Abstract
Background.
Motivational Interviewing plus Cognitive Behavior Therapy (MI/CBT) has been used to reduce adolescent substance use, but has rarely been applied in youth correctional settings. This trial compared MI/CBT against Relaxation Training plus Substance-Education/12-Steps (RT/SET) to reduce substance use and crime among incarcerated youth.
Methods.
Participants (N = 199) were incarcerated juveniles (64.8% non-White, 10.1% girls, mean age of 17.1 years). Two individual sessions of MI (or RT) were followed by 10 group sessions of CBT (or SET). Youth were randomized to condition with follow-ups at 3- and 6-months after release. Major outcomes included alcohol, marijuana and crimes involving aggression.
Results.
A marginal treatment by time interaction was found for percent heavy drinking days, with follow-up tests indicating less alcohol use in RT/SET than MI/CBT at 6 months, and increased use within MI/CBT from 3 to 6 months. A significant treatment by time interaction was found for alcohol-related predatory aggression, with follow-up tests indicating fewer youth engaged in this behavior from 3 to 6 months within RT/SET, and weak evidence favoring MI/CBT over RT/SET at 3 months. General predatory aggression decreased from 3 to 6-months for both treatments.
Conclusions.
Although weak evidence was found favoring MI/CBT with respect to alcohol-related predatory aggression, results generally support RT/SET in reducing percent heavy drinking days.
Keywords: Youth, incarcerated, substance use, treatment
1. Introduction
Rates of substance use among youth involved in the justice system are high. In a sample of detainees (N = 1826), 50.7% and 46.8% of males and females, respectively, had a substance use diagnosis, with just over 25% meeting criteria for alcohol disorder and over 40% meeting criteria for marijuana use disorder (Teplin et al., 2002). Within this sample, substance disorders were the 2nd most prevalent diagnosis (44.5%) behind behavioral disorders (46.3%; Abram et al., 2003). Other studies have found alarming rates of substance use among incarcerated youth in particular. A Canadian study (N = 205) found that 85.5% of males and 100% of females had a substance disorder (Gretton & Clift, 2011); whereas an American study (N = 162) found that in the last year, 59.9% and 88.9% had alcohol and marijuana use disorders, respectively (Stein, et al., 2011a).
Substance abuse is strongly related to aggression, delinquency and recidivism, and contributes to behaviors that result in juvenile crime (Doran et al., 2012). Common factors likely confer risk for substance use and aggression, which in turn reciprocally influence each other (Doran et al., 2012). Substance treatment reduces drug use and crime (Prendergast et al., 2002); and has been effective in reducing aggression and criminality in youth (Doran et al., 2012).
1.1. Interventions for incarcerated youth
Although there is great need, few studies have been conducted to evaluate efficacious interventions for substance using incarcerated youth. Extensive meta-analyses have been conducted on justice-involved youth to determine effective interventions to reduce recidivism more generally, and among the most effective are group-based and cognitive behavioral programs (Lipsey, 2009). At the same time, of over 548 study samples, only 12% were on incarcerated/institutionalized youth (Lipsey, 2009), suggesting the need for more work in this area. A large national survey of substance services in youth correctional agencies (N = 141) found that psycho-education was the most frequently offered intervention (88.5%), 92.9% offered group-based intervention, and 51.2% offered cognitive behavioral programming (i.e., relapse prevention; Young et al., 2007). Although Motivational Interviewing (MI) is recommended for correctional settings (Bogue and Nandi, 2012), few controlled studies have been conducted in these settings (McMurran, 2009). A series of studies indicate MI is efficacious in substance-using incarcerated youth in terms of enhancing treatment engagement (Stein et al., 2006), and in reducing drug use (Stein et al., 2011a) and other risky behaviors after release (Stein et al., 2011b). In a review of studies on justice-involved persons, MI was found to assist treatment retention and improve motivation for change (McMurran, 2009).
Studies indicate that over 40% of incarcerated youth are unmotivated to change substance use (Slavet et al., 2006; Clair et al., 2011). Although empirical evidence indicates Cognitive Behavioral Therapy (CBT) reduces adolescent substance use (Waldron & Kaminer, 2004), skills training approaches may not be appropriate for unmotivated persons, as skills-training assumes interest and readiness to change. Therefore, combined MI-CBT has been utilized in a variety of contexts including adult smokers leaving prison (Clarke et al., 2013) and adolescent marijuana users (Dennis et al., 2004).
Although MI and CBT have been applied separately to incarcerated youth, no studies have combined MI/CBT for them (Doran et al., 2012). MI has reduced aggressive behaviors in incarcerated youth (Clair-Michaud et al., 2016). CBT has been frequently studied in youth and has demonstrated effectiveness in reducing delinquency (Doran et al., 2012). Interventions, (e.g., MI/CBT) that focus on motivation, problem-solving, communication, mental health (i.e., anger, depression) and substances may be particularly useful for incarcerated youth (Doran et al., 2012). This is because these youth may have significant mental health and substance issues, but lack motivation and skills (e.g., problem-solving, communication) to address them. CBT is generally recommended for delinquent youth with the possible addition of MI for less compliant youth (OJJDP, 2010).
1.2. Purpose
This is a randomized clinical trial (RCT) testing the hypothesis that combined MI and CBT is more efficacious than a comparison intervention in reducing substance use and crime. Given the empirical support for CBT and the importance of engagement strategies for incarcerated youth, two individual sessions of MI were combined with ten group sessions of CBT to reduce substance use in incarcerated youth. Alcohol and marijuana were targeted because they are the most frequently used substances by justice-involved youth (Lebeau-Craven et al., 2003). The comparison condition was two individual sessions of relaxation training and visualization (RT) combined with ten group sessions of treatment as usual, which was substance-education and Twelve-Step introduction (SET). As an attention control for MI, RT was utilized, as these techniques are thought to be generally ineffective in reducing substance use (see Klajner et al., 1984; Holroyd, 1976; Miller et al., 1995). Psycho-education (Young et al., 2007) and Twelve-Step programming (Peters and Wexler, 2005) are common in correctional settings, and recommendations have been made to provide Twelve-Step programming to incarcerated youth (Sussman, 2010).
2. Methods
2.1. Participants
The study was conducted at a youth correctional facility in the northeastern United States (US). Youth are sentenced to the facility for a variety of infractions (e.g., drug dealing, sex offence). Approval to conduct the study was provided by a university Institutional Review Board and the youth facility. Informed consent was obtained for participants (youth <18 years provided assent) by study staff. Screening began 11/2005 and final follow-up was completed 3/2011. Youth meeting the following criteria were eligible: (a) ages 14–19 years; (b) sentenced for 4–12 months; and (c) in the year before incarceration they used marijuana or drank at least monthly, or they drank heavily (>5 standard drinks for boys, >4 for girls) at least once; or they used marijuana or drank in the 4 weeks before either the offense for which they were incarcerated, or before they were incarcerated.
2.2. Procedures
Immediately after adjudication, screening occurred. Screening was followed by consent, after which youth were assessed and then randomized to 2 individualized sessions of MI + 10 group sessions of CBT, or 2 individualized sessions of RT + 10 group sessions of SET. At 3 and 6 months after release, youth were assessed in the community. Assessments (60–90 min) were conducted by a trained bachelor’s, master’s or doctoral-level Research Assistant (RA) blind to condition. RAs had about 20 hours of training; senior level staff conducted in vivo observations to ensure proper assessment delivery. Following training, weekly supervision was provided by a PhD-level staff member; all assessment data were reviewed by a senior-level staff member. Adolescents received $230 and snacks for participation.
2.3. Interventions
Adolescents were randomized to MI/CBT or RT/SET by the Project Director, who had no contact with participants, using a random numbers table. All interventions were manualized, including fidelity procedures. Two Individual sessions (MI or RT) were 60–90 minutes each; 10 group sessions (CBT or SET) were 75 minutes each, gender segregated, used rolling admission, and occurred 1–3 times/week with a median of 3 participants/group session. Each counselor had 160 hours of manualized training, with weekly supervision. Training consisted of readings and role-plays with feedback. Intervention files were reviewed by a clinical psychologist. Counselors were 1 man and 5 women; all 6 were White; 4 had a master’s, 1 had a bachelor’s and 1 had a doctoral degree. Each counselor conducted both intervention types. All sessions were recorded, and fidelity coding was conducted. Any counselors falling below fidelity criteria received added individual supervision and tracking until fidelity again met acceptable levels.
MI provided feedback to clients to motivate change; emphasized personal responsibility for change; with permission, counselors provided advice and offered a menu of change-options; and counselors sought to enhance client efficacy (see Miller & Rollnick, 2013). In session 2, pending a youth’s interest, each collaborated on creating a change-plan; orientation to CBT was also provided. CBT, designed to be interactive, covered refusal skills; enhancing social support and communication; problem-solving; dealing with emotions; and coping with high-risk situations and urges (modeled after skills training as described in Dennis et al., 2004). Counselors in RT informed clients that reducing stress helps to reduce desire to use substances, and that RT will assist in reducing stress thereby mitigating substance use. Advice to stop substances was provided. Youths were instructed in progressive muscle relaxation, deep breathing, and in visualizing and describing a peaceful scene with focus on the five senses (e.g., “I smell popcorn,” not “I make popcorn”). Feedback was provided on use of techniques. On session 2, youth chose the technique they liked most, practiced again, decided when they might practice it in the future, and were oriented to SET. SET, based on usual substance abuse intervention provided by the facility, provided an overview of physical, psychological, and social consequences of drugs; twelve-steps and defense mechanisms such as denial; types of risky situations; and resources available after release. Format was didactic as well as interactive. Video tapes were used as part of the education process. As needed, groups focused on conflict resolution, gang participation, drug dealing, and independent living.
2.4. Intervention fidelity
Procedures to track MI and RT fidelity are detailed elsewhere (Stein et al., 2011). At the end of sessions, youth and counselors completed forms. Therapeutic relationship (e.g., empathy) was assessed (1 = strongly disagree to 4 = strongly agree), as was perceived utility of specific elements of MI and RT (topic not introduced [0]; topic not useful [1] to very useful [3]). Table 1 presents relevant comparisons demonstrating fidelity to intervention. Approach to group fidelity was based on Dennis et al. (2004). At the end of group sessions supervisors completed forms assessing how much CBT or SET techniques occurred (i.e., “adherence;” rated as 1 = not at all, to 5 = extensively), and the skill used to provide the intervention techniques (i.e., “competence;” rated as 0 = not done, 1 = very poor, to 7 = excellent). Table 2 presents relevant comparisons demonstrating fidelity to intervention. SET adherence within SET was rated significantly higher than CBT adherence within CBT, although for both treatments, the level of adherence was adequate. Skill ratings did not differ across intervention; both were delivered with adequate level of skill. Of sessions observed by supervisors, a random sample of 42% was double-coded for reliability. Intra-class correlation coefficients (ICCs) indicated at least adequate agreement (Cicchetti, 1994; Cohen, 1988; Barnett, 2006) with 0.66 for CBT and 0.59 for SET on adherence; and 0.87 for CBT and 0.56 for SET on skill.
Table 1.
Fidelity to Individual Treatment Assignment.
| Comparison | t(df) | p | ||
|---|---|---|---|---|
| Adolescent Ratings | ||||
| Relationship in MI Sessions | Relationship in RT Sessions | |||
| M (SD) | 3.55 (0.41) | 3.52 (0.45) | 0.44 (195) | =0.663 |
| RT Elements in MI Sessions | RT Elements in RT Sessions | |||
| M (SD) | 0.40 (0.79) | 2.40 (0.51) | 21.00 (167.79) | <0.001 |
| MI Elements in MI Sessions | RT Elements in MI Sessions | |||
| M (SD) | 2.39 (0.41) | 0.40 (0.79) | 22.83 (98) | <0.001 |
| MI Elements in MI Sessions | RT Elements in RT Sessions | |||
| M (SD) | 2.39 (0.41) | 2.40 (0.51) | 0.17 (184.62) | =0.865 |
| MI Elements in MI Sessions | MI Elements in RT Sessions | |||
| M (SD) | 2.39 (0.41) | 0.36 (0.68) | 25.28 (158.03) | <0.001 |
| RT Elements in RT Sessions | MI Elements in RT Sessions | |||
| M (SD) | 2.40 (0.51) | 0.36 (0.68) | 25.97 (96) | <0.001 |
| Counselor Ratings | ||||
| Relationship in MI Sessions | Relationship in RT Sessions | |||
| M (SD) | 3.43 (0.45) | 3.34 (0.48) | 1.33 (195) | =0.184 |
| RT Elements in MI Sessions | RT Elements in RT Sessions | |||
| M (SD) | 0.01 (0.05) a | 2.39 (0.43) | 54.52 (98.54) | <0.001 |
| MI Elements in MI Sessions | RT Elements in MI Sessions | |||
| M (SD) | 2.31 (0.42) | 0.01 (0.05) a | 55.49 (99) | <0.001 |
| MI Elements in MI Sessions | RT Elements in RT Sessions | |||
| M (SD) | 2.31 (0.42) | 2.39 (0.43) | 1.29 (195) | =0.199 |
| MI Elements in MI Sessions | MI Elements in RT Sessions | |||
| M (SD) | 2.31 (0.42) | 0.00 (0.00) a | 54.91 (99) | <0.001 |
| RT Elements in RT Sessions | MI Elements in RT Sessions | |||
| M (SD) | 2.39 (0.43) | 0.00 (0.00) a | 54.99 (96) | <0.001 |
MI = Motivational Interviewing, RT = Relaxation Training, REL = relationship rating, M = mean, SD = standard deviation, df = degrees of freedom; n (number of youth assigned to MI) = 100; n = 99 for RT;
data did not conform to distributional assumptions, however, mean comparisons illustrate fidelity expectations were met (e.g., counselor ratings of MI elements in MI sessions were greater than counselor rating of RT elements in MI sessions).
Table 2.
Supervisor Ratings of Fidelity to Group Treatment Assignment.
| Comparison | t(df) | p | ||
|---|---|---|---|---|
| SET Techniques in CBT Sessions | CBT Techniques in CBT Sessions | |||
| M (SD) | 1.02 (0.08) | 2.36 (0.26) | 42.69 (73) | <0.001 |
| SET Techniques in SET Sessions | CBT Techniques in SET Sessions | |||
| M (SD) | 2.48 (0.19) | 1.10 (0.30) | 33.70 (62) | <0.001 |
| SET Techniques in CBT Sessions | SET Techniques in SET Sessions | |||
| M (SD) | 1.02 (0.08) | 2.48 (0.19) | 60.00 (135) | <0.001 |
| CBT Techniques in CBT Sessions | CBT Techniques in SET Sessions | |||
| M (SD) | 2.36 (0.26) | 1.10 (0.30) | 26.70 (135) | <0.001 |
| CBT Techniques in CBT Sessions | SET Techniques in SET Sessions | |||
| M (SD) | 2.36 (0.26) | 2.48 (0.19) | 2.90 (132) | =0.004 |
| CBT Techniques in CBT Sessionsa | SET Techniques in SET Sessionsa | |||
| M (SD) | 4.50 (0.73) | 4.50 (0.62) | 0.34 (135) | =0.733 |
SET = Substance Education and Twelve Step Programming, CBT = Cognitive Behavior Therapy, M = mean, SD = standard deviation, df = degrees of freedom; n (number of CBT sessions rated by supervisors) = 74; n = 63 for SET;
skill rating.
2.5. Measures
2.5.1. Baseline assessment
Background Questionnaire records socio-demographic information including race and ethnicity, age and gender (e.g., male or female). Composite International Diagnostic Interview short-form (CIDI-SF; Kessler et al., 1998) alcohol and marijuana dependence modules asks a series of questions (“What is the largest number of drinks you had in any single day during the past 12 months?” None, 1–3, 4–10, 11–20, or >20) providing an indication of substance dependence (APA, 1994). Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1991; 20 items) asks a series of questions (e.g., “How often in the past week have you felt bothered by things that don’t usually bother you?” 0 days, 1–2 days, 3–4 days, 5–7 days) where higher score indicates more depressive symptoms.
2.5.2. Baseline and follow-up assessments
Delinquent Activities Scale (DAS; Reavy et al., 2014; Reavy et al., 2012) provides conduct disorder symptom count, and scales indicating crime involvement (representing primary crime outcomes) including predatory aggression, alcohol-related predatory aggression and marijuana-related drug-dealing/aggression (13, 12 and 5 items, respectively). A sample item is, “In the last 3 months, how many times were you involved in gang fights?” Three responses are requested separately for whether a behavior happened at all, if it happened while on (or behavior was done to get) alcohol, and if it happened while on/to get marijuana. Higher scores indicate more delinquent activities. Timeline Follow-back (TLFB; Sobell & Sobell, 1992), commonly employed to assess alcohol and marijuana use in adults (e.g., Hendricks et al., 2012) and youth (e.g., Stein et al., 2011a), was administered for the preceding 90 days. Recall of drinking patterns and deviations from patterns is assisted by providing respondents with a calendar and cuing recall by noting holidays, special events, work/school schedules and the like. Respondents are provided with examples of beverage sizes, are asked types of beverages consumed, approximate amount of alcohol consumed with each drink and so forth in order to calculate number of standard drinks consumed on a given day. TLFB assessed primary substance outcomes including average drinks/week, percent heavy drinking days, average number of joints/smoking day, average number of times smoked marijuana/week, and percent days used marijuana. Varian OnTrak Testik was utilized on-site to detect cannabinoids in urine > 50 ng/mL (Varian, 2004). Youth in a controlled environment for 100% of days during a follow-up did not have substance outcomes calculated. Youth claiming marijuana abstinence but who had positive, missing or contaminated urine screens were coded as marijuana positive for that assessment unless the reason for not providing a sample was unrelated to participant’s decision (Brown et al., 2009). When youth reported marijuana use, but urine screen was negative, self-report was accepted for analyses.
2.6. Analysis
Condition effects on outcome were analyzed using Generalized Estimating Equations (GEE; Zeger & Liang, 1986), which can handle correlated observations across time for participants. Models tested the effects of intervention condition on alcohol, marijuana and crime outcomes over the 3- and 6-month follow-ups. In these models, the main effect of intervention examined whether intervention group outcomes differed over the follow-up interval. The interaction of intervention group by time examined whether the effect of intervention differed at the 3- vs. 6-month follow-up. When significant time by treatment interactions emerged, main effects were not interpreted and follow-up tests were conducted (within time, results for each treatment were compared; and within treatment, results at each time were compared). Treatment condition was dummy-coded with MI/CBT as the reference group. Outcomes that had a continuous distribution were analyzed with a GEE model and Cohen’s d as the measure of effect size (Cohen, 1988). Dichotomous outcomes were examined using GEE models with a binomial distribution and logit link function, and provided odds ratios (ORs) as a measure of effect size. Covariates were determined by examining treatment differences on important variables (Table 3); more Hispanics were in RT/SET. Age correlated significantly across alcohol, marijuana and crime outcomes (p < .05) and was included as a covariate. For each analysis, baseline version of the dependent variable was included as a covariate. Step 1 of each model included covariates and main effects for treatment and time; step 2 included the interaction (treatment by time). Small, medium and large d are represented by 0.2, 0.5 and 0.8, respectively (Cohen, 1988); whereas for OR, small, medium and large effects are 1.5, 3.0 and 5.0, respectively (Chen et al., 2010). Correction for multiple comparison was not used as planned comparisons were conducted.
Table 3:
Baseline Differences on Demographics and Key Variables by Treatment Condition
| Variable | Sample Summary (n=199) N (%) or M (SD) | MI/CBT (n=100) N (%) or M (SD) | RT/SET (n=99) N (%) or M (SD) |
|---|---|---|---|
| Demographics | |||
| Age in years | 17.08 (1.04) | 17.05 (1.01) | 17.12 (1.08) |
| Gender: Female | 20 (10.1) | 12 (12.0) | 8 (8.1) |
| Ethnicity: Hispanic* | 79 (39.7) | 32 (32.0) | 47 (47.5) |
| Race: Non-White | 129 (64.8) | 66 (66.7) | 60 (61.9) |
| Number of previous detentions or incarcerations | 2.53 (2.34) | 2.83 (2.46) | 2.23 (2.19) |
| Alcohol dependent | 63 (31.7) | 32.0 (32.0) | 31.0 (31.3) |
| Marijuana dependent | 123 (61.8) | 56 (56.0) | 67 (67.7) |
| Conduct disorder symptom count | 7.96 (3.45) | 8.05 (3.55) | 7.88 (3.55) |
| Depressive symptoms | 19.18 (10.29) | 19.05 (10.24) | 19.31 (10.39) |
| Sessions attended | 9.12 (2.27) | 9.11 (2.28) | 9.13 (2.28) |
| Alcohol Use Variables | |||
| Average drinks per week | 10.89 (18.02) | 11.16 (19.04) | 10.62 (17.02) |
| % heavy drinking days | 12.04 (19.31) | 12.10 (19.57) | 11.97 (19.15) |
| Marijuana Use Variables | |||
| Average number of joints per smoking day | 5.42 (4.97) | 5.84 (5.57)a | 4.98 (4.25)b |
| Average number of times smoked marijuana per week | 17.86 (20.05) | 20.42 (22.08) | 15.26 (17.47)c |
| % days used marijuana | 64.36 (39.32) | 64.94 (40.44) | 63.78 (38.35)c |
| Crime Variables | |||
| Predatory aggression | 6.20 (3.47) | 6.35 (3.72) | 6.05 (3.22) |
| Alcohol related predatory aggressiond | 103 (51.8) | 54 (54.0) | 49 (49.5) |
| Marijuana related drug dealing and aggressiond | 128 (64.3) | 63 (63.0) | 65 (65.7) |
MI = Motivational Interviewing, CBT = Cognitive Behavior Therapy, RT = Relaxation Training, SET = Substance Education and Twelve Steps, M = Mean, SD = Standard Deviation, n = Number of participants, % = Percent.
n = 90 because 10 youth had zero smoking days;
n = 88 because 10 youth had zero smoking days and 1 youth did not complete the questionnaire;
n = 98 because 1 youth did not complete the questionnaire.
Dichotomized due to violations of distributional assumptions. Untransformed values presented. Significant difference by treatment condition and level of significance indicated by *p<.05.
Multiple imputation was performed for missing outcome variables using multiple linear or logistic regression plus a random component to produce the imputed values (McPherson et al., 2012; Hedeker et al., 2007). One-hundred-fifty imputed data sets were generated to yield estimates that were better than 95% efficient (Rubin, 1987; Schafer and Graham, 2002). Separate regression analyses were performed using all 150 of the imputed data sets, yielding effect sizes averaged across the 150 sets of estimates. Results did not differ in significance level from analyses without multiple imputation. Therefore, analyses with multiple imputation are not presented.
3. Results
3.1. Sample
Figure 1 shows numbers of youth enrolled and followed. Of 199 allocated to intervention, 171 (85.2%) and 163 (81.9%) completed, respectively, 3- and 6-month follow-up. Reasons for not completing 3- and 6-month follow-up were lack of interest (n = 8 and 16, respectively) and could not locate (n = 20, both times). At 3- and 6-months, n = 1 and 2, respectively, for disconfirmed urine; for youth in a controlled environment, n = 4 and 22, respectively. When youth reported they had used marijuana, but urine screen was negative, self-report was accepted for analyses: At 3-months n = 5 and n = 10, for MI/CBT and RT/SET, respectively; these figures for 6-months are n = 1 and n = 3.
Figure 1.
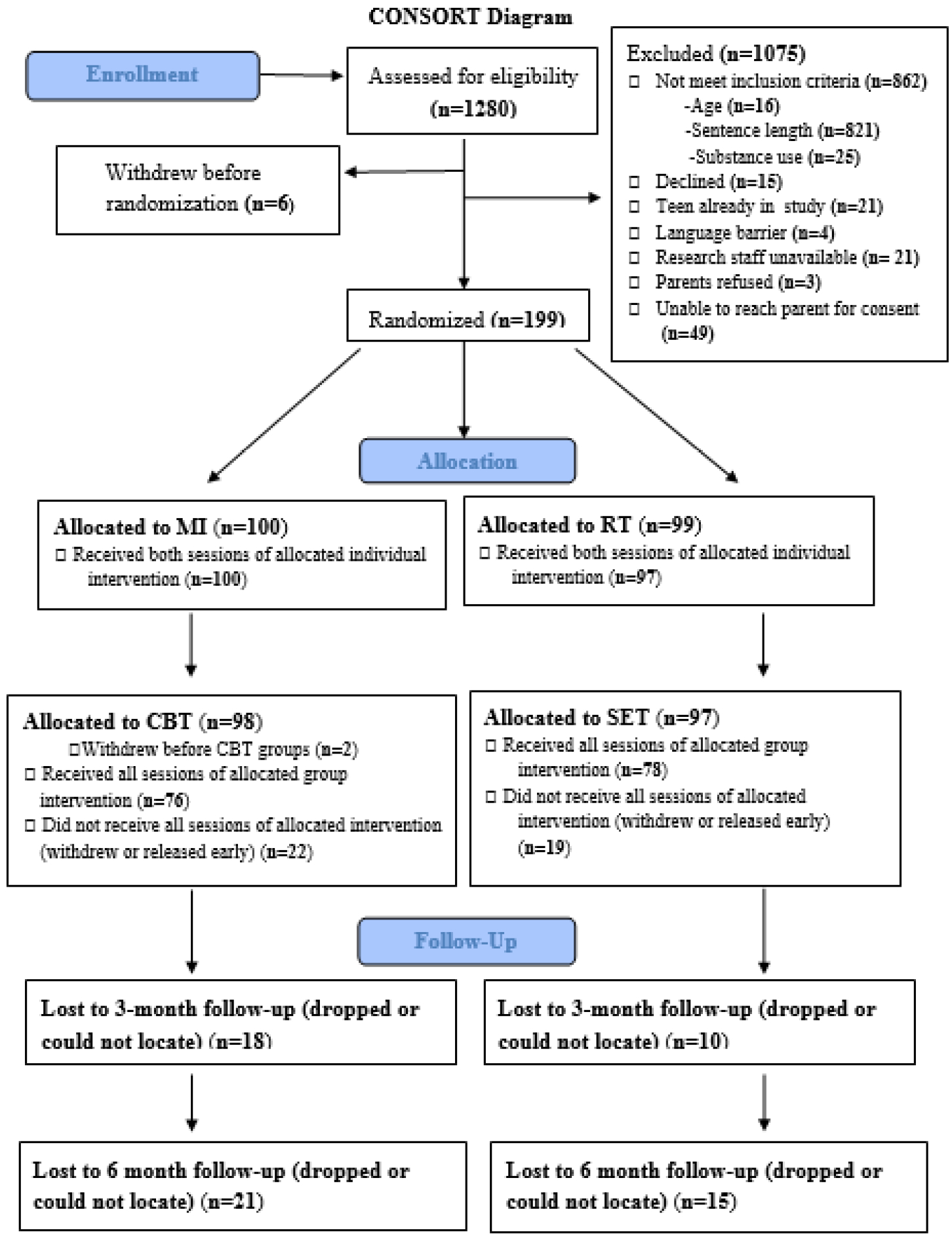
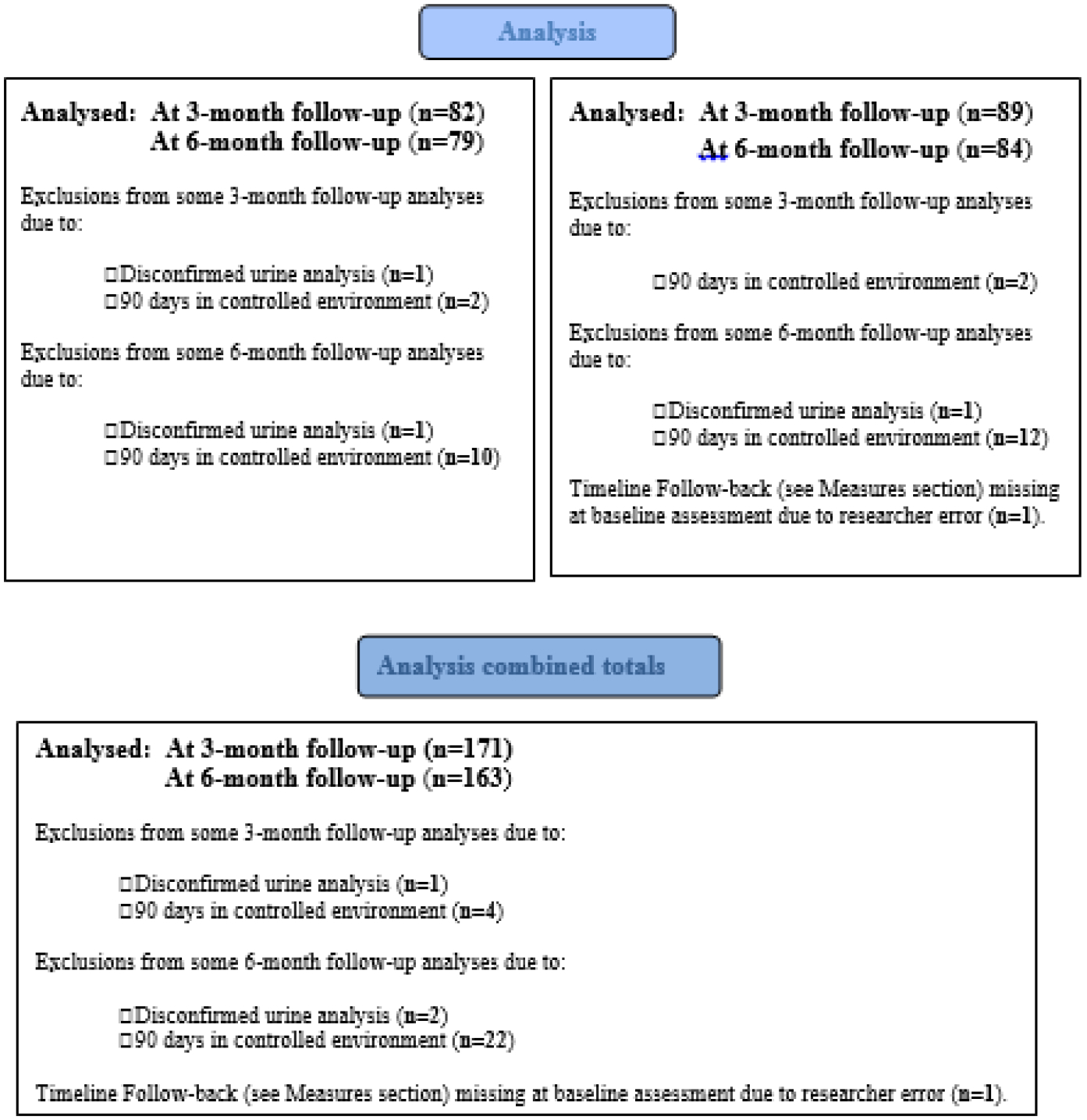
Consort Diagram.
MI = Motivational Interviewing; CBT = Cognitive Behavioral Therapy; RT = Relaxation Therapy; SET = Substance Education/Twelve Step Introduction. N for analyses is equivalent to subtracting N lost at follow-up from N allocated to individual treatment. Example: N allocated to RT is 99, N lost at 3-month follow-up in the RT/SET condition is 10, so that 99 – 10 = 89 for N Analyzed at 3-month follow-up.
Baseline sample characteristics are shown in Table 3. Those included in the study (n = 163) at furthest follow-up were compared to those not included (n = 36) on important variables (e.g., gender, ethnicity, race, age, previous detentions, days in controlled environment post-release, conduct disorder symptoms, substance disorder, depressive symptoms, treatment type, sessions attended). Youth completing furthest follow-up attended more group treatments (M = 9.62, SD = 1.23 for completers; M = 6.86, SD = 3.98 for non-completers; t(36.49) = 4.12, p < .001), and had fewer previous detentions (M = 2.36, SD = 2.27 for completers; M = 3.28, SD = 2.55 for non-completers; t(196) = 2.14, p < .034). Number of youth with data available for analyses at follow-up did not differ by treatment assignment, nor did number of treatment sessions relate to outcome or intervention assignment.
3.2. Outcomes
Analyses were completed with SPSS 24 (IBM Corp., 2016). Average drinks/week, percent heavy drinking days, average number of joints/smoking day and average number of times smoked marijuana/week were log transformed. Alcohol-related predatory aggression and marijuana-related drug-dealing/aggression were dichotomized because no transformation corrected the non-normal distributions. Table 4 shows descriptive statistics for baseline and follow-up values of outcome variables. Irrespective of intervention, problem behaviors appear to be generally lower after release from incarceration. Time from last intervention to first follow-up was unrelated to outcome or group assignment. With a = 0.05 and n ranging between 91 – 163 at 3- and 6-month follow-ups, power is estimated at 0.77 – 0.97 to detect small-medium effect sizes (Soper, 2016).
Table 4:
Outcomes at Baseline and Follow-Up by Treatment Condition.
| Variable | MI/CBT N (%) or M (SD) |
RT/SET N (%) or M (SD) |
|---|---|---|
| Average number of drinks per week | ||
| Baseline | 11.16 (19.04) | 10.62 (17.02) |
| 3-Mo FU | 5.16 (12.27) | 3.86 (9.16) |
| 6-Mo FU | 7.08 (13.69) | 3.57 (7.67) |
| % heavy drinking days | ||
| Baseline | 12.10 (19.57) | 11.97 (19.15) |
| 3-Mo FU | 6.95 (18.16) | 4.52 (12.90) |
| 6-Mo FU | 11.10 (23.08) | 4.48 (11.08) |
| Average number of joints per smoking day | ||
| Baseline | 5.84 (5.57) | 4.98 (4.25) |
| 3-Mo FU | 2.52 (2.37) | 2.48 (2.48) |
| 6-Mo FU | 2.48 (2.16) | 2.95 (3.71) |
| Average number of times smoked marijuana per week | ||
| Baseline | 20.42 (22.08) | 15.26 (17.47) |
| 3-Mo FU | 8.03 (12.46) | 5.37 (10.21) |
| 6-Mo FU | 6.78 (12.50) | 6.59 (12.68) |
| % days used marijuana | ||
| Baseline | 64.94 (40.44) | 63.78 (38.35) |
| 3-Mo FU | 36.88 (41.55) | 29.13 (39.11) |
| 6-Mo FU | 35.56 (41.62) | 34.78 (41.61) |
| Predatory aggression | ||
| Baseline | 6.35 (3.72) | 6.05 (3.22) |
| 3-Mo FU | 2.13 (2.69) | 1.92 (2.41) |
| 6-Mo FU | 1.89 (2.71) | 1.44 (2.03) |
| Alcohol related predatory aggressiona | ||
| Baseline | 54 (54.0) | 49 (49.5) |
| 3-Mo FU | 9 (11.3) | 16 (18.4) |
| 6-Mo FU | 9 (13.0) | 6 (8.3) |
| Marijuana related drug dealing and aggressiona | ||
| Baseline | 63 (63.0) | 65 (65.7) |
| 3-Mo FU | 11 (13.8) | 12 (13.8) |
| 6-Mo FU | 7 (10.1) | 9 (12.5) |
MI = Motivational Interviewing, CBT = Cognitive Behavior Therapy, RT = Relaxation Training, SET = Substance Education and Twelve Steps, M = Mean, SD = Standard Deviation, n = Number of participants, % = Percent., Mo = Month, FU = Follow-up.
Dichotomized due to violations of distributional assumptions. Untransformed values presented. n’s ranged from 44–100, with Mode = 100 and Median = 80 for MI/CBT; and 47–99, with Mode = 87 and Median = 87 for RT/SET.
3.2.1. Alcohol
Table 5 presents GEE results for all analyses. For percent heavy drinking days there was a marginal treatment by time interaction. For MI/CBT, percent heavy drinking days at 3 months was 6.95%, whereas at 6 months, it was 11.10%. For RT/SET, percent heavy drinking days at 3 months was 4.52%, whereas at 6 months, it was 4.48%. Follow-up tests at each time indicate percent heavy drinking days for RT/SET was lower than that for MI/CBT at 6 months (B = 0.22, SE = 0.09, p = 0.019; 95% CI [−0.36, 0.41], d = 0.40), but not at 3 months (B = 0.06, SE = 0.78, p = 0.44; 95% CI [−.092, 0.212], d = 0.11). Furthermore, follow-up tests within RT/SET indicate no differences in percent heavy drinking days at 3 months vs. 6 months (B = −0.009, SE = 0.055, p = 0.865; 95% CI [−.118, 0.099], d = 0.02), but within MI/CBT percent heavy drinking days was significantly higher at 6 months as compared to 3 months (B = 0.14, SE = 0.06, p = 0.033; 95% CI [0.01, 0.27], d = 0.25). For average number of drinks/week, no significant main effects for treatment or time were found, nor was a significant treatment by time interaction found.
Table 5:
Modeling Outcomes Using Generalized Estimating Equations.
| Dependent Variable Predictor | B | SE | Effect Size d or OR |
95% CI | p | |
|---|---|---|---|---|---|---|
| Average number of drinks/weeka | ||||||
| 1st step | Baseline number of drinks/weeka | 0.251 | 0.070 | 0.506 | 0.229, 0.782 | 0.000 |
| Hispanic (vs. Non-Hispanic) | −0.097 | 0.069 | −0.196 | −0.470, 0.078 | 0.161 | |
| Age | 0.047 | 0.032 | 0.095 | −0.030, 0.220 | 0.135 | |
| MI/CBT (vs. RT/SET)b | 0.079 | 0.068 | 0.159 | −0.112, 0.429 | 0.251 | |
| Timeb | 0.047 | 0.034 | 0.095 | −0.037, 0.228 | 0.158 | |
| 2nd step | Time × MI/CBT | 0.092 | 0.067 | 0.187 | −0.077, 0.450 | 0.165 |
| % heavy drinking daysa | ||||||
| 1st step | Baseline % heavy drinking daysa | 0.231 | 0.066 | 0.419 | 0.185, 0.652 | 0.000 |
| Hispanic (vs. Non-Hispanic) | −0.107 | 0.073 | −0.194 | −0.453, 0.065 | 0.143 | |
| Age | 0.047 | 0.034 | 0.085 | −0.036, 0.206 | 0.167 | |
| MI/CBT (vs. RT/SET)b | 0.126 | 0.074 | 0.229 | −0.032, 0.491 | 0.086 | |
| Timeb | 0.062 | 0.043 | 0.112 | −0.040, 0.265 | 0.148 | |
| 2nd step | Time × MI/CBT | 0.149 | 0.085 | 0.270 | −0.032, 0.573 | 0.080 |
| Average number of joints/smoking day (AJSD)a | ||||||
| 1st step | Baseline # joints/smoking daya | 0.174 | 0.091 | 0.476 | 0.250, −0.013 | 0.057 |
| Hispanic (vs. Non-Hispanic) | 0.068 | 0.063 | 0.186 | 0.172,−0.151 | 0.279 | |
| Age | −0.007 | 0.041 | −0.019 | 0.114, −0.243 | 0.865 | |
| MI/CBT (vs. RT/SET)b | 0.045 | 0.063 | 0.124 | 0.171, −0.212 | 0.469 | |
| Timeb | −0.014 | 0.034 | −0.037 | 0.930, −0.219 | 0.690 | |
| 2nd step | Time × MI/CBT | 0.010 | 0.682 | 0.027 | 0.187,−0.339 | 0.885 |
| Average number of times smoked marijuana/weeka | ||||||
| 1st step | Baseline # times marijuana/weeka | 0.271 | 0.064 | 0.497 | 0.268, 0.726 | 0.000 |
| Hispanic (vs. Non-Hispanic) | 0.001 | 0.076 | 0.002 | −0.273, 0.276 | 0.990 | |
| Age | 0.085 | 0.035 | 0.155 | 0.030, 0.281 | 0.015 | |
| MI/CBT (vs. RT/SET)b | 0.070 | 0.075 | 0.128 | −0.140, 0.396 | 0.349 | |
| Timeb | 0.009 | 0.038 | 0.017 | −0.120, 0.153 | 0.808 | |
| step | Time × MI/CBT | −0.115 | 0.075 | −0.212 | −0.481, 0.058 | 0.124 |
| % days used marijuana | ||||||
| 1st step | Baseline % days used marijuana | 0.214 | 0.067 | 0.005 | 0.002, 0.008 | 0.001 |
| Hispanic (vs. Non-Hispanic) | 2.382 | 5.864 | 0.058 | −0.223, 0.340 | 0.685 | |
| Age | 5.754 | 2.618 | 0.141 | 0.015, 0.267 | 0.028 | |
| MI/CBT (vs. RT/SET)b | 5.418 | 5.712 | 0.133 | −0.142, 0.407 | 0.343 | |
| Timeb | 3.431 | 3.025 | 0.084 | −0.061, 0.229 | 0.257 | |
| 2nd step | Time × MI/CBT | −7.136 | 5.988 | −0.175 | −0.462, 0.113 | 0.233 |
| Predatory Aggression | ||||||
| 1st step | Baseline predatory aggression | 0.281 | 0.047 | 0.114 | 0.077, 0.151 | 0.000 |
| Hispanic (vs. Non-Hispanic) | 0.124 | 0.282 | 0.050 | −0.174, 0.274 | 0.661 | |
| Age | 0.044 | 0.148 | 0.018 | −0.099, 0.135 | 0.766 | |
| MI/CBT (vs. RT/SET)b | 0.206 | 0.286 | 0.083 | −0.144, 0.310 | 0.472 | |
| Timeb | −0.393 | 0.192 | −0.159 | −0.311, −0.007 | 0.040 | |
| 2nd step | Time × MI/CBT | 0.234 | 0.388 | 0.095 | −0.213, 0.402 | 0.547 |
| Alcohol related predatory aggressionc | ||||||
| 1st step | Baseline alcohol aggressionc | 2.469 | 0.688 | 11.808 | 3.065, 45.494 | 0.000 |
| Hispanic (vs. Non-Hispanic) | 0.378 | 0.423 | 1.459 | 0.636, 3.347 | 0.372 | |
| Age | 0.099 | 0.183 | 1.104 | 0.772, 1.579 | 0.588 | |
| MI/CBT (vs. RT/SET)b | −0.258 | 0.417 | 0.773 | 0.341, 1.750 | 0.537 | |
| Timeb | −0.429 | 0.286 | 0.651 | 0.372, 1.141 | 0.134 | |
| 2nd step | Time × MI/CBT | 1.473 | 0.551 | 4.363 | 1.483, 12.833 | 0.007 |
| Marijuana related drug dealing and aggressionc | ||||||
| 1st step | Baselinec | 1.122 | 0.515 | 3.070 | 1.120, 8.417 | 0.029 |
| Hispanic (vs. Non-Hispanic) | 0.511 | 0.411 | 1.668 | 0.745, 3.734 | 0.214 | |
| Age | 0.306 | 0.171 | 1.358 | 0.971, 1.898 | 0.073 | |
| MI/CBT (vs. RT/SET)b | 0.009 | 0.415 | 1.009 | 0.447, 2.276 | 0.982 | |
| Timeb | −0.220 | 0.270 | 0.802 | 0.473, 1.362 | 0.415 | |
| 2nd step | Time × MI/CBT | −0.235 | 0.548 | 0.790 | 0.270, 2.313 | 0.668 |
Logged; analyzed as normally distributed; effect size is in standardized units of the dependent variable (d; Cohen, 1988).
Dummy coded (0 = 3-month follow-up, 1 = 6-month follow-up; MI/CBT = 1; RT/SET = 0).
Dichotomous; analyzed using binomial distribution; effect size is expressed as an odds ratio (OR). SE = Standard Error, % = percent, CI = Confidence Interval, MI = Motivational Interviewing, CBT = Cognitive Behavior Therapy, RT = Relaxation Therapy, SET = Substance Education and Twelve Step Programming.
3.2.2. Marijuana
For average number of joints smoked per smoking day, average number of times smoked marijuana/week, and percent days used marijuana, no significant main effects for treatment or time were found, nor was a significant treatment by time interaction found.
3.2.3. Crime
For alcohol-related predatory aggression there was a treatment by time interaction. For MI/CBT, the percent of adolescents involved in alcohol-related predatory aggression at 3 months was 11.3%, whereas at 6 months, it was 13.0%. For RT/SET, the percent of adolescents involved in alcohol-related predatory aggression at 3 months was 18.4%, whereas at 6 months, it was 8.3%. Follow-up tests at each time indicate that the proportion engaged in alcohol-related predatory aggression for RT/SET was marginally greater than MI/CBT at 3 months (B = −0.89, SE = 0.49, p = 0.072; 95% CI [−1.86, 0.08], OR = 0.41), but not at 6 months (B = 0.61, SE = 0.59, p = 0.300; 95% CI [−0.54, 1.76], OR = 1.84). Furthermore, follow-up tests within MI/CBT indicate no differences in percent engaged in alcohol-related predatory aggression at 3 months vs. 6 months (B = 0.14, SE = 0.52, p = 0.790; 95% CI [−0.89, 1.17], OR = 1.15), but within RT/SET the proportion engaged in alcohol-related predatory aggression was significantly higher at 3 months as compared to 6 months (B = −1.07, SE = 0.54, p = 0.045; 95% CI [−2.13, −0.23], OR = 0.34).
For general predatory aggression there was a main effect for time with no treatment effect or treatment by time interaction. At 3 months, M was 2.02 (SD = 2.55); and at 6 months, M was 1.66 (SD = 2.39). For marijuana-related drug dealing and aggression, no effects were found for treatment or time, or treatment by time interaction.
4. Discussion
For percent heavy drinking days, a weak treatment by time interaction was found. Follow-up tests indicated drinking increased significantly from 3 to 6 months after MI/CBT, but at 6 months, heavy drinking was significantly lower for the RT/SET condition than for those who received MI/CBT. Therefore, for effects on heavy drinking, RT/SET may be more beneficial over the 6-month period following release. A small but significant decrease was found in predatory aggression from 3- to 6-month follow-up in both conditions. However, youth engaged in alcohol-related predatory aggression decreased significantly from 3 to 6 months only after RT/SET, not after MI/CBT. At 3 months, although weak evidence suggested fewer youth in MI/CBT engaged in alcohol-related predatory aggression as compared to youth in RT/SET, RT/SET may be beneficial in the longer term. No effects were found for marijuana or marijuana-related crime, although older youth use marijuana significantly more frequently than younger youth. Previous literature has also found it difficult to obtain treatment effects for marijuana use (Dennis et al., 2004). Given that moderate beneficial effects were found for RT/SET, this approach may be a viable, lower cost treatment to administer in correctional settings, as it requires less training for counselors to administer than MI/CBT.
Given the dangers of heavy drinking (Dawson, 2011), especially for youth (Windle, 2016), the potential for RT/SET to reduce heavy drinking at 6-month follow-up is important. Results for crime-related outcomes may be considered particularly noteworthy. There appears to be an association between alcohol and violence (Lipsey et al., 2002) with some investigators indicating alcohol facilitates violence (Raskin-White, 2002), and others observing that alcohol may cause violence (Bushman, 2002). The reductions in alcohol-related violence found in this study are salient. Costs of crime are estimated at $3,532 per theft offense to $8.98M for murder, with a median cost of $7,974 per stolen property offense (McCollister et.al, 2010). Reducing the incidence of crimes and the numbers of youth engaging in them is critical, and this is especially true for violent crimes.
4.1. Limitations
Follow-up studies should examine mechanisms of action and extend follow-up time beyond 6 months. Current results may apply more readily to youth with slightly fewer previous detentions and who attend more treatment sessions, since youth lost to assessment at furthest follow-up differed on those dimensions as compared to youth included in analyses. The influence of context cannot be eliminated in this study. For example, youth may have received a consistent message to abstain from substances from multiple sources in addition to RT/SET, including social worker, staff, probation officer and judge, whereas MI/CBT emphasized harm-reduction, a message that may have been inconsistent with the general philosophy of the judicial system. It is possible that in part, it was the consistency in message that produced effects for RT/SET. It is possible that youth had difficulty attending to MI/CBT as compared to RT/SET. However, a meta-analysis (Tanner-Smith et al., 2013), including youth with arrest history, found MI/CBT is generally effective in reducing substance use, and that youth delinquency and comorbidity were not associated with effects. The MI/CBT manual also provided guidance on how to assist youth with delays or impairment, and staff were trained and supervised accordingly. Youth likely could attend appropriately to intervention.
5. Conclusions
Results are encouraging for use of RT/SET in reducing heavy drinking days and alcohol related predatory crime over time. At the same time, there is a need to enhance treatment effects, especially for marijuana. Among youth, there is a preponderance of support for CBT, and growing support for MI. However, there is also growing support for 12-Step approaches (see Kelly et al., 2011). In addition, RT as utilized in this study can be viewed a mindfulness approach (see Stein et al., 2011a), and as such may have contributed to intervention effects (Himelstein, 2011). Given better outcomes for RT/SET and that less training is required to administer it, further study of RT/SET is warranted in this setting.
This study has a number of strengths that may increase generalizability, including a racially and ethnically diverse sample of incarcerated youth, although future studies may wish to over-sample girls. Self-report was verified with biological sample for marijuana, retention rate at follow-up was over 80%, blinding and randomization were used, and fidelity to intervention was more than adequate. It is critical to reduce substance use and crime in incarcerated youth using methods that are relatively easily disseminated. Relaxation Training plus Substance Education/12-Steps appears to be a viable option. More work is needed to increase treatment effects.
Highlights.
Compared to MI/CBT, RT/SET useful in reducing alcohol use in youth after release
Both RT/SET and MI/CBT reduced predatory aggression
Compared to MI/CBT, RT/SET helpful in reducing alcohol-related predatory aggression
Acknowledgements
We wish to thank Suzanne Sales for managing data and conducting analyses. We also thank Laurel Murphy for data management, and for managing critical aspects of the project.
Role of Funding Source
This study was funded by a grant from the National Institutes of Health, R01-DA-018851, PI-Stein; and K05AA019681, PI-Monti. This work is the sole responsibility of the authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trial Registration: NCT00227890
Conflict of Interest
Authors Stein, Martin, Clair-Michaud, Lebeau, Kahler, Monti and Rohsenow received salary support during the grant. Multiple co-authors have collaborative relationships spanning multiple projects. No conflicts of interest are identified or claimed for authors, or their family members.
References
- Abram KM, Teplin LA, McClelland GM, Dulcan MK, 2003. Comorbid psychiatric disorders in youth in juvenile detention. Arch. Gen. Psychiatry 60, 1097–1108. 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders, fourth ed. American Psychiatric Association, Washington, DC. [Google Scholar]
- Barnett JJ, 2006. Effect size and measures of association. Summer Evaluation Institute sponsored by The American Evaluation Association and Centers for Disease Control and Prevention; University of Alabama, Birmingham. [Google Scholar]
- Bogue BM, Nandi A, 2012. Motivational Interviewing in Corrections: A Comprehensive Guide to Implementing MI in Corrections. U.S. Department of Justice, National Institute of Corrections, Washington, DC. [Google Scholar]
- Brown RA, Strong DR, Abrantes AM, Myers MG, Ramsey SE, Kahler CW, 2009. Effects on substance use outcomes in adolescents receiving motivational interviewing for smoking cessation during psychiatric hospitalization. Addict. Behav 34, 887–891. 10.1016/j.addbeh.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bushman BJ, 2002. Effects of alcohol on human aggression validity of proposed explanations, in: Galanter M (Ed.), Developments in Alcoholism, Volume 13, Alcohol and Violence. Kluwer Academic Publishers, New York, pp. 227–243. 10.1007/0-306-47141-8_13. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Chen S, 2010. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun. Stat. Simul. Comput 39, 860–864. 10.1080/03610911003650383. [DOI] [Google Scholar]
- Cicchetti DV, 1994. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess 6, 284–290. 10.1037/1040-3590.6.4.284. [DOI] [Google Scholar]
- Clair-Michaud M, Martin RA, Stein LAR, Bassett S, Lebeau R, Golembeske C, 2016. Impact of motivational interviewing on delinquent behaviors in incarcerated adolescents. J. Subst. Abuse. Treat 65, 13–19. 10.1016/j.jsat.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clair M, Stein LAR, Martin R, Barrnett NP, Colby SM, Monti PM, Golembeske C, Lebeau R, 2011. Motivation to change alcohol use and treatment engagement in incarcerated youth. Addict. Behav 36, 674–680. 10.1016/j.addbeh.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke JG, Stein LAR, Martin RA, Martin SA, Parker D, Lopes CE, McGovern AR, Simon R, Roberts M, Friedman P, Bock B, 2013. Forced smoking abstinence: Not enough for smoking cessation. JAMA Intern. Med 173, 789–794. 10.1001/jamainternmed.2013.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, 1988. Statistical Power Analysis for the Behavioral Sciences, second ed. Lawrence Erlbaum Associates, Hillsdale, NJ. [Google Scholar]
- Dawson DA, 2011. Defining risky drinking. Alcohol Res. Health 34, 144–156.. [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Liddle H, Titus JC, Kaminer Y, Webb C, Hamilton N, Funk R, 2004. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. J. Subst. Abuse Treat 27, 197–213. 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Doran N, Luczak SE, Bekman N, Koutsenok I, Brown SA, 2012. Adolescent substance use and aggression. Crim. Justice Behav 39, 748–769. 10.1177/0093854812437022. [DOI] [Google Scholar]
- Gretton HM, Clift RJW, 2011. The mental health needs of incarcerated youth in British Columbia, Canada. Int. J. Law Psychiatry 34, 109–115. 10.1016/j.ijlp.2011.02.004. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Mermelstein RJ, Demirtas H, 2007. Analysis of binary outcomes with missing data: Missing = smoking, last observation carried forward, and a little multiple imputation. Addict. 102, 1564–73. 10.1111/j.1360-0443.2007.01946.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Delucchi KL, Humfleet GL, Hall SM (2012). Alcohol and marijuana use in the context of tobacco dependence. Nicotine Tob. Res 14, 942–951. 10.1093/ntr/ntr312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelstein S, 2011. Meditation research: The state of the art in correctional settings. Int. J. Offender Ther. Comp. Criminol 55, 646–661. 10.1177/0306624X10364485. [DOI] [PubMed] [Google Scholar]
- Holroyd KA, 1976. Cognition and desensitization in the group treatment of test anxiety. J. Consult. Clin. Psychol 44, 991–1001. 10.1037/0022-006X.44.6.991. [DOI] [PubMed] [Google Scholar]
- IBM Corp., 2016. IBM SPSS Statistics (for Windows) Version 24.0. IBM Corp., Armonk, NY. [Google Scholar]
- Kelly J, Pagano M, Stout R, Johnson S, 2011. Influence of religiosity on 12-Step participation and treatment response among substance-dependent adolescents. J. Stud. Alcohol Drugs 72, 1000–1011. 10.15288/jsad.2011.72.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H, 1998. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int. J. Methods Psychiatr. Res 7, 171–185. 10.1002/mpr.47. [DOI] [Google Scholar]
- Klajner F, Hartman LM, Sobell MB, 1984. Treatment of substance abuse by relaxation training: A review of its rationale, efficacy and mechanisms. Addict. Behav 9, 41–55. 10.1016/0306-4603(84)90006-6. [DOI] [PubMed] [Google Scholar]
- Lebeau-Craven R, Stein L, Barnett N, Colby SL, Smith JL, Canto AL, 2003. Prevalence of alcohol and drug use in an adolescent training facility. Subst. Use Misuse 38, 825–834. 10.1081/JA-120017612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, 2009. The primary factors that characterize effective interventions with juvenile offenders: A meta-analytic overview. Vict. and Offenders 4, 124–147. 10.1080/15564880802612573. [DOI] [Google Scholar]
- Lipsey MW, Wilson DB, Cohen MA, Derzon JH, 2002. Is there a causal relationship between alcohol use and violence? A synthesis of evidence in: Galanter M (Ed.), Recent Developments in Alcoholism, Volume 13, Alcohol and Violence. Kluwer Academic Publishers, New York, pp. 245–282. 10.1007/0-306-47141-8_14. [DOI] [PubMed] [Google Scholar]
- McCollister KE, French MT, Fang H, 2010. The cost of crime to society: New crime-specific estimates for policy and program evaluation. Drug Alcohol Depend. 108, 98–109. 10.1016/j.drugalcdep.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurran M, 2009. Motivational interviewing with offenders: A systematic review. Legal Criminol. Psychol 14, 83–100. 10.1348/135532508X278326. [DOI] [Google Scholar]
- McPherson S, Barbosa-Leiker C, Burns GL, Howell D, Roll J, 2012. Missing data in substance abuse treatment research: Current methods and modern approaches. Exp. Clin. Psychopharmacol 20, 243–250. 10.1037/a0027146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Brown JM, Simpson TL, Handmaker NS, Bien TH, Luckie LF, Montgomery HA, Hester RK, Tonigan JS, 1995. What works? A methodological analysis of the alcoholism treatment outcome literature, in: Hester RK, Miller WR (Eds.), Handbook of Alcoholism Treatment Approaches, second ed. Allyn & Bacon, Boston, MA, pp. 12–44. [Google Scholar]
- Miller WR, Rollnick S, 2013. Motivational Interviewing: Helping People Change, third ed. Guilford Press, New York. [Google Scholar]
- Office of Juvenile Justice and Delinquency Prevention (OJJDP), 2010. Cognitive-Behavioral Treatment. Literature Review. Office of Justice Programs, Washington, DC: Accessed on October 13, 2019 https://www.ojjdp.gov/mpg/litreviews/Cognitive_Behavioral_Treatment.pdf. [Google Scholar]
- Peters R, Wexler HK, 2005. Substance Abuse Treatment for Adults in the Criminal Justice System (TIP 44). Substance Abuse and Mental Health Services Administration, Rockville, MD. [PubMed] [Google Scholar]
- Prendergast ML, Podus D, Chang E, Urada D, 2002. Effectiveness of drug abuse treatment: A meta-analysis of comparison group studies. Drug Alcohol Depend. 67, 53–72. 10.1016/S0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- Radloff LS, 1991. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J. Youth Adolesc 20, 149–166. 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Raskin-White H, 2002. Longitudinal Perspective on Alcohol Use and Aggression During Adolescence in: Galanter M (Ed.), Recent Developments in Alcoholism, Volume 13, Alcohol and Violence. Kluwer Academic Publishers, New York, pp. 81–103. 10.1007/0-306-47141-8_5. [DOI] [PubMed] [Google Scholar]
- Reavy R, Stein LAR, Paiva A, Quina K, Rossi JS, 2012. Validation of the delinquent activities scale for incarcerated adolescents. Addict. Behav 37, 875–879. 10.1016/j.addbeh.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reavy R, Stein LAR, Quina K, Paiva AL, 2014. Assessing conduct disorder: A new measurement approach. J. Correct. Health Care, 20, 4–17. 10.1177/1078345813505448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB, 1987. Multiple Imputation for Nonresponse in Surveys. Wiley, New York. [Google Scholar]
- Schafer JL, Graham JW, 2002. Missing data: Our view of the state of the art. Psychol. Methods 7, 147–177. 10.1037//1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Slavet JD, Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R, 2006. The marijuana ladder: Measuring motivation to change marijuana use in incarcerated adolescents. Drug Alcohol Depend. 83, 42–48. 10.1016/j.drugalcdep.2005.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, 1992. Timeline follow-back: A technique for assessing self-reported alcohol consumption, in: Litten RZ, Allen JP (Eds.), Measuring Alcohol Consumption: Psychosocial and Biological Methods. Humana Press, New Jersey, pp. 41–72. 10.1007/978-1-4612-0357-5_3. [DOI] [Google Scholar]
- Soper DS, 2016. Post-hoc Statistical Power Calculator for Hierarchical Multiple Regression [Software]. Accessed on July 8, 2016 http://www.danielsoper.com/statcalc.
- Stein LAR, Colby SM, Barnett NP, Lebeau R, Monti P, Golembeske C, 2011a. Motivational interviewing for incarcerated adolescents: Effects of depressive symptoms on reducing alcohol and marijuana use after release. J. Stud. Alcohol Drugs 72, 497–506. 10.15288/jsad.2011.72.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein L Colby AR, Barnett SM, Monti NP, Golembeske PM, Lebeau-Craven C, Miranda, R. R, 2006. Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychol. Serv 3, 25–34. 10.1037/1541-1559.3.1.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Clair M, Lebeau R, Colby SM, Barnett NP, Golembeske C, Monti PM, 2011b. Motivational interviewing to reduce substance-related consequences: Effects for incarcerated adolescents with depressed mood. Drug Alcohol Depend. 118, 475–478. 10.1016/j.drugalcdep.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, 2010. A review of Alcoholics Anonymous/Narcotics Anonymous programs for teens. Eval. Health Prof 33, 26–55. 10.1177/0163278709356186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Wilson SJ, Lipsey MW, 2013. Comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. J. Subst. Abuse Treat 44, 145–158. 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA, 2002. Psychiatric disorders in youth in juvenile justice. Arch. Gen. Psychiatry 59, 1133–1143. 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varian, 2004. Ontrak Teststik THC. Varian Inc., Lakeforest, CA. [Google Scholar]
- Waldron HB, Kaminer Y, 2004. On the learning curve: The emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addict. 99 (Suppl. 2), 93–105. 10.1111/j.1360-0443.2004.00857.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, 2016. Drinking over the lifespan: Focus on early adolescents and youth. Alcohol Res. 38, 95–101.. [PMC free article] [PubMed] [Google Scholar]
- Young DW, Dembo R, Henderson CC, 2007. A national survey of substance abuse treatment for juvenile offenders. J. Subst. Abuse Treat 32, 255–266. 10.1016/j.jsat.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Lang KY, 1986. Longitudinal data analysis for discrete and continuous outcomes. Biom. 42, 121–130. 10.2307/2531248. [DOI] [PubMed] [Google Scholar]


