Abstract
Objective To investigate the accuracy of the applied kinesiology muscle strength test for sacroiliac dysfunction and compared it with four validated orthopedic tests.
Methods This is a cross-sectional accuracy survey developed at a private practice in the city of Manaus, Brazil, during February 2017. The sample consisted of 20 individuals, with a median age of 33.5 years. Four tests were applied: distraction, thigh thrust, compression and sacral thrust, and the diagnosis was confirmed when three of these tests were positive. Soon after, the applied kinesiology test was applied to the piriformis muscle.
Results The prevalence of sacroiliac joint dysfunction was of 45%; the thigh thrust test had the highest specificity, and the sacral thrust test had the highest sensitivity. The applied kinesiology test presented good results (sensitivity: 0.89; specificity: 0.82; positive predictive value: 0.80; negative predictive value: 0.82; accuracy: 0.85; and area under the receiver operating characteristic [ROC] curve: 0.85).
Conclusion The applied kinesiology muscle strength test, which has great clinical feasibility, showed good accuracy in diagnosing sacroiliac joint dysfunction and greater discriminatory power for the existing dysfunction in comparison to other tests.
Keywords: sacroiliac joint, applied kinesiology, sensitivity and specificity
Introduction
The lumbar spine is the target of constant pain, namely low back pain; its prevalence ranges from 38.9% to 70% throughout life, 1 2 and it is considered a critical public health problem. 3 The sacroiliac joint is deemed the potential source of low back or gluteal region pain in 10% to 27% of the affected individuals. 4 5 6 Sacroiliac joint dysfunction (SIJD) results from a misalignment or abnormal movement of the ilium and sacrum bones, causing pain in or around the joint. 4
The gold standard diagnostic test for SIJD is joint blockade through fluoroscopy-guided intra-articular anesthetic injection. However, this is an invasive procedure involving exposure to radiation; in addition, its performance is challenging. 7 Compressive orthopedic tests, which cause pain, have good validity in diagnosing SIJD, 8 9 10 but require the application of four tests and positive results in at least three of them. 7 10 11 12
Applied kinesiology (AK) was developed in the 1960s by George Goodheart, an American chiropractor. Goodheart associated muscle function with the craniosacral system, energy meridians, hormonal, nutritional, and emotional factors, and reflexology; as such, each muscle is related to a specific body organ. 13 14 This assessment system uses specific diagnostic methods, including the manual muscle test, which evaluates changes in neuromuscular response to determine how and where the body is unbalanced so that it can be properly corrected. This method uses stimuli, also called challenges, to compare pretest and posttest muscle reactions; a challenge is considered positive when a muscle reaction is changed. 13 15 As such, when an unbalanced area is stimulated, an overloaded nervous system causes the previously normorreactive muscle to become temporarily non-reactive.
The International College of Applied Kinesiology (ICAK) has sought to test the effectiveness of its technique to facilitate both diagnosis and treatment 13 for various disorders, including low back pain. The few studies on AK often use chemical stimuli, with some substance that is harmful to humans, and emotional stimuli to seek proof of the method's effectiveness. 16 17 18 19 However, the literature lacks studies on the accuracy of the mechanical challenge, applying its concepts in patients with different types of musculoskeletal conditions. As such, the present study aimed to investigate the accuracy of the AK muscle strength test for SIJD using a mechanical challenge and comparing it with other validated orthopedic tests.
Methodology
A cross-sectional, descriptive accuracy study was conducted in February 2017. The non-probabilistic convenience sample consisted of 20 individuals. Individuals who visited the practice with suspected SIJD on the day of data collection were included and signed an informed consent form. The exclusion criteria were the presence of any kind of hip prostheses, congenital malformation and cognitive deficits which prevented the understanding of the test dynamics. The study was approved by the Human Research Ethics Committee of our institution, under CAAE number 62554916.7.0000.5020 and opinion number 1.901.399.
The subjects were evaluated by three different professionals. The first evaluator was responsible for ascertaining the patient's medical history, and for recording personal data and information about the sacroiliac joint pain. The second evaluator applied the four orthopedic tests – distraction, thigh thrust, compression and sacral thrust tests 4 20 –, which were chosen because of their high sensitivity and specificity. 4 7 8 10 20 21 22 The diagnosis of SIJD was established when at least three of these four tests were positive. 7 10 11 12
Shortly thereafter, the third evaluator, a physical therapist trained in osteopathy and AK methods, applied the manual AK strength test for SIJD using the mechanical challenge for the piriformis muscle (a muscle originating from this joint and chosen for the study). The initial position for muscle testing puts the muscle to be tested in the greatest advantage, with the synergists at a disadvantage, 23 24 as described subsequently. The test is performed as follows: 24
-
Stage 1 –Pretest muscle assessment:
1st step: with the patient in prone position, the evaluator asks him/her to flex one knee at 90° and to perform a slight external hip rotation and abduction, around 5° to 10°;
2nd step: the evaluator places the cephalic hand on the lateral aspect of the knee to prevent hip abduction, and the caudal hand on the most distal internal region of the flexed leg to resist external hip rotation;
3rd step: the patient is asked to perform an external thigh rotation and abduction against a manual resistance placed by the evaluator that will prevent movement resulting in an isometric contraction;
4th step: the evaluator will resist until he/she no longer detects increased strength against his/her hand. At this point, an additional, small force will be exerted by the evaluator on a tangent to the arc created by the body part to be tested, that is, in an attempt to internally rotate the thigh;
5th step: the evaluator verifies the tested muscle response, which can be pressure-resisting, normorreactive response, or a non-pressure-resisting response.
-
Stage 2 –Mechanical challenge:
To test a possible dysfunction, the evaluator performs a passive mobilization towards its correction, sustaining it for a few seconds and then abruptly releasing it, thus exacerbating a possible injury. In the present study, one of the following situations was manually performed to diagnose a possible dysfunction: anteroinferior mobilization of the right base of the sacrum; anterorinferior mobilization of the left base of the sacrum; posterosuperior mobilization of the right ilium; anteroinferior mobilization of the right ilium; posterosuperior mobilization of the left ilium; anterorinferior mobilization of the left ilium.
-
Stage 3 –Posttest muscle assessment:
After each challenge described in stage 2, the evaluator will redo the steps in stage 1 and check if the challenge was negative (that is, the muscle maintains the same reaction observed in the first stage) or positive (that is, the muscle reaction is different from the one observed in the first stage).
-
Stage 4 –Test conclusion:
Conclusion 1: if the evaluator detects no difference in the reactions before and after any of the stage-2 challenges, the test is considered negative for SIJD;
Conclusion 2: if the evaluator detects a difference in the reactions before and after any of the stage-2 challenges, the test is considered positive for SIJD; it is possible to accurately identify the dysfunction resulting in pain and to guide the treatment.
Data Analysis
The variables were descriptively studied according to their nature and distribution. Using the Statistical Package for the Social Sciences (SPSS, IBM Corp., Armonk, NY, US) software, version 22.0, the receiver operating characteristic (ROC) curve and the area under it were determined, as well as prevalence, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy for each test; SIJD was diagnosed when at least three of the four applied tests were positive. A 95% confidence interval (CI) was used.
Results
A total of 20 individuals were evaluated, with a median age of 33.5 years (26.8–43.0 years); 14 (70%) patients were men. The prevalence of SIJD was of 45% (n = 9), with 78% (7) of the cases symptomatic and 22% (2) asymptomatic regarding pain ( Table 1 ).
Table 1. Sample distribution according to gender, age and pain.
| Variable | Total sample ( n = 20) | SIJD + ( n = 9) | SIJD – ( n = 11) |
|---|---|---|---|
| Gender ( n ) | |||
| Female | 30% ( n = 6) | 50% ( n = 3) | 50% ( n = 3) |
| Male | 70% ( n = 14) | 42.9% ( n = 6) | 57.1% ( n = 8) |
| Age* (years) | 33.5 (26.8–43.0) | 36 (27.8–43.0) | 33.5 (26.8–43.0) |
| Pain | |||
| Yes | 55% ( n = 11) | 77.8% ( n = 7) | 36.4% ( n = 4) |
| No | 45% ( n = 9) | 22.2% ( n = 2) | 63.6% ( n = 7) |
Abbreviation: SIJD, sacroiliac joint dysfunction.
Note: *Result expressed in median and interquartile range (IQR) values.
The thigh thrust test showed maximum specificity and PPV (1.00), whereas the sacral thrust test showed the maximum sensitivity and NPV (1.00). As for accuracy, these same tests presented higher values than the others, and the thigh thrust was superior ( Table 2 ).
Table 2. Diagnostic accuracy of the clinical tests for sacroiliac joint evaluation.
| Distraction | Thigh thrust | Compression | Sacral thrust | Pain | Applied Kinesiology test | |
|---|---|---|---|---|---|---|
| Prevalence | 0.30 (0.15–0.52) | 0.40 (0.22–0.61) | 0.35 (0.18–0.57) | 0.55 (0.18–0.57) | 0.55 (0.18–0.57) | 0.50 (0.30–0.70) |
| Sensibility | 0.56 (0.27–0.81) | 0.89 (0.57–0.98) | 0.67 (0.35–0.88) | 1.00 (0.70–1.00) | 0.78 (0.45–0.94) | 0.89 (0.57–0.98) |
| Specificity | 0.91 (0.62–0.99) | 1.00 (0.74–1.00) | 0.91 (0.62–0.98) | 0.82 (0.52–0.95) | 0.64 (0.35–0.85) | 0.82 (0.52–0.95) |
| Positive predictive value | 0.83 (0.44–0.97) | 1.00 (0.68–1.00) | 0.86 (0.49–0.97) | 0.82 (0.52–0.95) | 0.64 (0.35–0.85) | 0.80 (0.49–0.94) |
| Negative predictive value | 0.71 (0.45–0.88) | 0.92 (0.65–0.99) | 0.77 (0.50–0.92) | 1.00 (0.70–1.00) | 0.78 (0.45–0.94) | 0.90 (0.60–0.98) |
| Accuracy | 0.75 (0.53–0.88) | 0.95 (0.76–0.99) | 0.80 (0.58–0.92) | 0.90 (0.70–0.97) | 0.70 (0.48–0.85) | 0.85 (0.64–0.95) |
| Area under the ROC curve | 0.73 (0.50–0.97) | 0.94 (0.82–1.00) | 0.79 (0.57–1.00) | 0.91 (0.77–1.00) | 0.71 (0.47–0.94) | 0.85 (0.67–1.00) |
Abbreviation: ROC, receiver operating characteristic.
Note: 95% confidence interval.
The AK muscle strength test had 0.89 of sensitivity and 0.82 of specificity, with a PPV of 0.80 and an NPV of 0.90 ( Table 2 ), and 85% of accuracy.
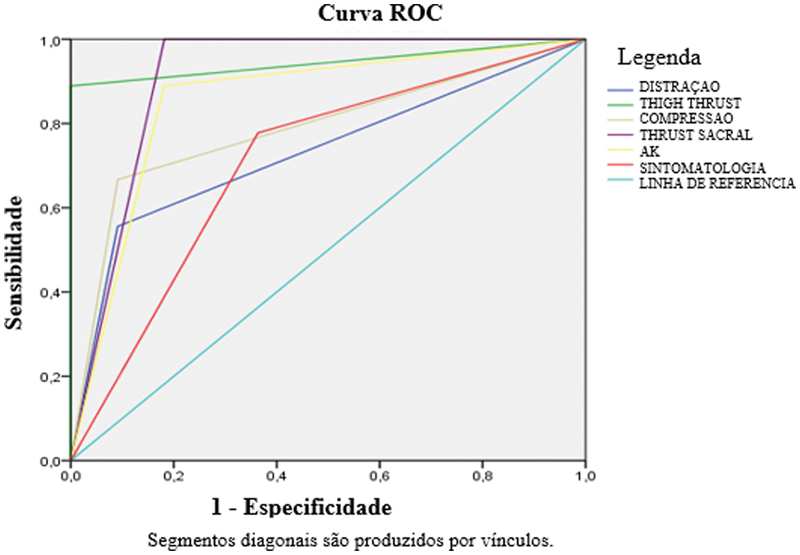
The ROC curve shown in Figure 1 demonstrated the superiority of the thigh thrust test, followed by the sacral thrust and the AK tests. These results are confirmed by the area under the ROC curve ( Table 2 ), in which these tests obtained values of 94%, 91% and 85% respectively. The compression and distraction tests, along with pain symptomatology, had lower accuracy (≤ 80%).
Fig. 1.
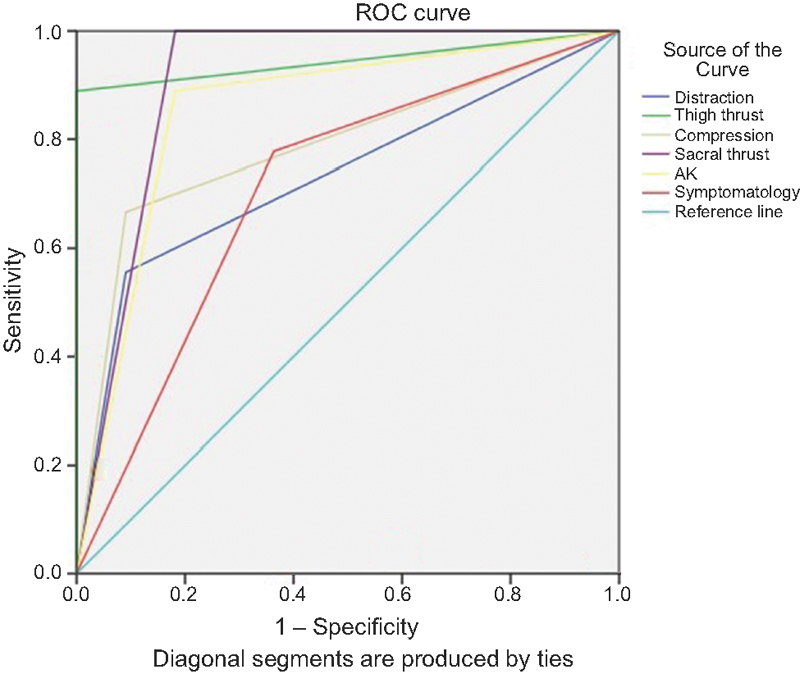
Receiver operating characteristic [ROC] curve from each test.
Discussion
The quality assessment of the AK muscle strength test to diagnose SIJD through a mechanical challenge yielded good results, with validity measures > 80%, highlighting its sensitivity and NPV.
The thigh thrust test had a high sensitivity value, of 89%, similar to the one found by Ramírez e Lemus, 4 of 83.3%. Its specificity was of 100%, confirming a finding from the systematic review performed by Stuber, 10 and consistent with the results from Arnbak et al, 25 of 85%. Laslett et al, 8 studying 48 patients from a radiology office in New Orleans, US, specialized in back pain diagnosis, showed that the thigh thrust test, when compared to the gold standard, had 88% of sensitivity and 92% of NPV, values close to the ones observed by us.
The thrust sacral test had 63% of sensitivity, 75% of specificity, 56% of PPV and 80% of VPN in the study by Laslett et al. 8 This test had expressive results in the present study, reaching the highest scores for sensitivity and NPV (100% in both), but also expressive results for specificity and PPV (82% in both). Ramírez and Lemus 4 obtained 100% sensitivity, whereas the highest value obtained by Stuber 10 was also for this item.
The four tests performed in the present study were also analyzed by Laslett et al, 8 who compared them to the gold standard and obtained 78% of specificity, 88% of sensitivity, 67% of PPV and 93% of NPV. In a concurrent validity, when comparing these results with those obtained with AK in the present study, absolute AK values are superior regarding specificity (82%), sensitivity (89%) and PPV (80%).
A relevant factor regarding the difference between the AK and both the gold standard and the compressive orthopedic tests is that the latter tests eventually diagnose a dysfunction due to a symptom, that is, pain. In addition, these tests do not specify which dysfunction is present, but only confirm its existence. The challenge-based AK test guides the therapist toward treatment, since a positive result indicates a specific dysfunction. 15 24 25 In the sacroiliac joint, these possible dysfunctions are described in the first step of stage 2 of the technique.
The AK muscle strength test is based on the principle of muscle response to a challenge. As such, if the muscle is able to adapt to the examiner's change in force, its neurological electrical function is intact. 26 27 Waxenegge et al 28 showed that the AK test was a useful tool in determining the prognosis of a therapy based on a cholesterol-reducing drug. In a review, Cuthbert and Goodheart 29 concluded that the AK test proved to be a clinically useful tool for diagnosing neuromusculoskeletal dysfunction.
The present study has some limitations, especially its small sample size. The small sample size might increase confidence intervals and reduce the precision in determining the accuracy of different tests. However, this is the first study investigating the accuracy of the AK muscle strength test for SIJD with methodological rigor in detailing the test application and blinding of the evaluators.
Conclusion
The AK muscle strength test has proven to be accurate in diagnosing SIJD, with accuracy similar to that of other known tests, such as the thigh thrust and sacral thrust test, and superior to the compression and distraction tests. The low cost and strong clinical feasibility of the AK test are noteworthy, along with its greater discriminatory power regarding the screening of an existing dysfunction. Further AK accuracy studies with larger samples of sacroiliac joints and comparison with a fluoroscopic joint blockade are recommended.
Conflito de Interesses Os autores declaram não haver conflito de interesses.
Trabalho desenvolvido na Universidade Federal do Amazonas, Manaus, AM, Brasil.
Work developed at Universidade Federal do Amazonas, Manaus, AM, Brazil.
Referências
- 1.Hoy D, Bain C, Williams G et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(06):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.van Tulder M, Becker A, Bekkering T et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15 02:S169–S191. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strine T W, Hootman J M. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57(04):656–665. doi: 10.1002/art.22684. [DOI] [PubMed] [Google Scholar]
- 4.Ramirez C R, Lemus D M. Disfunção da articulação sacro-ilíaca em jovens com dor lombar. Fisioter Mov. 2010;23(03):419–428. [Google Scholar]
- 5.Rupert M P, Lee M, Manchikanti L, Datta S, Cohen S P. Evaluation of sacroiliac joint interventions: a systematic appraisal of the literature. Pain Physician. 2009;12(02):399–418. [PubMed] [Google Scholar]
- 6.Hansen H C, McKenzie-Brown A M, Cohen S P, Swicegood J R, Colson J D, Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10(01):165–184. [PubMed] [Google Scholar]
- 7.Kennedy D J, Engel A, Kreiner D S, Nampiaparampil D, Duszynski B, MacVicar J. Fluoroscopically Guided Diagnostic and Therapeutic Intra-Articular Sacroiliac Joint Injections: A Systematic Review. Pain Med. 2015;16(08):1500–1518. doi: 10.1111/pme.12833. [DOI] [PubMed] [Google Scholar]
- 8.Laslett M, Aprill C N, McDonald B, Young S B. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(03):207–218. doi: 10.1016/j.math.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Robinson H S, Brox J I, Robinson R, Bjelland E, Solem S, Telje T. The reliability of selected motion- and pain provocation tests for the sacroiliac joint. Man Ther. 2007;12(01):72–79. doi: 10.1016/j.math.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Stuber K J. Specificity, sensitivity, and predictive values of clinical tests of the sacroiliac joint: a systematic review of the literature. J Can Chiropr Assoc. 2007;51(01):30–41. [PMC free article] [PubMed] [Google Scholar]
- 11.van der Wurff P, Buijs E J, Groen G J. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87(01):10–14. doi: 10.1016/j.apmr.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 12.Simopoulos T T, Manchikanti L, Singh V et al. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician. 2012;15(03):E305–E344. [PubMed] [Google Scholar]
- 13.Hall S, Lewith G, Brien S, Little P. A review of the literature in applied and specialised kinesiology. Forsch Komplement Med. 2008;15(01):40–46. doi: 10.1159/000112820. [DOI] [PubMed] [Google Scholar]
- 14.Gin R H, Green B N. George Goodheart, Jr., D.C., and a history of applied kinesiology. J Manipulative Physiol Ther. 1997;20(05):331–337. [PubMed] [Google Scholar]
- 15.Garten H. München: German Medical Society for Applied Kinesiology; 2008. Education: Diplomate of the International College of Applied Kinesiology. Introduction and: Systemic Disorders, General Strategies. [Google Scholar]
- 16.Schwartz S A, Utts J, Spottiswoode S J et al. A double-blind, randomized study to assess the validity of applied kinesiology (AK) as a diagnostic tool and as a nonlocal proximity effect. Explore (NY) 2014;10(02):99–108. doi: 10.1016/j.explore.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Schmitt W H, Jr, Leisman G.Correlation of applied kinesiology muscle testing findings with serum immunoglobulin levels for food allergies Int J Neurosci 199896(3-4):237–244. [DOI] [PubMed] [Google Scholar]
- 18.Peterson K B. A preliminary inquiry into manual muscle testing response in phobic and control subjects exposed to threatening stimuli. J Manipulative Physiol Ther. 1996;19(05):310–316. [PubMed] [Google Scholar]
- 19.Pollard H, Bablis P, Bonello R. Can the ileocecal valve point predict low back pain using manual muscle testing? Chiropr J Aust. 2006;36(02):58–62. [Google Scholar]
- 20.Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Manual Manip Ther. 2008;16(03):142–152. doi: 10.1179/jmt.2008.16.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eskander J P, Ripoll J G, Calixto F et al. Value of Examination Under Fluoroscopy for the Assessment of Sacroiliac Joint Dysfunction. Pain Physician. 2015;18(05):E781–E786. [PubMed] [Google Scholar]
- 22.Szadek K M, van der Wurff P, van Tulder M W, Zuurmond W W, Perez R S. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J Pain. 2009;10(04):354–368. doi: 10.1016/j.jpain.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Schmitt C, Hahn P T. A fisioterapia na síndrome do músculo piriforme: uma revisão da literatura. Rev UNINGÁ Rev. 2013;16(01):18–21. [Google Scholar]
- 24.Lawson A, Calderon L. Interexaminer agreement for applied kinesiology manual muscle testing. Percept Mot Skills. 1997;84(02):539–546. doi: 10.2466/pms.1997.84.2.539. [DOI] [PubMed] [Google Scholar]
- 25.Arnbak B, Jurik A G, Jensen R K, Schiøttz-Christensen B, van der Wurff P, Jensen T S. The diagnostic value of three sacroiliac joint pain provocation tests for sacroiliitis identified by magnetic resonance imaging. Scand J Rheumatol. 2017;46(02):130–137. doi: 10.1080/03009742.2016.1184308. [DOI] [PubMed] [Google Scholar]
- 26.Walter D S, Gavin D M. Pueblo: Systems DC; 1988. Applied Kinesiology. Synopsis. 2nd ed. [Google Scholar]
- 27.Oti J.The use of manual muscle testing to assess functional integration of high-threshold versus low-threshold alpha motor neuronsIn: Proceedings of the International College of Applied Kinesiology;2004
- 28.Waxenegger I, Endler P C, Wulkersdorfer B, Spranger H. Individual prognosis regarding effectiveness of a therapeutic intervention using pre-therapeutic “kinesiology muscle test”. ScientificWorldJournal. 2007;7:1703–1707. doi: 10.1100/tsw.2007.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuthbert S C, Goodheart G J., Jr On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat. 2007;15:4. doi: 10.1186/1746-1340-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]