Abstract
We aimed to evaluate the association of plasma biomarkers linked to inflammation (bacterial translocation, inflammatory response, and endothelial dysfunction), coagulopathy, and angiogenesis with the severity of liver cirrhosis (assessed by the Child-Pugh-Turcotte score, CTP) and Child-Pugh B cirrhosis (CTP 7–9) in patients with advanced hepatitis C virus (HCV)-related cirrhosis. We carried out a cross-sectional study in 97 patients with advanced HCV-related cirrhosis (32 HCV-monoinfected and 65 HIV/HCV-coinfected). Plasma biomarkers were measured by ProcartaPlex multiplex immunoassays. The outcome variable was the CTP score and the Child-Pugh B cirrhosis (CTP 7–9). HIV/HCV-coinfected patients and HCV-monoinfected patients with advanced HCV-related cirrhosis had near-equivalent values of plasma biomarkers. Higher values of plasma biomarkers linked to an inflammatory response (IP-10, IL-8, IL-6, and OPG), endothelial dysfunction (sVCAM-1 and sICAM-1), and coagulopathy (D-dimer) were related to higher CTP values. The most significant biomarkers to detect the presence of Child-Pugh B cirrhosis (CTP 7–9) were IP-10 (p-value= 0.008) and IL-6 (p-value=0.002). The AUC-ROC values of IP-10, IL-6, and both biomarkers combined (IP-10+IL-6) were 0.78, 0.88, and 0.96, respectively. In conclusion, HIV infection does not appear to have a significant impact on the analyzed plasma biomarkers in patients with advanced HCV-related cirrhosis. However, plasma biomarkers linked to inflammation (inflammatory response and endothelial dysfunction) were related to the severity of liver cirrhosis (CTP score), mainly IP-10 and IL-6, which discriminated patients with Child-Pugh B concerning Child-Pugh A.
Subject terms: Chemokines, Cytokines, Infectious diseases, Inflammation, Innate immunity, Hepatology, Hepatitis, HIV infections, Viral infection
Introduction
The hepatitis C virus (HCV) has a prevalence of active infection of around 1% worldwide (71 million people)1. HCV-infected patients progress slowly during decades (10 to 20 years), developing liver fibrosis and cirrhosis, which can evolve into decompensated cirrhosis and hepatocellular carcinoma2. Chronic hepatitis C causes chronic liver inflammation that accelerates the development of cirrhosis and other comorbidities3,4. The cirrhosis-associated immune dysfunction (CAID) is a pathophysiological process that appears in cirrhosis and is enhanced in advanced cirrhosis. The CAID is characterized by higher levels of inflammation, immune activation, and deregulation of the immune system, which are related to the progression to hepatic decompensation5,6. Patients with hepatic decompensation (Child–Turcotte–Pugh, CTP class B or C) could develop complications related to portal hypertension2. Additionally, chronic hepatitis C patients have an increased risk of thrombotic events because hepatocytes produce most blood proteins, and their concentration may be altered during cirrhosis progression7.
On the one hand, HCV infection is common among patients infected with human immunodeficiency virus (HIV) infection8. HIV/HCV coinfection influences the natural history of chronic hepatitis C, accelerating the progression to cirrhosis and end-stage liver disease in comparison to HCV-monoinfected patients9,10. This seems to be due to HIV infection that increases immune activation, HCV replication, HCV-induced hepatic inflammation, hepatocyte apoptosis, and microbial translocation5,11, which, in turn, contribute to the pathogenesis of both acquired immunodeficiency syndrome (AIDS) and non-AIDS related diseases12,13. Moreover, while suppressive antiretroviral therapy (ART) reduces the HIV impact on the body, it is unable to eradicate the virus. Thus, HIV-infected patients on suppressive ART still show increased bacterial translocation, immune activation, inflammation, and coagulopathy, which are linked to increased morbidity and mortality12.
On the other hand, HCV clearance with direct-acting antiviral agents (DAAs) promotes a decrease of liver disease severity and plasma biomarkers linked to bacterial translocation, immune activation, inflammation and coagulopathy in HIV/HCV-coinfected patients14–18 and HCV-monoinfected patients16,17,19,20. However, a percentage of patients maintain the risk of cirrhosis progression after HCV clearance with DAAs21,22. Besides, HIV/HCV-coinfected patients must face drug-drug interactions and hurdles with antiviral treatments, which support that patients coinfected with HIV/HCV might still be regarded as a particular population23.
Objective
We aimed to evaluate the association of plasma biomarkers linked to inflammation (bacterial translocation, inflammatory response, and endothelial dysfunction), coagulopathy, and angiogenesis with the severity of liver cirrhosis (assessed by the CTP score) and Child-Pugh B cirrhosis (CTP 7–9) in patients with advanced HCV-related cirrhosis.
Patients and methods
Patients
We carried out a cross-sectional study in 97 patients with advanced HCV-related cirrhosis who were selected from the ESCORIAL cohort (see Acknowledgements), which is a prospective cohort of patients with advanced HCV-related cirrhosis initiating anti-HCV therapy with all-oral DAAs at four tertiary referral hospitals in Madrid, Spain. All patients were enrolled between January and December 2015.
The inclusion criteria of the ESCORIAL cohort were: 1) plasma HCV RNA detectable by polymerase chain reaction; 2) one or more clinical criteria related to advanced cirrhosis (prior history of liver decompensation (ascites, bleeding esophageal varices, hepatic encephalopathy), or liver stiffness measurement (LSM) ≥25 kilopascals (kPa), or hepatic venous pressure gradient (HVPG) ≥10 mmHg, or CTP ≥7); 3) Initiation of all-oral DAA therapy; 4) a biological sample to carry out immunological assays. The exclusion criteria were: i) the previous diagnosis of hepatocellular carcinoma, ii) hepatitis B virus coinfection. The presence of HIV infection was not an exclusion criterion for the study.
In the present study, we only included patients with advanced HCV-related cirrhosis at baseline, when they had not yet started the HCV treatment. The ESCORIAL study included 112 patients, but 15 of them did not have a plasma sample at baseline, leaving only 97 patients available for the study (32 HCV-monoinfected patients and 65 HIV/HCV-coinfected patients.
The ESCORIAL study was conducted according to the Declaration of Helsinki, and the Research Ethics Committee of the Instituto de Salud Carlos III (CEI PI 41_2014) approved this study. Written informed consent was obtained by all the participants in the study.
Clinical data
Clinical and laboratory data were recorded using a standard database via an online form within each center, which satisfied local requirements of data confidentiality. This process was monitored to verify that all the information in the database was consistent with the patient’s records.
LSM was evaluated by trained operators by transient elastography (FibroScan, Echosens, Paris, France), as we previously described24, and results were reported in kPa, with a range of 2.5 to 75 kPa. The CTP score was calculated from five factors (total bilirubin, albumin, international normalized ratio, ascites, and encephalopathy) and range between 5 and 15 points25. CTP values serve to classify the patient into one of three severity classes of liver cirrhosis: A – Least severe liver disease (5–6 points), B – Moderately severe liver disease (7–9 points), and C – Most severe derangement (10–15 points). All HIV/HCV-coinfected patients were on ART and had undetectable plasma HIV viral load (<50 copies/mL) at least one year before the study.
Enzyme-linked immunosorbent assays
The Spanish HIV HGM BioBank collected plasma samples, which were stored until use at –80 °C. We evaluated plasma biomarkers by ProcartaPlex multiplex immunoassay (Bender MedSystems GmbH, Vienna, Austria) according to the manufacturer’s specifications using a Luminex 200 analyzer (Luminex Corporation, Austin, TX, United States). The plasma biomarkers measured by multiplex ELISA were: i) inflammatory response: IFN-γ-inducible protein 10 (IP-10), monocyte chemoattractant protein-1 (MCP1), IL-8, IL-1β, IL-18, IL-6, tumor necrosis factor-alpha (TNF-α), interleukin-1 receptor antagonist (IL-1RA), soluble receptor activator of nuclear factor- kappaB ligand (sRANKL) and osteoprotegerin (OPG); ii) endothelial dysfunction: soluble vascular cell adhesion molecule 1 (sVCAM-1), soluble intercellular cell adhesion molecule 1 (sICAM-1); and soluble tumor necrosis factor receptor 1 (sTNF-R1); iii) coagulopathy: plasminogen activator inhibitor-1 (PAI-1) and d-dimer; iv) angiogenesis/fibrosis: vascular endothelial growth factor A (VEGF-A) and soluble receptors for vascular endothelial growth factor (sVEGF-R1). In these assays, a high proportion of the analyzed samples were below the lower limit of detection (LOD), and the analysis software censored calculated biomarker levels. The measured fluorescence intensity (FI) values are an alternative to alleviate the concern of determining levels of LOD. Because of this, we did the data analysis using the raw FI values, without subtracting blank, as a relative quantification of the analyte abundances26. With this approach, there were no missing values, it was not necessary to specify a LOD, and we can analyze the low FI signals, which added more statistical power to the data analysis26,27. All measured FI (arbitrary units, a.u.) values were normalized using log10 transformation (log10 transformed).
The plasma biomarkers measured by simple ELISA were lipopolysaccharide-binding protein (LBP; (R&D Systems, Minneapolis, USA), sCD14, and fatty acid-binding protein 2 (FABP-2) (Raybiotech, Georgia, USA)). The lipopolysaccharide was evaluated by a Limulus amebocyte lysate chromogenic endpoint ELISA (LPS; Hycult Biotech, Uden, The Netherlands).
Statistical analysis
The statistical analysis was performed with Stata 15.0 (StataCorp, Texas, USA) and Statistical Package for the Social Sciences (SPSS) 22.0 (SPSS INC, Chicago, IL, USA). All p-values were two-tailed, and statistical significance was defined as p < 0.05.
For the descriptive analysis, categorical variables were analyzed by the chi-squared test or Fisher’s exact test, as required, and the Mann-Whitney test was used to analyze continuous data.
In this study, the outcome variables were the severity of liver cirrhosis, evaluated with the CTP score, and the presence of severe cirrhosis with Child-Pugh B (CTP 7–9). For the statistical association analysis, Generalized Linear Models (GLM) with a gamma distribution (log-link) were used to analyze the relationship among plasma biomarkers and the CTP score. Besides, GLM with binomial distribution was used to analyze the differences in plasma biomarkers between study groups. These tests give us: i) the arithmetic mean ratio (AMR) and the odds ratio (OR), and ii) significance levels (p-values), which were corrected for multiple testing using the false discovery rate (FDR) with Benjamini and Hochberg (q-values) procedure to reduce the risk of spurious results. GLM models were also adjusted by clinical and epidemiological co-variables: age, gender, smoker, alcohol intake, intravenous drug user (IVDU), previous IFNα therapy, statins treatment, HCV genotype, and log10 HCV RNA. Each plasma biomarker was included by forced entry (Enter algorithm), and the most significant co-variables were selected by a stepwise algorithm (at each step, co-variables are considered for entry with a p-value <0.20), allowing to avoid the over-fitting of the regression.
The accuracy of the biomarkers to separate the study groups was evaluated by the area under the ROC curve (AUC-ROC). Youden’s index was used to select the best cut-off.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and patients gave their written consent. The Institutional Review Board and the Research Ethic Committee of the Instituto de Salud Carlos III (ISCIII) approved the study.
Results
Patients
The characteristics of the 97 patients with advanced HCV-related cirrhosis (32 HCV-monoinfected patients and 65 HIV/HCV-coinfected patients) are shown in Table 1. HIV/HCV-coinfected patients had the lowest values of age (p-value <0.001) and CTP score (p-value= 0.012), lower percentages of previously treated with IFNα therapy (p-value= 0.037), and Child-Pugh B cirrhosis (CTP 7–9) (p-value= 0.009); while they had the highest percentages of males (p-value= 0.037) and IVDUs (p-value ≤0.001). The percentage of prior history of liver decompensation was similar in both groups (p = 0.375). Among patients with Child-Pugh A cirrhosis (CTP < 7), 11 had LSM < 25 kPa, and five had HVPG < 10 mmHg. All patients with Child-Pugh B cirrhosis (CTP 7–9) had LSM ≥25 kPa and HVPG ≥10 mmHg. No patients were in Child-Pugh C cirrhosis.
Table 1.
Summary of epidemiological and clinical characteristics in HCV-monoinfected patients and HIV/HCV-coinfected patients who had advanced HCV-related cirrhosis.
| All | HCV | HIV/HCV | p-values | |
|---|---|---|---|---|
| No. | 97 | 32 | 65 | |
| Gender (male) (n = 97) | 68 (70.1%) | 18 (56.3%) | 50 (76.9%) | 0.037 |
| Age (years) (n = 97) | 53 (48.8; 56.5) | 59.5 (52.6; 70) | 51.8 (48.7; 53.8) | <0.001 |
| Smoker (n = 96) | ||||
| Never | 19 (19.8%) | 11 (34.4%) | 8 (12.5%) | 0.589 |
| Previously (≥ 6 months) | 25 (26%) | 10 (31.3%) | 15 (23.4%) | 0.988 |
| Nowadays | 52 (54.2%) | 11 (34.4%) | 41 (64.1%) | 0.153 |
| Alcohol intake (n = 97) | ||||
| Never | 49 (50.5%) | 22 (68.8%) | 27 (41.5%) | 0.105 |
| Previously (≥ 6 months) | 40 (41.2%) | 9 (28.1%) | 31 (47.7%) | 0.507 |
| Nowadays | 8 (8.2%) | 1 (3.1%) | 7 (10.8%) | 0.120 |
| IVDU (n = 97) | ||||
| Never | 40 (41.2%) | 27 (84.4%) | 13 (20%) | <0.001 |
| Previously (≥ 6 months) | 57 (58.8%) | 5 (15.6%) | 52 (80%) | 0.009 |
| Current | 0 (0%) | 0 (0%) | 0 (0%) | — |
| Treatments | ||||
| Previous IFNα therapy (n = 97) | 49 (50.5%) | 21 (65.6%) | 28 (43.1%) | 0.037 |
| Statins (n = 97) | 11 (11.3%) | 1 (3.1%) | 10 (15.4%) | 0.073 |
| Antiretroviral therapy (n = 65) | ||||
| NRTI + NNRTI-based | — | — | 7 (10.8%) | |
| NRTI + II-based | — | — | 34 (52.3%) | |
| NRTI + PI-based | — | — | 9 (13.8%) | |
| PI + II + others-based | — | — | 4 (6.2%) | |
| Others | — | — | 11 (16.9%) | |
| HIV markers | ||||
| Prior AIDS (n = 65) | — | — | 23 (35.4%) | |
| Nadir CD4 + T-cells (cells/mm3) (n = 60) | — | — | 129 (70; 243.5) | |
| Nadir CD4 + < 200 cells/mm3 (n = 60) | — | — | 40 (66.7%) | |
| CD4 + T-cells (cells/mm3) (n = 65) | — | — | 444 (234; 719) | |
| CD4 + < 500 cells/mm3 (n = 65) | — | — | 38 (58.5%) | |
| Undetectable HIV-RNA (n = 65) | — | — | 65 (100%) | |
| HCV markers | ||||
| HCV genotype (n = 95) | ||||
| 1 | 65 (68.4%) | 25 (78.1%) | 40 (63.5%) | 0.335 |
| 3 | 14 (14.7%) | 4 (12.5%) | 10 (15.9%) | 0.503 |
| 4 | 16 (16.8%) | 3 (9.4%) | 13 (20.6%) | 0.708 |
| Log10 HCV-RNA (IU/mL) (n = 96) | 6.1 (5.5; 6.5) | 6.1 (5.4; 6.4) | 6.2 (5.6; 6.6) | 0.287 |
| HCV-RNA ≥ 850.000 IU/mL | 60 (62.5%) | 19 (59.4%) | 41 (64.1%) | 0.655 |
| Liver disease (n = 94) | ||||
| LSM (kPa) | 30.6 (24.5; 41.6) | 29.9 (26.3; 48) | 31 (22.3; 39.3) | 0.208 |
| <25 kPa | 24 (25.5%) | 6 (19.4%) | 18 (28.6%) | 0.926 |
| 25–40 kPa | 45 (47.9%) | 14 (45.2%) | 31 (49.2%) | 0.941 |
| ≥40 kPa | 25 (26.6%) | 11 (35.5%) | 14 (22.2%) | 0.774 |
| Child-Pugh Score (n = 91) | 5 (5; 6) | 5 (5; 7) | 5 (5; 5) | 0.012 |
| Child-Pugh B (7–9) | 13 (14.3%) | 8 (28.6%) | 5 (7.9%) | 0.009 |
| Prior history of liver decompensation | 30 (31%) | 8 (22.8%) | 22 (33.8%) | 0.375 |
Statistics: Values expressed as absolute number (percentage) and median (interquartile range). P-values were calculated by Chi-square, Fisher’s exact test, and Mann-Whitney tests, as required. The statistically significant differences are shown in bold.
Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus; IVDU, intravenous drug user; IFNα, interferon-alpha; NRTI, nucleoside analogue HIV reverse; NNRTI, non-nucleoside analogue HIV reverse transcriptase inhibitor; PI, protease inhibitor; II, integrase inhibitor; AIDS, acquired immune deficiency syndrome; HIV-RNA, HIV plasma viral load; HCV-RNA, HCV plasma viral load; LSM, liver stiffness measure; kPa, kilopascal.
HIV/HCV-coinfected patients vs. HCV-monoinfected patients
HIV/HCV-coinfected patients had lower values of sCD14 (p-value= 0.046), IL-1RA (p-value= 0.049) and sRANKL (p-value= 0.019) than HCV-monoinfected patients in adjusted regression analyses. However, all these significant differences disappeared after adjusting by multiple comparisons (see Supplementary Table 1). Therefore, HIV/HCV-coinfected patients on suppressive ART had quite similar values of plasma biomarkers than HCV-monoinfected patients.
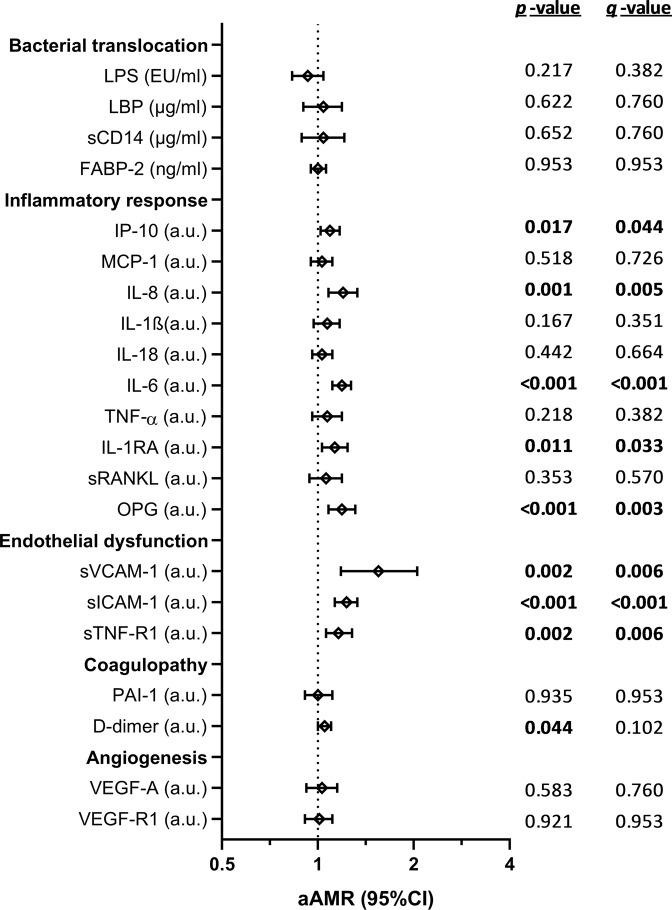
Relationship between plasma biomarkers and CTP score
Figure 1 shows the adjusted association values between plasma biomarkers and CTP score (full description in Supplementary Table 2). For all patients, higher values of plasma biomarkers linked to inflammatory response [IP-10 (q-value= 0.044), IL-8 (q-value= 0.005), IL-6 (q-value <0.001), and OPG (q-value= 0.003)],endothelial dysfunction [sVCAM-1 (q-value= 0.006), sICAM-1 (q-value <0.001), and sTNF-R1 (q-value= 0.006)] were related to higher CTP values. When patients were stratified by HIV infection, HCV-monoinfected patients had association with CTP score for IL-8 (q-value= 0.001), IL-6 (q-value= 0.002), OPG (q-value= 0.001), sVCAM-1 (q-value <0.001), sICAM-1 (q-value <0.001), and sTNF-R1 (q-value= 0.002); while HIV/HCV-coinfected patients only showed significant association with CTP score for IL-6 (q-value= 0.007) and sICAM-1 (q-value= 0.007).
Figure 1.
Association between values of plasma biomarkers (fluorescence intensity, arbitrary units) and Child-Pugh-Turcotte (CTP) score in patients with advanced HCV-related cirrhosis. Statistics: Values were expressed as arithmetic mean ratio (aAMR) and 95% confidence interval (95%CI). P-values were calculated by GLM models unadjusted and adjusted by the main clinical and epidemiological characteristics (see statistical analysis section). P-values, raw p-values; q-values, p-values corrected for multiple testing using the false discovery rate (FDR) with Benjamini and Hochberg procedure. The statistically significant differences are shown in bold. Abbreviations: HCV, hepatitis C virus; -1, human immunodeficiency virus type 1; a.u., arbitrary units of fluorescence; sCD14, soluble CD14; LPS, lipopolysaccharide; FABP2, fatty acid-binding protein 2; LBP, lipopolysaccharide binding protein; IL, interleukin; IL-1RA, interleukin-1 receptor antagonist; TNF-α, tumor necrosis factor alpha; IP-10, IFN-γ-inducible protein 10; MCP1, monocyte chemoattractant protein-1; OPG, osteoprotegerin; sRANKL, soluble receptor activator of nuclear factor- kappaB ligand; sVCAM-1, soluble vascular cell adhesion molecule 1; sICAM-1, soluble intercellular cell adhesion molecule 1; sTNF-R1, soluble tumor necrosis factor receptor 1; PAI-1, plasminogen activator inhibitor-1; VEGF-A; vascular endothelial growth factor A; sVEGF-R1, soluble receptors for vascular endothelial growth factor.
Patients with Child-Pugh B cirrhosis (CTP 7–9) had higher plasma values of IP-10, IL-6, OPG, sVCAM-1, sICAM-1, and D-dimer (p-value <0.05 and q-value <0.1) than patients with Child-Pugh A cirrhosis (CTP < 7) (Table 2). The AUC-ROC values of these biomarkers to separate the study groups (CTP < 7 vs CTP 7–9) were higher than 0.70 and significant for IP-10 (q-value= 0.012), IL-6 (q-value <0.001), OPG (q-value= 0.012), sVCAM-1 (q-value= 0.036), sICAM-1 (q-value= 0.023), and D-dimer (q-value= 0.036) (Table 2). We also selected, by a multivariate logistic regression with stepwise algorithm, IP-10 (p-value= 0.008) and IL-6 (p-value= 0.002) as the most significant biomarkers. The AUC-ROC of IP-10, IL-6, and both biomarkers combined (IP-10+IL-6) were 0.78, 0.88, and 0.96; respectively (Fig. 2). The value of 0.15 of IP-10 and IL-6 combined in a logistic regression model was the best cut-off (Youden’s index = 0.846), which showed a sensitivity and specificity of 92.3%, positive predictive value of 98.6% and negative predictive value of 66.7%.
Table 2.
Summary of plasma biomarkers (fluorescence intensity, arbitrary units) in patients with advanced HCV-related cirrhosis according to CTP score.
| All patients | GLM (binomial) | ROC curve | q-value | ||||
|---|---|---|---|---|---|---|---|
| CTP < 7 | CTP ≥ 7 | p-value | q-value | AUC-ROC (95%CI) | p-value | ||
| Bacterial translocation | |||||||
| LPS (EU/ml) | 1.04 (0.81; 1.51) | 0.92 (0.68; 1.23) | 0.124 | 0.258 | 0.39 (0.23; 0.56) | 0.214 | 0.281 |
| LBP (µg/ml) | 0.97 (0.67; 1.28) | 0.83 (0.69; 1.34) | 0.667 | 0.778 | 0.5 (0.32; 0.68) | 0.991 | 0.991 |
| sCD14 (µg/ml) | 2.23 (1.72; 3.08) | 3.26 (2.19; 3.8) | 0.135 | 0.258 | 0.65 (0.49; 0.82) | 0.075 | 0.169 |
| FABP-2 (ng/ml) | 0.47 (0.23; 0.91) | 0.65 (0.32; 1.25) | 0.787 | 0.870 | 0.56 (0.39; 0.74) | 0.478 | 0.558 |
| Inflammatory response | |||||||
| IP-10 (a.u.) | 1077.7 (724; 1573) | 2218.5 (1340; 2551.5) | 0.005 | 0.035 | 0.78 (0.63; 0.93) | 0.001 | 0.012 |
| MCP-1 (a.u.) | 427 (205.5; 651.5) | 553.5 (294; 714.5) | 0.316 | 0.474 | 0.58 (0.41; 0.74) | 0.373 | 0.461 |
| IL-8 (a.u.) | 100 (64; 147.5) | 154 (81; 220) | 0.054 | 0.142 | 0.65 (0.49; 0.82) | 0.081 | 0.169 |
| IL-1β (a.u.) | 15 (14; 22) | 17.5 (15; 28) | 0.277 | 0.447 | 0.66 (0.5; 0.81) | 0.067 | 0.169 |
| IL-18 (a.u.) | 857.5 (496; 1536) | 1024 (541; 1216) | 0.973 | 0.973 | 0.48 (0.34; 0.62) | 0.829 | 0.871 |
| IL-6 (a.u.) | 68.25 (36; 129) | 265 (167.5; 360) | <0.001 | 0.006 | 0.88 (0.78; 0.98) | <0.001 | <0.001 |
| TNF-α (a.u.) | 10 (7.5; 12) | 11 (9; 14) | 0.493 | 0.610 | 0.63 (0.48; 0.78) | 0.140 | 0.227 |
| IL-1RA (a.u.) | 37.5 (31; 51) | 62 (42; 77) | 0.437 | 0.574 | 0.67 (0.53; 0.82) | 0.049 | 0.147 |
| sRANKL (a.u.) | 25 (20; 35) | 36 (24.5; 58) | 0.048 | 0.142 | 0.64 (0.44; 0.84) | 0.102 | 0.179 |
| OPG (a.u.) | 188 (135.5; 277) | 347.5 (288; 486) | 0.016 | 0.066 | 0.76 (0.63; 0.9) | 0.002 | 0.012 |
| Endothelial dysfunction | |||||||
| sVCAM-1 (a.u.) | 10482 (8946; 11558.5) | 11956.5 (10603; 12554.5) | 0.019 | 0.066 | 0.72 (0.59; 0.86) | 0.010 | 0.036 |
| sICAM-1 (a.u.) | 87.75 (59; 130) | 198 (108.5; 288.5) | 0.002 | 0.023 | 0.77 (0.63; 0.91) | 0.002 | 0.012 |
| TNF-R1 (a.u.) | 28.75 (19; 41) | 38 (31; 57.5) | 0.186 | 0.326 | 0.62 (0.47; 0.78) | 0.156 | 0.234 |
| Coagulopathy | |||||||
| PAI-1 (a.u.) | 1026 (812; 1287) | 955 (815; 1187) | 0.883 | 0.927 | 0.48 (0.3; 0.65) | 0.794 | 0.871 |
| D-dimer (a.u.) | 1632.7 (602; 3825.5) | 5443 (4542.5; 7582) | 0.017 | 0.066 | 0.73 (0.58; 0.87) | 0.009 | 0.036 |
| Angiogenesis/Fibrosis | |||||||
| VEGF-A (a.u.) | 75.5 (55.5; 106) | 88 (72; 95) | 0.437 | 0.574 | 0.61 (0.47; 0.76) | 0.192 | 0.269 |
| VEGF-R1 (a.u.) | 44 (35; 68) | 52 (44.5; 129) | 0.104 | 0.243 | 0.65 (0.47; 0.82) | 0.093 | 0.178 |
Statistics: Values expressed as median (P25th; P75th), area under the ROC curve (AUC-ROC), and 95% of confidence interval (95%CI). P-values were calculated by GLMs adjusted by the main clinical and epidemiological characteristics (see statistical analysis section). P-values, raw p-values; q-values, p-values corrected for multiple testing using the false discovery rate (FDR) with Benjamini and Hochberg procedure. The statistically significant differences are shown in bold.
Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus; a.u., arbitrary units of fluorescence; sCD14, soluble CD14; LPS, lipopolysaccharide; FABP2, fatty acid-binding protein 2; LBP, lipopolysaccharide binding protein; IL, interleukin; IL-1RA, interleukin-1 receptor antagonist; TNF-α, tumor necrosis factor alpha; IP-10, IFN-γ-inducible protein 10; MCP1, monocyte chemoattractant protein-1; OPG, osteoprotegerin; sRANKL, soluble receptor activator of nuclear factor- kappaB ligand; sVCAM-1, soluble vascular cell adhesion molecule 1; sICAM-1, soluble intercellular cell adhesion molecule 1; sTNF-R1, soluble tumor necrosis factor receptor 1; PAI-1, plasminogen activator inhibitor-1; VEGF-A; vascular endothelial growth factor A; sVEGF-R1, soluble receptors for vascular endothelial growth factor.
Figure 2.
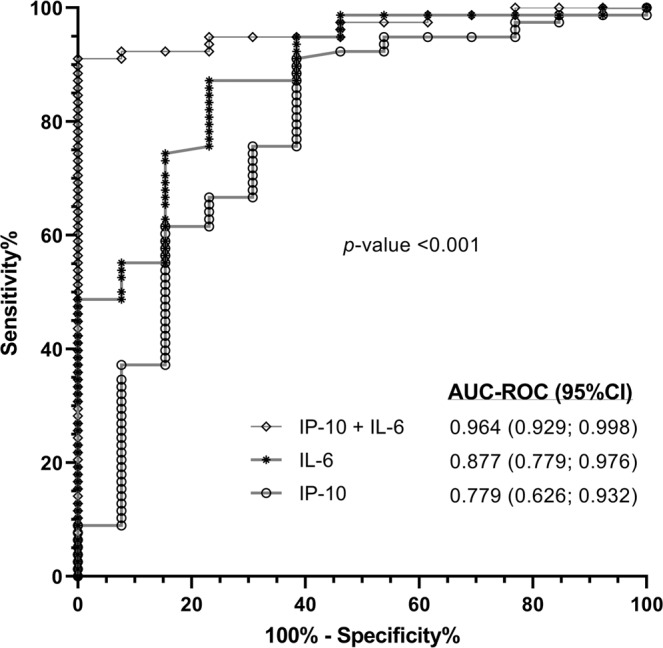
Receiver operating characteristic (ROC) curves of plasma biomarkers for predicting Child-Pugh B cirrhosis (CTP 7–9) in patients with advanced HCV-related cirrhosis. Statistics: Values were expressed as area under the receiver operating characteristic (AUC-ROCs) and 95% confidence interval (95%CI). Abbreviations: IP-10, IFN-γ-inducible protein 10; IL-6, interleukin 6.
Discussion
In this study, we have evaluated the profile of plasma biomarkers (inflammation, endothelial dysfunction, coagulopathy, and angiogenesis) in patients with advanced HCV-related cirrhosis. We found that HIV/HCV-coinfected patients on suppressive ART and HCV-monoinfected patients had near-equivalent values of plasma biomarkers. We also found that higher values of plasma biomarkers (IP-10, IL-8, IL-6, OPG, sVCAM-1, sICAM-1, and D-dimer) were related to higher values of liver disease severity (CTP), but only IP-10 and IL-6 had high accuracy in separating patients with Child-Pugh B cirrhosis (CTP 7–9).
HIV/HCV-coinfected patients usually have a faster progression of chronic hepatitis C28 and higher levels of plasma biomarkers of bacterial translocation, immune activation, inflammation, and coagulation, despite suppressive ART29. In our study, plasma values of biomarkers were very similar in HIV/HCV-coinfected and HCV-monoinfected patients with advanced HCV-related cirrhosis. This may be because our patients had advanced cirrhosis, where elevated immune activation, inflammation, and dysregulation of the innate immune system is usually present5,6. Thus, we could suggest that the weight of cirrhosis was so important that the impact of HIV infection, if any, was eclipsed. Another argument could be that HIV/HCV-coinfected patients were on suppressive ART, with long-term optimal control of HIV replication and significant immune recovery, as shown by the difference between the values of CD4+ T-cells nadir and current count.
Both HIV and HCV infections are characterized by an increased inflammatory response, which raises as the severity of the liver disease progresses4,24,30. Inflammation is also linked to endothelial dysfunction, which is related to the higher severity of liver disease31. Besides, inflammation (inflammatory response and endothelial dysfunction) is associated with increased risk of AIDS progression in HIV-infected patients, the development of comorbidities, chronic hepatitis C progression, and death30,32–34. In our study, we found a significant association between plasma biomarkers linked to inflammation [inflammatory response (IP-10, IL-8, IL-6, and OPG) and endothelial dysfunction (sVCAM-1 and sICAM-1)] and CTP score in all patients with advanced HCV-related cirrhosis so that the highest levels of these biomarkers were found in patients with greater severity of cirrhosis, suggesting a more pronounced inflammatory CAID phenotype, which is in line with previously published data in patients with severe cirrhosis5,6. Moreover, a large number of blood proteins are produced in the liver, and their blood levels may be altered in advanced stages of cirrhosis, leading to increased thrombotic risk7. Coagulopathy is related to increased risk of disease progression and death in people infected with HIV35 and HCV36. In this study, we found a significant association between D-dimer and the CTP score in all patients, but this disappeared when the population was stratified by HIV-infection, possibly because the association was affected by the decreased sample size when the sample was stratified by HIV infection. In any case, there are indications that higher levels of D-dimer are found in patients with a greater stage of cirrhosis. Besides systemic inflammation, the main reason for elevated D-dimer levels in decompensated cirrhosis (more precisely, patients with ascites) is systemic hyperfibrinolysis due to the intraperitoneal activation of the coagulation cascade by tissue factor-bearing extracellular vesicles37.
In our study, HIV infection seems to have had a significant impact on the association between plasma biomarkers and the CTP score. However, the associations had the same sense in the two study groups, although they were weaker in HIV/HCV-coinfected patients, possibly because CTP values had a narrower range in HIV/HCV-coinfected patients than in HCV-monoinfected patients. Thereby, HCV-monoinfected patients showed a significant association of plasma biomarkers of the inflammatory response (IL-8, IL-6, and OPG) and endothelial dysfunction (sVCAM-1, sICAM-1, and sTNF-R1) with CTP score; while HIV/HCV-coinfected patients showed only a significant association of IL-6 and sICAM-1 with CTP score. It is therefore complicated to state that, in our study, HIV infection had a relevant impact on the relationship between biomarkers and the CTP score; nevertheless, it seems clear that the association between inflammation and CTP score remains, independently of HIV infection.
High levels of inflammation is a feature of patients with advanced CAID, particularly in patients with hepatic decompensation5,6. In our study, we found patients who had Child-Pugh B cirrhosis (CTP 7–9) showed higher plasma values of biomarkers linked to the inflammatory response (IP-10, IL-6, and OPG) endothelial dysfunction (sVCAM-1 and sICAM-1) and coagulopathy (D-dimer). These biomarkers were practically the same as those discussed in the previous paragraphs. However, only IP-10 and IL-6 were independently associated with Child-Pugh B cirrhosis (CTP 7–9) with high accuracy. Increased plasma IL-6 and IP-10 levels are related to liver disease severity in HCV-infected patients11,38 and HIV/HCV-coinfected patients24, but in the current study, we found plasma IL-6 and IP-10 levels discriminated with great accuracy the presence of severe cirrhosis with Child-Pugh B (CTP 7–9). The severe cirrhosis seems to be the result of an inflammatory syndrome, which increases the risk of acute-on-chronic liver failure (ACLF)39. Besides, systemic inflammation could also be implicated in the pathogenesis of extrahepatic organ dysfunctions39. However, severe cirrhosis is easy to detect in the clinical setting by physical examination and abdominal ultrasound. This means the use of inflammatory serological markers to identify patients with Child-Pugh B (CTP 7–9) may be of little use in the clinic. Despite this, the AUROC analysis provides helpful information for these two significant inflammatory biomarkers (IL-6 and IP-10), because these two biomarkers also show distinctive elevated levels in Child-Pugh B (CTP 7–9) compared to Child-Pugh A (CTP 5–6), which can aid proper classification.
Limitations of the study
Firstly, this is a cross-sectional study with a low sample size, which may entail a lack of uniformity and could limit the possibility of finding statistical significance in some subgroups. However, despite this, we systematically find inflammation biomarkers associated with the CTP score values, which gives consistency to our results. Furthermore, the potential clinical translation may be limited by the cross-sectional design of our study. A different research design would be necessary to determine if the possible pathogenic factors evaluated in our study are involved in the progression of the liver disease since it cannot be revealed by a cross-sectional approach that does not describe the course of the disease over time. Secondly, all selected patients met a set of criteria for our study, and this may have introduced a selection bias. Longitudinal studies with a higher number of subjects, and with less restrictive criteria, would be necessary to generalize our conclusions to patients with advanced HCV-related cirrhosis and whether the IP-10 and/or IL-6 could predict the patients progressing from CTP A to CTP B.
Conclusions
Plasma biomarker values were quite similar in HIV/HCV-coinfected patients on suppressive ART and HCV-monoinfected patients. Besides, values of plasma biomarkers linked to inflammation (inflammatory response and endothelial dysfunction) were related to the severity of liver cirrhosis (CTP score), mainly IP-10 and IL-6, which discriminated patients with Child-Pugh B concerning Child-Pugh A.
Supplementary information
Acknowledgements
This study would not have been possible without the collaboration of all the patients, medical and nursery staff and data managers who have taken part in the ESCORIAL study: a) Hospital General Universitario Gregorio Marañón (Madrid, Spain): Cristina Díez, Luis Ibáñez, Leire Pérez-Latorre, Diego Rincón, Teresa Aldámiz-Echevarría, Vega Catalina, Pilar Miralles, Francisco Tejerina, María C Gómez-Rico, Esther Alonso, José M Bellón, Rafael Bañares, and Juan Berenguer. b) Hospital Universitario La Paz/IdiPAZ (Madrid, Spain): José Arribas, José I Bernardino, Carmen Busca, Javier García-Samaniego, Víctor Hontañón, Luz Martín-Carbonero, Rafael Micán, María L Montes-Ramírez, Victoria Moreno, Antonio Olveira, Ignacio Pérez-Valero, Eulalia valencia, and Juan González-García. c) Hospital Universitario Puerta de Hierro (Madrid, Spain): Elba Llop and José Luis Calleja. d) Hospital Universitario Ramón y Cajal (Madrid, Spain): Javier Martínez and Agustín Albillos. e) Fundación SEIMC/GeSIDA (Madrid, Spain): Marta de Miguel, María Illescas, and Herminia Esteban. We want to particularly acknowledge the support of the HIV BioBank, which is integrated into the Spanish AIDS Research Network and all collaborating Centres for the generous contribution with clinical samples for the present work. The HIV BioBank, is supported by Instituto de Salud Carlos III, Spanish Health Ministry (Grant n° RD06/0006/0035, RD12/0017/0037 and RD16/0025/0019) as part of the Plan Nacional R + D + I and cofinanced by ISCIII- Subdirección General de Evaluación y el Fondo Europeo de Desarrollo Regional (FEDER)”. The RIS Cohort (CoRIS) is funded by the Instituto de Salud Carlos III through the Red Temática de Investigación Cooperativa en SIDA (RIS C03/173, RD12/0017/0018 and RD16/0002/0006) as part of the Plan Nacional R + D + I and co-financed by ISCIII-Subdirección General de Evaluacion y e Fondo Europeo de Desarrollo Regional (FEDER). This study was supported by grants from Instituto de Salud Carlos III (ISCII; grant numbers PI14/01094 and PI17/00657 to JB, PI14/01581 and PI17/00903 to JGG, CP17CIII/00007 and PI18CIII/00028 to MAJS, and PI14CIII/00011 and PI17CIII/00003 to SR). The study was also funded by the RD16CIII/0002/0002, RD16/0025/0017, and RD16/0025/0018 projects as part of the Plan Nacional R + D + I and co-funded by ISCIII- Subdirección General de Evaluación and the Fondo Europeo de Desarrollo Regional (FEDER). JB is an investigator from the Programa de Intensificación de la Actividad Investigadora en el Sistema Nacional de Salud (I3SNS), Refs INT15/00079 and INT16/00100.
Author contributions
Conceptualization: S.R., J.B., and J.G.G. Data curation: J.B., J.G.G., M.L.M., L.P.L., E.L.H. P.G.B., L.I.S. Formal analysis: S.S., L.M.M., J.M.B., S.R., and M.A.J.S. Funding acquisition: J.B., J.G.G., M.A.J.S, and S.R. Investigation and methodology: S.S., and L.M.M. Project Administration: J.B. Supervision and visualization: S.R. Writing – original draft preparation: M.A.J.S., S.R. Writing – Review & Editing: S.S., J.G.G., J.B.
Data availability
The datasets used and/or analyzed during the current study may be available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Sergio Salgüero and Luz Maria Medrano.
Contributor Information
María Ángeles Jiménez-Sousa, Email: jimenezsousa@isciii.es.
Salvador Resino, Email: sresino@isciii.es.
Supplementary information
is available for this paper at 10.1038/s41598-020-67159-3.
References
- 1.WHO. Global Hepatitis Report. World Health Organization (2017).
- 2.Westbrook RH, Dusheiko G. Natural history of hepatitis C. Journal of hepatology. 2014;61:S58–68. doi: 10.1016/j.jhep.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Naggie S. Hepatitis C Virus, Inflammation, and Cellular Aging: Turning Back Time. Top Antivir Med. 2017;25:3–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Shin EC, Sung PS, Park SH. Immune responses and immunopathology in acute and chronic viral hepatitis. Nat Rev Immunol. 2016;16:509–523. doi: 10.1038/nri.2016.69. [DOI] [PubMed] [Google Scholar]
- 5.Irvine KM, Ratnasekera I, Powell EE, Hume DA. Causes and Consequences of Innate Immune Dysfunction in Cirrhosis. Frontiers in immunology. 2019;10:293. doi: 10.3389/fimmu.2019.00293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albillos A, Lario M, Alvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. Journal of hepatology. 2014;61:1385–1396. doi: 10.1016/j.jhep.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Reimers E, et al. Thrombin activation and liver inflammation in advanced hepatitis C virus infection. World journal of gastroenterology. 2016;22:4427–4437. doi: 10.3748/wjg.v22.i18.4427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koziel MJ, Peters MG. Viral hepatitis in HIV infection. The New England journal of medicine. 2007;356:1445–1454. doi: 10.1056/NEJMra065142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.López-Diéguez M, et al. The natural history of liver cirrhosis in HIV-hepatitis C virus-coinfected patients. AIDS. 2011;25:899–904. doi: 10.1097/QAD.0b013e3283454174. [DOI] [PubMed] [Google Scholar]
- 10.Macias J, et al. Fast fibrosis progression between repeated liver biopsies in patients coinfected with human immunodeficiency virus/hepatitis C virus. Hepatology. 2009;50:1056–1063. doi: 10.1002/hep.23136. [DOI] [PubMed] [Google Scholar]
- 11.Del Campo JA, Gallego P, Grande L. Role of inflammatory response in liver diseases: Therapeutic strategies. World journal of hepatology. 2018;10:1–7. doi: 10.4254/wjh.v10.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hunt PW, Lee SA, Siedner MJ. Immunologic Biomarkers, Morbidity, and Mortality in Treated HIV Infection. The Journal of infectious diseases. 2016;214(Suppl 2):S44–50. doi: 10.1093/infdis/jiw275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt PW. HIV and inflammation: mechanisms and consequences. Curr HIV/AIDS Rep. 2012;9:139–147. doi: 10.1007/s11904-012-0118-8. [DOI] [PubMed] [Google Scholar]
- 14.Schwabl P, et al. Interferon-free regimens improve portal hypertension and histological necroinflammation in HIV/HCV patients with advanced liver disease. Alimentary pharmacology & therapeutics. 2017;45:139–149. doi: 10.1111/apt.13844. [DOI] [PubMed] [Google Scholar]
- 15.Kostadinova L, et al. Soluble Markers of Immune Activation Differentially Normalize and Selectively Associate with Improvement in AST, ALT, Albumin, and Transient Elastography During IFN-Free HCV Therapy. Pathog Immun. 2018;3:149–163. doi: 10.20411/pai.v3i1.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandes, F. F. et al. Effectiveness of direct-acting agents for hepatitis C and liver stiffness changing after sustained virological response. J Gastroenterol Hepatol, 10.1111/jgh.14707 (2019). [DOI] [PubMed]
- 17.Macias J, et al. Similar recovery of liver function after response to all-oral HCV therapy in patients with cirrhosis with and without HIV coinfection. Journal of viral hepatitis. 2019;26:16–24. doi: 10.1111/jvh.12990. [DOI] [PubMed] [Google Scholar]
- 18.Lopez-Cortes LF, et al. Eradication of Hepatitis C Virus (HCV) Reduces Immune Activation, Microbial Translocation, and the HIV DNA Level in HIV/HCV-Coinfected Patients. The Journal of infectious diseases. 2018;218:624–632. doi: 10.1093/infdis/jiy136. [DOI] [PubMed] [Google Scholar]
- 19.Laursen, T. L. et al. Time-dependent improvement of liver inflammation, fibrosis, and metabolic liver function after successful direct-acting antiviral therapy of chronic hepatitis C. Journal of viral hepatitis, 10.1111/jvh.13204 (2019). [DOI] [PubMed]
- 20.Mandorfer M, et al. Changes in Hepatic Venous Pressure Gradient Predict Hepatic Decompensation in Patients Who Achieved Sustained Virologic Response to Interferon-Free Therapy. Hepatology. 2020;71:1023–1036. doi: 10.1002/hep.30885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conti F, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol. 2016;65:727–733. doi: 10.1016/j.jhep.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Forner, A., Reig, M. & Bruix, J. Hepatocellular carcinoma. Lancet, 10.1016/S0140-6736(18)30010-2 (2018). [DOI] [PubMed]
- 23.Sulkowski MS. HCV-HIV coinfected patients: no longer a ‘special’ population? Liver international: official journal of the International Association for the Study of the Liver. 2016;36(Suppl 1):43–46. doi: 10.1111/liv.13021. [DOI] [PubMed] [Google Scholar]
- 24.Medrano LM, et al. Elevated liver stiffness is linked to increased biomarkers of inflammation and immune activation in HIV/hepatitis C virus-coinfected patients. AIDS. 2018;32:1095–1105. doi: 10.1097/QAD.0000000000001787. [DOI] [PubMed] [Google Scholar]
- 25.Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. Journal of hepatology. 2005;42(Suppl):S100–107. doi: 10.1016/j.jhep.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Breen EJ, Tan W, Khan A. The Statistical Value of Raw Fluorescence Signal in Luminex xMAP Based Multiplex Immunoassays. Sci Rep. 2016;6:26996. doi: 10.1038/srep26996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breen EJ, Polaskova V, Khan A. Bead-based multiplex immuno-assays for cytokines, chemokines, growth factors and other analytes: median fluorescence intensities versus their derived absolute concentration values for statistical analysis. Cytokine. 2015;71:188–198. doi: 10.1016/j.cyto.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 28.Lo RV, 3rd, et al. Hepatic decompensation in antiretroviral-treated patients co-infected with HIV and hepatitis C virus compared with hepatitis C virus-monoinfected patients: a cohort study. Annals of internal medicine. 2014;160:369–379. doi: 10.7326/M13-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abutaleb A, Sherman KE. A changing paradigm: management and treatment of the HCV/HIV-co-infected patient. Hepatol Int. 2018;12:500–509. doi: 10.1007/s12072-018-9896-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Younas M, Psomas C, Reynes J, Corbeau P. Immune activation in the course of HIV-1 infection: Causes, phenotypes and persistence under therapy. HIV medicine. 2016;17:89–105. doi: 10.1111/hiv.12310. [DOI] [PubMed] [Google Scholar]
- 31.Akcam FZ, Tigli A, Kaya O, Ciris M, Vural H. Cytokine levels and histopathology in chronic hepatitis B and chronic hepatitis C. J Interferon Cytokine Res. 2012;32:570–574. doi: 10.1089/jir.2012.0048. [DOI] [PubMed] [Google Scholar]
- 32.Lagathu C, et al. Basic science and pathogenesis of ageing with HIV: potential mechanisms and biomarkers. AIDS. 2017;31(Suppl 2):S105–S119. doi: 10.1097/QAD.0000000000001441. [DOI] [PubMed] [Google Scholar]
- 33.Marquez M, Fernandez Gutierrez del Alamo C, Giron-Gonzalez JA. Gut epithelial barrier dysfunction in human immunodeficiency virus-hepatitis C virus coinfected patients: Influence on innate and acquired immunity. World journal of gastroenterology. 2016;22:1433–1448. doi: 10.3748/wjg.v22.i4.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin W, Weinberg EM, Chung RT. Pathogenesis of accelerated fibrosis in HIV/HCV coinfection. The Journal of infectious diseases. 2013;207(Suppl 1):S13–18. doi: 10.1093/infdis/jis926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leeansyah E, Malone DF, Anthony DD, Sandberg JK. Soluble biomarkers of HIV transmission, disease progression and comorbidities. Current opinion in HIV and AIDS. 2013;8:117–124. doi: 10.1097/COH.0b013e32835c7134. [DOI] [PubMed] [Google Scholar]
- 36.Sherman KE. Advanced liver disease: what every hepatitis C virus treater should know. Top Antivir Med. 2011;19:121–125. [PMC free article] [PubMed] [Google Scholar]
- 37.Mandorfer, M. et al. in The Internatinal Liver Congress 2019 Vol. 70 (ed EASL) e625-e853 (Journal of Hepatology, Vienna, 2019).
- 38.Ferrari SM, et al. Immunomodulation of CXCL10 Secretion by Hepatitis C Virus: Could CXCL10 Be a Prognostic Marker of Chronic Hepatitis C? J Immunol Res. 2019;2019:5878960. doi: 10.1155/2019/5878960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bernardi M, Moreau R, Angeli P, Schnabl B, Arroyo V. Mechanisms of decompensation and organ failure in cirrhosis: From peripheral arterial vasodilation to systemic inflammation hypothesis. Journal of hepatology. 2015;63:1272–1284. doi: 10.1016/j.jhep.2015.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study may be available from the corresponding author upon reasonable request.