAAr, YIA, FAA. Drafting of manuscript: HMSL. Critical revision: All authors discussed the results and contributed to the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. None.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This research was approved by the KFMC Institutional Review Board.
References
- 1. Sohrabi C, Alsafi Z, O'Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg 2020;76:71–6. 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lai C-C, Shih T-P, Ko W-C, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020;55:105924. 10.1016/j.ijantimicag.2020.105924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang P, Anderson N, Pan Y, et al. The SARS-CoV-2 outbreak: diagnosis, infection prevention, and public perception. Clin Chem 2020:644–51. 10.1093/clinchem/hvaa080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lababidi H, Shehadeh F, Almozainy S, et al. Pressure ulcer prevention in the intensive care unit: applying CRESENT system integration model. Proceedings of the Saudi Health Simulation Conference 2018 Adv Simul 2018;3:6. [Google Scholar]
- 5. AlMoziny S, AlMarshad A, Azizalrahman A, et al. Simulation-Based system integration in commissioning new emergency department. Proceedings of the Saudi Health Simulation Conference 2018 Adv Simul 2018;3:6. [Google Scholar]
- 6. Saudi MOH. Prevention from COVID-19 (Arabic). Available: https://www.moh.gov.sa/Documents/2020-01-29-002.pdf
- 7. Jernigan DB, CDC COVID-19 Response Team . Update: Public Health Response to the Coronavirus Disease 2019 Outbreak - United States, February 24, 2020. MMWR Morb Mortal Wkly Rep 2020;69:216–9. 10.15585/mmwr.mm6908e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dunn W, Deutsch E, Maxworthy J, et al. Brazil V: Systems Integration. In: Levine AI, DeMaria Jr S, Schwartz AD, et al., eds. The comprehensive textbook of healthcare simulation. New York: Springer, 2013: 121–33. [Google Scholar]
- 9. Murray M, Bullard M, Grafstein E, et al. Revisions to the Canadian emergency department triage and acuity scale implementation guidelines. CJEM 2004;6:421–7. 10.1017/S1481803500009428 [DOI] [PubMed] [Google Scholar]
- 10. Cao Y, Li Q, Chen J, et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med 2020;27:309–11. 10.1111/acem.13951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020. 10.1001/jama.2020.4031 [DOI] [PubMed] [Google Scholar]
- 12. Spina S, Marrazzo F, Migliari M, et al. The response of Milan's emergency medical system to the COVID-19 outbreak in Italy. Lancet 2020;395:e49–50. 10.1016/S0140-6736(20)30493-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abualenain JT, Al-Alawi MM. Simulation-Based training in Ebola personal protective equipment for healthcare workers: experience from King Abdulaziz university hospital in Saudi Arabia. J Infect Public Health 2018;11:796–800. 10.1016/j.jiph.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 14. Cardeñosa N, Domínguez A, Carratalà J, et al. Usefulness of simulated cases for assessing pandemic influenza preparedness plans. Clin Microbiol Infect 2010;16:1364–7. 10.1111/j.1469-0691.2010.03144.x [DOI] [PubMed] [Google Scholar]
- 15. Klein KR, Atas JG, Collins J. Testing emergency medical personnel response to patients with suspected infectious disease. Prehosp Disaster Med 2004;19:256–65. 10.1017/S1049023X00001850 [DOI] [PubMed] [Google Scholar]
- 16. Phrampus PE, O'Donnell JM, Farkas D, et al. Rapid development and deployment of Ebola readiness training across an academic health system: the critical role of simulation education, consulting, and systems integration. Simul Healthc 2016;11:82–8. 10.1097/SIH.0000000000000137 [DOI] [PubMed] [Google Scholar]
- 17. Lee MH, Lee GA, Lee SH, et al. A systematic review on the causes of the transmission and control measures of outbreaks in long-term care facilities: back to basics of infection control. PLoS One 2020;15:e0229911. 10.1371/journal.pone.0229911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hammerschmidt J, Manser T. Nurses' knowledge, behaviour and compliance concerning hand hygiene in nursing homes: a cross-sectional mixed-methods study. BMC Health Serv Res 2019;19:547. 10.1186/s12913-019-4347-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McFadden KL, Stock GN, Gowen CR. Leadership, safety climate, and continuous quality improvement: impact on process quality and patient safety. Health Care Manage Rev 2015;40:24–34. 10.1097/HMR.0000000000000006 [DOI] [PubMed] [Google Scholar]
- 20. Almoziny S, Lababidi H. CRESENT system integration Committee: an innovative approach to system integration in healthcare simulation. Adv Simul 2018;3:A2. [Google Scholar]
- 21. Huh S. How to train the health personnel for protecting themselves from novel coronavirus (COVID-19) infection during their patient or suspected case care. J Educ Eval Health Prof 2020;17:10. 10.3352/jeehp.2020.17.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schwartz J, King C-C, Yen M-Y. Protecting health care workers during the COVID-19 coronavirus outbreak -Lessons from Taiwan's SARS response. Clin Infect Dis 2020:ciaa255. 10.1093/cid/ciaa255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Su A. “Doctors and Nurses fighting Coronavirus in China die of both infection and fatigue,” Los Angeles Times (Feb. 25, 2020). Available: https://www.latimes.com/world-nation/story/2020-02-25/doctors-fighting-coronavirus-in-china-die-of-both-infection-and-fatigueAccessed [Accessed 21 Mar 2020].
- 24. Ran L, Chen X, Wang Y, et al. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis 2020:ciaa287. 10.1093/cid/ciaa287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. International Council of Nurses . High proportion of healthcare workers with COVID- 19 in Italy is a Stark warning to the world: protecting nurses and their colleagues must be the number one priority. Available: https://www.icn.ch/news/high-proportion-healthcare-workers-covid-19-italy-stark-warning-world-protecting-nurses-and
- 26. Hsu S-M, Chien L-J, Tseng S-H, et al. A No-Notice drill of hospital preparedness in responding to Ebola virus disease in Taiwan. Health Secur 2015;13:339–44. 10.1089/hs.2015.0022 [DOI] [PubMed] [Google Scholar]
- 27. Foote MMK, Styles TS, Quinn CL. Assessment of Hospital Emergency Department Response to Potentially Infectious Diseases Using Unannounced Mystery Patient Drills - New York City, 2016. MMWR Morb Mortal Wkly Rep 2017;66:945–9. 10.15585/mmwr.mm6636a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. None.


