Abstract
Background
This survey was focused on the provision of neurointerventional services, the current practices of managing patients under COVID-19 conditions, and the expectations for the future.
Methods
Invitations for this survey were sent out as a collaborative effort of the European Society of Minimally Invasive Neurological Therapy (ESMINT), the Society of NeuroInterventional Surgery (SNIS), the Sociedad Iberolatinoamericana de Neuroradiologia Diagnostica y Terapeutica (SILAN), the Society of Vascular and Interventional Neurology (SVIN), and the World Federation of Interventional and Therapeutic Neuroradiology (WFITN).
Results
Overall, 475 participants from 61 countries responded (six from Africa (1%), 81 from Asia (17%), 156 from Europe (33%), 53 from Latin America (11%), and 172 from North America (11%)). The majority of participants (96%) reported being able to provide emergency services, though 26% of these reported limited resources. A decrease in emergency procedures was reported by 69% of participants (52% in ischemic and hemorrhagic stroke, 11% ischemic, and 6% hemorrhagic stroke alone). Only 4% reported an increase in emergency cases. The emerging need for social distancing and the rapid adoption of remote communication was reflected in the interest in establishing case discussion forums (43%), general online forums (37%), and access to angio video streaming for live mentoring and support (33%).
Conclusion
Neurointerventional emergency services are available in almost all centers, while the number of emergency patients is markedly decreased. Half of the participants have abandoned neurointerventions in non-emergent situations. There are considerable variations in the management of neurointerventions and in the expectations for the future.
Keywords: stroke, intervention, standards, political, thrombectomy
The COVID-19 pandemic has caused an unparalleled disruption of public life and confronted healthcare systems with challenges unprecedented in modern history. While pneumonia and multi-organ failure has been the primary focus, there have been early reports suggesting an increased incidence of stroke secondary to large vessel occlusion in unusual populations.1 Moreover, likely due to a combination of a decline in the number of patients seeking medical attention due to fear of becoming infected, and the exhaustion of healthcare resources, the pandemic has brought widespread changes in the ability to perform urgent and time-sensitive interventions. In many regions, elective procedures were put on hold altogether, further broadening the impact on neurointerventional practices.
COVID-19 was declared a global pandemic by the WHO on March 11, 2020.2 At that time, anecdotal evidence and individual lessons gleaned were exchanged between practitioners and finally formalized in mid to end April, 2020, when the Society of NeuroInterventional Surgery (SNIS),3 the European Society of Minimally Invasive Neurological Therapy (ESMINT),4 and the Society of Vascular and Interventional Neurology (SVIN)5 published individual recommendations and guidance statements for the care of emergent neurointerventional patients in the setting of COVID-19.
At the same time, this survey was conducted as a joint effort of five national and international societies in the field of neurointerventions. Key areas of the survey were the provision of neurointerventional services in general, the current practices of managing patients under COVID-19 conditions, and the take-away lessons and expectations for the future. The aim of this survey was to understand potential geographical differences in perceptions and management of the crisis. We hypothesized that there were considerable geographical differences in the impact of COVID-19 on neurointerventional service organizations worldwide.
Methods
Invitations for participation in this anonymous online survey were sent out as a collaborative effort of the European Society of Minimally Invasive Neurological Therapy (ESMINT), the Society of NeuroInterventional Surgery (SNIS), the Sociedad Iberolatinoamericana de Neuroradiologia Diagnostica y Terapeutica (SILAN), the Society of Vascular and Interventional Neurology (SVIN), and the World Federation of Interventional and Therapeutic Neuroradiology (WFITN). Because the survey was anonymous, it is possible that several members of one team from one center answered the survey.
The survey questions (online supplementary appendix) were modified based on the learnings from an initial ESMINT survey (conducted mid-March 2020, n=136 participants) in a short but constructive discussion with the survey committee of SNIS. A more extensive agreement process with all the societies would have delayed the survey deployment. The survey results were collected between April 2 and April 20, 2020. The results are presented mainly as cumulative and relative data. Whenever statistical testing was done, a χ2 test was used with a p value of <0.05 considered to reveal a statistically significant difference. Countries were aggregated to regions (Africa, Asia, Europe, Latin America, and North America) and considered individually for the purpose of selected analyses only if five or more participants from that country provided answers.
neurintsurg-2020-016349supp001.pdf (84.6KB, pdf)
Results
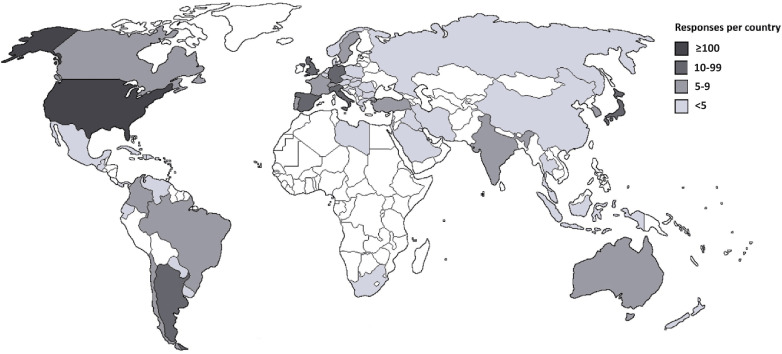
Overall, 475 participants from 61 countries responded (six from Africa (1%), 81 from Asia (17%), 156 from Europe (33%), 53 from Latin America (11%), and 172 from North America (36%) (figure 1).
Figure 1.
Number of responses per country.
Situation of Neurointerventional Services in General
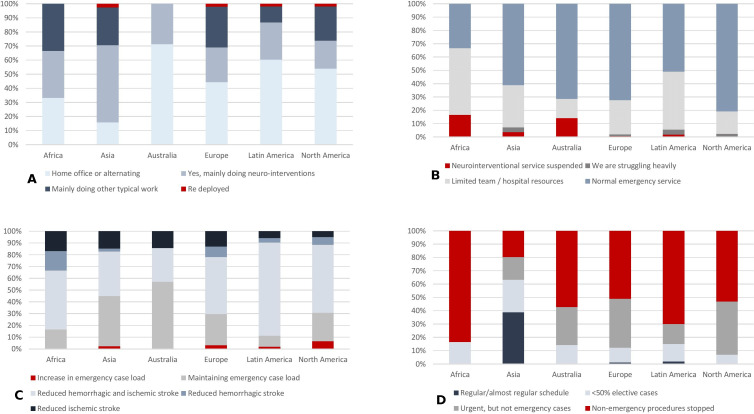
Are you (the practitioner) coming into the hospital every day? Two hundred and fourteen participants (45%) reported to be working from their home office or are alternating between home office and the hospital, typically for a week at a time; 135 (28%) of the participants reported doing mainly neurointerventions, while 117 participants (25%) reported doing mainly other typical work, such as administrative work and diagnostic readings. Only nine participants (2%) reported being re-deployed in the hospital for other tasks. There were clear differences in organizational approach between the different regions (figure 2).
Figure 2.
Situation of neurointerventional services under COVID-19 in working patterns (A), treatment of endovascular emergency cases (B), case volume in emergency cases (C), and case volume in non-emergency procedures (D).
Have you or any of your team contracted COVID-19 in 2020? Of all participants, 370 (78%) reported no COVID-19 infection among their team members, 98 (21%) had at least one team member infected, and seven (2%) were currently tested but with unknown results. The highest rates of infection were reported from Spain (16/37; 43%), the UK (5/12; 42%), and France (8/14; 36%).
Are you able to provide the usual service for emergencies (stroke, subarachnoid hemorrhage)? The overwhelming majority of participants (96%) reported being able to provide emergency services, though 26% of these reported limited team and/or hospital resources. Only 2% of the participants reported suspension of emergency services altogether (figure 2).
Have you noticed a reduction in emergency cases? There was a decrease in emergency procedures in 69% of participants (52% in ischemic and hemorrhagic stroke, 11% ischemic, and 6% hemorrhagic stroke alone) (figure 2); 27% of the participants reported no significant changes and 4% reported an increase in emergency case load (n=19). Eleven of the participants (58%) reporting an increase were located in North America. Despite this, they represented a minority even within their region, with 70% of the centers in North America reporting a decrease in emergency case volume.
How do you deal with non-emergency procedures? Only 7% of the centers reported a regular or almost regular case volume of non-emergency procedures, with by far the highest such rate in Asian countries (39%) that were less affected during the period during which the survey was conducted. In 49% of the centers, non-emergency procedures were stopped completely. Urgent, non-emergency cases were still being performed in 32% of the centers.
Current Practices of Managing Patients
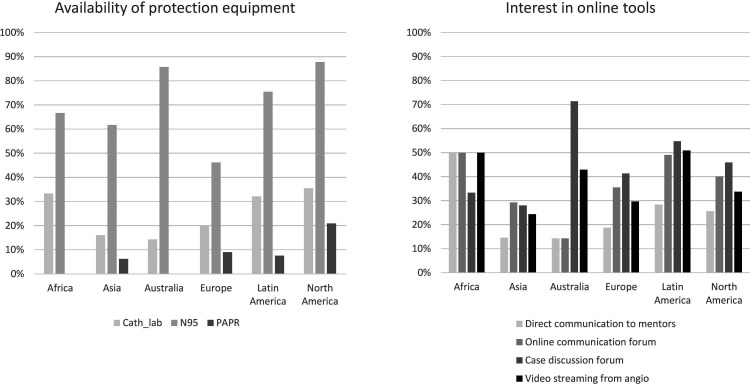
What kind of personal protection do you use for COVID+ or suspected cases? A regular face mask (with shield) as the sole protective measure was reportedly used by 95 participants (20%). A catheter lab dedicated for COVID+ patients was reported to be available for 125 participants (26%). N95 masks were available for 329 participants (69%), with considerable differences ranging from 47% in Europe to 90% in North America (figure 3). There was no statistically significant difference in the rate of COVID+ practitioners reported for teams without and with availability of specific protection measures such as angio labs dedicated for COVID+ (20% vs 22%, p=0.275), FP95 masks (19% vs 24%, p=0.169), and powered air-purifying respirators (PAPR; 20% vs 24%, p=0.806). In fact, across the board, there was a tendency towards higher availability of such protective measures in centers with higher rates of infection.
Figure 3.
Left: availability of protection equipment. Right: interest in different online tools to face future challenges with expected limited travel options. PAPR, powered air-purifying respirators.
Video consultations were used for connecting within the primary hospital (18%) and with other hospitals (11%). At least one type of video consultation was used by 21% of the participants. The rate of participants using such technology ranged from 0% (Africa) to 37% (North America).
How do you manage anesthesia in your emergency procedures? The most frequent approaches to anesthesia were to either routinely intubate all patients (41%), or to avoid intubation, unless the airway became compromised (36%). A more selective approach was followed by a minority, intubating only suspected and confirmed COVID+ patients (20% of centers) or else intubating only confirmed COVID+ patients only (5%). There was no association between the rates of COVID+ observed in teams intubating all patients routinely (43/197, 22%), as opposed to teams who only intubated when the airway was compromised (38/170, 22%).
Expectations for Developments After the Pandemic
When do you expect to re-commence to full capacity with non-emergency procedures? The majority of participants (53%) expected to be going back to full case load in less than 3 months or to see no decrease in non-emergency procedures (2%). Overall, only 6% of the participants expected that it was going to take longer than 6 months to get back to normal, and 3% were unable to provide any estimation. The national rate of participants expecting the services to normalize within 3 months varied considerably, from 20% to 88% (table 1).
Table 1.
Countries with five or more survey participants with national infection rates and expectations on the time to re-commence to full capacity of non-emergency procedures
| Survey participants | COVID-19 infections* | Expected duration to re-commence to full capacity (%) | |||||||
| Total (n) | April 2, 2020 | April 20, 2020 | Not stopped | <3 months | 3–6 months | 6–12 months | >12 months | Unclear | |
| USA | 166 | 74 | 145 | 0% | 65% | 30% | 3% | 0% | 2% |
| Japan | 41 | 2 | 9 | 5% | 45% | 31% | 10% | 2% | 7% |
| Spain | 37 | 238 | 426 | 0% | 68% | 27% | 0% | 0% | 5% |
| Germany | 22 | 78 | 177 | 0% | 41% | 41% | 5% | 14% | 0% |
| Italy | 18 | 192 | 302 | 0% | 33% | 61% | 0% | 0% | 6% |
| Argentina | 15 | 3 | 7 | 0% | 80% | 20% | 0% | 0% | 0% |
| France | 14 | 85 | 233 | 0% | 50% | 43% | 0% | 0% | 7% |
| UK | 12 | 45 | 188 | 0% | 0% | 83% | 0% | 0% | 17% |
| Brazil | 9 | 4 | 20 | 0% | 44% | 44% | 0% | 11% | 0% |
| S. Korea | 9 | 19 | 21 | 44% | 11% | 11% | 22% | 0% | 11% |
| India | 8 | 0 | 1 | 0% | 88% | 13% | 0% | 0% | 0% |
| Australia | 6 | 20 | 26 | 0% | 0% | 50% | 50% | 0% | 0% |
| Canada | 6 | 29 | 100 | 0% | 50% | 17% | 0% | 0% | 33% |
| Chile | 6 | 16 | 58 | 0% | 17% | 83% | 0% | 0% | 0% |
| Portugal | 6 | 90 | 210 | 0% | 100% | 0% | 0% | 0% | 0% |
| Sweden | 6 | 60 | 150 | 0% | 17% | 67% | 17% | 0% | 0% |
| Turkey | 6 | 22 | 111 | 0% | 33% | 33% | 33% | 0% | 0% |
| Colombia | 5 | 3 | 8 | 0% | 80% | 0% | 20% | 0% | 0% |
| Switzerland | 5 | 211 | 311 | 0% | 20% | 60% | 0% | 0% | 20% |
*Confirmed COVID-19 infections per 100 000 inhabitants at the beginning and end of survey period (source: https://coronavirus.jhu.edu/map.html).
Which methods of remote support would be suitable to you? Participants expressed most interest in secure case discussion forums (43%), an online community forum (37%), and 24/7 access to angio video streaming for live discussion (33%). Preferences clearly differed between continents (figure 3). At least one of the methods of remote support was deemed suitable by 182 participants (38%), two methods by 86 participants (18 %), three methods by 49 participants (10%), and four methods by 44 participants (9%); and 114 participants (24%) reported no suitable method.
Discussion
This survey, conducted between April 2 and April 20, 2020, provides a snapshot in the development of the COVID-19 pandemic. Countries were in different phases of the pandemic, with resultant varying effects on healthcare systems, at the time the survey was performed. The results of this survey provide a broad picture of the current situation for countries affected by the COVID-19 pandemic and are not necessarily representative for the true conditions in each country. The data are estimates from the neurointerventional physician perspective and do not necessarily reflect quantitative case volumes.
Neurointerventional emergency service was being maintained according to the vast majority of the participants (96%), while the emergency case load was reportedly decreasing according to 69% of the participants, in most cases affecting both ischemic and hemorrhagic stroke. An absolute increase in emergency case volume was reported by 4% of the participants only. One logical explanation for the decrease is a reduced number of transfers from referring hospitals.6 Another factor might be patients’ fear at the prospect of coming to the hospital during the pandemic. This assumption is supported by the decreased number of patients presenting, in particular with minor strokes and transient ischemic attacks.6 At the same time longer onset-to-door and door-to-treatment times have been observed in patients with major strokes.6 The centers reporting a stable or even increasing case load may be the centers that remain open in their geographical area where others have seized their acute interventions and transfer patients to the major hub. A quantitative analysis of these data is ongoing in many centers and is expected to be published in the coming months.
Non-emergency procedures were stopped altogether in the centers of half of the participants worldwide. This rate was lowest in Asia (20%) with 51/81 responses coming from Japan and South Korea, where the infection rate was low among the population at the time of the survey. In-hospital acquisition of COVID-19 may represent a considerable problem.7 Urgent, non-emergency cases were abandoned by about half of the participants. Canceling or postponing urgent procedures could be detrimental to patients who have a higher risk of imminent stroke than they do of being harmed by potential nosocomial infection. Balancing the risks of a delayed therapy versus the risk of a potential nosocomial COVID-19 infection is a challenge. Communicating these considerations to patients is likely to be even more difficult. Patients might avoid coming to the hospital out of fear, both for emergencies and urgent procedures.
There are considerable differences in the availability of protective equipment and dedicated treatment areas (figure 3). Participants from North America report the highest rate of catheter labs dedicated for COVID-19 patients, the highest rate of availability of N95 masks and, by far, the highest rate of availability of PAPR. It is quite alarming that N95 masks were available for only about half of the participants in Europe. However, protective equipment availability can change rapidly. Interestingly, there was no association between the availability of protective equipment and the rate of COVID-19 infections among the neurointerventional team members. It is difficult to draw firm conclusions from this lack of association, as such equipment might be made available where there is a sense of urgency based on an overall deteriorating situation, with rising population infection rates.
The majority of participants (52%) expected to go back to full case load in less than 3 months, while only 6% of participants expected that a lower case load would last longer than 6 months. North Americans were the most optimistic about the speed of recovery (table 1).
One major result of the COVID-19 pandemic and the need for social distancing is the rapid adoption of remote communication, particularly using conferencing tools. At least one type of video consultation was reportedly currently being used by 21% of the participants already, either within the hospital or to connect with other hospitals (11%). Thirty-three percent of participants from all societies were interested in having access to 24/7 remote physician support via a live streaming platform. The interest in this technology ranged from 24% in Asia to 51% in Latin America (figure 3). With the decrease in cases being performed, many programs have modified their coverage models to reduce resident exposure and risk, while also allowing for backup options should physicians fall ill or come under quarantine.8 Neurointerventional teams are typically small. Splitting them into alternating teams may result in having more senior or more junior team members in the hospital at any given time. A recent study confirmed the feasibility of remote mentoring of thrombectomy procedures.9 This technology could now prove instrumental in including senior advice and guidance in emergency situations. This may remain critical in the future, as travel options may remain limited for an extended period of time.
Limitations
Systematic bias could have been introduced both by the relatively high rate of responses from countries that were most affected (eg, Spain, table 1) and by the different success in activating the available neurointerventionalists in general. The responses by country were limited to fewer than five responses for two thirds of the countries. For this reason, the countries were aggregated by continent, even in the presence of a substantial heterogeneity among the countries within a continent. Many more survey questions could have been asked. Any survey is a trade-off between complexity and the number of participants willing to complete the survey. Our focus was to achieve a high number of responses and we expected that a more complex survey would have led to lower participation and to considerable sampling and non-response bias.
Conclusion
Neurointerventional emergency services are available in almost all centers at present, while the number of emergency patients is reportedly markedly decreased in the vast majority of the centers. Half of the participants have abandoned neurointerventions in non-emergent situations. There are considerable variations in the management of neurointerventions during the COVID-19 pandemic and in the expectations for the future.
Acknowledgments
The authors thank the members of the participating societies for their valuable contribution.
Footnotes
Twitter: @CDiazNeuroInter, @JoshuaAHirsch, @italolinfante, @docroc99
Contributors: JF: Designing the research plan, conducting the data analysis and drafting the manuscript, PB, CD, JAH, ZK, DL, IL, PL, WJ, JM, RN, DBO, JMMP, MT, AT: Critically revising the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: Consultancy: Acandis, Bayer, Boehringer Ingelheim, Cerenovus, Medtronic, Microvention, Stryker, CD: Proctor Medtronic. DL: Consultant to Cerenovus, Genentech, Stryker, Medtronic as Imaging Core Lab. WJ: Consultancy: Rebound Therapeutics, Integra, Viseon, Imperative Care, Medtronic, Q’Apel, Stream Biomedical, Spartan Micro; Investor: Cerebrotech, Endostream, Viseon, Rebound, and Spartan Micro, JMM: Disclosures are: Penumbra: speaker’s bureau, Stryker: Consultant.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. No patient data included.
References
- 1. Oxley TJ, Mocco J, Majidi S, et al. . Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med 2020;382:e60. 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahajan A, Hirsch JA. Novel coronavirus: what neuroradiologists as citizens of the world need to know. AJNR Am J Neuroradiol 2020;41:552–4. 10.3174/ajnr.A6526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fraser JF, Arthur AS, Chen M, et al. . Society of neuroInterventional surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19. J Neurointerv Surg 2020;12:539–41. 10.1136/neurintsurg-2020-016098 [DOI] [PubMed] [Google Scholar]
- 4. Aggour M, White P, Kulcsar Z, et al. . European Society of Minimally Invasive Neurological Therapy (ESMINT) recommendations for optimal interventional neurovascular management in the COVID-19 era. J Neurointerv Surg 2020;12:542–4. 10.1136/neurintsurg-2020-016137 [DOI] [PubMed] [Google Scholar]
- 5. Nguyen TN, Abdalkader M, Jovin TG, et al. . Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the Society of Vascular and Interventional Neurology. Stroke 2020;51:1896–901. 10.1161/STROKEAHA.120.030100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baracchini C, Pieroni A, Viaro F, et al. . Acute stroke management pathway during coronavirus-19 pandemic. Neurol Sci 2020;41:1003–5. 10.1007/s10072-020-04375-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang D, Hu B, Hu C, et al. . Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. 10.1001/jama.2020.1585. [Epub ahead of print: 07 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bambakidis NC, Tomei KL, Editorial TKL. Editorial. impact of COVID-19 on neurosurgery resident training and education. J Neurosurg 2020:1–2. 10.3171/2020.3.JNS20965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bechstein M, Buhk J-H, Frölich AM, et al. . Training and supervision of thrombectomy by remote live streaming support (RESS) : randomized comparison using simulated stroke interventions. Clin Neuroradiol 2019. 10.1007/s00062-019-00870-5. [Epub ahead of print: 20 Dec 2019]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2020-016349supp001.pdf (84.6KB, pdf)