Abstract
Background
Cytomegalovirus retinitis is an infectious sight-threatening condition that usually occurs in immunosuppressed individuals, but rare cases of Cytomegalovirus retinitis have been reported in immunocompetent patients.
Findings
A 68-year-old woman without any history of systemic diseases referred to the emergency ward of Farabi eye hospital with a two-week history of decreased vision in her left eye. Fundoscopy of the left eye revealed mild venous tortuosity, hemorrhagic retinitis within the macula, and papillitis. The right eye had a history of Cytomegalovirus retinitis 2 years ago that complicated with rhegmatogenous retinal detachment. Immunologic evaluations were normal without any sign of immunosuppressive conditions. She was treated with intravenous ganciclovir for 2 weeks, intravitreal ganciclovir (twice weekly) for 1 week, and also daily oral valganciclovir as maintenance therapy for 6 months resulted in resolving of retinitis patches and improving her best-visual acuity from hand motions to 20/100. Forty-five days after stopping maintenance therapy recurrence occurred. So we started the treatment again to stabilize the patient. She is currently maintained on valganciclovir 900 mg daily without recurrence for 9 months.
Conclusions
Cytomegalovirus retinitis can recur in the same or contralateral eye of immunocompetent patients, especially without prophylactic medication.
Keywords: Cytomegalovirus retinitis, Posterior uveitis, CMV, CMV retinitis in immucocompetent patients, Prevention and control
Introduction
Cytomegalovirus retinitis (CMVR) is a sight-threatening condition usually affecting immunosuppressed individuals but few cases of CMVR have been reported in immunocompetent patients [1]. Herein, we report an immunocompetent patient with unsynchronized bilateral involvement without a previous predisposing factor for acquiring CMVR.
Case presentation
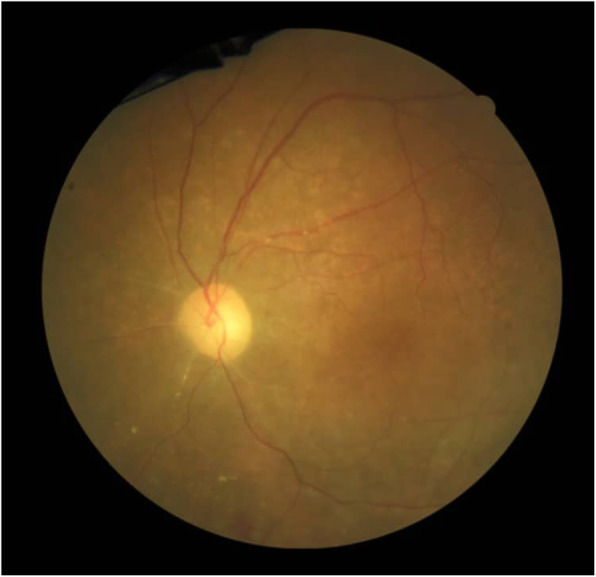
A 68-year-old woman without any history of systemic diseases was referred to the emergency ward of Farabi eye hospital with a two-week history of decreased vision in her left eye. At presentation, her best-corrected visual acuity (BCVA) was hand motions in her left eye and no light perception in the right eye. On the slit-lamp examination, the left eye had fine diffuse keratic precipitates and 1+ anterior chamber cells. Also, fundoscopy revealed mild venous tortuosity, hemorrhagic retinitis within the macula, and papillitis (Fig. 1). The first episode of CMVR has been occurred in the right eye about 2 years ago which complicated with the rhegmatogenous retinal detachment (RRD) after 3 months treatment with valganciclovir and underwent pars planavitrectomy with silicone oil injection. Current fundus examination of the right eye revealed pale optic disc, occluded retinal vessels, and diffuse chorioretinal atrophy (Fig. 2).
Fig. 1.

Fundoscopy of the left eye: mild venous tortuosity, hemorrhagic retinitis within the macula, and papillitis
Fig. 2.
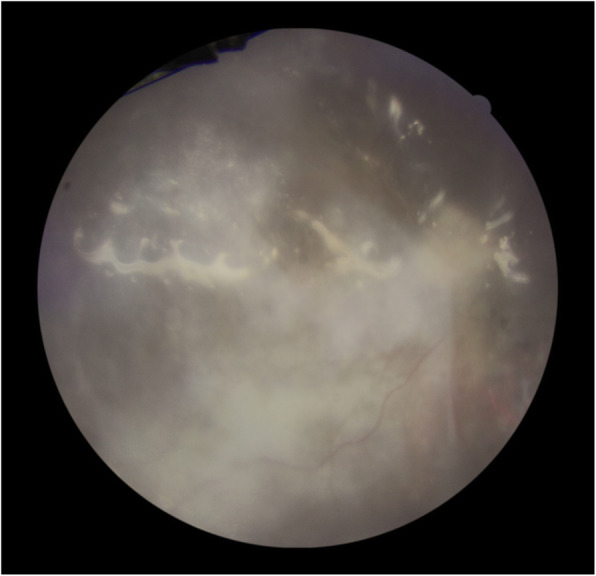
Fundoscopy of the right eye: Silicone oil-filled vitreous, pale optic disk, occluded retinal vessels, and diffuse chorioretinal atrophy
The referring ophthalmologist confirmed the diagnosis of CMVR in the right eye after vitreous sampling and CMV PCR assessment. The patient had close follow up visits and immunologic status including complete blood cell count and lymphocytes count have been checked out frequently without any sign of immunosuppression. Upon initiating symptoms in the left eye, the patient was referred to our center for more assessments.
Due to unusual presentations of patient, infectious and hematologic consultations and vitreous sampling were scheduled. The requested laboratory tests including complete blood count (CBC), Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein, absolute count of lymphocytes, CD3+, CD4+ (609 cells/μl), CD8+, CD16+ and CD56+ lymphocyte count, complement system function, autoimmune antibodies like Anti – Neutrophil Cytoplasmic Antibody (C-ANCA, P-ANCA), Anti-Nuclear Antibody (ANA), and Rheumatoid Factor (RF), Veneral Disease Research Laboratory (VDRL), Fluorescent Treponemal Antibody Absorption (FTA-ABS), liver function tests, creatinine, Fasting Blood Sugar (FBS), Purified Protein Derivative (PPD), Hepatitis B virus antigen (HBs Ag), Hepatitis C virus antibody (HCV Ab), anti-HIV antibody, all were in normal laboratory ranges. DNA PCR of Varicella-zoster Virus (VZV), Herpes Simplex Virus (HSV), and CMV on either whole blood or vitreous samples were negative except positive CMV DNA PCR of the vitreous sample. Also, requested consultations did not reveal any underlying immunodeficiency and malignancy evaluation was negative.
Because of clinical features and previous history of CMVR, treatment has been started against CMV. The devastating course of the disease in the fellow eye and involvement of the posterior pole and optic disk persuasive us for aggressive treatment. So we started the treatment with intravenous ganciclovir 10 mg/kg/day for 2 weeks and 2 mg injections of intravitreal ganciclovir (twice weekly) for 1 week. The treatment followed by 900 mg daily oral valganciclovir as maintenance therapy for 6 months. During the treatment, her visual acuity improved from hand motions to 20/100, and patches of retinitis start to fade from the macula (Fig. 3). Forty-five days after stopping maintenance therapy with valganciclovir retinitis recurred in the left eye and visual acuity dropped to counting fingers at 3 m (Fig. 4), so we started the treatment again to stabilize the patient. She is currently maintained on valganciclovir 900 mg daily without recurrence for 9 months with 20/100 visual acuity.
Fig. 3.
Fundoscopy of the left eye after the treatment
Fig. 4.
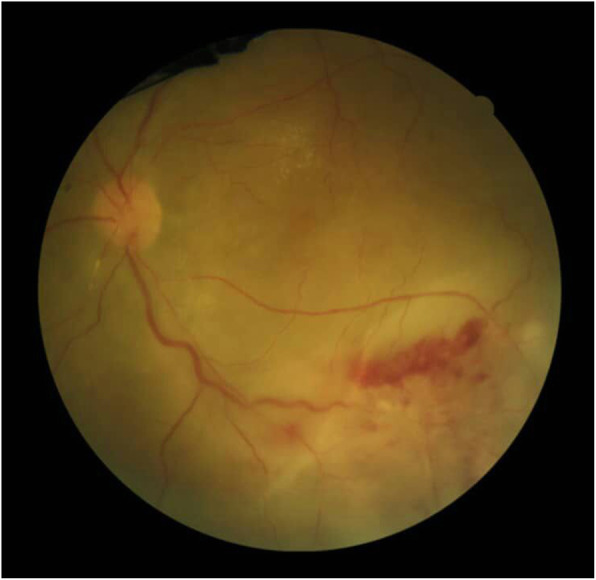
Fundoscopy of the left eye, recurrence after stopping maintenance therapy
Discussion
CMVR accounts as the most common opportunistic viral infection in HIV patients which often manifests in CD4+ counts lower than 50/μl [1]. Also, the other immunosuppressive conditions like leukemia, lymphoma, and organ transplant surgery may prone the patient to this form of posterior uveitis [1]. Few reports of CMVR in immunocompetent patients can be found in the literature. However, the majority of these cases have been suffered from subclinical immunosuppression such as diabetes mellitus (DM) [2–6].
Moreover, the role of intravitreal injections is considerable; there are several reports of developing CMVR after intravitreal injection of corticosteroids such as triamcinolone acetonide (TA) [2, 3, 5]. Also,Witmer et al. [7] reported this condition after the administration of intravitreal dexamethasone implant in an immunocompetent old woman. The interesting point is available reports of CMVR after intravitreal injection of anti-vascular endothelial growth factors (anti-VEGFs) like bevacizumab [4, 6]. Although the immunosuppressive effects of corticosteroids may justify the occurrence of this condition, anti-VEGF drugs have not this property. We speculated the disruption of the blood-retinal barrier and subclinical immunosuppression by diabetic retinopathy is the main predisposing factor for the occurrence of CMVR in these cases and considering a separate role for intravitreal injections is difficult. Similar to our case, the majority of previous studies have reported the CMVR in old aged immunocompetent patients. Thus, we think old ages may be associated with higher rates of CMVR. However, Hosseini et al. [8] reported CMVR in a 4-month-old healthy infant recently. A brief review of some of the recent reports of CMV retinitis in immunocompetent patients and issues including age, laterality of involvement, risk factors, manifestations, treatment, and the visual outcome are summarized in Table 1.
Table 1.
A brief review of some of the recent reports of CMV retinitis in immunocompetent patients. (Abbreviations: Diabetes mellitus (DM), injection of triamcinolone acetonide (IVTA), central retinal vein occlusion (CRVO))
| case (Reference) | Age | Laterality | Systemic and ocular history | Manifestation | Treatment | Initial visual acuity | Final visual acuity |
|---|---|---|---|---|---|---|---|
| 1 [1] | 61 | Right eye | None | Fine keratic precipitates, 1+ aqueous cells, mild vitritis, patches of hemorrhagic retinitis and perivascular sheathing | Intravitreal ganciclovir followed by oral valganciclovir | 4/20 | 8/20 |
| 2 [9] | 51 | Both eyes | None | Fine keratic precipitates, 1+ aqueous cell, and flare, 1+ vitritis in both eyes, areas of confluent retinitis and hemorrhage and peripheral necrosis and fibrosis | Oral valganciclovir |
20/60 (right eye) and 20/50 (left eye) |
20/70 (right eye) and 20/60 (left eye) |
| 3 [5] | 75 | Left eye | Diabetes mellitus (DM), intravitreal injection of triamcinolone acetonide (IVTA) | The rare cell in the anterior chamber, no vitreous cells, arcuate retinal whitening (which appeared full-thickness) along the temporal vascular arcades | Intravitreal ganciclovir followed by oral valganciclovir | 20/80 | 20/400 |
| 4 [2] | 77 | Right eye | DM, IVTA | Fine keratic precipitates, 2 + vitritis, foci of oedematous retinitis with dense retinal whitening, hemorrhages and inflammatory retinal vascular sheathing |
Intravitreal injection of ganciclovir + intravenous administration of ganciclovir followed by oral valganciclovir |
counting fingers at 1.8 m | 20/200 |
| 5 [2] | 69 | Right eye | DM, central retinal vein occlusion (CRVO), Vitrectomy surgery, IVTA | Keratic precipitates, 2 + cells in the anterior chamber, moderate vitritis, necrotizing retinitis extending throughout the entire retina with hemorrhages, retinal opacification and periphlebitis |
Intravitreal injection of ganciclovir + intravenous administration of ganciclovir followed by oral valganciclovir |
20/200 | 20/400 |
| 6 [3] | 54 | Left eye | Carrier of human T-cell lymphotropic virus type 1, DM, CRVO, vitrectomy surgery, IVTA | Small granulomatous keratic precipitates, 1+ aqueous cell and flare, 1+ vitritis, papillitis, retinal vasculitis, and retinal exudates |
Intravenous injections of ganciclovir + Intravitreous injections of foscarnet |
1.0 | 0.5 |
| 7 [10] | 78 | Right eye | IVTA | Keratic precipitates, 2+ cells in the anterior chamber and moderate vitritis, hemorrhagic sheathing of branch arteries, inflammatory vascular sheathings in the periphery and areas of retinal whitening in the peripheral superior nasal part | Intravitreous injections of ganciclovir + intravenous ganciclovir followed by oral valganciclovir | 20/40 | 20/25 |
| 8 [4] | 61 | Left eye | DM, intravitreal injection of bevacizumab | 4+ cells and in the anterior chamber, dense vitritis and retinal vascular obliteration, necrotizing retinitis with dense retinal whitening and hemorrhage | Intravenous administration of ganciclovir | Hand motions | Not reported |
| 9 [6] | 75 | Left eye | DM, intravitreal injection of ranibizumab | Mild anterior segment inflammation, low-grade vitritis, and foci of retinitis in the peripheral fundus along with retinal and subretinal hemorrhages, exudates, and macular edema | Intravitreal ganciclovir | 4/10 | 5/10 |
| 10 [11] | 74 | Right eye | Multiple intraocular surgeries, long-term use of immunosuppressive eye drops such as corticosteroids and cyclosporine | No inflammatory cells in the anterior chamber or the anterior vitreous, confluent exudate the entire peripheral retina | Intravenous ganciclovir+ intravitreal ganciclovir injections followed by oral valganciclovir | Hand motions | Not reported |
To the best of the author’s knowledge and database searches like PubMed, few cases of CMVR have been reported in patients without any type of systemic immunosuppression. The physiopathology of developing CMVR in completely immunocompetent patients is not clear. We hypothesized maybe genetic susceptibility acts as a predisposing factor in these cases, similar to the patients with AIDS [12].
CMVR should be differentiated from acute retinal necrosis (ARN), progressive outer retinal necrosis (PORN), toxoplasmosis, and syphilis [13]. History of this form of posterior uveitis, clinical characteristics, and also positive PCR sampling were differentiating points in this case. It is noticeable up to 24% of CMVR cases may lead to RRD as happened in the right eye of the current case we reported [1].
Unsynchronized bilateral involvement is a remarkable aspect of this case. Another unique aspect of this case is recurrence after stopping valganciclovir that debates a challenging question about the duration of prophylaxis in patients without immunosuppression. The answer to this question is not clear and none of the previous reports discussed this issue. Previously, CMVR in an HIV patient indicated life-long anti-CMV therapy. However, development of new treatment options made discontinuation of maintenance therapy safe in these patients due to quantitative immune recovery in low counts of CD4+ lymphocytes as the predisposing factor. According to CDC guidelines maintenance therapy or secondary prophylaxis in AIDS-related CMV retinitis should be continued until reaching to adequate immune recovery which defines as sustained raise of CD4+ cell counts to above 100 cells/μl for at least 3–6 months with inactive CMVR characterized by retinal scarring. These guidelines also mentioned that valganciclovir primary prophylaxis against CMVR is not neccessary once CMVR treatment is successfully completed unless CD4+ count has decreased to < 100 cells/μL [14]. It seems in patients without clear predisposing factor discontinuing of the treatment is not rational and routine ophthalmic monitoring appears useful.
Conclusion
This report targets bringing issues to light that CMVR can recur in the same or contralateral eye of immunocompetent patients, especially without prophylactic medication.
Acknowledgments
None.
Abbreviations
- CMVR
cytomegalovirus retinitis
- CMV
cytomegalovirus
- RRD
rhegmatogenous retinal detachment
- AIDS
acquired immunodeficiency syndrome
- VEGF
vascular endothelial growth factor
- CD
a cluster of differentiation
- PCR
polymerase chain reaction
- DM
diabetes mellitus
- IVTA
injection of triamcinolone acetonide
- CRVO
central retinal vein occlusion
Authors’ contributions
BBS reviewed the patient at first presentation, performed treatment and post-operative care and also collated and prepared the patient data. KC wrote the manuscript. SAT and EK revised the manuscript. All authors read and approved final manuscript.
Funding
Not applicable.
Availability of data and materials
The data in the current case report are available from the Farabi Eye Hospital medical records. The data is available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent was taken from the individual for publication of personal data.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Seyed Ali Tabatabaei, Email: alitabatabaei77@yahoo.com.
Kasra Cheraqpour, Email: cheraqpourk@gmail.com.
Elias Khalili Pour, Email: ekhalilipour@gmail.com.
Bahram Bohrani Sefidan, Email: bohranibahram@yahoo.com.
References
- 1.Karkhaneh R, Lashay A, Ahmadraji A. Cytomegalovirus retinitis in an immunocompetent patient: a case report. J Current Ophthalmol. 2016;28(2):93–95. doi: 10.1016/j.joco.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delyfer MN, Rougier MB, Hubschman JP, Aouizérate F, Korobelnik JF. Cytomegalovirus retinitis following intravitreal injection of triamcinolone: report of two cases. Acta Ophthalmol Scand. 2007;85(6):681–683. doi: 10.1111/j.1600-0420.2007.00915.x. [DOI] [PubMed] [Google Scholar]
- 3.Furukawa M, Kumagai K, Ogino N, Okinami S, Uemura A, Larson E. Cytomegalovirus retinitis after intravitreous triamcinolone treatment of a vitrectomized eye in an immunocompetent patient. Retinal Cases Brief Reports. 2007;1(4):205–207. doi: 10.1097/ICB.0b013e31804d1e3f. [DOI] [PubMed] [Google Scholar]
- 4.Bae SH, Kim TW, Chung H, Heo JW. Cytomegalovirus retinitis after intravitreal bevacizumab injection in an immunocompetent patient. Korean J Ophthalmol. 2013;27(1):61–63. doi: 10.3341/kjo.2013.27.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saidel MA, Berreen J, Margolis TP. Cytomegalovirus retinitis after intravitreous triamcinolone in an immunocompetent patient. Am J Ophthalmol. 2005;140(6):1141–1143. doi: 10.1016/j.ajo.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 6.Zafeiropoulos P, Tamboura P, Dimou M, Christodoulou E, Stefaniotou M. Cytomegalovirus retinitis, in a diabetic immunocompetent patient, after intravitreal ranibizumab injection. Eur J Ophthalmol. 2019;29(1):NP10–NNP2. doi: 10.1177/1120672118772525. [DOI] [PubMed] [Google Scholar]
- 7.Witmer MT, Connolly BP. Cytomegalovirus retinitis after an intravitreal dexamethasone implant in an immunocompetent patient. Retinal Cases Brief Reports. 2019. [DOI] [PubMed]
- 8.Hosseini SM, Moosavi M-N, Shoeibi N, Sakhaee M, Ghavamsaeedi H. Bilateral cytomegalovirus retinitis in a healthy infant. J Current Ophthalmol. 2017;29(1):66–68. doi: 10.1016/j.joco.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart MW, Bolling JP, Mendez JC. Cytomegalovirus retinitis in an immunocompetent patient. Arch Ophthalmol. 2005;123(4):572–574. doi: 10.1001/archopht.123.4.572. [DOI] [PubMed] [Google Scholar]
- 10.Vertes D, Snyers B, De Potter P. Cytomegalovirus retinitis after low-dose intravitreous triamcinolone acetonide in an immunocompetent patient: a warning for the widespread use of intravitreous corticosteroids. Int Ophthalmol. 2010;30(5):595–597. doi: 10.1007/s10792-010-9404-x. [DOI] [PubMed] [Google Scholar]
- 11.Toriyama K, Suzuki T, Hara Y, Ohashi Y. Cytomegalovirus retinitis after multiple ocular surgeries in an immunocompetent patient. Case Reports Ophthalmol. 2012;3(3):356–359. doi: 10.1159/000343705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sezgin E, Jabs DA, Hendrickson SL, Van Natta M, Zdanov A, Lewis RA, et al. Effect of host genetics on the development of cytomegalovirus retinitis in patients with AIDS. J Infect Dis. 2010;202(4):606–613. doi: 10.1086/654814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeung IY, Downes KM, Cunningham E, Sen HN. CMV retinitis: reduced incidence, still a threat. Review of Ophthalmology May 10th Issue. 2016
- 14.Benson CA, Brooks JT, Holmes KK, Kaplan JE, Masur H, Pau A. Guidelines for prevention and treatment opportunistic infections in HIV-infected adults and adolescents; recommendations from CDC, the National Institutes of Health, and the HIV medicine association/Infectious Diseases Society of America. 2009. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data in the current case report are available from the Farabi Eye Hospital medical records. The data is available from the corresponding author on reasonable request.


