1. INTRODUCTION
Oxygen is one of the most basic medical therapies we have for acute respiratory illnesses and it has been an established part of medical practice for over 100 years. However, most patients who may benefit from oxygen in low‐ and middle‐income countries will not receive it—either because oxygen is not available or because their need for oxygen is unrecognized. This gap takes an enormous toll, with modeling estimates suggesting that improved pulse oximetry and oxygen access could avert 148 000 under‐five child pneumonia deaths annually in the 15 countries with the highest pneumonia burden 1 . This commentary explores the reasons for this gap, using Nigeria as an illustrative case study in how oxygen access can be improved globally, and concluding with key actions for policy and practice.
2. CHILD MORTALITY AND HYPOXEMIA IN NIGERIA
Nigeria is a large lower middle‐income country that ranks second in the number of child pneumonia deaths globally, contributing one‐sixth of under‐five pneumonia deaths globally. 1 , 2 Pneumonia causes 18% of under‐five deaths in Nigeria, followed by malaria (14%), complications of prematurity (12%), neonatal encephalopathy and trauma (11%), and diarrheal diseases (10%). 2 Nigerian studies suggest that hypoxemia affects approximately 14% of children admitted to hospital, including 28% to 49% of children with pneumonia and 22% to 41% of neonates. 3 , 4 , 5 , 6 Hypoxemia ranks alongside severe acute malnutrition as a major predictor of mortality, with recent data from 12 Nigerian hospitals showing that children with hypoxemia had seven‐fold higher risk of death than those who did not. 3
Despite the high burden of hypoxemia and increasing recognition of its position as a key sign of illness severity, pulse oximetry, and oxygen therapy have been inadequately used in most Nigerian hospitals. Facility evaluations of Nigerian hospitals have shown that oxygen supply is often not available on pediatric wards, pulse oximeters are uncommonly used outside operating theaters, and healthcare workers lack training on how to use oxygen and pulse oximeters. 7 , 8
These findings in Nigeria are echoed globally. Hypoxemia is common and deadly, 9 , 10 yet access to oxygen and pulse oximeters remains limited and healthcare worker skills and confidence using oxygen is low 11 , 12 , 13 , 14 —especially in health centers and smaller hospitals where most sick children first present.
3. KEY BARRIERS TO IMPROVING OXYGEN ACCESS AND USE
At the hospital level, there are three key barriers to improving oxygen access and use.
3.1. First, oxygen‐related equipment, if available, is often low quality, faulty, and poorly maintained
A recent study in 12 south‐west Nigerian hospitals found that 92% (11/12) of hospitals had some access to oxygen supplies, 42% (5/12) had oxygen available on pediatric wards at the time of evaluation, and 8% (1/12) used pulse oximetry for pediatric care. 7 Testing of 57 oxygen concentrators revealed that 5% (3/57) were producing medical‐grade oxygen (defined as >85% purity), and 48% (24/50) of those that turned on and blew gas were simply blowing out air. 7 Data from hospitals in northern Nigeria showed that the situation was even worse in these poorer, more rural, locations—11% of hospital pediatric wards had functional oxygen, 2% had pulse oximeters. 8 In both regions, procurement of oxygen equipment was haphazard, motivated by price and availability of donated items, with little regard to quality or appropriateness. Hospitals lacked preventive maintenance programs and many technicians reported that they were not aware of the procurement of oxygen equipment until it was brought to them broken for repair. 7
3.2. Second, clinical guidance, training, and support to use oxygen is limited and poorly implemented
Oxygen therapy is unlike most other medications, being administered using equipment and titrated by nurses based on serial clinical assessments (including pulse oximetry). Clinical use of oxygen is not complicated, but healthcare workers do require some basic knowledge and skills. In Nigeria, most nurses receive little training on oxygen, and no training on pulse oximetry, either in nursing school or in‐service training—unless they work in anesthetics/theater. 7 As such, pulse oximetry is rarely used on pediatric wards, and oxygen (when it is available) is used at excessive flow rates and primarily for those with very obvious respiratory distress; many hypoxemic patients will not receive oxygen. 7 , 8
3.3. Third, oxygen‐related care is expensive to hospitals and patients
Maintaining supply of medical oxygen is expensive, and is made costlier by faulty equipment (eg, leaky cylinders and piping), and poor clinical practices (eg, without pulse oximetry to guide therapy). In Nigeria, oxygen‐related patient fees are substantial, typically around ₦3,900 per day 7 (USD$21, 2015). These costs fall most heavily on those who are sickest and require longer hospitalization and may result in treatment refusal or discharge against medical advice.
3.4. These hospital‐level barriers exist in a social and political context
In Nigeria (and many other countries), health financing deficiencies result in patients facing substantial out‐of‐pocket costs in accessing hospital care. The decentralized hospital system in Nigeria gives individual hospitals more autonomy and responsibility for procuring and maintaining medical equipment. However, without technical support or a strong regulatory framework, hospitals often end up with a haphazard array of cheap equipment that they are unable to maintain or repair—exacerbated further by poorly considered equipment donation programs.
4. PROGRESS AND FUTURE OPPORTUNITIES
4.1. Progress
Nigerian clinicians, hospital administrators, and policymakers have made substantial progress towards improving oxygen access and use. At the national policy level, the Federal Ministry of Health has revised the essential medicines and equipment lists to include oxygen and oxygen‐related products, updated the pneumonia clinical guidelines, created a new clinical guideline and hospital policy on oxygen, 15 and developed a national strategy for scaling up oxygen nationally. 16 This strategy includes the nomination of personnel in the Federal and State Ministries of Health who will be responsible for addressing oxygen access issues in their jurisdiction.
Demonstration projects in Nigeria, have shown that the barriers to improving oxygen services can be overcome using existing commercially available equipment, local maintenance teams, and team‐based approaches to learning and quality improvement. Results from these projects have demonstrated improved pulse oximetry use on pediatric wards (from <20% to >75%), improved oxygen provision to hypoxaemic children (from <20% to >85%), and reduced mortality from child pneumonia. 17 , 18
Global policies have also shifted to better support oxygen systems strengthening. In 2013, WHO/UNICEF added oxygen to the Global Action Plan for Pneumonia and Diarrhea, correcting an omission from the first edition. 19 , 20 This establishes oxygen therapy as a core treatment in the Protect, Prevent, Treat framework (Figure 1). In the past 4 years, the WHO has revised the Model List of Essential Medicines for Children to include oxygen for the treatment of hypoxemia in children, 21 published technical specifications for concentrators 22 and other oxygen therapy devices, 23 and released a new oxygen clinical guidelines for children 24 —all of which have been used and adapted by Nigeria and other countries.
Figure 1.
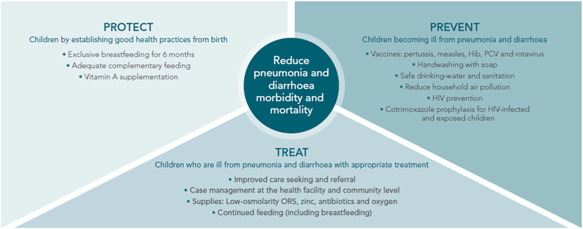
WHO/UNICEF's Protect Prevent Treat framework for reducing mortality from childhood diarrhea and pneumonia, from the Global Action Plan for Pneumonia and Diarrhea (2013) 19 [Color figure can be viewed at wileyonlinelibrary.com]
4.2. Future opportunities
Oxygen therapy is an essential medical therapy for hospital care and should be recognized as a cost‐effective investment for improving health care quality and health outcomes. We identify the following key opportunities for improving oxygen therapy for children globally.
First, existing evidence shows that improving oxygen systems is a cost‐effective intervention that improves the quality of health services and health outcomes. Just as healthcare workers understand the value of oxygen as a basic medical therapy, policy‐makers should now be able to recognize that oxygen is a sound financial investment that will make health services better overall. Better oxygen systems should not only improve access to oxygen therapy but also strengthen broader hospital quality of care systems and stimulate the adoption of other essential health technologies as well.
Second, we know enough to enact national‐scale implementation of improved oxygen systems. Experiences from Nigeria, Ethiopia, Papua New Guinea, and elsewhere, have identified contextual challenges and solutions to improving oxygen systems. These solutions will not be situated within vertically structured programming, but by accepting oxygen therapy as a basic hospital service within a universal health coverage agenda. Policymakers and program managers can be guided by policy documents and technical specifications from WHO and UNICEF 22 , 23 , 24 and Every Breath Counts and United for Oxygen consortiums. However, national oxygen strategies must adopt this guidance to local contexts, defining specific responsibilities for those involved in pharmaceutical, medical device, and financing services.
Third, pulse oximetry is a low‐cost, relatively easily implemented, component of oxygen systems. Essential to the identification of hypoxemia, pulse oximetry is also embraced by healthcare workers as a valuable tool in assessing and monitoring sick patients that improves the quality of care more generally. As such, pulse oximetry scale‐up represents “low‐hanging fruit” for improving hospital care, and may also play an important role in facilitating referral from primary care. 14 , 25
Fourth, existing oxygen technologies are suboptimal in hot, humid, dusty conditions, or environments that lack strong maintenance structures. We need better technology to provide reliable oxygen in places where power failures are common, produce and store oxygen locally, and efficiently deliver oxygen from the oxygen source to patients.
Fifth, previous studies have demonstrated the mortality impact of pulse oximetry and improved oxygen systems for young children with pneumonia, but little data exist for other children or neonates (in whom oxygen is also used commonly). The neonatal cohort represents a particular group of interest, as they can suffer adverse effects from administration of excessive oxygen (eg, retinopathy of prematurity, bronchopulmonary dysplasia). 26 , 27
5. CONCLUSIONS
Oxygen therapy is an essential medical therapy that is poorly available and suboptimally used in many low‐ and middle‐income countries. Recent policy and programmatic experience in Nigeria has shown how oxygen services can be improved for the benefit of children and health services.
AUTHOR CONTRIBUTIONS
HG drafted the manuscript. AAB, CF, OQ, TD, and AGF provided substantial comments to the writing of the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENT
Hamish Graham, Ayobami A. Bakare, Chizoba Fashanu, Owens Wiwa, Trevor Duke, and Adegoke G. Falade received payment for services related to this paper from the Bill and Melinda Gates Foundation (OPP1123577 and OPP1133417).
REFERENCES
- 1. Floyd J, Wu L, Hay Burgess D, Izadnegahdar R, Mukanga D, Ghani AC. Evaluating the impact of pulse oximetry on childhood pneumonia mortality in resource‐poor settings. Nature. 2015;528(7580):S53‐S59. [DOI] [PubMed] [Google Scholar]
- 2. WHO and Maternal and Child Epidemiology Estimation Group (MCEE) . UNICEF data: monitoring the situation of children and women: cause of death. 2015; http://data.unicef.org. Accessed April 4, 2017
- 3. Graham H, Bakare AA, Ayede AI, et al. Hypoxaemia in hospitalised children and neonates: a prospective cohort study in Nigerian secondary‐level hospitals. EClinicalMedicine. 2019;16:51‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Orimadegun AE, Ogunbosi BO, Carson SS. Prevalence and predictors of hypoxaemia in respiratory and non‐respiratory primary diagnoses among emergently ill children at a tertiary hospital in south western Nigeria. Trans R Soc Trop Med Hyg. 2013;107(11):699‐705. [DOI] [PubMed] [Google Scholar]
- 5. Abdulkadir MB, Ibraheem RM, Gobir AA, Johnson WB. Hypoxaemia as a measure of disease severity in young hospitalised Nigerian children with pneumonia: a cross‐sectional study. SAJCH South African J Child Health. 2015;9(2):53‐56. [Google Scholar]
- 6. Adebola O, Babatunde O, Bose O. Hypoxemia predicts death from severe falciparum malaria among children under 5 years of age in Nigeria: the need for pulse oximetry in case management. Afr Health Sci. 2014;14(2):397‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bakare AA, Graham H, Ayede AI, et al. Providing oxygen to children and newborns: a multi‐faceted technical and clinical assessment of oxygen access and oxygen use in secondary‐level hospitals in southwest Nigeria. Int Health. 2019;12(1):60‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CHAI . CHAI Nigeria Final Narrative . Abuja, Nigeria: Clinton Health Access Initiative (CHAI); 2016. [Google Scholar]
- 9. Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T. The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect Dis. 2009;9:219‐227. [DOI] [PubMed] [Google Scholar]
- 10. Lazzerini M, Sonego M, Pellegrin MC. Hypoxaemia as a mortality risk factor in acute lower respiratory infections in children in low and middle‐income countries: systematic review and meta‐analysis. PLOS One. 2015;10(9):e0136166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Graham H, Tosif S, Gray A, et al. Providing oxygen to children in hospitals: a realist review. Bull World Health Organ. 2017;95(4):288‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ginsburg AS, Gerth‐Guyette E, Mollis B, Gardner M, Chham S. Oxygen and pulse oximetry in childhood pneumonia: surveys of clinicians and student clinicians in Cambodia. Trop Med Int Health. 2014;19(5):537‐544. [DOI] [PubMed] [Google Scholar]
- 13. Ginsburg AS, Van cleve, WC , Thompson MIW, English M. Oxygen and pulse oximetry in childhood pneumonia: A survey of healthcare providers in resource‐limited settings. J Trop Pediatr. 2012;58:389‐393. [DOI] [PubMed] [Google Scholar]
- 14. King C, Graham H, McCollum E. Point‐of‐care pulse oximetry for children in low‐resource settings In: Atkinson K, Mabey D, eds. Revolutionizing Tropical Medicine. Hoboken, NJ: John Wiley and Sons Inc; 2019. [Google Scholar]
- 15. Nigeria FMoH . National Policy on Medical Oxygen in Health Facilities . Abuja, Nigeria: Federal Ministry of Health Nigeria; 2017. [Google Scholar]
- 16. Nigeria FMoH . National Strategy for the Scale‐up of Medical Oxygen in Health Facilities 2017‐2022. Abuja, Nigeria: Federal Ministry of Health Nigeria; 2017. [Google Scholar]
- 17. Graham HR, Bakare AA, Ayede AI, et al. Oxygen systems to improve clinical care and outcomes for children and neonates: a stepped‐wedge cluster‐randomised trial in Nigeria. PLOS Med. 2019;16(11):e1002951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fashanu C, Mekonnen T, Omale J, et al. A program evaluation of improved oxygen systems at hospitals in three Nigerian states. Pediatr Pulmonol, 2020. [DOI] [PubMed] [Google Scholar]
- 19. WHO/UNICEF . Ending Preventable Child Deaths from Pneumonia and Diarrhoea by 2025: The integrated Global Action Plan for Pneumonia and Diarrhoea (GAPPD). Geneva, Switzerland: World Health Organization (WHO); 2013. [Google Scholar]
- 20. WHO/UNICEF . Global Action Plan for Prevention and Control of Pneumonia (GAPP). Geneva, Switzerland: World Health Organization (WHO) The United Nations Children's Fund (UNICEF); 2009. [Google Scholar]
- 21. WHO . WHO Model List of Essential Medicines for Children: 6th List. Geneva, Switzerland: World Health Organization (WHO); 2017. [Google Scholar]
- 22. WHO . Technical specifications for oxygen concentrators WHO Medical Device Technical Series. Geneva, Switzerland: World Health Organization (WHO); 2015. [Google Scholar]
- 23. WHO, UNICEF . WHO‐UNICEF technical specifications and guidance for oxygen therapy devices. Geneva, Switzerland: World Health Organization (WHO); 2019. [Google Scholar]
- 24. WHO . Oxygen therapy for children. Geneva, Switzerland: World Health Organization (WHO); 2016. [Google Scholar]
- 25. McCollum E, King C, Colbourn T, et al. Pulse oximetry in paediatric primary care: catalyzing implementation in low‐income and middle‐income countries. Lancet Resp. 2019;7:1001‐1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gilbert C, Malik ANJ, Nahar N, et al. Epidemiology of ROP update ‐ Africa is the new frontier. Semin Perinatol. 2019;43:317‐322. [DOI] [PubMed] [Google Scholar]
- 27. Walker PJB, Bakare AA, Ayede AI, et al. Using intermittent pulse oximetry to guide neonatal oxygen therapy in a low‐resource context. Arch Dis Childhood – Fetal & Neonatal Edition. 2019;0:F1‐F6. [DOI] [PMC free article] [PubMed] [Google Scholar]


