Abstract
Measures of physical functioning are among the strongest predictors of mortality, but no previous study has assessed whether the predictive value of such measures varies by race/ethnicity, as has been done for the simple self-rated health question. The current study tests whether the relationship between two measures of physical functioning (the number of self-reported functional limitations and measured walking speed) and mortality is weaker (has a lower hazard ratio) for Latinos and blacks than for whites. Data were drawn from the 1998–2014 waves of the Health and Retirement Study, with mortality follow-up through 2016. We used Cox hazard models with household random effects to test for interactions between race/ethnicity and these measures of physical functioning and verified earlier findings for self-rated health. The number of self-reported functional limitations is significantly related to mortality for all racial/ethnic groups, but has a substantially lower hazard ratio for blacks and Latinos than for whites, as hypothesized. This hazard ratio remains lower for blacks and Latinos after adjustment for sociodemographic characteristics and health conditions. These findings suggest that the higher rates of functional limitations observed among Latinos and blacks compared with whites may reflect a history of strenuous physical work, inadequately controlled pain, lower leisure-time physical activity, or untreated/under-treated mobility problems that can lead to reduced physical performance without necessarily having a substantial effect on mortality risk. On the other hand, we do not detect significant racial/ethnic differences in the association between measured walking speed and subsequent mortality. This may be a result of the smaller sample size for the walking speed tests, the more nuanced nature of the continuous walking speed measure, or the fact that the walking speed test captures only a subset of the limitations included in the self-reports.
Keywords: Mortality, physical functioning, functional limitations, race/ethnicity
1. Introduction
Physical limitations, such as difficulties walking, carrying, or lifting, are strongly predictive of survival throughout the life course. Because physical limitations are believed to emerge largely from serious or chronic illnesses, such as heart disease and stroke (Verbrugge & Jette, 1994), the large mortality risk associated with them is not surprising. What is surprising, however, is that the association is likely to vary by race/ethnicity. Most research indicates that Latinos, both immigrants and US-born, have higher rates of disability and functional limitations than non-Latino whites (Boen and Hummer 2019; Angel et al. 2014; Haas and Rohlfsen 2010; Hayward et al. 2014). This Latino disadvantage occurs even though this group has a distinct survival advantage over whites: Latinos have life expectancies at least as high as, and often higher than, whites, despite their lower average socioeconomic status and poorer access to health care, a pattern referred to as the Latino or Hispanic mortality paradox (Abraido-Lanza et al. 1999; Markides and Eschbach 2005). Together, these two findings for Latinos—more functional limitations yet lower mortality than whites—strongly suggest that physical functioning may be more weakly associated with mortality for Latinos than for whites.
Despite growing interest in developing better algorithms to predict survival, recent emphasis has been on inclusion of large amounts of clinical information rather than on self-reported health-related variables, even though recent findings indicate that self-reported measures are often more powerful predictors of survival than biological markers (Goldman et al. 2016). Moreover, prognostic research typically fails to recognize that the strength of a prediction may vary considerably within a population according to an individual’s social and demographic characteristics, such as race/ethnicity.
One exception to the paucity of research in this area has been a set of analyses that examine how the association between the simple self-rated health (SRH) question – i.e., respondents rate their overall health typically using one of five adjectives – varies across racial/ethnic groups. Most of these studies conclude that SRH is more weakly associated with survival for both blacks and Latinos than for whites (Assari et al. 2016; Lee et al. 2007; Woo and Zajacova 2016). Because SRH is a subjective global assessment that is influenced by cultural and social factors and depends on the underlying reference group (Idler et al. 1999; Jylhä 2009), this racial differential may not apply to reported measures of specific physical limitations, which are believed to be more objective.
A second exception is a recent study that explored racial/ethnic variability in a broad set of health-related predictors (Goldman et al. 2017). These researchers concluded that measures of self-reported functional limitations and disability were among the top 10 predictors for each racial/ethnic group and that the predictive power of these measures appeared to be stronger for whites than for Latinos and blacks, although the methods used did not permit a clear test of this relationship.
These prior studies suggest that functional limitations may also have a weaker association with survival for blacks than for whites. In contrast to patterns for Latinos, however, this would not create the apparent paradox between rates of functional limitations and survival relative to whites. Blacks have rates of disability and functional limitations that are considerably higher than those for whites (Boen and Hummer 2019; Haas and Rohlfsen 2010; Melvin et al. 2014), consistent with their lower life expectancy.
To the best of our knowledge, to date no study has tested whether physical functioning is less strongly associated with mortality among racial/ethnic minorities. Our objective is to fill this gap in the literature by investigating whether the relationship between physical functioning and survival varies by race/ethnicity. Using the hazard ratio as our metric, we examine the magnitude of the association between survival and two types of measures of physical functioning – self-reports and performance tests – for three groups: Latinos, whites and blacks. In the remainder of the paper, we use the term Latino synonymously with Hispanic and the terms whites and blacks for non-Hispanic whites and non-Hispanic blacks. These two types of measures, sometimes thought of as subjective vs. objective assessments of physical functioning, are both predictive of downstream health and survival and are clearly correlated, yet they appear to capture distinct constructs (Andrasfay 2020; Goldman et al. 2014), and provide a unique opportunity to assess the consistency of findings across measures. For comparison with earlier studies, we also estimate racial/ethnic variation in the association between the simple SRH question and survival. An additional aim of this study is to assess the extent to which sociodemographic characteristics, health-related behaviors, or comorbid conditions explain the racial/ethnic variation that we detect.
The remainder of the paper is organized as follows. Section 2 reviews the disablement process and racial/ethnic differences in this process; Section 3 describes the data and analytic strategy; Section 4 presents our results; and Section 5 concludes with a discussion.
2. Background
2.1. The disablement process
Our theoretical framework builds upon a model known as the disablement process – a stylized aging progression through which individuals acquire underlying pathology, which, in turn, results in impairments, physical limitations, disability, and ultimately, death (Verbrugge and Jette 1994). Far from being a uniform, linear development through these stages, the disablement process can manifest in different ways: individuals need not progress through each stage of the process or they may experience improvements in health and move in reverse (Crimmins et al. 2004; Latham et al. 2015; Verbrugge and Jette 1994). Additionally, the speed at which individuals progress through these stages can vary depending on their risk factors, underlying pathology type and severity, and mediating factors including medical care, the environment, and lifestyle (Crimmins 2004; Kail et al. 2018; Verbrugge and Jette 1994). Many of the underlying pathologies responsible for physical decline, including hypertension, diabetes, cardiovascular disease, inflammation, and smoking-related illnesses, are also strongly associated with mortality, while others, including osteoarthritis and injuries, are not (Crimmins et al. 2004; Kail et al. 2018; Rosano et al. 2011; Van Oyen et al. 2014; Verbrugge and Jette 1994; Verghese et al. 2011).
2.2. Racial/ethnic differences in the disablement process
Figure 1, adapted from Verbrugge and Jette (1994), summarizes the disablement process and underscores the many opportunities for racial/ethnic differences to intervene. To begin with, there is substantial variation in risk profiles, which may result in differential accumulation of pathologies and impairments. Several scholars have speculated that, compared with other racial/ethnic groups, the high prevalence of functional impairments and disability among Latinos may be driven more by the types of physically demanding and dangerous jobs that Latinos are likely to hold rather than by rates of chronic illnesses (Goldman, 2016; Hayward et al. 2014; Sheftel and Heiland 2018). Latinos, especially foreign-born Latinos, as well as blacks, are more likely than whites to hold lower-skilled, physically demanding occupations that are associated with workplace injuries and musculoskeletal disorders (Del Río and Alonso-Villar 2015; Seabury et al. 2017; Toussaint-Comeau 2006). These injuries and disorders can result in diminished functioning but are not inherently fatal.
Figure 1:
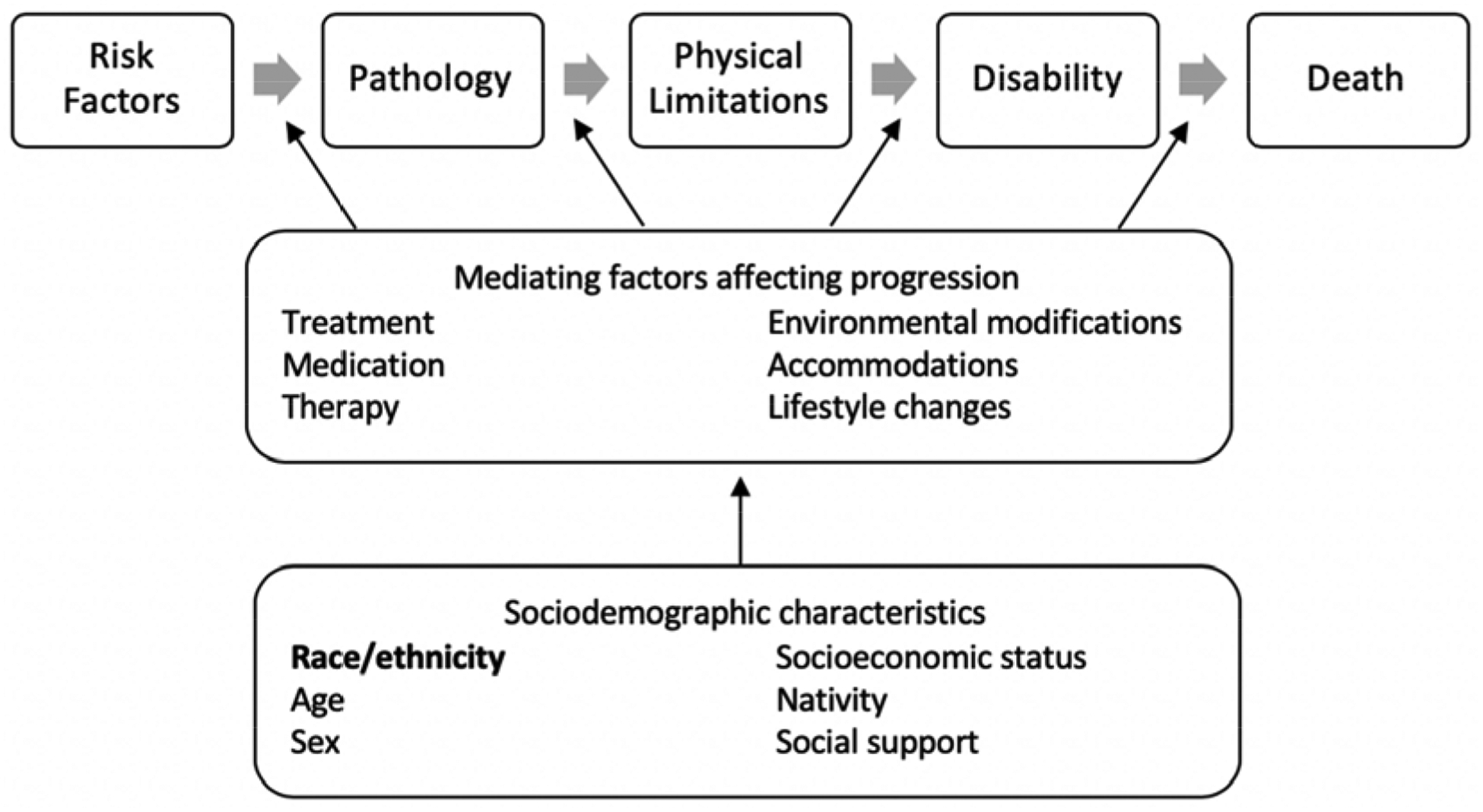
The Disablement Process. Adapted from Verbrugge and Jette (1994).
There are also racial/ethnic differences in behavioral risk factors. Black and Latina older women have a higher prevalence of obesity than older white women (Fakhouri and Kit 2012; Flegal et al. 2012). Though less strongly related to mortality at older ages, both overweight and obesity are associated with functional limitations and disability at older ages (Alley and Chang 2007; Jenkins 2004; Snih et al. 2007). Compared to whites, Latinos are much less likely to have been smokers, a behavioral advantage that is responsible for much of the Latino mortality advantage (Fenelon 2013; Lariscy et al. 2015). In contrast, blacks are at least as likely to have smoked as whites and have lower cessation rates, a disadvantage that accounts for part of the black-white gap in older adult mortality (Ho and Elo 2013). Smoking is also related to physical functioning decline and disability onset through its effects on lung function decline and fatal chronic conditions (Rostron et al. 2014; Van Oyen et al. 2014).
After the onset of pathology and physical limitations, blacks and Latinos are less likely than whites to receive care to improve their quality of life or to prevent further functional decline. Such undertreatment often has a notable impact on physical function, for example, through higher levels of pain or restricted mobility, while having little effect on survival. Several studies have documented that blacks and Latinos are more likely to have their pain underestimated by physicians and are less likely to receive prescriptions to treat their pain (Cintron and Morrison, 2006; Mossey 2011). Blacks and Latinos are also more likely than whites to experience disability associated with arthritis, one of the most common chronic conditions among older adults and a major cause of functional limitations (Dunlop et al. 2001) although not of mortality.
Given these varying risk profiles and use of buffering resources by race/ethnicity, we hypothesize that physical limitations may have a different etiology among Latinos and blacks, such that the link between these limitations and survival may be weaker for these groups than for whites.
3. Data and Methods
3.1. Data
Data are drawn from the Health and Retirement Study (HRS), which began in 1992 as a longitudinal study of older American adults and their spouses who were interviewed every two years about their health, finances, work and retirement, and family. Subsequent waves added additional birth cohorts, and, beginning with the 1998 wave, the HRS became nationally representative of adults over age 50 (Sonnega et al. 2014). Additional in-home physical functioning tests were first administered in 2004 to a random subsample of HRS respondents; beginning with the 2006 wave, these tests were administered to alternating halves of the HRS sample (Crimmins et al. 2008). For our analyses, we use data from the 1998 – 2014 waves and mortality follow-up through the 2016 wave. These data were compiled from the RAND HRS 2014 file (version 2) (RAND 2018), the HRS 2014 tracker file (Health and Retirement Study 2017), and the HRS 2016 tracker file (Health and Retirement Study 2019).
3.2. Sample Restrictions
Of the 33,493 individuals in the HRS between 1998–2014, we restricted our analysis to sampled respondents and their spouses at initial interview who reported a race/ethnicity of white, black, or Latino, and to person-waves in which the individual was at least 50 years of age. We include waves in which the interview was completed via a proxy.
Because we are interested in both self-reported functional limitations and performance-based measures of walking speed, and the latter are not available in all waves, we define two analytic samples. The first, the full sample, contains all person-waves described above [N = 160,647 observations (67,360 male, 93,287 female) of 30,494 respondents (13,233 male, 17,261 female)]; on average, respondents participated in 5.3 waves. The second, the walking speed assessment subsample, is restricted to individuals who participated in the in-home walking speed tests, which were administered only to respondents aged 65 and older. This sample includes 39,835 observations (16,413 male, 23,422 female) of 11,857 respondents (4,993 male, 6,864 female). Respondents could participate in up to four waves of in-home physical performance tests. In the walking speed assessment subsample, respondents participated in an average of 1.9 walking speed tests.
3.3. Measures
3.3.1. Mortality
The outcome variable, mortality, is ascertained by the HRS either through linkage to the National Death Index (NDI) or ongoing mortality surveillance (Sonnega et al. 2014). Deaths occurring through the end of 2011 have been verified by the HRS against the NDI (Weir 2016). Where possible, we use the decedent’s NDI-verified date of death; otherwise, we use the month and year of death reported (a) during the respondent’s exit interview by the respondent’s next-of-kin, (b) during the spouse’s core interview, or (c) during follow-up attempts. Respondents without a reported date of death are censored at the month and year they were last known alive to the HRS, typically their (or their spouses’) last interview or the last time they were contacted by the HRS. Following HRS convention, we impute the day of death or censoring to be the last of the month.
3.3.2. Physical Functioning and Self-Rated Health
In each wave, respondents were asked to report whether they experience difficulty with 11 physical activities, excluding temporary difficulties that the respondent expects to last less than three months. We consider the respondent to have a functional limitation if the respondent reports he/she has difficulty, cannot do, or does not do a particular task. We sum the number of limitations from 11 physical activities: walking several blocks; walking one block; sitting for two hours; getting up from a chair; climbing several flights of stairs without resting; climbing one flight of stairs without resting; stooping, kneeling or crouching; extending arms above shoulders; pushing or pulling large objects; lifting or carrying at least 10 pounds; and picking up a dime. This results in a measure of functional limitations ranging from 0 to 11.
Our main interest is in functional limitations, but we include SRH for comparison with previous studies. Respondents were asked to rate their overall health at each wave as excellent, very good, good, fair, or poor. We dichotomize this measure as fair/poor SRH versus all other categories.
In addition to the count of self-reported functional limitations and SRH, we include a performance-based measure of normal walking speed. The HRS includes additional performance-based measures (grip strength, peak expiratory flow, and balance tests), but we include only walking speed as it is the measure most closely related to the mobility components of the respondents’ self-reported functional limitations. We distinguish between two types of missing values for this measure. We consider respondents to be completely missing the measurement if they were not in the sample randomly selected to participate in the enhanced face-to-face interview for a given wave; they were ineligible due to age; they refused; they did not understand the instructions; there was no suitable space to conduct the test; the equipment malfunctioned; or there was some “other” reason given. In contrast, we consider a respondent to be unable to perform a test if measurement is missing for the following reasons: the respondent or interviewer felt it would be unsafe; the respondent tried but could not complete the test; the respondent could not stand; or the respondent had a health condition that would contraindicate participating in the test, including recent surgery or injury. There are up to six reasons given for why the respondent did not perform the task; we take the first reason given to determine whether the respondent was unable or otherwise missing (i.e., ineligible, refused, etc.).
Normal walking speed (meters/second) was measured by the interviewer as the respondent walked 2.5 meters (98.5 inches) at a normal pace, with a walking aid if necessary. The respondent was asked to perform this walk twice; the faster of the two trials is used in our analysis. In our analytic models, we use an indicator for inability to perform the walking speed test, standardized walking speed, and a quadratic term for walking speed to allow for nonlinear associations between walking speed and mortality.
3.3.3. Covariates
In addition to the key variable of interest–race/ethnicity defined as white, black, or Latino—we include a set of demographic, socioeconomic, and health-related variables that have been shown to be correlated with physical functioning and/or survival (Crimmins 2004; Verbrugge and Jette 1994). Many of these variables have different distributions by race/ethnicity (Cintron and Morrison 2006; Dunlop et al. 2001; Fakhouri et al. 2012; Fenelon 2013; Flegal et al. 2012; Ho and Elo 2013; Mossey 2011) and thus may contribute to racial/ethnic variation in the association between physical functioning and survival.
Demographic characteristics include sex, an indicator for whether the respondent is married, and nativity (foreign-born vs. native-born). Socioeconomic status is captured by years of education (centered on 12 years), log household income, and log household wealth (individuals with negative or zero household income or household wealth are coded as having $1). The wave of the HRS is included as a measure of time.
Variables reflecting health conditions include self-reports of ever receiving a diagnosis from a doctor of the following conditions: stroke, high blood pressure, diabetes, and arthritis. We also include the following health-related behaviors: indicators for whether the respondent ever smoked, was ever obese (derived from their report of maximum weight and height at first interview), and is often troubled by pain. In the models of walking speed, we additionally include respondent’s height, as walking speed is influenced by height (Samson et al. 2001).
3.3.4. Missing Data and Time-Varying Covariates
Missing data on self-reported demographic and health characteristics were imputed using the Amelia package in R to produce 10 data sets (Honaker et al. 2011). The imputation procedure included all variables described above and their lags and leads, i.e., prior and subsequent values of a time-varying variable are used to predict the current value of a variable. The frequency of missing values at first observation is noted in Table 1.
Table 1:
Unweighted Summary Statistics of Analytic Samples at First Observation
| Full Sample | Walking Speed Subsample | |||
|---|---|---|---|---|
| Mean (SD) or Percent | Percent Missing | Mean (SD) or Percent | Percent Missing | |
| Demographics | ||||
| Age (years) | 63.2 (10.8) | 0 % | 73.8 (7.1) | 0 % |
| Female | 56.6 % | 0 % | 57.89 % | 0 % |
| Race/Ethnicity | 0 % | 0 % | ||
| White | 69.87 % | 77.56 % | ||
| Black | 18.27 % | 13.68 % | ||
| Latino | 11.86 % | 8.76 % | ||
| Married | 63.38 % | 0.1% | 59.42 % | 0.02 % |
| Foreign-born | 11.4 % | 0.05 % | 8.96 % | 0.07 % |
| Died in follow-up period | 39.07 % | 0 % | 33.95 % | 0 % |
| Mean follow-up (years) | 11.2 (5.9) | 0 % | 6.9 (3.3) | 0 % |
| Socioeconomic Characteristics | ||||
| Education (years) | 12.2 (3.4) | 0.28 % | 12.3 (3.2) | 0.04 % |
| Household income | $58,000 ($98,900) | 0 % | $55,200 ($119,400) | 0 % |
| Household wealth | $309,900 ($1,044,000) | 0 % | $521,000 ($1,205,000) | 0 % |
| Health Characteristics | ||||
| Often troubled by pain | 30.3 % | 0.11 % | 34.19 % | 0.08 % |
| Ever smoked | 58.13 % | 0.45 % | 57.34 % | 0.45 % |
| Ever diagnosed with arthritis | 43.82 % | 0.10 % | 66.08 % | 0.10 % |
| Ever diagnosed with diabetes | 14.33 % | 0.08 % | 22.75 % | 0.14 % |
| Ever diagnosed with high blood pressure | 43.74 % | 0.1 % | 62.48 % | 0.15 % |
| Ever had a stroke | 6.28 % | 0.05 % | 9.74 % | 0.10 % |
| Obese at maximum weight | 46.44 % | 18.59 % | 46.04 % | 1.23 % |
| Number of limitations | 2.7 (3.1) | 0.89 % | 3.3 (3) | 0.41 % |
| Fair/poor self-rated health | 31.27 % | 0 % | 29.26 % | 0 % |
| Walking speed (meters/second) | 0.8 (0.3) | 0 % | ||
| Unable to perform walking speed task | 7.19 % | 0 % | ||
| Number of respondents | 30,494 | 11,857 | ||
| Number of observations | 160,647 | 39,835 | ||
Notes: Means and percentages are defined for respondents not missing the variable. These statistics refer to the first observation of a respondent in the sample.
All measures, with the exception of sex, race/ethnicity, nativity, and years of education, are treated as time-varying. Because the timed walks are not conducted at every wave, performance on this test is carried forward in future waves until it is updated in a subsequent enhanced face-to-face interview. In cases where a respondent participates or is unable to complete the test in one wave but refuses to participate or is missing in a future wave, the original value or indicator of inability is carried forward to the next wave. Self-reported variables are updated with every wave.
3.4. Methods
We focus the analysis on assessing variability in the magnitude of the association between physical functioning and mortality by race/ethnicity. We do so by comparing hazard ratios of mortality across groups from a series of survival models. We first estimate a base model including only sex, race/ethnicity, the measure of physical functioning/health, and the interaction between race/ethnicity and the measure of physical functioning/health. This base model allows us to establish whether physical functioning is less predictive of mortality (i.e., has a smaller hazard ratio) among black and Latino older adults compared with whites. Second, we estimate a full model including all covariates described above in order to determine whether racial/ethnic variation in the association between physical functioning and mortality can be explained by sociodemographic characteristics, health-related behaviors, or comorbid conditions. In these models, the interest is on the interaction terms between race/ethnicity and the measure of physical functioning or health (the number of functional limitations, SRH, or walking speed). We separately fit each of these models including only one of the following predictors at a time (and its interaction terms): the count of functional limitations, fair/poor self-reported health, or walking speed.
We estimate these models using Cox proportional hazards, a nonparametric survival model. The time-clock for these models is age at interview; respondents are considered at risk of mortality until death or censoring. These survival models do not include survey weights because we include demographic variables related to sample selection as covariates, a method that produces unbiased and efficient estimates (Solon et al. 2015; Winship and Radbill 1994). Moreover, we address the clustered nature of the data that arises from the HRS interviewing respondents and their spouses by including household random effects in the hazard models. This allows us to account for shared frailty between spouses, a well-documented phenomenon that may arise from shared behaviors and environment of married couples and a “widowhood effect” following bereavement (Moon et al. 2011). These models are summarized in equation 1.
| Equation 1 |
where λij(a) denotes the hazard of mortality for individual i in household j at age a, λ0(a) denotes the baseline hazard at age a (the age-specific risk of mortality for individuals with all Xij = 0 and hj = 0), Xij represents a vector of time-varying covariates, including some with interactions with age (see below), and hj is the household random effect, which is distributed normally with mean 0 and variance .
Preliminary models revealed that the proportional hazards assumption was violated for the following predictors: sex, race/ethnicity, marital status, number of limitations, fair/poor SRH, inability to complete walking speed test, ever smoking, arthritis, often troubled by pain, and diabetes. We address this issue by including interactions between these predictors and age, thereby allowing the effects of the specified covariates to vary by age (i.e., to be non-proportional across the age span in this analysis). Because these interactions render the regression results difficult to interpret, we present results from these models as hazard ratios at three selected ages (60, 70, and 80). All hazard ratios presented are pooled estimates from analyses that were run individually on each of 10 imputed data sets and combined to account for the uncertainty associated with these imputations (Rubin 2004).
4. Results
4.1. Descriptive Statistics
Table 1 displays the unweighted summary statistics of the analytic samples and the frequency of missing data for the first observation of each respondent. Summary statistics are displayed by race/ethnicity in Appendix Table A1. In both samples, compared to white respondents, Latino and black respondents are younger, have lower educational attainment, lower household income and wealth, and they are more likely to report being troubled by pain, ever having been diagnosed with diabetes, and having a maximum weight that would be classified as obese. Blacks are the most likely, while Latinos are the least likely, to have ever had a stroke. On average, in the full sample, blacks report the highest number of functional limitations at first observation (3.2), followed by Latinos (2.9) and whites (2.6), while Latinos are most likely to report fair/poor SRH (47%), followed by blacks (41%) and whites (26%). In the walking speed subsample, both blacks and Latinos have slower average walking speeds (0.7 meters/second) than whites (0.9 meters/second). Blacks are more likely to be unable to perform the walking speed task (12.3%) compared to Latinos (7.8%) and whites (6.2%).
4.2. Associations between physical functioning and mortality
The results are displayed in two sets of figures. The first set is based on observed hazard rates for specified numbers of limitations, and, separately, by category of self-reported health status, for the three racial/ethnic groups. The second set presents estimated hazard ratios for specified ages for the three racial/ethnic groups derived from the two statistical models described above (the base model and the full model), separately for self-reported limitations, self-reported health, and walking speed.
Figure 2 displays the smoothed observed log hazard of mortality by age and self-reported number of limitations, stratified by race/ethnicity. The numbers of limitations displayed (0, 2, and 5) refer approximately to the 25th, 50th and 75th percentiles. Among whites at any given age, larger numbers of limitations are associated with a notable increase in the mortality hazard. Among Latinos, however, the difference in hazard rates between 2 and 5 limitations is often small, and, among blacks, there is virtually no difference in the hazard rates between 0 and 2 limitations. Figure 3 displays corresponding smoothed log hazards by self-rated health status. Here too there is evidence of a stronger relationship between SRH and mortality among whites than among blacks and Latinos, as shown by a wider gap among whites between excellent/very good/good and fair/poor health at most ages.
Figure 2:
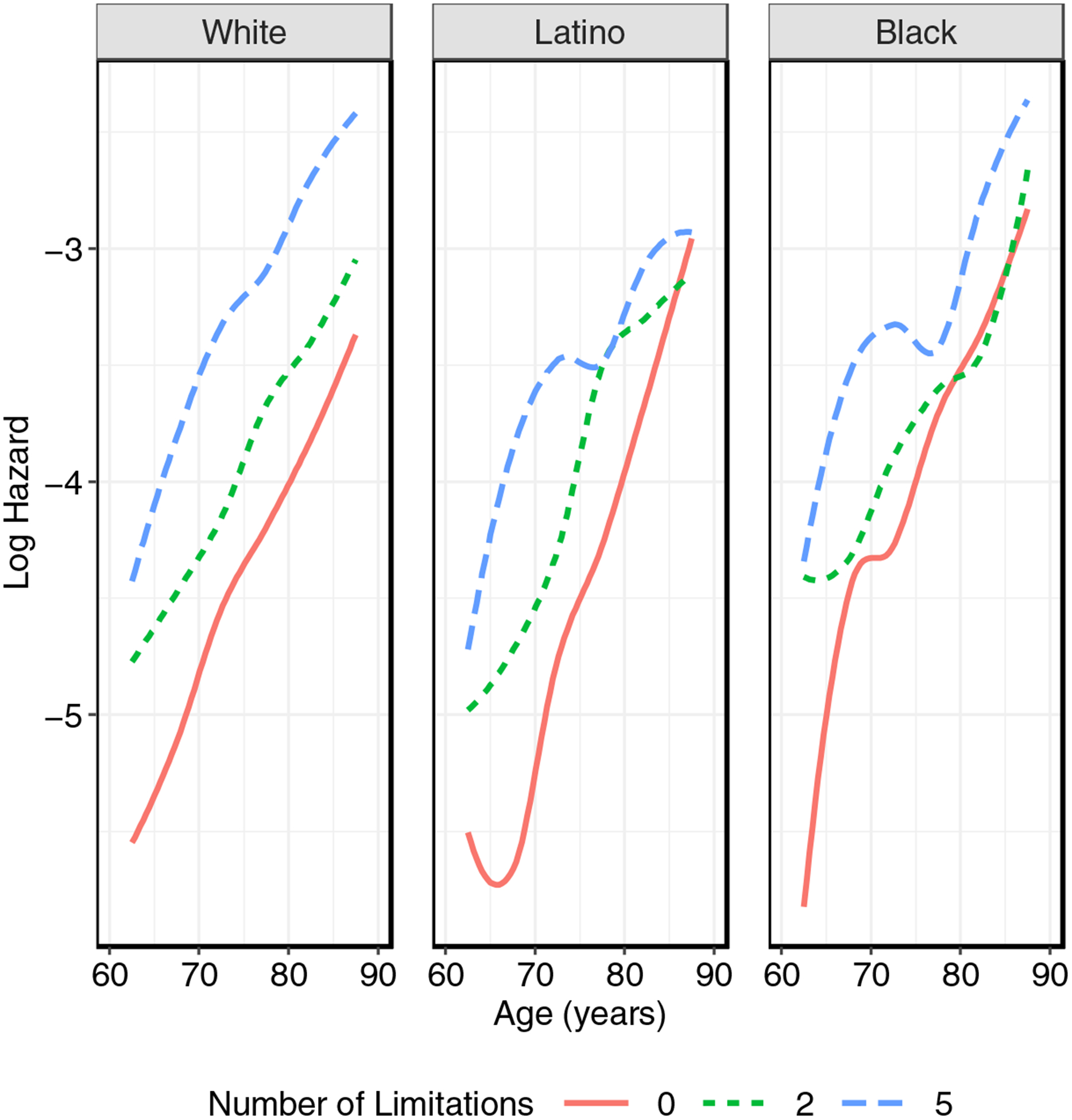
Observed smoothed log hazard of mortality by age, self-reported number of limitations, and race/ethnicity. The numbers of limitations displayed (0, 2, and 5) refer approximately to the 25th, 50th and 75th percentiles.
Figure 3:
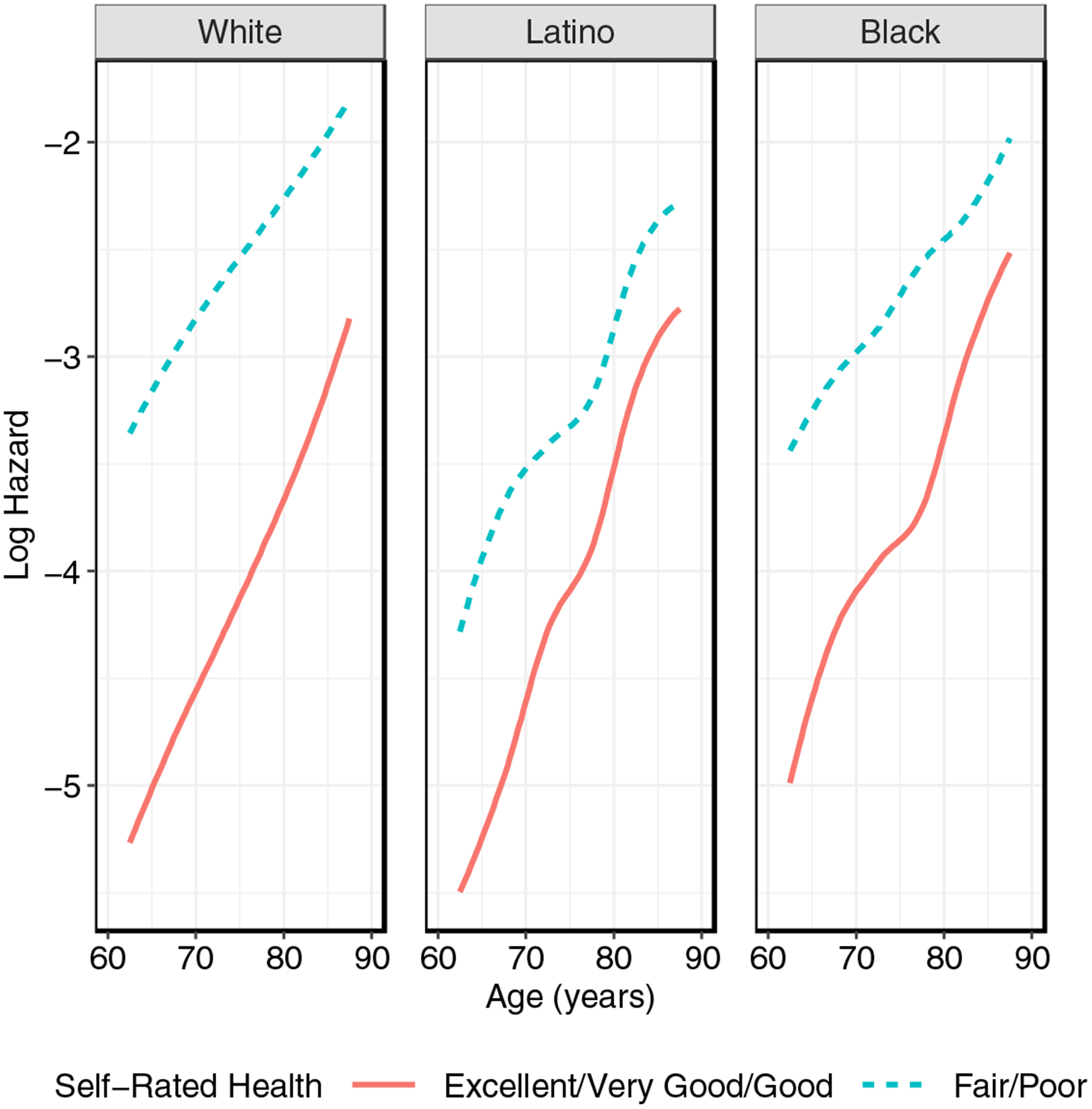
Observed smoothed log hazard of mortality by age, self-rated health, and race/ethnicity.
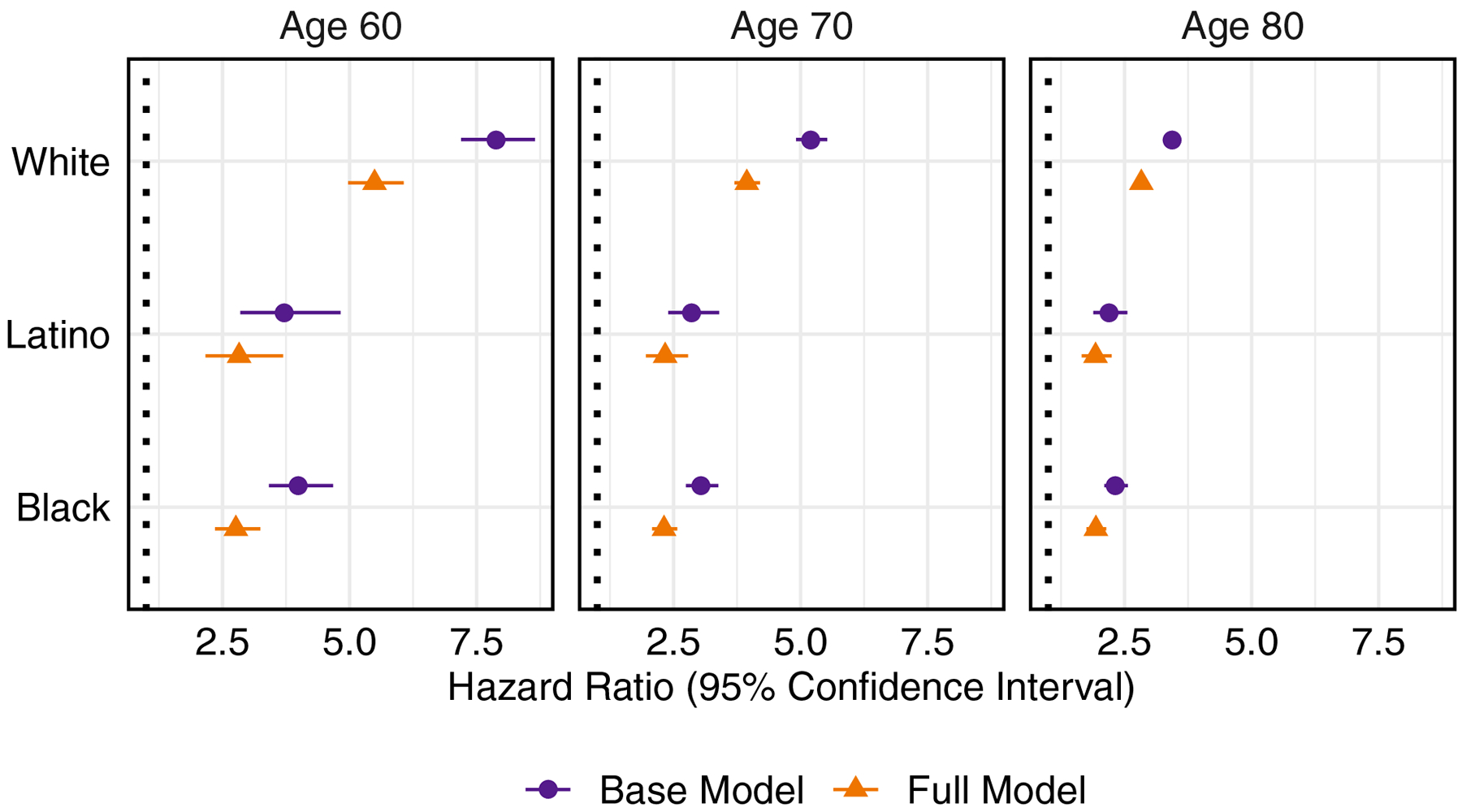
Figure 4 displays hazard ratios and 95% confidence intervals for the self-reported number of limitations by race/ethnicity at ages 60, 70, and 80 from the base and full models. These hazard ratios and confidence intervals are displayed in Appendix Table A2, and the hazard ratios for all variables in these models are shown in Appendix Table A3. For all racial/ethnic groups, the number of limitations becomes less predictive of mortality with increasing age. At each of these ages, the hazard ratio associated with an additional limitation is largest for whites, and significantly lower for Latinos and blacks. These hazard ratios are attenuated in the full model, but remain significantly lower in blacks and Latinos compared to whites at each of these ages. For example, in the full model, at age 70, an additional limitation is associated with a 28% increased risk of death for whites, compared to a 21% increased risk for Latinos and 18% increased risk for blacks.
Figure 4:
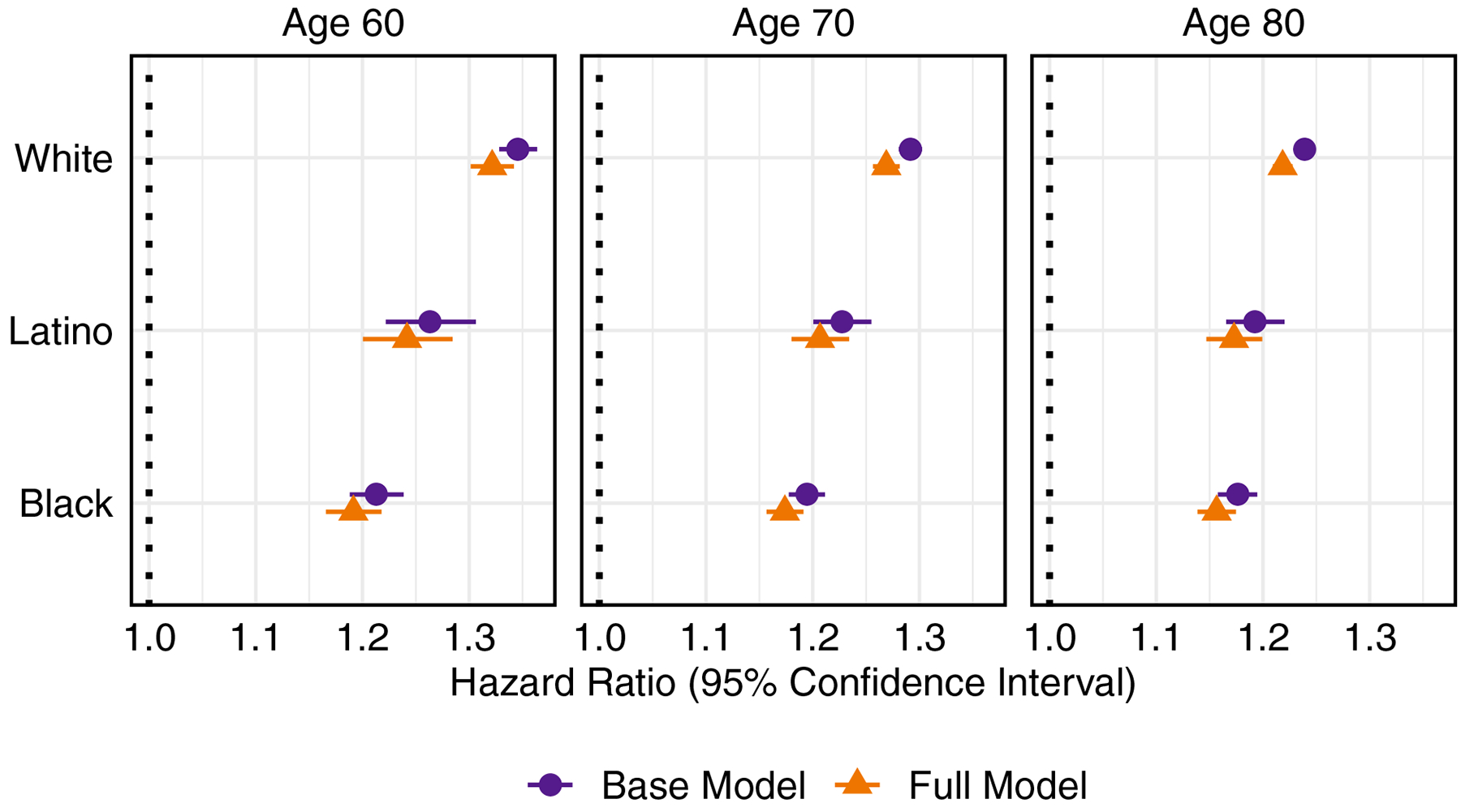
Hazard ratios (95% confidence intervals) from the base and full models associated with number of limitations by age and race/ethnicity.
Figure 5 displays hazard ratios and 95% confidence intervals associated with fair/poor SRH by race/ethnicity at ages 60, 70, and 80. Corresponding hazard ratios from Figure 5 and for all variables in these models can be found in Appendix Table A2 and Appendix Table A4, respectively. As with the number of limitations, the hazard ratio declines with increasing age, but at each of these ages, it is significantly larger for whites than for Latinos and blacks. The variation in hazard ratios remains in the full model such that at age 70, fair/poor SRH is associated with four times the risk of mortality for whites, compared to 2.4 times the risk for Latinos and blacks.
Figure 5:
Hazard ratios (95% confidence intervals) from the base and full models associated with fair/poor self-rated health by age and by race/ethnicity.
Figure 6 displays hazard ratios and 95% confidence intervals associated with inability to complete the walking speed test and a one-SD below average walking speed, by race/ethnicity at age 70. Corresponding hazard ratios from Figure 6 and for the full set of variables are in Appendix Table A2 and Appendix Table A5, respectively. There is no statistical evidence that the mortality risks associated with inability to complete the walking speed test or performance on the walking speed test vary by race/ethnicity. Compared to the results for number of functional limitations and fair/poor SRH, the confidence intervals associated with being unable to complete the walking speed test and standardized walking speed are much larger, reflecting the smaller sample that participated in these tests.
Figure 6:
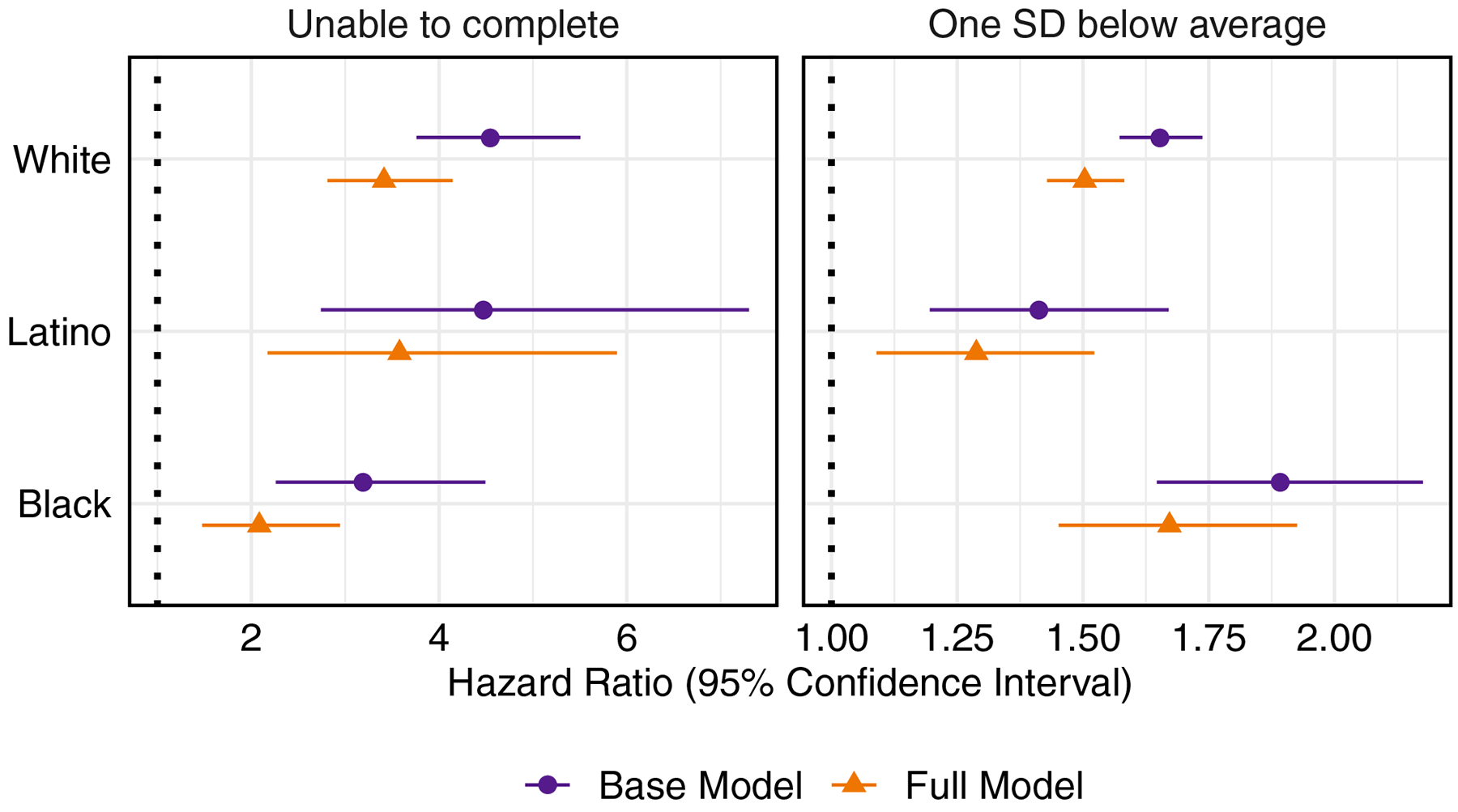
Hazard ratios (95% confidence intervals) from the base and full models associated with inability to complete walking speed test and one SD below average walking speed at age 70 by race/ethnicity.
4.3. Sensitivity Analyses
In addition to our main analyses using mixed effects Cox models, we also stratified these analyses by sex. Though these sex-specific analyses had less power to detect significant differences by race/ethnicity, the findings were largely similar. We also modeled mortality with a Gompertz distribution instead of the non-parametric Cox model and found that our results were not sensitive to the choice of parameterization.
5. Discussion
In this paper we examine whether measures of physical functioning are more weakly associated with mortality for blacks and Latinos than they are for whites and find this to be the case for the count of self-reported functional limitations. In contrast, we do not detect significant racial/ethnic variation in the association between measured walking speed and mortality.
5.1. Possible Explanations
One plausible explanation for the weaker association between self-reported limitations and mortality for Latinos and blacks is reporting error. A prior study using HRS data and anchoring vignettes found higher thresholds for mobility problems among black and Latino respondents compared to whites (Dowd and Todd 2011). We explored this possibility in the subsample of HRS individuals who completed the in-home physical functioning tests. Among those reporting a given functional limitation, blacks and Latinos had worse measured walking speed and peak expiratory flow and a higher prevalence of being unable to complete these tests than whites, indicating a higher threshold for reporting a limitation compared to whites. The impact of varying thresholds by race/ethnicity on the strength of the association between functional limitations and survival is unclear since the thresholds may vary across particular limitations. Moreover, in cases where blacks and Latinos have a higher threshold than whites, those who report a given limitation are likely more severely impaired than whites reporting the same limitation, which would imply a stronger association with mortality, but those who do not report this limitation are also likely to be more impaired than the corresponding group of whites, which would imply a weaker association with mortality. Given these complexities, it is not clear how different thresholds would affect the association between functional limitations and mortality among blacks and Latinos. However, the fact that there is no evidence to suggest that Latinos and blacks over-report limitations implies that our findings reflect a higher burden of impairment in these groups that is less strongly associated with mortality than it is for whites.
Another hypothesis relates to racial/ethnic differences in the severity of illnesses and experience of pain. Although our models control for major chronic diseases and conditions as well as whether the respondent reports being frequently troubled by pain, we are unable to determine the severity of the health conditions, the degree to which pain is managed or the inherent subjectivity of reported pain. The fact that blacks and Latinos receive less treatment for pain than whites (Cintron and Morrison, 2006; Mossey, 2011) may contribute to their worse physical functioning and weaken the relationship between physical functioning measures and mortality for these groups.
A related argument for the attenuated relationship between functional limitations and survival among Latinos and blacks is that it reflects racial/ethnic differences in health maintenance and related treatments and behaviors that we are unable to measure well, if at all. For example, several studies have found that blacks and Latinos are less likely than whites to receive joint replacements to treat osteoarthritis (Escalante et al. 2000; Lopez et al. 2005; Skinner et al. 2003), which is rarely fatal but can severely limit functioning. In addition, Latino and black older adults engage less frequently than whites in leisure-time physical activity – an important component of maintaining physical functioning at older ages (Crespo et al. 1996; Dai et al. 2015; DiPietro 2001). It is also likely that our models have an inadequate control for obesity: although maximum BMI is a preferable measure for predicting mortality than current BMI (Mehta et al. 2014), it relies on accurate recall of weight for what may be many years prior to interview and captures obesity at only a single time point. Because Latinos and blacks have a higher prevalence of obesity than whites, unmeasured obesity throughout the life course may account for part of the weaker association between functional limitations and survival for these groups.
Lastly, our results are consistent with the hypothesis that Latinos and blacks are more likely than whites to experience limitations as a result of their overrepresentation in strenuous and dangerous jobs that are frequently associated with workplace injuries and musculoskeletal disorders (Del Río and Alonso-Villar 2015; Melvin et al. 2014; Seabury et al. 2017; Toussaint-Comeau 2006). Although such work is likely to decrease physical functioning, it may have a much smaller impact on survival. Several studies support the link between strenuous working conditions and impaired physical functioning (Lahelma et al. 2012; Missikpode et al. 2016; Møller et al. 2015), but there has been very little research on the effects of working conditions on racial/ethnic differences in health at older ages.
All of these explanations could apply as well to walking speed, yet racial/ethnic differences in the association between walking speed and mortality are not significant. Because walking speed tests were administered to a subset of HRS participants over the age of 65, these analyses are based on substantially smaller sample sizes, especially for black and Latino respondents, thereby limiting the statistical power to detect differences by race/ethnicity. Nevertheless, we suspect that sample size (or a select subsample) is not a sufficient explanation of the difference in findings between self-reported limitations and walking speed. When we repeat the analysis of self-reported limitations on the subsample with walking speed information, the association remains significantly weaker among blacks and Latinos than among whites but with wider confidence intervals (see Appendix Table A6 and Appendix Figure A2).
There are two other possible explanations for why racial/ethnic variation in the association between walking speed and mortality differs from that between the number of functional limitations and mortality. One pertains to the different types of physical restrictions that underlie the two measures of physical functioning. Walking speed was chosen for this analysis because it was the performance measure most closely related to activities captured in the self-reports, but it is unlikely to reflect limitations of upper-body mobility (e.g., difficulty lifting objects or picking up a dime), which may have the weakest link to survival. Variations in the prevalence of specific limitations across racial/ethnic groups may then result in different predictive abilities of the self-reports vs. walking speed by race/ethnicity. A second hypothesis is suggested by the walking speed findings for blacks. There is suggestive (but not significant) evidence from Figure 6 that inability to complete the walking speed test is more strongly related to mortality for whites than for blacks, whereas worse performance on the walking speed test has a stronger association for blacks. The finding that functional limitations are a weaker predictor of survival for blacks relative to whites, whereas walking speed (for those able to do the test) may be as strong if not a stronger predictor for blacks, may result in part from walking speed being a continuous and hence more nuanced measure of performance. Tabulations shown in Appendix Figure A1 indicate that it is primarily very slow walking speeds that are more strongly linked to mortality for blacks than whites, perhaps because these speeds reflect extreme severity of diseases such as stroke or hypertension (which are more common among blacks) that cannot be captured in yes/no responses to questions about difficulty in performing specific activities.
For comparison, we also examined racial/ethnic differences in the association between SRH and mortality. Our findings confirm those of McGee et al. (1999) and Woo and Zajacova (2016), who found that SRH is a stronger predictor of mortality for whites compared to other racial/ethnic groups, consistent with the results for self-reported functional limitations. Previous researchers have hypothesized that the variation in predictive ability of SRH may be due to differences in education or access to care that influence one’s knowledge about his/her health, differences in the respondent’s reference group, or, in the case of Latinos, differences in the meaning of the categories when the question is asked in Spanish (McGee et al. 1999; Woo and Zajacova 2016). However, these explanations are less applicable to self-reported functional limitations. Respondents’ assessment of whether or not they have difficulty performing basic activities is probably less dependent on socioeconomic predictors or reference groups than their evaluation of their overall health status; moreover, the questions on functional limitations are likely to be less sensitive to translation compared with the response categories used for the SRH question.
5.2. Limitations
Our study has several limitations. One, discussed above, is the reduced sample size for the walking speed test, underscoring the need for future studies with larger samples of performance measures for Latinos and blacks. A second concern is our inability to examine the role of occupational characteristics and leisure-time physical activity because these variables may be the result rather than the cause of poor health, and measures at earlier points in the life course are not available in these data. A third issue is loss-to-follow-up, which may occur more frequently for less healthy individuals. This is a particular concern for less healthy Latino immigrants who may return to their countries of origin, a theory often referred to as “salmon bias” (Abraido-Lanza et al. 1999). In our data, Latinos were more likely than blacks or whites to exit the sample through attrition (as opposed to through death), but the Latinos that exited through attrition had initial health profiles similar to or healthier than Latinos that remained in the study. Thus, our findings do not appear to be driven by selective loss-to-follow-up of the least healthy Latino individuals.
5.3. Implications of Findings
These results have implications for future mortality research and clinical practice. Although studies have demonstrated that self-reported physical limitations are among the best discriminators between survivors and decedents for short-term survival (Goldman et al. 2016), few have recognized heterogeneity in predictive ability (Goldman et al. 2017). Variations in the strength of associations of functioning with survival across racial/ethnic groups suggests the need for more nuanced prognostic models that allow for such variability and incorporate non-clinical information. Accurate prognostic tools not only enable social science and medical researchers to improve their understanding of pathways leading to health deterioration and ultimately death, but also empower clinicians to have more informed discussions with patients about end-of-life decision making.
These findings are important not only with regard to prognosis, but also because of the implications for quality of life. In particular, a relatively weak association between functional limitations and mortality has important negative implications for Latinos and blacks, because it implies that these groups will spend a larger proportion of their remaining years functionally limited and disabled compared with whites (Hayward et al. 2014). Because foreign-born Latinos, particularly those who are undocumented, are often ineligible for publicly-funded insurance and frequently do not have health insurance through employers, family members are likely to assume much of the burden of care for relatives with poor physical functioning. Moreover, if these functional impairments are already manifest during working ages, they would present particularly acute problems for Latinos and blacks who often face challenging work conditions, restricted opportunities to change jobs, poor access to quality medical care and inadequate financial resources (Catanzarite and Trimble 2008; Choi et al. 2016; Kochhar and Fry 2014; Singh and Lin 2013).
Supplementary Material
Highlights.
Physical functioning is a powerful predictor of mortality at older ages
We investigate whether this association varies by race and ethnicity
Functional limitations are more weakly linked to mortality for blacks and Latinos
This may be due to racial/ethnic differences in jobs, pain, activity, or treatment
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
Contributor Information
Theresa Andrasfay, Office of Population Research, Princeton University.
Noreen Goldman, Office of Population Research, Woodrow Wilson School of Public and International Affairs, Princeton University.
References
- Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, & Turner JB (1999). The Latino mortality paradox: a test of the” salmon bias” and healthy migrant hypotheses. American journal of public health, 89(10), 1543–1548. 10.2105/AJPH.89.10.1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alley DE, & Chang VW (2007). The Changing Relationship of Obesity and Disability, 1988–2004. JAMA, 298(17), 2020–2027. 10.1001/jama.298.17.2020 [DOI] [PubMed] [Google Scholar]
- Angel RJ, Angel JL, & Hill TD (2014). Longer lives, sicker lives? Increased longevity and extended disability among Mexican-origin elders. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(4), 639–649. 10.1093/geronb/gbu158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T, 2020. Changes in Physical Functioning as Short-Term Predictors of Mortality. The Journals of Gerontology: Series B 75, 630–639. 10.1093/geronb/gby133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, Lankarani MM, & Burgard S (2016). Black–white difference in long-term predictive power of self-rated health on all-cause mortality in United States. Annals of epidemiology, 26(2), 106–114. 10.1016/j.annepidem.2015.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen CE, Hummer RA, 2019. Longer—but Harder—Lives?: The Hispanic Health Paradox and the Social Determinants of Racial, Ethnic, and Immigrant–Native Health Disparities from Midlife through Late Life. J Health Soc Behav 60, 434–452. 10.1177/0022146519884538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catanzarite L, & Trimble L (2008). Latinos in the United States Labor Market In Rodríguez H, Sáenz R, & Menjívar C (Eds.), Latinas/os in the United States: Changing the Face of América (pp. 149–167). Boston, MA: Springer US; 10.1007/978-0-387-71943-6_10 [DOI] [Google Scholar]
- Choi E, Tang F, & Copeland VC (2017). Racial/Ethnic Inequality Among Older Workers: Focusing On Whites, Blacks, and Latinos Within the Cumulative Advantage/Disadvantage Framework. Journal of Social Service Research, 43(1), 18–36. 10.1080/01488376.2016.1235068 [DOI] [Google Scholar]
- Cintron A, & Morrison RS (2006). Pain and ethnicity in the United States: A systematic review. Journal of palliative medicine, 9(6), 1454–1473. 10.1089/jpm.2006.9.1454 [DOI] [PubMed] [Google Scholar]
- Crespo CJ, Keteyian SJ, Heath GW, & Sempos CT (1996). Leisure-time physical activity among US adults: results from the Third National Health and Nutrition Examination Survey. Archives of internal medicine, 156(1), 93–98. [PubMed] [Google Scholar]
- Crimmins E, Guyer H, Langa K, Ofstedal MB, Wallace R, & Weir D (2008). Documentation of physical measures, anthropometrics and blood pressure in the Health and Retirement Study. HRS Documentation Report DR-011, 14(1–2), 47–59. [Google Scholar]
- Crimmins EM (2004). Trends in the Health of the Elderly. Annual Review of Public Health, 25(1), 79–98. 10.1146/annurev.publhealth.25.102802.124401 [DOI] [PubMed] [Google Scholar]
- Dai S, Carroll DD, Watson KB, Paul P, Carlson SA, & Fulton JE (2015). Participation in types of physical activities among US adults—National Health and Nutrition Examination Survey 1999–2006. Journal of Physical Activity and Health, 12(s1), S128–S140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Río C and Alonso-Villar O. 2015. “The Evolution of Occupational Segregation in the United States, 1940–2010: Gains and Losses of Gender–Race/Ethnicity Groups.” Demography 52(3):967–988. [DOI] [PubMed] [Google Scholar]
- DiPietro L (2001). Physical activity in aging: changes in patterns and their relationship to health and function. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 56(suppl_2), 13–22. [DOI] [PubMed] [Google Scholar]
- Dowd JB, & Todd M (2011). Does Self-reported Health Bias the Measurement of Health Inequalities in U.S. Adults? Evidence Using Anchoring Vignettes From the Health and Retirement Study. The Journals of Gerontology: Series B, 66B(4), 478–489. 10.1093/geronb/gbr050 [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Manheim LM, Song J, & Chang RW (2001). Arthritis prevalence and activity limitations in older adults. Arthritis & Rheumatism, 44(1), 212–221. [DOI] [PubMed] [Google Scholar]
- Escalante A, Espinosa-Morales R, Rincón ID, Arroyo RA, & Older SA (2000). Recipients of hip replacement for arthritis are less likely to be Hispanic, independent of access to health care and socioeconomic status. Arthritis & Rheumatism, 43(2), 390–399. [DOI] [PubMed] [Google Scholar]
- Fakhouri THI, Ogden CL, Carroll MD, Kit BK, & Flegal KM (2012). Prevalence of Obesity Among Older Adults in the United States, 2007–2010 (No. 106) (p. 8). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Fenelon A (2013). Revisiting the Hispanic mortality advantage in the United States: The role of smoking. Social Science & Medicine, 82, 1–9. 10.1016/j.socscimed.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, & Ogden CL (2012). Prevalence of Obesity and Trends in the Distribution of Body Mass Index Among US Adults, 1999–2010. JAMA, 307(5), 491–497. 10.1001/jama.2012.39 [DOI] [PubMed] [Google Scholar]
- Goldman N, Glei DA, Rosero-Bixby L, Chiou S-T, & Weinstein M (2014). Performance-based measures of physical function as mortality predictors: Incremental value beyond self-reports. Demographic research, 30(7), 227–252. 10.4054/DemRes.2013.30.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N (2016). Will the Latino Mortality Advantage Endure? Research on Aging, 38(3), 263–282. 10.1177/0164027515620242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Glei DA, & Weinstein M (2016). What matters most for predicting survival? A multinational population-based cohort study. PLoS One, 11(7), e0159273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Glei DA, & Weinstein M (2017). The Best Predictors of Survival: Do They Vary by Age, Sex, and Race? Population and development review, 43(3), 541–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas S, & Rohlfsen L (2010). Life course determinants of racial and ethnic disparities in functional health trajectories. Social science & medicine, 70(2), 240–250. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Hummer RA, Chiu C-T, González-González C, & Wong R (2014). Does the Hispanic paradox in US adult mortality extend to disability? Population Research and Policy Review, 33(1), 81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] Health and Retirement Study, Tracker File 2014 (V1.0) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, 2017. [Google Scholar]
- [dataset] Health and Retirement Study, Tracker File 2016 (V3.0) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, 2019. [Google Scholar]
- Ho JY, & Elo IT (2013). The Contribution of Smoking to Black-White Differences in U.S. Mortality. Demography, 50(2), 545–568. 10.1007/s13524-012-0159-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honaker J, King G, & Blackwell M (2011). Amelia II: A program for missing data. Journal of statistical software, 45(7), 1–47. [Google Scholar]
- Idler EL, Hudson SV, & Leventhal H (1999). The Meanings of Self-Ratings of Health: A Qualitative and Quantitative Approach. Research on Aging, 21(3), 458–476. 10.1177/0164027599213006 [DOI] [Google Scholar]
- Jenkins KR (2004). Obesity’s Effects on the Onset of Functional Impairment Among Older Adults. The Gerontologist, 44(2), 206–216. 10.1093/geront/44.2.206 [DOI] [PubMed] [Google Scholar]
- Jylhä M (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social science & medicine, 69(3), 307–316. [DOI] [PubMed] [Google Scholar]
- Kail BL, Taylor MG, & Rogers N (2018). Double Disadvantage in the Process of Disablement: Race as a Moderator in the Association Between Chronic Conditions and Functional Limitations. The Journals of Gerontology: Series B. [DOI] [PubMed] [Google Scholar]
- Kochhar R, & Fry R (2014). Wealth inequality has widened along racial, ethnic lines since end of Great Recession. Washington, D.C.: Pew Research Center. [Google Scholar]
- Lahelma Eero, Laaksonen Mikko, Lallukka Tea, Martikainen Pekka, Olli Pietiläinen Peppina Saastamoinen, Gould Raija, and Rahkonen Ossi. 2012. Working Conditions as Risk Factors for Disability Retirement: A Longitudinal Register Linkage Study. BMC Public Health 12(1):309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lariscy JT, Hummer RA, & Hayward MD (2015). Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic paradox. Demography, 52(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham K, Clarke PJ, & Pavela G (2015). Social Relationships, Gender, and Recovery From Mobility Limitation Among Older Americans. The Journals of Gerontology: Series B, 70(5), 769–781. 10.1093/geronb/gbu181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Moody-Ayers SY, Landefeld CS, Walter LC, Lindquist K, Segal MR, & Covinsky KE (2007). The relationship between self-rated health and mortality in older black and white Americans. Journal of the American Geriatrics Society, 55(10), 1624–1629. [DOI] [PubMed] [Google Scholar]
- Lopez JPF, Burant CJ, Siminoff LA, Kwoh CK, & Ibrahim SA (2005). Patient perceptions of access to care and referrals to specialists: a comparison of African-American and white older patients with knee and hip osteoarthritis. Journal of the National Medical Association, 97(5), 667–673. [PMC free article] [PubMed] [Google Scholar]
- Markides KS, & Eschbach K (2005). Aging, migration, and mortality: current status of research on the Hispanic paradox. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(Special_Issue_2), S68–S75. [DOI] [PubMed] [Google Scholar]
- McGee DL, Liao Y, Cao G, & Cooper RS (1999). Self-reported health status and mortality in a multiethnic US cohort. American journal of epidemiology, 149(1), 41–46. [DOI] [PubMed] [Google Scholar]
- Melvin J, Hummer R, Elo I, & Mehta N (2014). Age patterns of racial/ethnic/nativity differences in disability and physical functioning in the United States. Demographic Research, 31, 497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, Stenholm S, Elo I, Aromaa A, Heliövaara M, & Koskinen S (2014). Weight Histories and Mortality among Finnish Adults: The Role of Duration and Peak BMI. Epidemiology, 25(5), 707–710. 10.1097/EDE.0000000000000147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Missikpode Celestine, Michael Yvonne L., and Wallace Robert B.. 2016. “Midlife Occupational Physical Activity and Risk of Disability Later in Life: National Health and Aging Trends Study.” Journal of the American Geriatrics Society 64(5):1120–1127. [DOI] [PubMed] [Google Scholar]
- Møller Anne, Reventlow Susanne, Hansen Åse M., Andersen Lars L., Siersma Volkert, Lund Rikke, Avlund Kirsten, Andersen Johand H., and Mortensen Ole S.. 2015. “Does Physical Exposure Throughout Working Life Influence Chair-Rise Performance in Midlife? A Retrospective Cohort Study of Associations Between Work and Physical Function in Denmark.” BMJ Open 5(11):e009873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon JR, Kondo N, Glymour MM, Subramanian SV, 2011. Widowhood and Mortality: A Meta-Analysis. PLoS One 6 10.1371/journal.pone.0023465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossey JM (2011). Defining racial and ethnic disparities in pain management. Clinical Orthopaedics and Related Research®, 469(7), 1859–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] RAND HRS Longitudinal File 2014 (V2). Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. Santa Monica, CA, 2018. [Google Scholar]
- Rosano C, Longstreth WT, Boudreau R, Taylor CA, Du Y, Kuller LH, & Newman AB (2011). High Blood Pressure Accelerates Gait Slowing in Well-Functioning Older Adults over 18-Years of Follow-Up. Journal of the American Geriatrics Society, 59(3), 390–397. 10.1111/j.1532-5415.2010.03282.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostron BL, Chang CM, & Pechacek TF (2014). Estimation of Cigarette Smoking–Attributable Morbidity in the United States. JAMA Internal Medicine, 174(12), 1922–1928. 10.1001/jamainternmed.2014.5219 [DOI] [PubMed] [Google Scholar]
- Rubin DB, 2004. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons. [Google Scholar]
- Samson MM, Crowe A, de Vreede PL, Dessens JAG, Duursma SA, & Verhaar HJJ (2001). Differences in gait parameters at a preferred walking speed in healthy subjects due to age, height and body weight. Aging Clinical and Experimental Research, 13(1), 16–21. 10.1007/BF03351489 [DOI] [PubMed] [Google Scholar]
- Seabury SA, Terp S, & Boden LI (2017). Racial And Ethnic Differences In The Frequency Of Workplace Injuries And Prevalence Of Work-Related Disability. Health Affairs, 36(2), 266–273. 10.1377/hlthaff.2016.1185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheftel MG, & Heiland FW (2018). Disability crossover: Is there a Hispanic immigrant health advantage that reverses from working to old age? Demographic Research, 39, 209–250. [Google Scholar]
- Singh GK, & Lin SC (2013). Marked ethnic, nativity, and socioeconomic disparities in disability and health insurance among US children and adults: the 2008–2010 American Community Survey. BioMed research international, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J, Weinstein JN, Sporer SM, & Wennberg JE (2003). Racial, Ethnic, and Geographic Disparities in Rates of Knee Arthroplasty among Medicare Patients. New England Journal of Medicine, 349(14), 1350–1359. 10.1056/NEJMsa021569 [DOI] [PubMed] [Google Scholar]
- Snih SA, Ottenbacher KJ, Markides KS, Kuo Y-F, Eschbach K, & Goodwin JS (2007). The Effect of Obesity on Disability vs Mortality in Older Americans. Archives of Internal Medicine, 167(8), 774–780. 10.1001/archinte.167.8.774 [DOI] [PubMed] [Google Scholar]
- Solon G, Haider SJ, Wooldridge JM, 2015. What Are We Weighting For? J. Human Resources 50, 301–316. 10.3368/jhr.50.2.301 [DOI] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort profile: the health and retirement study (HRS). International journal of epidemiology, 43(2), 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toussaint-Comeau M (2006). The occupational assimilation of Hispanic immigrants in the US: Evidence from panel data. International Migration Review, 40(3), 508–536. [Google Scholar]
- Van Oyen H, Berger N, Nusselder W, Charafeddine R, Jagger C, Cambois E, et al. (2014). The effect of smoking on the duration of life with and without disability, Belgium 1997–2011. BMC Public Health, 14(1), 723 10.1186/1471-2458-14-723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, & Jette AM (1994). The disablement process. Social Science & Medicine, 38(1), 1–14. 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Verghese J, Holtzer R, Oh-Park M, Derby CA, Lipton RB, & Wang C (2011). Inflammatory Markers and Gait Speed Decline in Older Adults. The Journals of Gerontology: Series A, 66A(10), 1083–1089. 10.1093/gerona/glr099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir DR (2016). Validating mortality ascertainment in the Health and Retirement Study. Ann Arbor, Michigan: Survey Research Center, Institute for Social Research, University of Michigan; https://hrs.isr.umich.edu/publications/biblio/9022. [Google Scholar]
- Winship C, Radbill L, 1994. Sampling weights and regression analysis. Sociological Methods & Research 23, 230–257. [Google Scholar]
- Woo H, & Zajacova A (2017). Predictive strength of self-rated health for mortality risk among older adults in the United States: does it differ by race and ethnicity? Research on aging, 39(7), 879–905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


