Abstract
Patient satisfaction is a useful predictor of adherence and outcomes of cardiovascular diseases (CVDs) treatment. This study explored the satisfaction of Vietnamese CVDs inpatients and outpatients using a scale specifically designed for CVDs patients and examined the factors associated with satisfaction towards CVDs treatment services. Interviews of 600 patients at the Hanoi Heart Hospital were conducted. We developed a measurement scale for both inpatient and outpatient services. Multivariate Tobit regression was used to determine the associated factors with patient satisfaction. For inpatients, Cronbach’s alpha reported for the domains were in the range of 0.72–0.97, while for outpatients, Cronbach’s alpha was within 0.61–0.97. Overall, patients were more satisfied with inpatient services (Mean = 81.8, SD = 5.8) than outpatient services (Mean = 79.7, SD = 5.2, p<0.05). In inpatients, the highest complete satisfaction was in “Attitude of Nurse” item (42.0%), the highest satisfaction score was in “Care and treatment” domain (Mean = 85.6, SD = 9.7) and the lowest in “Hospital facilities” domain (Mean = 78.3; SD = 9.2). Among outpatients, the highest complete satisfaction was in “Attitude of physicians when examining, guiding and explaining to the patient” item (19.7%), the highest satisfaction score was in “Attitude of medical staff” domain (Mean = 82.8; SD = 7.9) and the lowest in “Waiting time” domain (Mean = 76.6; SD = 8.2). People not having health insurances had significantly higher scores in “Waiting time”, “Hospital facilities” and “Attitude of staff” domains (for outpatients) and in “Health service accessibility”, “Hospital facilities” domains (for inpatients) as well as higher total satisfaction score than those having health insurance. Findings discovered through the application of the newly developed instrument showed low satisfaction regarding hospital facilities for inpatients and waiting time for outpatients, suggesting renovation efforts, while inferiority regarding patient satisfaction of health insurance covered patients compared to those without implied policy reform possibility. Further enhancement and validation of the developed instrument was required.
Introduction
Patient satisfaction has long been considered a pivotal element not only for achieving an optimal relationship between patient and health professionals/providers but also for the design of quality assurance and improvement initiatives [1, 2]. From the perspective of healthcare service providers, assessment of patient's experience and satisfaction with health care services could capture whether the services attend to an acceptable standard and highlight potential areas for quality improvement [3]. In addition, although the correlation between patient satisfaction and positive health outcomes have not been found to be definitive [4], a number of studies indicated that satisfied patients were more likely to exert better treatment adherence, which potentially would lead to outcome improvement over time [5, 6]. Enhancing patient satisfaction has also been found to be an effective way to improve patient retention and referrals [7], consequently, increase the market presence and revenue of health facilities [5].
Cardiovascular diseases (CVDs) are among the most significant health problems of the 21st century, causing not only more fatality than any other leading cause of deaths [8] but also substantial morbidity and disability [9]. The burden of CVDs on low and middle-income countries (LMICs) has been disproportionately higher than that on high-income countries [10, 11], partly due to under-developed health systems having limited capability in providing sufficient and effective CVDs care [12]. Cardiovascular conditions include both acute episodes and long term disability that require curative care as a component of a continuous coordinated care model covering primary care, hospital care and post-acute care [13]. Given the influence of patient satisfaction on quality and effectiveness of acute/ hospital care as well as the acute on chronic nature of CVDs, assessing patient satisfaction toward healthcare services among CVDs patients in LMICs setting can be seen as crucial to improve patient experience and health status of these patients.
Nonetheless, how to assess patient satisfaction has still been a subject of debate in literature for the last decades, with measuring patient satisfaction claimed to be a rather challenging [14]. One of the issue with patient satisfaction measurement is arguably the subjective and complex nature of ‘satisfaction’–how a patient define their satisfaction would be influenced by their expectations and grounded on their set of “values, beliefs, attitudes and experiences” [14]. Patient satisfaction measurement developed for and utilized on patients from one country, for instance, would probably face adaptation problems when being applied to people from another country, due to cultural variations and dissimilar characteristics of diverse health systems [15]. Another concern over patient satisfaction measurement has been the reliability and/ validity of measuring instruments [16]. Numerous tools have been developed to examine patient satisfaction, including ones provided by private companies and those of publicly and standardized ones such as consumer assessment health plans (CAHPS) [17] and patient satisfaction questionnaires (PSQ-18) [18], yet criticisms remain that although these existing instruments had good validity and reliability, the scope of these tools was limited such as difficulties in customization, not including professionalism, hospital environment or privacy and security [2]. On the other hand, internally developed instruments that aim to capture specific aspects of patient care, being created through entirely de novo generation or adoptions of questions from other prevailing standardized tools, have been proven to be applicable in cases when the existing measuring scales deemed inappropriate [3].
Thus, an attempt to examine the patient satisfaction of people suffering CVDs, especially in low resource settings would first require the construction and evaluation of a contextualized patient satisfaction scale. Such exercise is particularly important in the context of Vietnam, given the high prevalence and burden of CVDs in the country as CVDs accounted for 31% of all deaths in Vietnam in 2016 [19] and the lack of literature exploring the issue of patient satisfaction among CVD patients. Furthermore, the establishment of an instrument with appropriate validity would potentially facilitate comparison in a wider context, for instance between different medical settings or diseases. This study aimed to investigate the patient satisfaction towards hospital care of people with CVDs, for both inpatient and outpatient services, by employing a scale specifically designed for the study. The reliability and validity of such an instrument would be examined prior to application. In addition, factors potentially associated with CVDs patients’ satisfaction would also be explored.
Materials and methods
Study designs and participants
A cross-sectional study was conducted in Hanoi Heart Hospital, one of the largest central cardiovascular hospitals from July to December 2016. There were approximately 600 outpatients visiting the hospital per day. Moreover, this hospital had 276 inpatient beds with 276 inpatients being treated at the same time in the hospital. The patients admitted in this hospital were not only from Hanoi but also referred by health facilities of provincial and lower levels across Vietnam, thus were likely to reflect diverse socio-economic backgrounds well as disease profiles of Vietnamese heart patients. We invited both inpatients and outpatients who had been examined and treated in Hanoi Heart Hospital to participate in the study. The eligibility criteria: 1) Able to respond to the questionnaire (i.e. not suffering critical physical or psychological conditions that could affect responses); 2) Utilizing services in the hospital during the study period and 3) Accepting to participate in the study. We first briefly explain the study and then invited eligible patients to enroll in the study and asked them to provide written informed consent.
In this study, we used the formula to estimate a population proportion with specified relative precision to compute the necessary sample size. We used α = 0.05, anticipated population proportion P = 0.86 (based on a previous study on patient satisfaction in Vietnam [20]), relative precision ɛ = 0.05. The essential sample size was 251 patients per group. We added 20% for compensating drop-out patients given that most of the patients were older adults or had severe health states which might be more likely to refuse to participate or withdraw to the study. The sample consists of 600 patients (included 300 out-patients and 300 in-patients from 7 departments in Hanoi Heart Hospital) with the response rate of 100%.
Measures and instruments
We conducted face-to-face interviews using a structured questionnaire. The data collection team included well-trained post-graduate students in the field of Public Health. The questionnaires were designed based on the Patient Satisfaction Questionnaire from the Ministry of Health [21]. The variables of concern were described as below:
Patient satisfaction
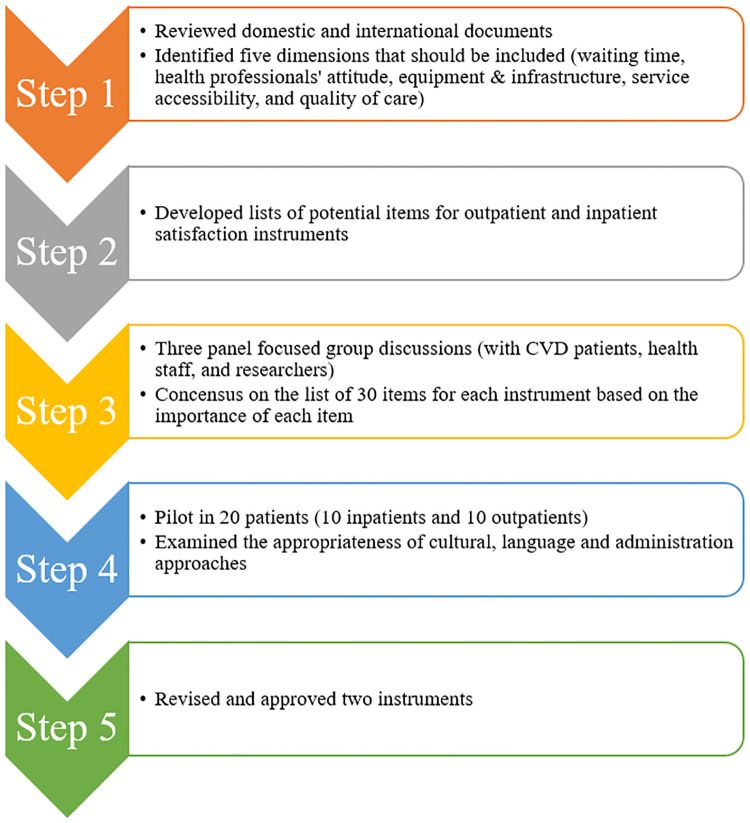
A systematic procedure was used to develop a patient's satisfaction scale. First, we reviewed national and international literature to determine the potential items of patient satisfaction with heart-related services [22–24]. We identified following dimensions that should be included in the instrument: 1) Waiting time; 2) Attitude of physicians, nurses and other medical staffs; 3) Equipment and infrastructure of the hospital; 4) The accessibility of essential health service, and 5) Quality of care and treatment. However, because outpatients and inpatients have different procedures (e.g. outpatients might use more services than inpatient), we developed a separate list of items for outpatients and inpatients. Then, we performed three focused group discussions with patients with heart diseases, health staff, and researchers to examine the face validity of the instrument. Finally, we developed a list of items and selected them based on the importance of each item through the focus group discussions. We then piloted the tool in 20 patients (10 outpatients and 10 inpatients at the Hanoi Heart Hospital) to examine the appropriateness of cultural, language and administration approaches. After receiving patients’ feedback about the text, logical order of the questionnaire, we revised and finalized the questionnaire, as well as sought the approval from leaderboard of the hospital for survey. Finally, there were two questionnaires: one questionnaire measured satisfaction of outpatients, and another one measured satisfaction of inpatients. Each questionnaire had 30 items. The response options included a 5-level Likert scale from 1 “complete dissatisfaction” to 5 “complete satisfaction”, respectively. The score of each domain was calculated by summing the score of domain-related items and then transform to the 100-point scale, in which higher scores meant higher levels of satisfaction. The tool development process was illustrated in Fig 1.
Fig 1. Tool development process.
Other characteristics
We also collected socio-demographic characteristics, comprising age, living area, educational attainment, gender, and health insurance. Health-related quality of life (HRQOL) of patients were examined by using the EuroQol-5 Dimensions– 5 Levels (EQ-5D-5L). Five evaluated dimensions include mobility, self-care, usual activity, pain/discomfort and anxiety/depression. Each dimension has five options for response from no problem to extreme problem [25], producing 3125 possible health states, which can be converted to 3125 corresponding health utility index (or EQ-5D index) by using the Vietnamese cross-walk value set [26]. Patients answering “No problem” was classified into “No problem” group; otherwise, they were categorized into “Having problem” group. Furthermore, we used the EQ-Visual Analogue Scale (VAS) to measure the global health state of patients, with a score ranging from 0 “The worse health that you can imagine” to 100 “The best health that you can imagine” [25]. The EQ-VAS score was transformed to 1-point scale by dividing patients’ score to 100.
Statistical analysis
Stata version 13 (Stata Corp. LP, College Station, USA) was used to analyze the data. Exploratory factor analysis (EFA) was used to determine construct validity of the scales by identifying factors and distributing items into these factors in order to enhance the scales’ interpretability. Eigenvalues of 1.30 (for outpatient satisfaction scale) and 1.20 (for inpatient satisfaction scale) were used to define a threshold to flatten out the eigenvalue curves. These thresholds were determined by using the scree test (in S1 and S2 Figs). In addition, Orthogonal Varimax rotation with Kaisers' normalization were applied to reconstruct the items. A value of 0.35 was used as the cut-off point for factor loadings. Cronbach’s alpha was computed to examine the internal consistency of scales and subscales. Because data on patient satisfaction were right censored (with 100 point as maximum score), multivariate Tobit regression was used to determine the associated factors with each domain of the scale. P-value <0.05 was considered the statistical significance.
Ethics approval
This research proposal was approved by the IRB of Hanoi Medical University. Participants were requested to give written informed consent and were informed that they could withdraw at any time. Their contact details were coded and ensured to be confidential (code: 03.18/HDDDDHYHN).
Results and discussion
Table 1 showed the demographic characteristics of respondents. The mean age of patients was 57.2 (SD = 19.9) years old. The majority was female (58.5%), having less than high school education (65.5%), living in rural areas (53.3%) and having health insurance (82.7%). There were statistically significant differences in gender, education, age and having health insurance between outpatients and hospitalized patients in this study.
Table 1. Demographic characteristics of respondents.
| Characteristics | Outpatients | Inpatients | Total | p-value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Total | 300 | 50.0 | 300 | 50.0 | 600 | 100.0 | |
| Gender | |||||||
| Male | 89 | 29.7 | 160 | 53.3 | 249 | 41.5 | <0.01 |
| Female | 211 | 70.3 | 140 | 46.7 | 351 | 58.5 | |
| Education | |||||||
| < High school | 189 | 63.0 | 204 | 68.0 | 393 | 65.5 | <0.01 |
| High school | 71 | 23.7 | 39 | 13.0 | 110 | 18.3 | |
| > High school | 40 | 13.3 | 57 | 19.0 | 97 | 16.2 | |
| Living location | |||||||
| Urban | 141 | 47.0 | 139 | 46.3 | 280 | 46.7 | 0.87 |
| Rural | 159 | 53.0 | 161 | 53.7 | 320 | 53.3 | |
| Having health insurance | |||||||
| Yes | 212 | 70.7 | 284 | 94.7 | 496 | 82.7 | <0.01 |
| No | 88 | 29.3 | 16 | 5.3 | 104 | 17.3 | |
| Having problems in | |||||||
| Mobility | 69 | 23.0 | 80 | 26.7 | 149 | 24.8 | 0.30 |
| Self-care | 46 | 15.3 | 73 | 24.3 | 119 | 19.8 | <0.01 |
| Usual activities | 58 | 19.3 | 78 | 26.0 | 136 | 22.7 | 0.51 |
| Pain/ Discomfort | 129 | 43.0 | 104 | 34.7 | 233 | 38.8 | 0.04 |
| Anxiety/Depression | 124 | 41.3 | 87 | 29.0 | 211 | 35.2 | 0.02 |
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 59.5 | 12.9 | 54.8 | 24.9 | 57.2 | 19.9 | <0.01 |
| EQ-5D index | 0.82 | 0.20 | 0.81 | 0.22 | 0.82 | 0.21 | 0.76 |
| EQ-VAS | 0.77 | 0.13 | 0.79 | 0.14 | 0.78 | 0.14 | 0.02 |
Table 2 revealed that after conducting EFA for the patient satisfaction scale for inpatient service, five domains were detected namely: “Attitude of medical staff” (14 items), “Care and Treatment” (4 items), “Health service accessibility” (5 items), “Waiting time” (4 items) and “Hospital facilities” (3 items), with the values of Cronbach’s alpha being 0.97; 0.94; 0.79; 0.72; and 0.74, respectively. The highest percentage of people having complete satisfaction was 42.0% in “Attitude of Nurse”, while the lowest percentage was 4.3% in “Flat hospital walkway and corridor, which made people easy to go”. People had the highest score in “Care and treatment” (Mean = 85.6, SD = 9.7) and the lowest score in “Hospital facilities” (Mean = 78.3; SD = 9.2).
Table 2. Factor loading and reliability of the patient satisfaction scale for inpatient service.
| % completely satisfy | The attitude of medical staff | Care and treatment | Health service accessibility | Waiting time | Hospital facilities | |
|---|---|---|---|---|---|---|
| Nurses guide patients on how to take medicine daily | 27.7 | 0.868 | ||||
| Medical staff informed about the drug clearly to patients before taking drugs | 27.3 | 0.866 | ||||
| An attitude of physicians and nurses when doing professional techniques on patients | 31.7 | 0.852 | ||||
| Staff guide carefully administrative procedure when the patient discharge | 24 | 0.849 | ||||
| Physicians guide carefully patients how to self-care | 30.3 | 0.833 | ||||
| Attitude of physicians | 40.3 | 0.814 | ||||
| Physicians explain carefully illness conditions to the patient | 34.7 | 0.81 | ||||
| Attitude of nurses | 42 | 0.801 | ||||
| An attitude of medical staff when patients admitted to the hospital | 40.3 | 0.795 | ||||
| The attitude of staff when doing payment procedures | 21.7 | 0.78 | ||||
| Provide sufficient hospital clothes | 26 | 0.755 | ||||
| Physicians guide carefully when the patient discharge | 25 | 0.752 | ||||
| Medical staff had a friendly attitude when communicating | 42 | 0.703 | ||||
| Hospital has good security | 21.3 | 0.601 | ||||
| Satisfaction with the overall effectiveness of service | 28 | 0.876 | ||||
| Physicians’ quality of diagnosis and treatment | 28 | 0.85 | ||||
| Satisfaction with overall quality of care | 33.3 | 0.78 | ||||
| Nurse’s quality of care and treatment | 37.3 | 0.704 | ||||
| Clear and understandable signboards, maps to show the way to go to the Department, | 5.7 | 0.816 | ||||
| Building block, stair, rooms are easy to find | 5.3 | 0.805 | ||||
| Time for visiting patients is informed clearly | 4.7 | 0.686 | ||||
| Patients can call or ask medical staff if need. | 19.7 | 0.685 | ||||
| Flat hospital walkway and corridor, which made people easy to go | 4.3 | 0.581 | ||||
| Waiting time for diagnosis | 11 | 0.724 | ||||
| Waiting time for admitting hospital | 10 | 0.699 | ||||
| Waiting time when needing medical staff | 13.3 | 0.6 | ||||
| Waiting time when paying hospital fee | 19.6 | 0.564 | ||||
| Equipment and facilities in the room are sufficient | 7.3 | 0.824 | ||||
| Equipment and facilities for doing professional techniques are sufficient | 7.7 | 0.765 | ||||
| Hospital had the good hygienic condition | 10 | 0.686 | ||||
| Cronbach’s Alpha | 0.966 | 0.940 | 0.794 | 0.724 | 0.736 | |
| Mean | 85.5 | 85.6 | 80.1 | 79.5 | 78.3 | |
| SD | 8.6 | 9.7 | 6.0 | 7.3 | 9.2 |
Table 3 showed the EFA results for the patient satisfaction scale for outpatient service. We also separated these items into five domains namely: “Attitude of medical staff” (10 items), “Care and Treatment” (3 items), “Health service accessibility” (4 items), “Waiting time” (10 items) and “Hospital facilities” (3 items), with the values of Cronbach’s alpha being 0.97; 0.86; 0.90; 0.91; and 0.61, respectively. The highest percentage of people having complete satisfaction was 19.7% in “Attitude of physicians when examining, guiding and explaining to the patient”, while the lowest percentage was 4.3% in “Good hygienic condition”. People had the highest score in “Attitude of medical staff” (Mean = 82.8; SD = 7.9) and the lowest score in “Waiting time” (Mean = 76.6; SD = 8.2).
Table 3. Factor loading and reliability of the patient satisfaction scale for outpatient service.
| % completely satisfy | The attitude of medical staff | Care and treatment | Health service accessibility | Waiting time | Hospital facilities | |
|---|---|---|---|---|---|---|
| The attitude of the staff in the abdominal/ vascular ultrasound department | 17 | 0.942 | ||||
| The attitude of staff in the echocardiography department | 17.7 | 0.941 | ||||
| The attitude of staff at the laboratory | 17.3 | 0.941 | ||||
| The attitude of staff in electrocardiogram room | 17.3 | 0.933 | ||||
| The attitude of staff collecting hospital fee | 18.3 | 0.901 | ||||
| The attitude of the nurse to patients before the examination | 18.3 | 0.881 | ||||
| Attitude of receptionist | 18 | 0.877 | ||||
| The attitude of physicians when examining, guiding and explaining to the patient | 19.7 | 0.815 | ||||
| Security staff had the good attitude with patients | 19.3 | 0.806 | ||||
| Hospital had good security condition | 11.7 | 0.59 | ||||
| Satisfaction with the overall effectiveness of service | 11.3 | 0.872 | ||||
| Physicians’ quality of diagnosis and treatment | 10.3 | 0.86 | ||||
| Satisfaction with overall quality of care | 12.7 | 0.676 | ||||
| Building block, stair, rooms are easy to find | 5.3 | 0.906 | ||||
| Clear and understandable signboards, maps to show the way to go to the Department, | 5.3 | 0.895 | ||||
| Flat hospital walkway and corridor, easy to go | 5.3 | 0.85 | ||||
| Patients can call or ask medical staff if need. | 10.7 | 0.73 | ||||
| Waiting time for X-ray and getting X-ray results | 5 | 0.825 | ||||
| Waiting time for payment procedure at the reception desk | 7 | 0.810 | ||||
| Waiting time for electrocardiogram | 6.3 | 0.797 | ||||
| Waiting time for abdominal/vascular ultrasound | 5 | 0.786 | ||||
| Waiting time for counseling | 7 | 0.785 | ||||
| Waiting time for echocardiography | 5 | 0.763 | ||||
| Waiting time for a medical examination | 6 | 0.743 | ||||
| Waiting time for testing and getting test results | 5.7 | 0.682 | ||||
| Waiting time for taking medicine at the drug store | 7.7 | 0.644 | ||||
| Waiting time for reading the results at physician’s room | 5 | 0.632 | ||||
| Good hygienic condition | 4.3 | 0.779 | ||||
| Ensuring the confidentiality and privacy when examination or doing technique | 6 | 0.691 | ||||
| Good light and water | 4.7 | 0.589 | ||||
| Cronbach’s Alpha | 0.973 | 0.863 | 0.900 | 0.913 | 0.612 | |
| Mean | 82.8 | 80.5 | 80.4 | 76.6 | 78.1 | |
| SD | 7.9 | 8.0 | 5.9 | 8.2 | 7.5 |
Table 4 compared the score of different domains of patient satisfaction according to EFA results. Domains "Attitude of staff", "Care and treatment", and "Hospital facilities" had significantly higher scores in inpatients than those in outpatients (p<0.01). Meanwhile, there was no difference in "Health service accessibility" and "Hospital facilities" for inpatients and outpatients. Overall, patients were more satisfied with inpatient service (Mean = 81.8, SD = 5.8) than outpatient services (Mean = 79.7, SD = 5.2, p<0.01).
Table 4. Comparison of patient’s satisfaction between inpatients and outpatients.
| Factors | Inpatients | Outpatients | p-value | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | % rate 100 point | Mean | SD | % rate 100 point | ||
| Health service accessibility | 80.1 | 6.0 | 5.0 | 80.4 | 5.9 | 3.3 | 0.60 |
| Waiting time | 79.5 | 7.3 | 4.3 | 76.6 | 8.2 | 4.3 | <0.01 |
| Hospital facilities | 78.3 | 9.2 | 9.7 | 78.1 | 7.5 | 6.3 | 0.82 |
| Attitude of staff | 85.5 | 8.6 | 4.0 | 82.8 | 7.9 | 14.3 | <0.01 |
| Care and treatment | 85.6 | 9.7 | 8.0 | 80.5 | 8.0 | 26.0 | <0.01 |
| Total score | 81.8 | 5.8 | 1.7 | 79.7 | 5.2 | 1.3 | <0.01 |
Table 5 presents the results of multivariate regression to identify the predictors of the satisfaction score among outpatients. People not having health insurance had significantly higher scores in “Health service accessibility”, “Waiting time”, “Hospital facilities” and “Attitude of staff” domains as well as “Overall satisfaction”. People having pain/discomfort, anxiety/depression and problems with self-care had significantly lower satisfaction scores in “Care and Treatment” and overall satisfaction. Similarly, having a higher EQ-5D index was associated with a significantly lower satisfaction score in similar domains.
Table 5. Factors associated with patient satisfaction among outpatients.
| Variables | Health service accessibility | Waiting time | Hospital facilities | Attitude of staff | Care and treatment | Overall satisfaction | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | |
| Age groups (vs < 30 yearsa) | ||||||||||||
| 30-<45 years | 1.7 | -3.8; 7.1 | 5.4 | -1.9; 12.7 | -1.7 | -8.4; 4.9 | -9.7* | -17.4; -2.0 | -1.9 | -9.4; 5.5 | -1.0 | -5.6; 3.5 |
| 45-<60 years | 1.9 | -3.2; 7.1 | 5.1 | -1.7; 12.0 | 0.4 | -5.9; 6.6 | -7.0 | -14.3; 0.3 | -0.1 | -7.1; 6.8 | 0.1 | -4.1; 4.4 |
| ≥ 60 years | 1.5 | -3.6; 6.6 | 4.0 | -2.8; 10.7 | -1.1 | -7.2; 5.1 | -6.6 | -13.8; 0.7 | -1.2 | -8.1; 5.7 | -0.5 | -4.7; 3.7 |
| Gender (Female vs Malea) | 0.8 | -0.8; 2.4 | 1.5 | -0.7; 3.6 | 0.1 | -1.9; 2.0 | 0.5 | -1.8; 2.7 | 0.4 | -1.8; 2.6 | 0.6 | -0.7; 2.0 |
| Education attainment (vs < High schoola) | ||||||||||||
| High school | -1.0 | -2.7; 0.8 | -1.2 | -3.6; 1.1 | -2.0 | -4.1; 0.2 | -0.1 | -2.5; 2.3 | -0.6 | -3.0; 1.7 | -0.9 | -2.4; 0.5 |
| > High school | -1.2 | -3.4; 1.1 | 1.6 | -1.4; 4.6 | -1.3 | -4.0; 1.5 | 1.6 | -1.5; 4.8 | -1.2 | -4.2; 1.8 | -0.1 | -2.0; 1.7 |
| Living location (Rural vs Urbana) | -0.5 | -2.0; 1.0 | -0.6 | -2.6; 1.4 | 1.9* | 0.1; 3.7 | -0.1 | -2.2; 1.9 | -1.4 | -3.4; 0.6 | -0.1 | -1.4; 1.1 |
| Having health insurance (No vs Yesa) | 1.6* | 0.0; 3.2 | 3.2* | 1.1; 5.3 | 3.0* | 1.0; 4.9 | 2.7* | 0.5; 4.9 | 0.3 | -1.9; 2.4 | 2.0* | 0.7; 3.3 |
| Having problems in | ||||||||||||
| Pain/ Discomfort (Yes vs Noa) | -2.5 | -6.3; 1.2 | -3.6 | -8.6; 1.4 | -3.3 | -7.9; 1.2 | -4.8 | -9.9; 0.4 | -9.9* | -15.2; -4.6 | -4.4* | -7.4; -1.3 |
| Anxiety/Depression (Yes vs Noa) | -0.3 | -3.3; 2.6 | -3.8 | -7.8; 0.1 | -2.1 | -5.7; 1.4 | -1.6 | -5.6; 2.5 | -5.7* | -9.9; -1.6 | -2.5* | -4.9; -0.0 |
| Mobility (Yes vs Noa) | -1.9 | -5.3; 1.6 | 1.8 | -2.9; 6.4 | -0.9 | -5.1; 3.4 | -0.7 | -5.5; 4.1 | -1.3 | -6.1; 3.5 | -0.5 | -3.4; 2.4 |
| Self-care (Yes vs Noa) | -0.8 | -5.2; 3.6 | -3.0 | -8.9; 2.8 | 2.3 | -3.0; 7.7 | -2.4 | -8.4; 3.6 | -7.7* | -13.7; -1.7 | -2.0 | -5.7; 1.6 |
| Usual activities (Yes vs Noa) | 1.0 | -3.4; 5.4 | -1.1 | -7.0; 4.8 | -3.9 | -9.3; 1.4 | -0.4 | -6.5; 5.6 | -3.2 | -9.3; 2.8 | -1.5 | -5.1; 2.2 |
| EQ-VAS | -1.8 | -7.8; 4.1 | 4.0 | -3.9; 12.0 | 5.9 | -1.3; 13.1 | 1.7 | -6.5; 9.9 | 1.7 | -6.4; 9.7 | 2.3 | -2.6; 7.2 |
| EQ-5D index | -7.4 | -26.3; 11.6 | -16.2 | -41.5; 9.1 | -17.8 | -40.8; 5.3 | -15.0 | -41.2; 11.1 | -44.8* | -72.2; -17.5 | -18.2* | -33.9; -2.5 |
a reference group;
*p<0.05.
Table 6 presents the factors associated with patient satisfaction among inpatients. Being older than 60 years old was found to associated with significantly higher satisfaction in “Waiting time”, “Hospital facilities”, “Care and treatment” domains and overall satisfaction. Females had significantly higher scores in “Health service accessibility”, “Hospital facilities”, “Attitude of staff” domains as well as overall. Having anxiety/depression was found to correlate with the lower score in the domains of “Waiting time”, “Attitude of staffs” and Overall satisfaction. In contrast, people having problems with self-care reported significantly higher satisfaction score overall as well as in “Health service accessibility” and “Waiting time” domains. People not having health insurance had higher scores in “Health service accessibility”, “Hospital facilities” and overall satisfaction.
Table 6. Factors associated with patient satisfaction among inpatients.
| Variables | Health service accessibility | Waiting time | Hospital facilities | Attitude of staff | Care and treatment | Overall satisfaction | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | Coef. | 95%CI | |
| Age groups (vs < 30 yearsa) | ||||||||||||
| 30-<45 years | -0.7 | -3.8; 2.5 | 0.2 | -3.5; 4.0 | -0.6 | -5.5; 4.3 | 2.8 | -2.2; 7.7 | -0.4 | -7.0; 6.2 | 0.1 | -2.8; 2.9 |
| 45-<60 years | -1.0 | -3.4; 1.5 | 1.4 | -1.5; 4.3 | -0.0 | -3.8; 3.7 | -0.2 | -4.0; 3.5 | 2.0 | -3.1; 7.1 | 0.2 | -2.0; 2.4 |
| ≥ 60 years | 0.1 | -2.0; 2.2 | 2.5 | -0.0; 5.0 | 3.4* | 0.1; 6.6 | 2.6 | -0.7; 5.9 | 5.2* | 0.8; 9.7 | 2.3* | 0.4; 4.2 |
| Gender (Female vs Malea) | 1.6* | 0.2; 3.0 | 0.9 | -0.8; 2.5 | 2.0 | -0.2; 4.2 | 2.7* | 0.5; 4.9 | 2.1 | -0.9; 5.1 | 1.6* | 0.3; 2.9 |
| Education attainment (vs< High schoola) | ||||||||||||
| High school | -1.1 | -3.2; 1.1 | 0.5 | -2.1; 3.1 | 2.3 | -1.1; 5.7 | 0.0 | -3.3; 3.4 | 1.3 | -3.3; 5.8 | 0.4 | -1.6; 2.4 |
| > High school | 0.3 | -1.6; 2.3 | 1.6 | -0.7; 3.9 | -1.1 | -4.1; 2.0 | 0.5 | -2.6; 3.5 | 0.2 | -3.9; 4.4 | 0.1 | -1.6; 1.9 |
| Living location (Rural vs Urbana) | -0.3 | -1.8; 1.2 | -0.3 | -2.1; 1.5 | -1.8 | -4.1; 0.6 | -1.4 | -3.7; 1.0 | -1.3 | -4.5; 1.8 | -0.9 | -2.2; 0.5 |
| Having health insurance (No vs Yesa) | 3.8* | 0.6; 7.0 | 2.4 | -1.3; 6.2 | 6.0* | 1.0; 10.9 | 1.7 | -3.2; 6.6 | 2.3 | -4.3; 9.0 | 3.1* | 0.2; 5.9 |
| Having problems in | ||||||||||||
| Pain/Discomfort (Yes vs Noa) | -1.7 | -4.8; 1.3 | -2.0 | -5.6; 1.6 | -2.6 | -7.3; 2.1 | -2.1 | -6.8; 2.7 | -0.6 | -6.9; 5.8 | -1.7 | -4.4; 1.1 |
| Anxiety/Depression (Yes vs Noa) | -1.2 | -3.6; 1.2 | -3.9* | -6.7; -1.1 | -0.9 | -4.5; 2.8 | -4.7* | -8.5; -1.0 | -3.7 | -8.7; 1.3 | -2.5* | -4.7; -0.4 |
| Mobility (Yes vs Noa) | -0.1 | -3.9; 3.7 | 2.2 | -2.4; 6.7 | -1.9 | -7.8; 4.0 | 2.0 | -3.9; 8.0 | 1.3 | -6.9; 9.4 | 0.6 | -2.9; 4.0 |
| Self-care (Yes vs Noa) | 4.7* | 0.8; 8.5 | 4.6 | -0.0; 9.2 | 2.6 | -3.4; 8.5 | 4.7 | -1.3; 10.6 | 2.0 | -6.2; 10.1 | 3.5* | 0.1; 7.0 |
| Usual activities (Yes vs Noa) | -5.1* | -9.5; -0.7 | -3.9 | -9.1; 1.3 | -0.3 | -7.1; 6.4 | -6.6 | -13.4; 0.1 | -2.6 | -11.9; 6.6 | -3.5 | -7.4; 0.5 |
| EQ-VAS | 0.6 | -5.3; 6.5 | 3.0 | -4.1; 10.0 | 7.8 | -1.3; 16.9 | -8.9 | -18.0; 0.3 | -5.0 | -17.4; 7.5 | -0.1 | -5.5; 5.2 |
| EQ-5D index | -4.3 | -18.8; 10.2 | -2.8 | -20.2; 14.5 | -5.0 | -27.5; 17.5 | -0.8 | -23.4; 21.8 | 2.7 | -27.8; 33.2 | -2.1 | -15.3; 11.0 |
a reference group;
*p<0.05.
Discussion
In the absence of an officially available instrument to examine the satisfaction of patients with CVDs in Vietnam, we have developed and applied our own assessment questionnaire based on research on existing literature on the subject. With satisfactory internal consistency, our instrument can be used with suitable modifications to measure the level of satisfaction of patients with CVDs in various settings. The results of our analysis provide some interesting insights into the level and determinants of satisfaction among those with heart disease, which in turn suggest that improvements at both facility-level and policy-level are needed for improving outcomes of treatment services.
The Cronbach’s alpha reliability coefficient of this scale, as derived from our analyses, was within a range of values considered sufficient for a patient satisfaction scale to be reliable [27]. In general, test developers typically strive for an instrument with a coefficient for reliability in the range of .80 to .90, in some other cases a minimum of 0.7 for Cronbach’s alpha might be considered as a good result [27–29]. Our efforts in distinguishing between inpatient and outpatient services when developing the scale have enabled a more sophisticated capture of patient satisfaction regarding each of these services. Nonetheless, as the capacity of Cronbach’s alpha in determining the reliability of an instrument has been subjected to debate in existing literature [30, 31], it is recommended that future researches employing our scale conduct an additional investigation as well as consider alternative measures of instrument reliability.
In accordance with findings from other studies on patients’ perception of the quality of care, “Attitude of medical staff” and “Care and treatment” domains had the highest score in outpatient and inpatient groups, respectively [15]. A previous study indicated that positive experience with medical staffs is closely associated with the subjective evaluation of the patients regarding quality of health care received during their hospital stay [28], while other researches highlighted the importance of having confidence in expertise and attentiveness of nurses and doctors on perception of patients on care quality [32, 33]. Existing literature also suggested that healthcare provider’s interpersonal communication skills and behaviors towards the patients were directly linked with patient satisfaction [34] This implies the dependency of providing the better quality of care on enhancing the capacity of medical staff both in terms of expertise and interpersonal, “soft” skills. Meanwhile, “Hospital facilities” appeared to be the area that more attention should be focused in an attempt to improve the satisfaction of inpatients, in line with findings elsewhere [35]. It has been proposed that since patients cannot reliably differentiate positive experiences with the physical environment from positive experiences with care, an improved, patient-centered hospital environment with features like reduced noise, improved natural light, visitor-friendly facilities, well-decorated rooms, and hotel-like amenities would lead to higher satisfaction of patients as well as medical staff [36]. The need for renovating and upgrading the physical environment of the hospitals thus should not be overlooked. "Waiting time" was the lowest score for outpatients, reflecting a well-established argument that longer waiting periods were negatively correlated with patient satisfaction ratings from the healthcare provider [37]. As a result, consideration should be made in conducting systematic metrics to reduce a long wait-times at the hospital level as part of the provision of better quality services [38].
In addition, our results echo findings from a number of existing studies where older age was reported to be positively associated with satisfaction score among those using inpatients services [39–41]. On the other hand, the correlation between being female and higher satisfaction scores found in our study adds to the wealth of mixed evidence on relationship between gender and satisfaction: while some studies found male gender to be the predictor of higher patient satisfaction score [39–41], others found opposite results [42] or no significant association [43]. Nonetheless, it was interesting to note that compared with those having health insurance, people without health insurance had a higher score in overall satisfaction as well as in domains relating to care accessibility and hospital facilities. This partly reflected an issue suggested elsewhere regarding the implementation of health insurance in Vietnam context, when patients covered by health insurance faced a higher likelihood of receiving a lower quality of services compared to those who make out-of-pocket, full payment for services instead of utilizing health insurance or due to lack of health insurance [44]. The existence of premium services at hospital–providing patients with higher quality care and facilities, a private room with nurses on call at all time, for instance [45], which are not covered by insurance may also be a reason for higher perceived satisfaction among those paying out-of-pocket in comparison with those using insurance-covered services. In addition, the lower satisfaction score given for “Attitude of staff” of those having insurance may be a sign of a problem that has been made aware by medical authority and reported by the media–the discrimination of health staff towards insurance holders [46, 47]. Nonetheless, further investigation into this matter should be encouraged to improve the effectiveness of the health insurance system and ensure fairness in the treatment received by patients.
This study has several implications. As our newly developed contextualized patient satisfaction scale was proved to be internally reliable, it can be utilized as the basis for further enhancement and validation that would ideally involve the support of authorities–Ministry of Health, for instance, to be sufficiently reliable for application beyond one hospital setting. Insights regarding the perceived satisfaction of patients with heart disease discovered through the application of such scale would pinpoint directions for improving the quality of care and experience of patients with treatment. This would be immensely valuable for Vietnamese hospitals as managerial and financial autonomy introduced through hospital administration reform imposed by the government force them to strive for better performance as service providers. Measuring the satisfaction of patients can also be conducted periodically as part of a quality assurance process as well as a component of larger service improvement strategies. In addition, finding concerning generally lower satisfaction of health insurance covered patients over non-covered ones prompts examination and possible reform of health insurance policy.
Nevertheless, the findings of this study should be view in light of its inherent limitations. First, the cross-sectional of the survey would allow only a ‘snap-shot' capture of the current situation. The self-reported design of the questionnaire meant that answers would be subjective. In addition, although the attempt was made to include a reasonably large number of participants in this study, further researches involving large sample sets and/or several studied sites are called for to better understand the factors associated with patient satisfaction and potentially enhance the design of the scale. Future studies should also consider clustering of patients based on their response, as such analysis would potentially shed more lights on heterogeneity and other sub-structures in patients’ experiences, providing a better understanding of patient satisfaction and associated factors.
Conclusions
The aim of this research is to evaluate the cardiovascular patient’s satisfaction in Vietnam through a patient satisfaction measurement scale developed and validated especially for the concerned population. Analyses indicated the scale to be internally reliable. Findings discovered through the application of the newly developed instrument showed low satisfaction regarding hospital facilities for inpatients and waiting time for outpatients, suggesting renovation efforts, while inferiority regarding patient satisfaction of health insurance covered patients compared to those without implied policy reform possibility. Further enhancement and validation of the developed instrument was required, which called for more support from the Ministry of Health.
Supporting information
(TIF)
(TIF)
Acknowledgments
We would like to express our gratitude to healthcare staff and participants at Hanoi Heart Hospital for supporting us perform this study.
Data Availability
Data cannot be shared publicly because of data restriction regulation of the Hanoi Heart Hospital. Requests for data can be sent to the Department of Quality Insurance, Hanoi Heart Hospital (Dr. Nguyen Thi Thu Huyen, hanoibvt@gmail.com) for researchers who meet the criteria for access to confidential data.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Sixma HJ, Kerssens JJ, Campen CV, Peters L. Quality of care from the patients' perspective: from theoretical concept to a new measuring instrument. Health Expect. 1998;1(2):82–95. Epub 2001/04/03. 10.1046/j.1369-6513.1998.00004.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dawn AG, Lee PP. Patient satisfaction instruments used at academic medical centers: results of a survey. American journal of medical quality: the official journal of the American College of Medical Quality. 2003;18(6):265–9. Epub 2004/01/14. 10.1177/106286060301800607 . [DOI] [PubMed] [Google Scholar]
- 3.Al-Abri R, Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman medical journal. 2014;29(1):3–7. Epub 2014/02/07. 10.5001/omj.2014.02 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg. 2014;260(4):592–8; discussion 8–600. Epub 2014/09/10. 10.1097/SLA.0000000000000932 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shirley ED, Sanders JO. Patient satisfaction: Implications and predictors of success. The Journal of bone and joint surgery American volume. 2013;95(10):e69 Epub 2013/05/17. 10.2106/JBJS.L.01048 . [DOI] [PubMed] [Google Scholar]
- 6.Wartman SA, Morlock LL, Malitz FE, Palm EA. Patient understanding and satisfaction as predictors of compliance. Med Care. 1983;21(9):886–91. Epub 1983/09/01. 10.1097/00005650-198309000-00005 . [DOI] [PubMed] [Google Scholar]
- 7.Marquis MS, Davies AR, Ware JE Jr. Patient satisfaction and change in medical care provider: a longitudinal study. Med Care. 1983;21(8):821–9. Epub 1983/08/01. 10.1097/00005650-198308000-00006 . [DOI] [PubMed] [Google Scholar]
- 8.Cardiovascular diseases (CVDs) 2017 [cited 2018 1 June]. http://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
- 9.Institute of Medicine (US) Committee on Social Security Cardiovascular Disability Criteria. Cardiovascular Disability Trends Cardiovascular Disability: Updating the Social Security Listings. Washington (DC): National Academies Press (US); 2010. [PubMed] [Google Scholar]
- 10.Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. 2018;18(1):975 10.1186/s12889-018-5806-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59. Epub 2017/09/19. 10.1016/S0140-6736(17)32154-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yusuf S, Wood D, Ralston J, Reddy KS. The World Heart Federation's vision for worldwide cardiovascular disease prevention. Lancet. 2015;386(9991):399–402. Epub 2015/04/22. 10.1016/S0140-6736(15)60265-3 . [DOI] [PubMed] [Google Scholar]
- 13.Martin CM. Chronic disease and illness care: adding principles of family medicine to address ongoing health system redesign. Can Fam Physician. 2007;53(12):2086–91. Epub 2007/12/14. . [PMC free article] [PubMed] [Google Scholar]
- 14.Collins K, Nicolson P. The meaning of 'satisfaction' for people with dermatological problems: reassessing approaches to qualitative health psychology research. J Health Psychol. 2002;7(5):615–29. Epub 2002/09/01. 10.1177/1359105302007005681 . [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez N, Quintana JM, Bilbao A, Escobar A, Aizpuru F, Thompson A, et al. Development and validation of an in-patient satisfaction questionnaire. International journal for quality in health care: journal of the International Society for Quality in Health Care / ISQua. 2005;17(6):465–72. Epub 2005/08/16. 10.1093/intqhc/mzi067 . [DOI] [PubMed] [Google Scholar]
- 16.Kleefstra SM, Kool RB, Veldkamp CM, Winters-van der Meer AC, Mens MA, Blijham GH, et al. A core questionnaire for the assessment of patient satisfaction in academic hospitals in The Netherlands: development and first results in a nationwide study. Quality & safety in health care. 2010;19(5):e24 Epub 2010/06/26. 10.1136/qshc.2008.030825 . [DOI] [PubMed] [Google Scholar]
- 17.Homer CJ, Fowler FJ, Gallagher PM, Shaul J, Uyeda M, Zaslavsky A, et al. The Consumer Assessment of Health Plan Study (CAHPS) survey of children's health care. The Joint Commission journal on quality improvement. 1999;25(7):369–77. Epub 1999/07/21. 10.1016/s1070-3241(16)30452-7 . [DOI] [PubMed] [Google Scholar]
- 18.Thayaparan AJ, Mahdi E. The Patient Satisfaction Questionnaire Short Form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Medical education online. 2013;18:21747 Epub 2013/07/26. 10.3402/meo.v18i0.21747 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. Cardiovascular diseases (CVD) in Viet Nam 2019 [cited 2019 19 October]. https://www.who.int/vietnam/health-topics/cardiovascular-diseases.
- 20.Trần Thị Cẩm Tú và cs. Nghiên cứu sự hài lòng của người bệnh về công tác khám chữa bệnh tại Bệnh viện Trung ương Huế năm 2012. Tạp chí Y học thực hành, 903: p54-60. 2014.
- 21.Decision No 3869/QD-BYT issuing forms and guide surveys on measuring satisfaction of patient and health care workers, (2019).
- 22.Norhayati MN, Masseni AA, Azlina I. Patient satisfaction with doctor-patient interaction and its association with modifiable cardiovascular risk factors among moderately-high risk patients in primary healthcare. PeerJ. 2017;5:e2983 Epub 2017/03/01. 10.7717/peerj.2983 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weidemann R, Schoenfelder T, Klewer J, Kugler J. Patient satisfaction in cardiology after cardiac catheterization: Effects of treatment outcome, visit characteristics, and perception of received care. Herz. 2016;41:313–9. 10.1007/s00059-015-4360-x [DOI] [PubMed] [Google Scholar]
- 24.Asadi-Lari M, Packham C, Gray D. Patients' satisfaction and quality of life in coronary artery disease. Health Qual Life Outcomes. 2003;1:57 Epub 2003/11/14. 10.1186/1477-7525-1-57 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.EQOL G. EQ-5D-5L User Guide: Basic information on how to use the EQ-5D-5L instrument. Rotterdam, The Netherlands2011.
- 26.Mai VQ, Sun S, Minh HV, Luo N, Giang KB, Lindholm L, et al. An EQ-5D-5L Value Set for Vietnam. Quality of Life Research. 2020. 10.1007/s11136-020-02469-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bujang MA, Omar ED, Baharum NA. A Review on Sample Size Determination for Cronbach's Alpha Test: A Simple Guide for Researchers. Malays J Med Sci. 2018;25(6):85–99. Epub 2019/03/28. 10.21315/mjms2018.25.6.9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goel S, Sharma D, Singh A. Development and validation of a patient satisfaction questionnaire for outpatients attending health centres in North Indian cities. J Health Serv Res Policy. 2014;19(2):85–93. Epub 2013/10/31. 10.1177/1355819613508381 . [DOI] [PubMed] [Google Scholar]
- 29.Bonett DG, Wright TA. Cronbach's alpha reliability: Interval estimation, hypothesis testing, and sample size planning. 2015;36(1):3–15. 10.1002/job.1960 [DOI] [Google Scholar]
- 30.McNeish D. Thanks coefficient alpha, we'll take it from here. Psychol Methods. 2018;23(3):412–33. Epub 2017/05/31. 10.1037/met0000144 [DOI] [PubMed] [Google Scholar]
- 31.Konerding U. Which kind of psychometrics is adequate for patient satisfaction questionnaires? Patient Prefer Adherence. 2016;10:2083–90. Epub 2016/10/28. 10.2147/PPA.S112398 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shan L, Li Y, Ding D, Wu Q, Liu C, Jiao M, et al. Patient Satisfaction with Hospital Inpatient Care: Effects of Trust, Medical Insurance and Perceived Quality of Care. PLoS One. 2016;11(10):e0164366 Epub 2016/10/19. 10.1371/journal.pone.0164366 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aiken LH, Sloane DM, Ball J, Bruyneel L, Rafferty AM, Griffiths P. Patient satisfaction with hospital care and nurses in England: an observational study. BMJ Open. 2018;8(1):e019189 10.1136/bmjopen-2017-019189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson R, Barbara A, Feldman S. What patients want: A content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 2007;22(5):255–61. Epub 2007/05/15. . [PubMed] [Google Scholar]
- 35.Grogan S, Conner M, Norman P, Willits D, Porter I. Validation of a questionnaire measuring patient satisfaction with general practitioner services. Qual Health Care. 2000;9(4):210–5. Epub 2000/12/02. 10.1136/qhc.9.4.210 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siddiqui ZK, Zuccarelli R, Durkin N, Wu AW, Brotman DJ. Changes in patient satisfaction related to hospital renovation: experience with a new clinical building. J Hosp Med. 2015;10(3):165–71. Epub 2015/02/06. 10.1002/jhm.2297 . [DOI] [PubMed] [Google Scholar]
- 37.Bleustein C, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014;20(5):393–400. Epub 2014/09/03. . [PubMed] [Google Scholar]
- 38.Almomani I, AlSarheed A. Enhancing outpatient clinics management software by reducing patients' waiting time. J Infect Public Health. 2016;9(6):734–43. Epub 2016/10/30. 10.1016/j.jiph.2016.09.005 . [DOI] [PubMed] [Google Scholar]
- 39.Nguyen Thi PL, Briancon S, Empereur F, Guillemin F. Factors determining inpatient satisfaction with care. Soc Sci Med. 2002;54(4):493–504. Epub 2002/02/19. 10.1016/s0277-9536(01)00045-4 . [DOI] [PubMed] [Google Scholar]
- 40.Quintana JM, Gonzalez N, Bilbao A, Aizpuru F, Escobar A, Esteban C, et al. Predictors of patient satisfaction with hospital health care. BMC Health Serv Res. 2006;6:102 Epub 2006/08/18. 10.1186/1472-6963-6-102 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sahin B, Yilmaz F, Lee KH. Factors affecting inpatient satisfaction: structural equation modeling. J Med Syst. 2007;31(1):9–16. Epub 2007/02/08. 10.1007/s10916-006-9038-8 . [DOI] [PubMed] [Google Scholar]
- 42.Bener A, Ghuloum S. Gender difference on patients' satisfaction and expectation towards mental health care. 2013;16(3):285–91. 10.4103/1119-3077.113448 [DOI] [PubMed] [Google Scholar]
- 43.Chimatiro GL, Rhoda AJ, De Wit L. Stroke patients' outcomes and satisfaction with care at discharge from four referral hospitals in Malawi: A cross-sectional descriptive study in limited resource. Malawi Med J. 2018;30(3):152–8. Epub 2019/01/11. 10.4314/mmj.v30i3.4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Joint Annual Health Review 2012: Improving quality of medical services. Hanoi: Vietnam Ministry of Health, 2012.
- 45.Le N. Vietnam upgrades premium healthcare to attract high-spending patients. VnExpress. 2019 August 14, 2019.
- 46.Dang M. Congressman tells the story of being discriminated when seeking healthcare with health insurance. CAND online (candcomvn). 2013 November 9.
- 47.Hoang L. Public hospitals focusing on premium services, neglecting insurance holders? Tuoi tre online. 2019 August 8.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
Data Availability Statement
Data cannot be shared publicly because of data restriction regulation of the Hanoi Heart Hospital. Requests for data can be sent to the Department of Quality Insurance, Hanoi Heart Hospital (Dr. Nguyen Thi Thu Huyen, hanoibvt@gmail.com) for researchers who meet the criteria for access to confidential data.