Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection was declared a pandemic on 11 March 2020. We have since seen its fast spread worldwide. A likely contributing factor was the lack of symptoms of some of the carriers, making them unaware of their risk of spreading to other more vulnerable individuals. The other important finding has been the reported cases of infectivity despite lack of symptoms. We describe the SARS‐CoV‐2 pneumonia patterns in asymptomatic individuals. The common computed tomography (CT) thorax patterns found are peripheral ground‐glass opacification (GGO) with upper or lower lobe predominance. We believe screening for 2019‐novel coronavirus (COVID‐19) in high‐risk individuals may help identify the patients needing longer follow‐up.
Keywords: Computed tomography, COVID‐19, ground‐glass opacification, pneumonia, SARS‐CoV‐2
We describe the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) pneumonia patterns in asymptomatic individuals. The common computed tomography (CT) thorax patterns found are peripheral ground‐glass opacification (GGO) with upper or lower lobe predominance. We believe screening for 2019‐novel coronavirus (COVID‐19) in high‐risk individuals may help identify the patients needing longer follow‐up.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection was declared a pandemic by the World Health Organization on 11 March 2020. 2019‐Novel coronavirus (COVID‐19) is a positive single‐stranded RNA virus belonging to the β‐coronavirus cluster. To date, two fatal respiratory diseases in human history are SARS in 2002 and Middle East respiratory syndrome (MERS) in 2012.
Case Series
Case 1
An asymptomatic 45‐year‐old woman with no known medical illness was screened for SARS‐CoV‐2 after travelling back from Scotland. She tested positive for COVID‐19 and was admitted. Her oxygen saturation was 99% on room air with a respiratory rate (RR) of 16 breaths per minute (bpm). Examination of the respiratory system was unremarkable. Chest radiograph showed bilateral lower zone air space opacities (Fig. 1A). Her Modified Early Warning Score (MEWS) was 1. We proceeded with a high‐resolution computed tomography (HRCT), which showed bilateral peripheral lower zone ground‐glass opacification (GGO) (Fig. 1B). She was treated with oral hydroxychloroquine (HCQ), azithromycin, and lopinavir/ritonavir. Chest radiograph five days later showed significant improvement of GGO (Fig. 1C). COVID‐19 real‐time reverse transcription‐polymerase chain reaction (RT‐PCR) test was detected at day 10 of illness and became negative at day 14. She was discharged well.
Figure 1.
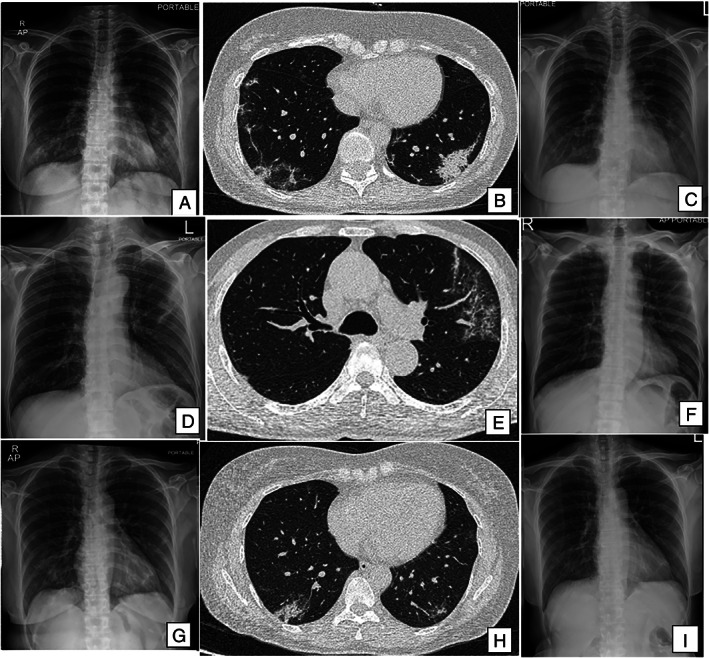
(A, D, G) Chest radiographs on admission showing various degrees of pneumonia. (B, E, H) High‐resolution computed tomography (HRCT) scans showing both ground‐glass opacification (GGO) and consolidation in the three patients. (C, F, I) Repeat chest radiographs showing resolution with treatment.
Case 2
A 62‐year‐old asymptomatic man was admitted after testing positive for COVID‐19 during contact screening. He was afebrile with RR of 20 bpm and oxygen saturation of 95% on room air. Chest examination was normal. Chest radiograph showed left upper zone peripheral consolidation (Fig. 1D). HRCT thorax showed peripheral GGOs involving both the left upper and right lower lobes (Fig. 1E). He was treated with HCQ and azithromycin. The MEWS remained at 1 point throughout admission. Repeated chest radiograph at day 5 showed resolution of the GGOs (Fig. 1F).
Case 3
A 52‐year‐old asymptomatic woman tested positive during screening after contact with a COVID‐19 individual. She had a background history of hypertension and was on perindopril 4 mg od. Clinical examination revealed a temperature of 37°C, RR of 16 bpm, and oxygen saturation of 99% on room air. Lung examination was clear. Chest radiograph showed air space opacities in the right lower zone (Fig. 1G). Her MEWS score was 2, and HRCT thorax showed evidence of bilateral lower zone peripheral GGOs (Fig. 1H). She was initiated on HCQ and azithromycin. She recovered well with interval radiological improvement (Fig. 1I, Table 1).
Table 1.
Demographics, clinical characteristics on admission, treatment, and outcomes of three patients with COVID‐19.
| Variables | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Demographics | |||
| Age | 47 | 62 | 52 |
| Gender | Female | Male | Female |
| Comorbidities | None | None | Hypertension |
| Smoking status | Lifelong non‐smoker | Smoker | Lifelong non‐smoker |
| Days from testing positive to admission | 2 | 5 | 6 |
| Clinical findings on presentation | |||
| Temperature (°C) | 36.9 | 37 | 37 |
| Respiratory rate (bpm) | 16 | 20 | 16 |
| O2 saturation (in room air, %) | 99 | 95 | 99 |
| Blood pressure (mmHg) | 108/64 | 147/87 | 163/97 |
| Heart rate (bpm) | 96 | 105 | 110 |
| MEWS | 1 | 2 | 1 |
| Laboratory results | |||
| Total white cell count (×109/L) | 5.1 | 8.0 | 5.1 |
| Absolute lymphocyte count (×109/L) | 2.2 | 2.3 | 2.1 |
| Absolute monocyte count (×109/L) | 0.4 | 1.2 | 0.5 |
| Absolute neutrophil count (×109/L) | 2.4 | 4.4 | 2.4 |
| Platelet (×109/L) | 285 | 467 | 414 |
| LDH (U/L) | 335 | 349 | 306 |
| C‐reactive protein (mg/dL) | 0.21 | 1.57 | 2.13 |
| D‐dimer (ng/mL) | 0.28 | 0.27 | 1.89 |
| Ferritin (μg/mL) | 182.72 | — | 103.67 |
| Fibrinogen (g/L) | 2.5 | 5.7 | 2.7 |
| Procalcitonin (ng/dL) | <0.02 | <0.02 | <0.02 |
| Radiological imaging | |||
| Chest radiograph | Left upper zone peripheral consolidation | Left upper zone peripheral consolidation | Air space opacities in the right lower zone |
| HRCT | Bilateral lower zone peripheral GGOs | Peripheral GGOs involving both the left upper and right lower lobes | Bilateral lower zone peripheral GGOs |
| Treatment and outcome | |||
| Drug therapy | HCQ | HCQ | HCQ |
| 400 mg bd Day 1 | 400 mg bd Day 1 | 400 mg bd Day 1 | |
| 200 mg bd Days 2–10 azithromycin | 200 mg bd Days 2–5 azithromycin | 200 mg bd Days 2–10 azithromycin | |
| 500 mg od Day 1 | 500 mg od Day 1 | 500 mg od Day 1 | |
| 250 mg od Days 2–5 lopinavir/ritonavir | 250 mg od Days 2–5 | 250 mg od Days 2–5 | |
| 400/100 mg bd Days 1–10 | |||
| Length of hospital stay (days) | 14 | 10 | 16 |
| Repeated COVID‐19 RT‐PCR test | Positive at day 10. Negative at days 13 and 14 | Negative at days 10 and 13 | Negative at days 10 and 13 |
bd, Twice daily; bpm, breaths per minute; COVID‐19, 2019‐novel coronavirus; GGO, ground‐glass opacification; HCQ, hydroxychloroquine; HRCT, high‐resolution computed tomography; LDH, lactate dehydrogenase; MEWS, Modified Early Warning Score; RT‐PCR, reverse transcription‐polymerase chain reaction.
Discussion
Patients with COVID‐19 have a wide range of symptoms with the majority presenting with an influenza‐like illness of fever, cough, rhinorrhoea, and sore throat [1]. Less common non‐respiratory symptoms include diarrhoea, anosmia, pericarditis, Guillain–Barré syndrome, or acute necrotizing encephalopathy [2, 3]. Observational studies have reported up to 12% of transmissions occurring before the onset of clinical symptoms [4].
Published data have shown that up to 75% of positive SARS‐CoV‐2 patients can be asymptomatic [5, 6]. All three patients in our case series displayed no symptoms of COVID‐19 disease despite showing radiological evidence of pneumonia. With the absence of symptoms, these patients may not have voluntarily come forward for screening. Screening based on symptoms alone may miss a significant amount of asymptomatic COVID‐positive patients. Targeted screening in these patients have allowed immediate isolation from the community and initiation of treatment which may have prevented disease progression and achieved earlier recovery.
The common laboratory abnormalities are lymphopenia, increased lactate dehydrogenase, and elevated C‐reactive protein [7]. These parameters are non‐specific and their clinical usefulness is limited. These abnormalities may be related to the cytokine storm in COVID‐19 and the changes are similar to patients with SARS and MERS.
We performed the initial imaging tool of chest radiograph which showed varying locations of pneumonia (Fig. 1). As COVID‐19 is a novel disease, we chose to proceed with a HRCT to allow further clarification on the extent of the pathologies. We found GGO with peripheral distribution and upper and lower lobes predominance in our patients. Our findings are similar with the known initial computed tomography (CT) manifestations of COVID‐19 [8]. The most common reported CT findings are isolated GGO or a combination of GGO and consolidative opacities [8]. Less common findings include interlobular septal thickening, bronchiectasis, pleural effusion, pleural thickening, and subpleural involvement, cavitation and lymphadenopathy [8]. On average, CT findings are most prominent on day 10 of illness and improve after day 14 [9].
In a study including nine hospitals from the region of Hubei, 16 (11.7%) out of 117 patients died from COVID‐19 disease [10]. A systematic review found the mortality rate to be higher from studies in Wuhan, the epicentre of this outbreak, with lower prevalence of death among patients from outside Wuhan. They also found that older patients with comorbidities may have a more severe impact from the disease [11].
All three patients in our report had a negative RT‐PCR test by day 13 of illness. A study reported a median of 36 days from the date of symptoms to the date of first negative RT‐PCR test, with the longest reported at 45 days from symptom onset [10]. More recent studies have shown that pharyngeal virus shedding does not equate to infectivity. This shedding appears to peak at day 4 and is the highest during the first week of symptoms [12].
This case series describes SARS‐CoV‐2 pneumonia patterns in asymptomatic individuals. The common CT thorax patterns found are peripheral GGO with upper or lower lobe predominance. We believe screening for COVID‐19 in high‐risk individuals is important to see the extent of pulmonary damage and assess the possible need for long‐term lung function follow‐up.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case series and accompanying images.
At the time this report was accepted for publication, the authors declared that the patients in this report had not been included in any previously published report on COVID‐19 that they had authored.
Ng, BH , Nik Abeed, NN , Abdul Hamid, MF , Soo, CI , Low, HJ , Ban, Y‐L . (2020) What happens when we treat the “Typhoid Mary” of COVID‐19. Respirology Case Reports, 8(6), e00604 10.1002/rcr2.604
Associate Editor: Tow Keang Lim
References
- 1. Guan W‐J, Ni Z‐Y, Hu Y, et al. 2020. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382(18):1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pan L, Mu M, Yang P, et al. 2020. Clinical characteristics of COVID‐19 patients with digestive symptoms in Hubei, China: a descriptive, cross‐sectional, multicenter study. Am. J. Gastroenterol. 115(5):766–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sedaghat Z, and Karimi N. 2020. Guillain Barre syndrome associated with COVID‐19 infection: a case report. J. Clin. Neurosci. 76:233–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Qian G, Yang N, Ma AHY, et al. 2020. A COVID‐19 transmission within a family cluster by presymptomatic infectors in China. Clin. Infect. Dis. 2020 Mar 23:ciaa316. 10.1093/cid/ciaa316. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Day M. 2020. Covid‐19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ 368:m1165. [DOI] [PubMed] [Google Scholar]
- 6. Tian S, Hu N, Lou J, et al. 2020. Characteristics of COVID‐19 infection in Beijing. J. Infect. 80(4):401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Salehi S, Abedi A, Balakrishnan S, et al. 2020. Coronavirus disease 2019 (COVID‐19): a systematic review of imaging findings in 919 patients. Am. J. Roentgenol. 1–7. 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 8. Pan F, Ye T, Sun P, et al. 2020. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID‐19) pneumonia. Radiology. 295(3):715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Xiao AT, Tong YX, and Zhang S. 2020. False‐negative of RT‐PCR and prolonged nucleic acid conversion in COVID‐19: rather than recurrence. J. Med. Virol. 10.1002/jmv.25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liu K, Fang YY, Deng Y, et al. 2020. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. 133(9):1025–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fu L, Wang B, Yuan T, et al. 2020. Clinical characteristics of coronavirus disease 2019 (COVID‐19) in China: a systematic review and meta‐analysis. J. Infect. 80(6):656–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wölfel R, Corman VM, Guggemos W, et al. 2020. Virological assessment of hospitalized patients with COVID‐2019. Nature. 581(7809):465–469. [DOI] [PubMed] [Google Scholar]


