Abstract
Background
In this study, our aim was to compare the effects of tourniquet and tranexamic acid (TXA) use on tibial cement penetration in primary total knee arthroplasty (TKA) using radiograph images. In addition, we also aimed at investigating the effects of age, gender, body mass index (BMI), and bone mineral density on cement penetration.
Methods
One hundred seventy patients who underwent TKA for primary osteoarthritis were retrospectively evaluated. TXA was administered to patients in group 1 (n = 96), and tourniquet application was used in patients in group 2 (n = 74). Tibial cement penetration was evaluated radiologically on a total of 4 zones: 2 anteroposterior and 2 lateral zones. In addition, age, gender, BMI, and bone mineral density were recorded in each group.
Results
The mean cement penetration in the total study population was 2.34 ± 0.24 mm, with a mean of 2.33 ± 0.25 mm in the TXA group and a mean of 2.35 ± 0.24 mm in the tourniquet group (P = .453). A negative correlation was detected between BMI and anteroposterior 1 values in the total and TXA groups (P = .022 and P = .029). In the evaluation of the differences between genders, significantly higher penetration values were observed only in the females in the tourniquet group (P = .024).
Conclusions
The use of TXA instead of a tourniquet does not reduce the depth of cement penetration in TKA. The clinical implications of individual-induced penetration differences may be significant for future implant survival.
Keywords: Cement penetration, Total knee arthroplasty, Tourniquet, Tranexamic acid
Introduction
Although total knee arthroplasties (TKAs) are widely and successfully used in osteoarthritis, aseptic loosening of the tibial component is still one of the most important issues [[1], [2], [3]]. Aseptic loosening may be caused by individual differences, the surgical technique, or the type of implants used [2,4]. The strength of the cement-bone interface is extremely important in the survival of the TKA and the need for revision [[5], [6], [7], [8]].
Cement must be able to penetrate the cancellous bone under the tibial component in sufficient amounts and homogeneously [2,7,9]. Penetration is related with the type of cement used, the cementation technique, and the cleanliness of the bone surface [[10], [11], [12]]. The reduction of perioperative hemorrhage results in a clean bone surface, thus a better penetration of the cement in the cancellous bone [3,13], whereas blood mixed with cement affects the penetration negatively [12,14].
In our day, intensive effort is put to reduce bleeding with minimum side effects in TKA surgery. Although the widely used tourniquet application reduces the perioperative hemorrhage, it causes increased postoperative and total blood loss, venous thromboembolic problems, and bad functional knee scores in the early period [15,16]. On the other hand, antifibrinolytic agents such as tranexamic acid (TXA), which are becoming more widely used, reduce blood loss and avoid tourniquet-induced morbidities [17]. Yet, there are occasions in which combined use of TXA and tourniquet is still preferred.
In this study, we aimed at comparing the effects of tourniquet and TXA use in primary TKA on the cement penetration in the tibial bone on radiograph images. In addition, we aimed to investigate the effects of age, gender, body mass index (BMI), and bone mineral density (BMD) on cement penetration.
Material and methods
Approval for the study was obtained from the local ethics committee of our institution. Two hundred thirty patients who underwent TKA for primary osteoarthritis in our clinic between 2014 and 2017 were retrospectively evaluated. Bilateral cases, revision cases, and knees with excessive deformities were excluded from the study. In the remaining 170 cases, we used TXA on group 1 patients (n = 96) and tourniquet on group 2 patients (n = 74). The mean age of the patients was 65.8 ± 8.4 years. Both groups were similar in terms of patient characteristics (Table 1).
Table 1.
Comparison of the demographic data between the groups.
| TXA (n = 96) |
Tourniquet (n = 74) |
Total |
P | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Gender | |||||||
| Male | 20 | (20.83) | 15 | (20.27) | 35 | (20.59) | .928b |
| Female | 76 | (79.17) | 59 | (79.73) | 135 | (79.41) | |
| Side | |||||||
| Right | 55 | (57.29) | 40 | (54.05) | 95 | (55.88) | .673b |
| Left | 41 | (42.71) | 34 | (45.95) | 75 | (44.12) | |
| Agea | 66.12 ± 8.78 | 66.00 | 65.34 ± 7.94 | 66.00 | 65.78 ± 8.41 | 66.00 | .547c |
| BMIa | 32.72 ± 5.73 | 32.00 | 32.83 ± 5.80 | 32.22 | 32.77 ± 5.75 | 32.05 | .863d |
| BMD g/cm2a | 1.006 ± 0.196 | 0.982 | 1.004 ± 0.186 | 1.002 | 1.005 ± 0.188 | 0.994 | .978c |
BMD, bone mineral density; BMI, body mass index; TXA, tranexamic acid.
Instead of n, mean ± SD, and instead of %, median values are given.
Chi-square test.
Student’s t-test.
Mann-Whitney U test.
Surgical procedure and patient care
The choice of performing general or regional anesthesia was jointly made by the patient and the anesthesiologist. The patients were operated on by the same surgical team using the same brand knee prosthesis (NexGen LPS-Flex Knee; Zimmer Biomet, Warsaw, IN). All surgical procedures were performed at 18°C and 55% humidity.
In the tourniquet group, a 10.5-cm-wide tourniquet was padded and inflated up to 150 mmHg over the systolic pressure with simple elevation and was not deflated during the whole surgery. In all cases, a medial parapatellar approach and measured resection technique was used. An extramedullary incision guide was used for the tibia and an intramedullary guide for the femur. An autologous bone was used to fill the femoral medullary canal before implant cementation. A lavage system was used for cleaning the bone surfaces.
In all cases, the same cement (Hi-Fatigue; Zimmer Biomet, Warsaw, IN) was stirred manually, without using a vacuum mixer, in the mixing bowl for approximately 4 minutes, and it was considered ready for use when it did not stick to the glove. First, the cement was applied to the lower surface of the tibial component outside the stem (meaning the stem was not applied cement) and was then adapted to the bone surface. After the placement of the insert, the femoral component was covered with cement and adapted to the bone surface. No additional cement was applied to the bone surfaces. The knee was kept in extension for 10 minutes to ensure the hardening of the cement. The excess cement overbrimming the components was removed using a curette.
Closure was routinely performed with the knee positioned in flexion. Electrocautery and routine hemostasis were performed in all cases during surgery. No tourniquet application was performed in the TXA group. The patients were given 15 mg/kg TXA 15 minutes before and 2 hours after the surgery intravenously with 100 mL of saline.
All patients were given prophylactic antibiotherapy and analgesia for 2 days after surgery, and a single dose of antithrombotic enoxaparin 4,000 IU was administered subcutaneously 12 hours after surgery.
Age, gender, operated side, BMI, and BMD of the patients were recorded in both groups. A Horizon WI S/N 200475 device (Hologic, Inc., Bedford, MA) was used for BMD measurements of the lumbar region.
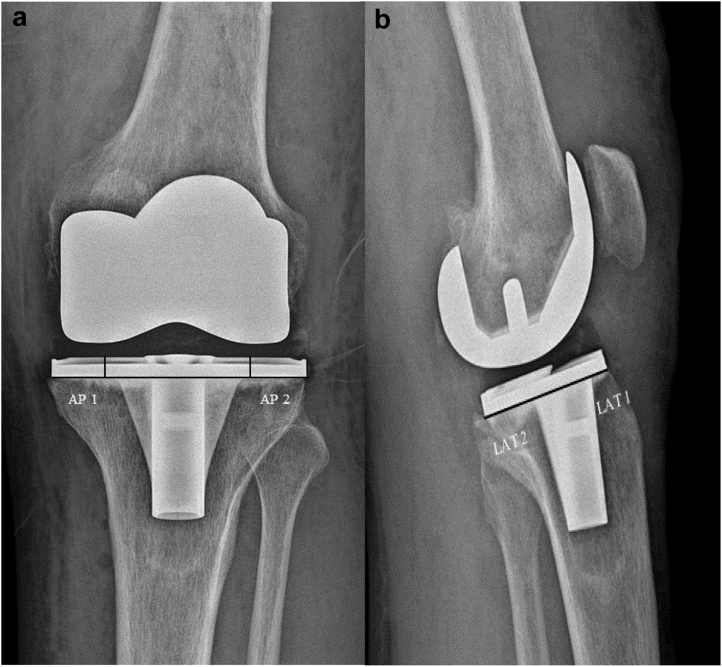
Cement penetration measurements were made using the hospital’s Picture Archiving and Communication System (Sectra AB, Linköping, Sweden). Based on the Knee Society Scoring system, the tibia was divided into zones on the anteroposterior (AP) and lateral (L) radiographs taken on the second postoperative day [18]. Because the keels of the tibial component posed challenges, we used only the medial (AP 1) and L zones (AP 2) on the AP plane and the anterior (LAT 1) and posterior zones (LAT 2) on the L plane (Fig. 1) for the measurements. For intraobserver and interobserver reliability, cement penetration measurements were repeated twice a week apart by an orthopaedic surgeon.
Figure 1.
(a-b) Measurement zones on postoperative (a) AP and (b) lateral radiograph images.
Statistical analyses were performed using the SPSS v.17.0 software. Histograms and the Kolmogorov-Smirnov test were used in evaluating the normal distribution of the variables. The mean, standard deviation, and median values were used to present descriptive analyses. The data were compared using Pearson’s chi-square and Fisher’s exact tests. The Student t test was used in intergroup evaluation of the variables that showed normal distribution (that were parametric), whereas the Mann-Whitney U test was used for evaluating the groups that did not show normal distribution (nonparametric groups). Spearman’s correlation test was used in the analysis of measurable data with each other. P values of less than .05 were considered statistically significant.
Results
The mean cement penetration was 2.33 ± 0.25 mm in the TXA group and 2.35 ± 0.24 mm in the tourniquet group (P = .453) (Table 2).
Table 2.
Comparison of the penetration values between the groups.
| AP 1 (mm) | AP 2 (mm) | LAT 1 (mm) | LAT 2 (mm) | Total (mm) | Mean (mm) | |
|---|---|---|---|---|---|---|
| TXA | 2.27 ± 0.44 | 2.45 ± 0.45 | 2.12 ± 0.33 | 2.41 ± 0.37 | 9.26 ± 1.01 | 2.33 ± 0.25 |
| Tourniquet | 2.32 ± 0.29 | 2.50 ± 0.37 | 2.17 ± 0.25 | 2.50 ± 0.24 | 9.49 ± 0.94 | 2.35 ± 0.24 |
| Total | 2.30 ± 0.37 | 2.47 ± 0.41 | 2.15 ± 0.29 | 2.46 ± 0.31 | 9.38 ± 0.97 | 2.34 ± 0.24 |
| P | 0.655a | 0.665b | 0.639a | 0.491b | 0.453b | 0.453b |
LAT, lateral zone.
Student t test.
Mann-Whitney U test.
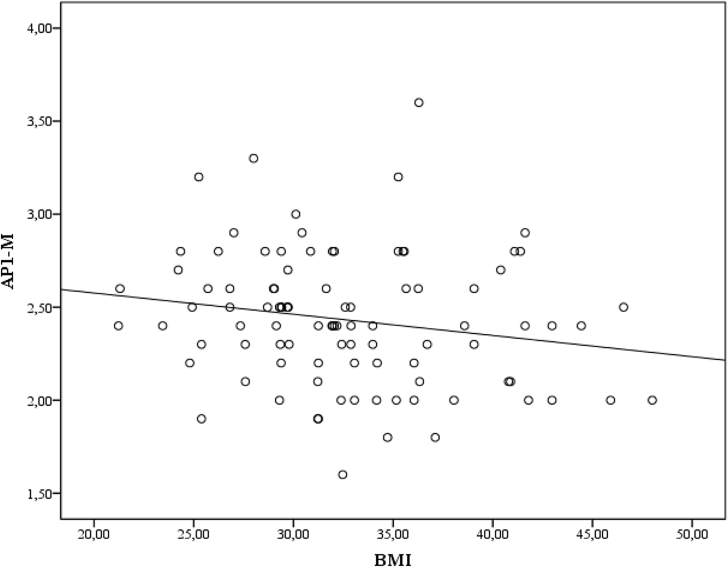
In the total case group, when the correlation between age, BMI, BMD, and cement penetration was examined, only AP 1 measurement results showed a negative correlation with BMI (P = .022) (Table 3). A similar evaluation of correlation in the TXA and tourniquet groups revealed a negative correlation only between AP 1 measurement and the BMI in the TXA group (P = .029) (Fig. 2).
Table 3.
Spearman’s correlation between the BMI and BMD and penetration values in the total study population.
| AP 1 | AP 2 | LAT 1 | LAT 2 | Mean | |
|---|---|---|---|---|---|
| Age | |||||
| r | 0.016 | −0.254 | −0.277 | −0.301 | −0.288 |
| P | .920 | .104 | .076 | .053 | .065 |
| BMI | |||||
| r | −0.352 | 0.199 | −0.107 | 0.045 | −0.034 |
| P | .022 | .207 | .501 | .777 | .830 |
| BMD | |||||
| r | −0.074 | −0.055 | −0.178 | −0.130 | −0.108 |
| P | .641 | .731 | .258 | .412 | .495 |
LAT, lateral zone.
Significant P values are written in bold.
Figure 2.
The correlation between the BMI and AP 1 zone measurement results in the TXA group (r = −0.352, P = .022).
The BMD value was significantly lower in females in the total and tourniquet groups (P = .002 and P = .007, respectively) (Table 4). In evaluation of the differences between genders, significantly higher penetration values were observed only in the females in the tourniquet group (P = .024) (Table 5, Table 6).
Table 4.
Comparison of the BMI, BMD, and penetration values in all patients based on gender.
| Male |
Female |
P | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age | 67.43 ± 7.30 | 65.83 ± 7.09 | .673b |
| BMI | 32.68 ± 7.45 | 35.96 ± 4.53 | .088b |
| BMD | 1.218 ± 0.15 | 0.962 ± 0.17 | .002b |
| AP 1 | 2.30 ± 0.22 | 2.30 ± 0.40 | .986a |
| AP 2 | 2.33 ± 0.34 | 2.50 ± 0.42 | .309b |
| LAT 1 | 2.04 ± 0.24 | 2.17 ± 0.30 | .313a |
| LAT 2 | 2.40 ± 0.23 | 2.47 ± 0.32 | .454b |
| Total | 9.07 ± 0.89 | 9.44 ± 0.99 | .344b |
| Mean | 2.27 ± 0.22 | 2.36 ± 0.25 | .344b |
LAT, lateral zone; SD, standard deviation.
Significant P values are written in bold.
Student t test.
Mann-Whitney U test.
Table 5.
Gender-based comparison of the BMI, BMD, and penetration values in the TXA group.
| Male |
Female |
P | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age | 67.00 ± 7.44 | 66.71 ± 7.89 | .857b |
| BMI | 32.73 ± 6.83 | 36.67 ± 4.58 | .097b |
| BMD | 1.138 ± 0.13 | 0.975 ± 0.20 | .073b |
| AP 1 | 2.29 ± 0.32 | 2.45 ± 0.06 | .076a |
| AP 2 | 2.48 ± 0.41 | 2.58 ± 0.17 | .752b |
| LAT 1 | 2.15 ± 0.24 | 2.17 ± 0.26 | .886a |
| LAT 2 | 2.50 ± 0.24 | 2.51 ± 0.24 | .928b |
| Total | 9.45 ± 1.02 | 9.67 ± 0.61 | .517b |
| Mean | 2.36 ± 0.25 | 2.39 ± 0.15 | .517b |
LAT, lateral zone; SD, standard deviation.
Student t test.
Mann-Whitney U test.
Table 6.
Gender-based comparison of the BMI, BMD, and penetration values in the tourniquet group.
| Male |
Female |
P | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age | 68.00 ± 8.72 | 65.00 ± 6.37 | .801b |
| BMI | 32.61 ± 9.84 | 35.29 ± 4.52 | .481b |
| BMD | 1.324 ± 0.13 | 0.951 ± 0.13 | .007b |
| AP 1 | 2.10 ± 0.17 | 2.30 ± 0.47 | .484a |
| AP 2 | 2.00 ± 0.10 | 2.53 ± 0.44 | .020b |
| LAT 1 | 1.90 ± 0.17 | 2.16 ± 0.34 | .217a |
| LAT 2 | 2.27 ± 0.15 | 2.44 ± 0.39 | .204b |
| Total | 8.27 ± 0.38 | 9.43 ± 0.99 | .024b |
| Mean | 2.07 ± 0.09 | 2.36 ± 0.25 | .024b |
LAT, lateral zone; SD, standard deviation.
Significant P values are written in bold.
Student t test.
Mann-Whitney U test.
The correlation coefficient for intraobserver reliability was 0.99 (95% CI: 0.98-0.99) and 0.99 (95% CI: 0.98-0.99) for each observer, respectively. The correlation of interobserver reliability was 0.98 (95% CI: 0.98-0.99).
Discussion
The most important finding of our study was that the use of TXA in primary TKA in the absence of tourniquet application did not negatively affect the cement penetration. To our knowledge, both the effect of TXA on cement penetration and the correlation between tibial cement penetration and age, gender, BMI, and BMD have not been investigated previously.
The popularity of TXA as an alternative method has been increasing over tourniquet application in TKA, which is widely preferred because of reduced perioperative hemorrhage but also associated with postoperative morbidity [19,20]. Pfitzner et al. [3] stated that the use of tourniquet increased the thickness of the cement mantle in the cumulative measurements; however, surgeons should not ignore postoperative bleeding and pain.
On the other hand, there is a close relationship between the implant stability and depth of cement penetration [21,22]. For the cement to reach the first transverse trabeculae, 2- to 3-mm penetration is required [6]. Previously, Hofmann et al. [23] reported 2.7 mm of cement penetration on average, whereas Ozkunt et al. [24] found an average of 2.35-mm penetration and that the presence of tourniquet had no effect on cement penetration. In the study by Touzopoulos et al. [25], the average penetration measurements at all levels remained below 2 mm, whereas the penetration in the tourniquet group was found to be 1.2 mm more cumulatively. When comparing the tourniquet and TXA groups in our study, we could not find any difference between the mean and cumulative values, and our average penetration values were 2-3 mm in accordance with the literature.
The depth of the cement penetration is influenced by many factors. Low temperature and high humidity prolong the curing time for cement [26]. In our study, the surgical technique, implant and the type of cement used, the cementing technique, and room conditions were the same in both groups. The use of a tourniquet or TXA as a variable could affect penetration through having an impact on perioperative bleeding; however, this did not happen. In addition, it is known that the porosity of the cancellous bone at the level of tibial incision affects the penetration. Tibial bone porosity is affected by alignment, BMD, and BMI [[26], [27], [28]].
We used lumbar BMD values in our study. In their study, Yoon et al. [29] showed a positive correlation between lumbar BMD and L and medial tibial condyle BMD values. The authors noted higher BMD values in the medial condyles of the knees of gonarthrosis patients with varus alignment. In addition, they detected a positive correlation between the BMI and BMD value of the knee.
The penetration decreases because of increased bone density in the medial plateau in varus knees and in the L plateau in valgus knees [26]. There is a negative correlation between local BMD and cement penetration [28,30]. We believe that the negative correlation between the BMI and the medial tibial condyle penetration in the total case group was due to the effect of both the BMI and medial alignment on penetration. In addition, we believe that the lower BMD values in females in the tourniquet group are associated with increased cement penetration.
Our study had some limitations. First, it had a nonrandomized design, which introduces the possibility of selection bias. Second, instead of using quantitative computed tomography, the BMD measurements were performed with dual energy X-ray absorptiometry (DEXA) because of low cost and low radiation. In addition, although our cases had similar varus alignment, the alignment between the groups was not evaluated. Because aseptic loosening is often related to the tibia and radiologic evaluation of the femoral component is technically complicated, only the thickness of the cement under the tibial component was evaluated. The effect of TXA only on the mantle thickness of cement was investigated; its effect on the tibial component survival in the long term may be the focus of another study.
Our study showed that similar cement penetration values were obtained in the tourniquet and TXA groups. In addition, we demonstrated that preoperative alignment, BMI, and BMD had effects on penetration.
In conclusion, the use of TXA instead of a tourniquet does not reduce the depth of the cement penetration in TKA. The clinical implications of individual-induced penetration differences may be significant for future implant survival.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
Authors' contributions: Y.M.D., B.G., M.U.C., A.H.D., and R.V. contributed to conceptualization of the study; Y.M.D., A.S., B.G., and E.A. contributed to data analysis; statistical analysis was carried out by Y.M.D.; the study was performed under the supervision of A.S. and Y.M.D. All authors read, reviewed, and approved the final manuscript.
Availability of data and material: The data set used to support the findings of this study is available from the corresponding author on request.
Appendix A. Supplementary data
References
- 1.Gu S., Kuriyama S., Nakamura S., Nishitani K., Ito H., Matsuda S. Underhang of the tibial component increases tibial bone resorption after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1270. doi: 10.1007/s00167-018-5309-4. [DOI] [PubMed] [Google Scholar]
- 2.Westerman R.W. Can tibial cementation be enhanced in knee arthroplasty surgery? J Knee Surg. 2016;29(5):391. doi: 10.1055/s-0035-1564595. [DOI] [PubMed] [Google Scholar]
- 3.Pfitzner T., von Roth P., Voerkelius N. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):96. doi: 10.1007/s00167-014-3341-6. [DOI] [PubMed] [Google Scholar]
- 4.Ritter M.A., Keating E.M., Sueyoshi T. Twenty-five-years and greater, results after nonmodular cemented total knee arthroplasty. J Arthroplasty. 2016;31(10):2199. doi: 10.1016/j.arth.2016.01.043. [DOI] [PubMed] [Google Scholar]
- 5.Insall J., Scott W.N., Ranawat C.S. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61(2):173. [PubMed] [Google Scholar]
- 6.Lutz M.J., Pincus P.F., Whitehouse S.L., Halliday B.R. The effect of cement gun and cement syringe use on the tibial cement mantle in total knee arthroplasty. J Arthroplasty. 2009;24(3):461. doi: 10.1016/j.arth.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Peters C.L., Craig M.A., Mohr R.A., Bachus K.N. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res. 2003;409:158. doi: 10.1097/01.blo.0000058638.94987.20. [DOI] [PubMed] [Google Scholar]
- 8.van Loon C.J., de Waal Malefijt M.C., Buma P., Verdonschot N., Veth R.P. Femoral bone loss in total knee arthroplasty. A review. Acta Orthop Belg. 1999;65(2):154. [PubMed] [Google Scholar]
- 9.Bert J.M., McShane M. Is it necessary to cement the tibial stem in cemented total knee arthroplasty? Clin Orthop Relat Res. 1998;356:73. doi: 10.1097/00003086-199811000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Ritter M.A., Herbst S.A., Keating E.M., Faris P.M. Radiolucency at the bone-cement interface in total knee replacement. The effects of bone-surface preparation and cement technique. J Bone Joint Surg Am. 1994;76(1):60. doi: 10.2106/00004623-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Banwart J.C., McQueen D.A., Friis E.A., Graber C.D. Negative pressure intrusion cementing technique for total knee arthroplasty. J Arthroplasty. 2000;15(3):360. doi: 10.1016/s0883-5403(00)90762-9. [DOI] [PubMed] [Google Scholar]
- 12.Breusch S., Heisel C., Müller J., Borchers T., Mau H. Influence of cement viscosity on cement interdigitation and venous fat content under in vivo conditions: a bilateral study of 13 sheep. Acta Orthop Scand. 2002;73(4):409. doi: 10.1080/00016470216320. [DOI] [PubMed] [Google Scholar]
- 13.Juliusson R., Flivik G., Nilsson J., Ryd L., Onnerfält R. Circulating blood diminishes cement penetration into cancellous bone. In vivo studies of 21 arthrotic femoral heads. Acta Orthop Scand. 1995;66(3):234. doi: 10.3109/17453679508995531. [DOI] [PubMed] [Google Scholar]
- 14.Majkowski R.S., Bannister G.C., Miles A.W. The effect of bleeding on the cement-bone interface. An experimental study. Clin Orthop Relat Res. 1994;299:293. [PubMed] [Google Scholar]
- 15.Sapega A.A., Heppenstall R.B., Chance B., Park Y.S., Sokolow D. Optimizing tourniquet application and release times in extremity surgery: a biochemical and ultrastructural study. J Bone Joint Surg Am. 1985;67(2):303. [PubMed] [Google Scholar]
- 16.Worland R.L., Arredondo J., Angles F., Lopez-Jimenez F., Jessup D.E. Thigh pain following tourniquet application in simultaneous bilateral total knee replacement arthroplasty. J Arthroplasty. 1997;12(8):848. doi: 10.1016/s0883-5403(97)90153-4. [DOI] [PubMed] [Google Scholar]
- 17.Xie J., Ma J., Yao H., Yue C., Pei F. Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplasty. 2016;31(11):2458. doi: 10.1016/j.arth.2016.04.034. [DOI] [PubMed] [Google Scholar]
- 18.Ewald F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9. [PubMed] [Google Scholar]
- 19.Zhang W., Li N., Chen S. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014;9(1):13. doi: 10.1186/1749-799X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Z., Ma J., Shen B., Pei F. Combination of intravenous and topical application of tranexamic acid in primary total knee arthroplasty: a prospective randomized controlled trial. J Arthroplasty. 2014;29(12):2342. doi: 10.1016/j.arth.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 21.Scott C.E., Biant L.C. The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br. 2012;94(8):1009. doi: 10.1302/0301-620X.94B8.28289. [DOI] [PubMed] [Google Scholar]
- 22.Walker P.S., Soudry M., Ewald F.C., McVickar H. Control of cement penetration in total knee arthroplasty. Clin Orthop Relat Res. 1984;185:155. [PubMed] [Google Scholar]
- 23.Hofmann A.A., Goldberg T.D., Tanner A.M., Cook T.M. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty. 2006;21(3):353. doi: 10.1016/j.arth.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Ozkunt O., Sariyilmaz K., Gemalmaz H.C., Dikici F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Medicine (Baltimore) 2018;97(4):e9668. doi: 10.1097/MD.0000000000009668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Touzopoulos P., Ververidis A., Mpogiatzis C., Chatzigiannakis A., Drosos G.I. The use of tourniquet may influence the cement mantle thickness under the tibial implant during total knee arthroplasty. Eur J Orthop Surg Traumatol. 2019;29(4):869. doi: 10.1007/s00590-019-02369-8. [DOI] [PubMed] [Google Scholar]
- 26.Cawley D.T., Kelly N., McGarry J.P., Shannon F.J. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J. 2013;95-B(3):295. doi: 10.1302/0301-620X.95B3.29586. [DOI] [PubMed] [Google Scholar]
- 27.Reina N., Cavaignac E., Pailhé R. BMI-related microstructural changes in the tibial subchondral trabecular bone of patients with knee osteoarthritis. J Orthop Res. 2017;35(8):1653. doi: 10.1002/jor.23459. [DOI] [PubMed] [Google Scholar]
- 28.Schlegel U.J., Bishop N.E., Püschel K., Morlock M.M., Nagel K. Comparison of different cement application techniques for tibial component fixation in TKA. Int Orthop. 2015;39(1):47. doi: 10.1007/s00264-014-2468-x. [DOI] [PubMed] [Google Scholar]
- 29.Yoon C., Chang M.J., Chang C.B. Bone mineral density around the knee joint: correlation with central bone mineral density and associated factors. J Clin Densitom. 2018;23(1):82. doi: 10.1016/j.jocd.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Raiss P., Pape G., Kleinschmidt K. Bone cement penetration pattern and primary stability testing in keeled and pegged glenoid components. J Shoulder Elbow Surg. 2011;20(5):723. doi: 10.1016/j.jse.2010.09.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.