Summary
Background
A transition from a subtyping to a phenotyping approach in rosacea is underway, allowing individual patient management according to presenting features instead of categorization by predefined subtypes. The ROSacea COnsensus (ROSCO) 2017 recommendations further support this transition and align with guidance from other working groups.
Objectives
To update and extend previous global ROSCO recommendations in line with the latest research and continue supporting uptake of the phenotype approach in rosacea through clinical tool development.
Methods
Nineteen dermatologists and two ophthalmologists used a modified Delphi approach to reach consensus on statements pertaining to critical aspects of rosacea diagnosis, classification and management. Voting was electronic and blinded.
Results
Delphi statements on which the panel achieved consensus of ≥ 75% voting ‘Agree’ or ‘Strongly agree’ are presented. The panel recommends discussing disease burden with patients during consultations, using four questions to assist conversations. The primary treatment objective should be achievement of complete clearance, owing to previously established clinical benefits for patients. Cutaneous and ocular features are defined. Treatments have been reassessed in line with recent evidence and the prior treatment algorithm updated. Combination therapy is recommended to benefit patients with multiple features. Ongoing monitoring and dialogue should take place between physician and patients, covering defined factors to maximize outcomes. A prototype clinical tool (Rosacea Tracker) and patient case studies have been developed from consensus statements.
Conclusions
The current survey updates previous recommendations as a basis for local guideline development and provides clinical tools to facilitate a phenotype approach in practice and improve rosacea patient management.
What's already known about this topic?
A transition to a phenotype approach in rosacea is underway and is being recommended by multiple working groups.
New research has become available since the previous ROSCO consensus, necessitating an update and extension of recommendations.
What does this study add?
We offer updated global recommendations for clinical practice that account for recent research, to continue supporting the transition to a phenotype approach in rosacea.
We present prototype clinical tools to facilitate use of the phenotype approach in practice and improve management of patients with rosacea.
Short abstract
Linked Comment: Elewski. Br J Dermatol 2020; 182:1090–1091.
Plain language summary available online
Rosacea is an inflammatory dermatosis predominantly affecting the facial skin and eyes. A system for rosacea diagnosis and subtype‐based classification was first proposed by the National Rosacea Society (NRS) in 2002,1 which has formed the foundation for subsequent research and publications on the subject.2, 3, 4, 5, 6, 7, 8, 9, 10, 11 However, scientific progress has superseded the subtype approach and revealed its limitations, which have been previously discussed,12, 13, 14, 15 leading to the need for a more patient‐focused approach in accord with the latest research and clinical experience.12
The global ROSacea COnsensus (ROSCO) project comprises an international expert panel with dermatologists and ophthalmologists from Africa, Asia, Europe, North America and South America. The 2017 ROSCO consensus recommended transitioning from a subtype to a phenotype approach for rosacea diagnosis, classification and management,12, 13 which aligns with those of the NRS and American Acne and Rosacea Society (AARS).15, 16 A phenotype approach allows for rosacea diagnosis and management according to a patient's presenting disease features, rather than grouping into prespecified subtypes, thus individualizing care and optimizing treatment outcomes.13, 14, 16, 17, 18 It acknowledges the limitations of subtyping, while enabling progression within the field by managing each patient as an individual,13 and is being increasingly incorporated into evidence‐based systematic reviews, national treatment recommendations and discussion in the literature.18, 19, 20, 21 However, a formalized transition is still in its infancy and support is required to promote its widespread uptake.14
Here, we report the results of the ROSCO 2019 project, which update previous recommendations in line with the latest research, further them inclusive of multiple patient types and continue supporting adoption of the phenotype approach through clinical tool development.
Materials and methods
Expert panel
The 2019 expert panel consisted of 19 dermatologists, representing Argentina (n = 1), Brazil (n = 1), Canada (n = 1), France (n = 1), Germany (n = 2), India (n = 1), Italy (n = 1), the Netherlands (n = 1), Qatar (n = 1), Singapore (n = 1), South Africa (n = 1), the U.K. (n = 1) and the U.S.A. (n = 6); and two ophthalmologists, one from Germany and one from the U.S.A. Two chairpersons from the main panel oversaw the process and were involved in panel selection and the Delphi design. Panel members were selected for their contribution to the rosacea field, and their global expertise with a range of skin phototypes, treatment modalities and ocular rosacea.
The modified Delphi approach
The modified Delphi process used by the ROSCO panel has been described previously.13 Between August and November 2018, six e‐surveys were used to gather information and capture voting responses, with a group virtual meeting held to allow discussion of contentious points. A literature review of 140 unique references was conducted to inform the e‐survey content (Appendix S2; see Supporting Information). The process is outlined in Figure 1.
Figure 1.
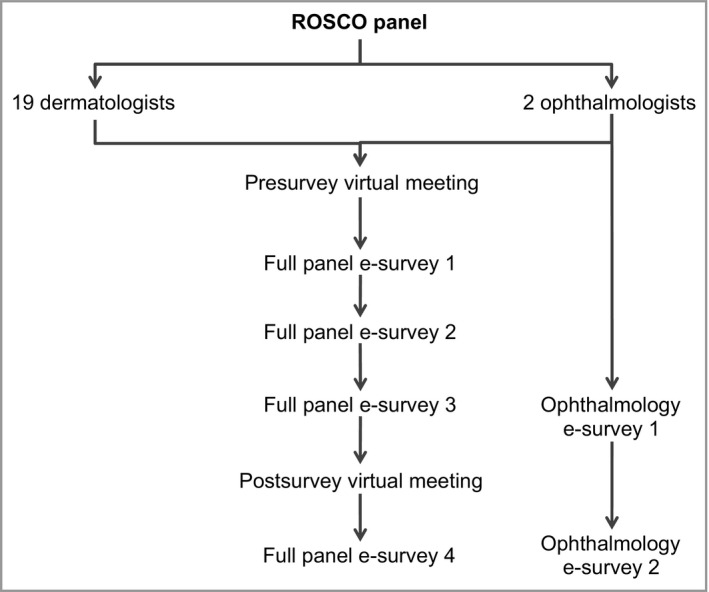
The ROSacea COnsensus (ROSCO) modified Delphi process.
E‐survey development and administration
Consensus statements were structured to assess the level of agreement using the terms ‘strongly disagree’, ‘disagree’, ‘agree’ or ‘strongly agree’. Consensus was defined as achievement of ≥ 75% ‘agree’ or ‘strongly agree’. Some questions were open‐ended to allow for the development of consensus statements in a subsequent round of voting. Items not achieving consensus in e‐surveys 1–3 were discussed during the virtual meeting. Discussion was used to refine the consensus statements, which were voted on in an e‐survey 4. E‐surveys were programmed, administered and responses collated by Ogilvy Health, in order to maintain the blind nature of the study.
Results
Definition of consensus recommendations
Consensus statement voting is given in brackets (e.g. 15/21 voted ‘agree’ or ‘strongly agree’). Some panellists abstained when their clinical expertise did not extend to a particular subject. Full statements are available in Appendix S3 (see Supporting Information).
Burden of disease and treatment goals
Box 1. Recommendations on burden of disease and treatment goals.
-
Rosacea can have a high burden for some patients, independently of clinically assessed severity (n = 21/21). Disease burden should be discussed during consultations (n = 19/21) and before deciding on treatment in conjunction with patients (n = 20/21).
This includes nonvisible symptoms, which can have a particularly adverse impact (n = 20/21)
There is a lack of guidance on measuring patient satisfaction with rosacea treatments (n = 20/21).
-
The Dermatology Life Quality Index (DLQI) can provide valuable insight into the quality of life (QoL) of patients with rosacea (n = 17/21). Certain elements are particularly relevant:
Facial symptoms of itch, soreness, pain or stinging (n = 19/21)
Embarrassment or self‐consciousness (n = 20/21)
Impact on social or leisure activities (n = 18/21)
-
Since the DLQI is not disease‐specific, alternative questions for clinical use (based on previously identified factors associated with high disease burden)22 can be asked of the patient [also incorporated into the Rosacea Tracker; Appendix S4 (see Supporting Information)]. If an individual scores highly on the following questions, the panel recommended that the physician considers using the full DLQI to assess the patient's burden of disease and/or refer for psychological consult (n = 21/21):
In the past month, how much have your rosacea signs and symptoms affected your QoL (n = 20/21)?
In the past month, how much has the time lost to your rosacea affected your QoL (n = 19/21)?
In the past month, how much has rosacea affected productivity in the workplace or education (n = 20/21)?
In the past month, how well controlled has your rosacea been (n = 21/21)?
Achieving clear skin vs. almost clear should be the primary objective when treating rosacea (n = 20/21), in order to minimize disease impact on patients’ QoL (n = 20/21), maximize time to disease relapse (n = 15/19) and maximize patient satisfaction from treatment (n = 20/21).
Additional comments
The DLQI is not disease‐specific, but offers an option in the absence of other appropriate disease‐specific tools. Although the RosaQol questionnaire is specific to rosacea, the ROSCO 2017 recommendations have previously considered it to be impractical for daily clinical usage.13 Furthermore, a minimal important difference has not been established, making result interpretation difficult.
While achieving skin clearance of rosacea is ideal, this may not be possible for all patients due to limitations such as cost or access and some patients are satisfied with subtotal improvement. It has been demonstrated that achieving complete clearance in rosacea with papules/pustules and erythema can delay time to disease relapse;23 however, further evaluation is required for other rosacea features.
Diagnosis, classification and assessment
Box 2. Recommendations on rosacea diagnosis, classification and assessment.
Additional comments
Together with considerations for severity, the cutaneous feature descriptions can help improve and standardize disease diagnosis and monitoring. Melanin can camouflage erythema and telangiectases, leading to underdiagnosis or underappreciation in skin phototypes V and VI. Minor features are subjective and individuals may experience or describe these features differently. Patient validation would therefore be valuable for these descriptions.
Table 1.
Descriptions of cutaneous rosacea features by consensus
| Cutaneous rosacea features | Description |
|---|---|
| Diagnostic features | |
| Phymatous changes | Facial skin thickening due to fibrosis and/or sebaceous glandular hyperplasia. Most commonly affects the nose, where it can impart a bulbous appearance (n = 19/20) |
| Persistent erythema | Background ongoing centrofacial redness. May periodically intensify in response to variable triggers. In darker skin phototypes (V and VI), erythema may be difficult to detect visually (n = 19/20) |
| Major features | |
| Flushing/transient erythema | Temporary increase in centrofacial redness, which may include sensations of warmth, heat, burning and/or pain (n = 20/20) |
| Papules and pustules | Red papules and pustules, usually in the centrofacial area. Some may be larger and deeper (n = 18/20) |
| Telangiectases | Visible vessels in the centrofacial region but not only in the alar area (n = 19/20) |
| Minor features | |
| Burning sensation of the skin | An uncomfortable or painful feeling of heat, typically in the centrofacial region (n = 19/20) |
| Stinging sensation of the skin | An uncomfortable or painful sharp, pricking sensation, typically in the centrofacial region (n = 19/20) |
| Dry sensation of the skin | Skin that feels rough. May be tight, scaly and/or itchy (n = 19/20) |
| Oedema | Localized facial swelling. Can be soft or firm (nonpitting) and may be self‐limited in duration or persistent (n = 20/20) |
Table 2.
Considerations for severity assessment of minor cutaneous rosacea features by consensus
| Cutaneous rosacea features | Considerations when assessing severity |
|---|---|
| Burning sensation of the skin | Duration; frequency; intensity; extent (areas involved); associations with flushing; triggers; and impact on daily life (n = 19/19) |
| Stinging sensation of the skin | Duration; frequency; intensity; extent (areas involved); triggers; characteristic of the sensation; and impact on daily life (n = 19/19) |
| Dry sensation of the skin | Duration; frequency; intensity; extent (areas involved); pruritus; roughness; scale; tightness; peeling; how often moisturizers need to be applied; and impact on daily life (n = 20/20) |
| Oedema | Duration; frequency; degree of swelling (depth, pitting and distortion); extent (areas involved); daily fluctuation; and impact on daily life (n = 19/19) |
Treatment and monitoring
Box 3. Recommendations on rosacea treatment.
-
In line with recently published evidence, the 2017 treatment algorithm has been updated with consensus recommendations for treatment options based on quality of evidence and weight of clinical experience (Appendix S5; Supporting Information). Updates include:
Topical alpha‐adrenergic modulating agents and oral beta blockers have been removed, as there is limited evidence to support their use for treatment of flushing/transient erythema (n = 16/17 and n = 17/18, respectively). However, clinical experience suggests that these agents could be considered in certain situations
Topical alpha‐adrenergic modulating agents (n = 20/20), intense pulsed light (IPL; n = 15/15) and vascular lasers (e.g. pulsed‐dye laser and 532‐nm potassium titanyl phosphate laser; n = 18/18) have been added as treatment options for persistent centrofacial erythema. Use of IPL and vascular lasers in darker skin phototypes requires consideration by a healthcare provider with experience in this situation (n = 16/18), as it can result in dyspigmentation
-
Combination treatment could benefit some patients with more severe rosacea (n = 20/20) and those presenting with multiple rosacea features (n = 20/21).
The benefits of combining treatments in rosacea include: helping achieve skin clear of rosacea (n = 19/20); helping some patients achieve treatment goals more quickly (n = 19/20); maximizing remission periods (n = 19/20); and minimizing burden of disease (n = 19/20)
While the availability of new evidence for combining treatment in patients with multiple rosacea features can help to improve patient outcomes (n = 21/21), there remains an ongoing need for more studies to support combination treatment use in rosacea (n = 21/21).
Box 4. Recommendations on rosacea monitoring.
Rosacea is a chronic disease that requires long‐term management (n = 21/21) and, as such, requires ongoing dialogue between patient and physician.
When monitoring treatment satisfaction, the highest priority factors for discussion during consultations are tolerability (n = 21/21), cost (n = 20/21) and primary efficacy (n = 19/21).
To maximize treatment adherence, the highest priority factors for discussion during consultations are expectations of treatment duration (n = 21/21); time to onset of efficacy (n = 19/21); additional requirements (e.g. general skincare, trigger avoidance, camouflage) (n = 17/21); need for maintenance therapy (n = 17/21); chances of achieving clear skin (n = 17/21); and potential for side‐effects (n = 17/21).
Additional comments
The individual nature of each patient's rosacea phenotype and personal circumstances demands individualized treatment and management. Not all treatments and considerations recommended here will apply to every patient or every country, but instead provide a guide or a range of options that can be tailored in discussion between physician and patient. Prior recommendations and cautions, particularly those around minimizing use of full‐dose antibiotics to avoid developing resistance, remain valid.17
Ocular rosacea
Consensus statements
Box 5. Recommendations on ocular rosacea.
Optimal diagnosis of ocular rosacea (n = 21/21) and description of its features (n = 20/21) remain unmet needs.
The following ocular rosacea features require referral by a dermatologist to an ophthalmologist for treatment: blepharokeratoconjunctivitis (n = 20/21); sclerokeratitis (n = 20/21); anterior uveitis (n = 19/21); and blepharoconjunctivitis (n = 16/21).
Systematic, evidence‐based guidelines for ocular rosacea are still required (n = 16/16).
The panel reached consensus on descriptions of ocular rosacea features as recommended by the ophthalmologist panellists (Table 3), and recommended considerations for assessing severity of ocular rosacea features (Table 4; note that these are recommended rather than consensus, due to n = 2). Photographs have been provided in an image library (Appendix S6; see Supporting Information) to support descriptions and aid diagnosis.
Table 3.
Descriptions of ocular rosacea features
| Ocular rosacea features | Description |
|---|---|
| Lid margin telangiectasia | Visible vessels around the eyelid margins. May be difficult to detect visually in darker skin phototypes (V and VI) |
| Blepharitis | Inflammation of the eyelid margin, most commonly arising from Meibomian gland dysfunction |
| Keratitis | Inflammation of the cornea that can lead to defects and, in the most severe cases, vision loss |
| Conjunctivitis | Inflammation of the mucous membranes lining the inner surface of the eyelids and bulbar conjunctiva. Typically associated with injection or vascular congestion and conjunctival oedema |
| Anterior uveitis | Inflammation of the iris and/or ciliary body |
Note that these are recommendations rather than consensus due to n = 2. Both ophthalmologists voted ‘Agree’ or ‘Strongly agree’ to the descriptions.
Table 4.
Considerations for severity assessment of ocular rosacea features
| Ocular rosacea features | Considerations when assessing severity |
|---|---|
| Lid margin telangiectasia | Degree of vascularization; density; Meibomian gland dysfunction; presence of evaporative tear dysfunction |
| Blepharitis | Degree of eyelid inflammation; pain; swelling |
| Keratitis | Location; degree of inflammation; defects on staining (e.g. ulceration); pain; foreign body sensation |
| Conjunctivitis | Presence of interpalpebral congestion; degree of conjunctival injection; foreign body sensation |
| Anterior uveitis | Anterior chamber cell count; flare |
Note that these are recommendations rather than consensus due to n = 2. Both ophthalmologists voted ‘Agree’ or ‘Strongly agree’ to the descriptions.
Additional comments
Ocular rosacea may often be overlooked by dermatologists. Education on ocular rosacea for ophthalmologists, dermatologists and general practitioners could improve screening, diagnosis and management of these patients. Similarly, greater involvement of ophthalmologists in rosacea clinical studies would increase the evidence base for ocular features, as high‐quality evidence is limited.
Clinical tools and ongoing uptake of the phenotype approach
Overall, the ROSCO 2017 consensus has been well received and has coincided with an increase in the use of the phenotype approach in rosacea (Fig. 2). Some panellists reported challenges to implementing the approach in daily practice and recommended items to facilitate uptake in multiple areas; notable among these were photographs, record‐keeping sheets and case studies. Consensus statements from the current ROSCO project have been used to develop a clinical checklist14 into the Rosacea Tracker prototype tool, which is targeted at dermatologists, ophthalmologists and patients. It aims to provide an ongoing record of a patient's rosacea phenotype and to help monitor changes in disease features, patient impact and response to treatment. The panel has suggested further validation and refinement of this tool. To exemplify treatment of common phenotypes and support practical use of the 2017 treatment algorithm,17 further consensus was gained on seven patient case studies representing common phenotypes; an accompanying phenotype image library with feature descriptions and multiple skin phototypes is also provided. All are available in Appendix S7 (see Supporting Information).
Figure 2.
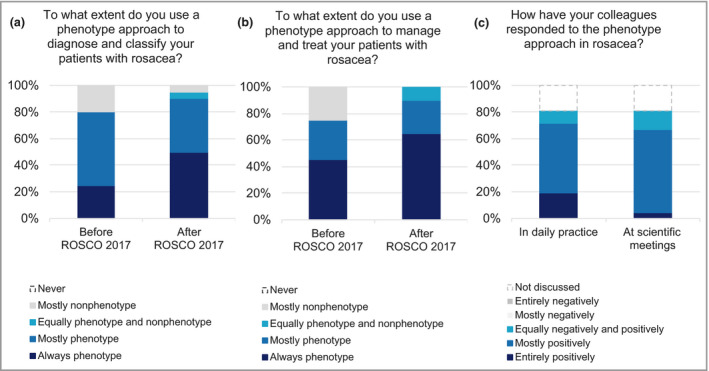
Usage and reception of the phenotype approach in rosacea. (a) The extent to which ROSacea COnsensus (ROSCO) panel members report using a phenotype approach for rosacea diagnosis and classification before and after the ROSCO 2017 recommendations (n = 20). (b) The extent to which ROSCO panel members report using a phenotype approach for rosacea management and treatment before and after the ROSCO 2017 recommendations (n = 20). (c) Response of ROSCO panellists’ colleagues to the phenotype approach in rosacea in daily practice and at scientific meetings (n = 21).
Discussion
This ROSCO 2019 consensus further refines and extends recommendations for a phenotype approach in rosacea diagnosis, classification and management. These recommendations integrate recently published evidence with expert clinical opinion and cover multiple topics pertinent to patients with cutaneous and/or ocular rosacea.
The impact of rosacea on the lives of patients has not been fully appreciated and remains inadequately addressed.22, 24, 25, 26 There is no short, practical, rosacea‐specific tool to assess disease burden across all rosacea phenotypes. The panel has therefore proposed a methodology and prototype tool to evaluate this problem, based upon the demonstrated importance of clearing a patient of rosacea,23 with the aim of fully controlling this chronic condition.
Despite growing evidence and guidance for ocular rosacea pathogenesis and management, discussion of ocular abnormalities and associations with cutaneous rosacea features is conflicting and guidance has not been offered beyond the ROSCO 2017 recommendations.13, 16, 17, 19, 26, 27, 28 The present consensus strives to remedy this, by providing practical support for diagnosis and referral points for patients with ocular rosacea.
Challenges to adoption of the phenotype approach have been identified and discussed.14 Key elements include tools and guidance to facilitate use of the phenotype approach in the clinic.14 The ROSCO project endeavours to support this approach, by developing clinical tools based on its 2019 recommendations. This guidance can support implementation of a phenotype approach globally, while evidence for the benefits of combining treatments continues to grow.18, 29, 30, 31, 32
The advantages and limitations of the Delphi process in relation to the ROSCO project have been discussed in detail previously.13, 17 The majority of concerns surround the use of clinical opinion to develop consensus statements, rather than published evidence.33, 34 However, in assessing the clinical approach to rosacea, where high‐quality evidence is limited,5 the Delphi process is a systematic, egalitarian method well suited to developing clinical recommendations, until additional appropriate evidence becomes available.35 The ROSCO panel continues to base recommendations on a large body of clinical experience, with published evidence where possible, informed through literature searches. We attempt to overcome bias in the Delphi voting process through blinded voting.
Conclusion
The ROSCO project continues to provide a global perspective on rosacea diagnosis, classification and management, and supports the transition to a phenotype approach. This updated consensus offers recommendations for assessing the burden of rosacea, aiming for clear as a treatment goal; diagnosing, classifying and describing disease features; managing patients using combination therapy; and disease monitoring. Further work is still needed, particularly education around ocular rosacea and continued development, refinement and validation of tools to facilitate both daily practice and clinical research. However, these recommendations can provide a basis for local guideline development and help to improve outcomes in all patients with rosacea by individualizing management.
Supporting information
Appendix S1 Conflicts of interest.
Appendix S2 Literature search.
Appendix S3 Consensus statements and voting results.
Appendix S4 Rosacea tracker.
Appendix S5 ROSCO project 2019: updated treatment algorithm.
Appendix S6 Phenotype image library.
Appendix S7 Patient case studies.
Powerpoint S1 Journal Club Slide Set.
Video S1 Author video.
Acknowledgments
Medical writing and administrative support was provided by Ellie Hughes PhD and Victoria Smith BSc at Ogilvy Health.
Funding sources The planning and delivery of this project was funded by Galderma. The sponsor was not involved in the voting, discussion or handling of data. All authors participated in consensus statement development and in the drafting, critical revision and approval of the final version of the manuscript.
Conflicts of interest See Appendix S1.
Plain language summary available online
References
- 1. Wilkin J, Dahl M, Detmar M et al Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002; 46:584–7. [DOI] [PubMed] [Google Scholar]
- 2. van Zuuren EJ, Graber MA, Hollis S et al Interventions for rosacea. Cochrane Database Syst Rev 2004; CD003262. [DOI] [PubMed] [Google Scholar]
- 3. van Zuuren EJ, Graber MA, Hollis S et al Interventions for rosacea. Cochrane Database Syst Rev 2005; CD003262. [DOI] [PubMed] [Google Scholar]
- 4. van Zuuren EJ, Kramer S, Carter B et al Interventions for rosacea. Cochrane Database Syst Rev 2011; CD003262. [DOI] [PubMed] [Google Scholar]
- 5. van Zuuren EJ, Fedorowicz Z, Carter B et al Interventions for rosacea. Cochrane Database Syst Rev 2015; CD003262. [DOI] [PubMed] [Google Scholar]
- 6. Dahl MV. Rosacea subtypes: a treatment algorithm. Cutis 2004; 74:21–7. [PubMed] [Google Scholar]
- 7. Odom R. The nosology of rosacea. Cutis 2004; 74:5–8. [PubMed] [Google Scholar]
- 8. Powell FC. Clinical practice. Rosacea. N Engl J Med 2005; 352:793–803. [DOI] [PubMed] [Google Scholar]
- 9. Goldgar C, Keahey DJ, Houchins J. Treatment options for acne rosacea. Am Fam Physician 2009; 80:461–8. [PubMed] [Google Scholar]
- 10. Odom R, Dahl M, Dover J et al Standard management options for rosacea, part 1: overview and broad spectrum of care. Cutis 2009; 84:43–7. [PubMed] [Google Scholar]
- 11. Reinholz M, Tietze JK, Kilian K et al Rosacea – S1 guideline. J Dtsch Dermatol Ges 2013; 11:768–80. [DOI] [PubMed] [Google Scholar]
- 12. Tan J, Steinhoff M, Berg M et al Shortcomings in rosacea diagnosis and classification. Br J Dermatol 2017; 176:197–9. [DOI] [PubMed] [Google Scholar]
- 13. Tan J, Almeida LMC, Bewley A et al Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176:431–8. [DOI] [PubMed] [Google Scholar]
- 14. Tan J, Berg M, Gallo RL, Del Rosso JQ. Applying the phenotype approach for rosacea to practice and research. Br J Dermatol 2018; 179:741–6. [DOI] [PubMed] [Google Scholar]
- 15. Del Rosso JQ, Thiboutot D, Gallo R et al Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 1: a status report on the disease state, general measures, and adjunctive skin care. Cutis 2013; 92:234–40. [PubMed] [Google Scholar]
- 16. Gallo RL, Granstein RD, Kang S et al Standard classification and pathophysiology of rosacea: the 2017 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol 2018; 78:148–55. [DOI] [PubMed] [Google Scholar]
- 17. Schaller M, Almeida LMC, Bewley A et al Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176:465–71. [DOI] [PubMed] [Google Scholar]
- 18. van Zuuren EJ, Fedorowicz Z, Tan J et al Interventions for rosacea based on the phenotype approach: An updated systematic review including GRADE assessments. Br J Dermatol 2019; 181:65–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reinholz M, Ruzicka T, Steinhoff M et al Pathogenesis and clinical presentation of rosacea as a key for a symptom‐oriented therapy. J Dtsch Dermatol Ges 2016; 14 (Suppl. 6):4–15. [DOI] [PubMed] [Google Scholar]
- 20. Woo YR, Lim JH, Cho DH, Park HJ. Rosacea: molecular mechanisms and management of a chronic cutaneous inflammatory condition. Int J Mol Sci 2016; 17:E1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Drucker AM. Taking steps to improve the assessment and management of rosacea. Br J Dermatol 2017; 176:283–4. [DOI] [PubMed] [Google Scholar]
- 22. Rosacea: Beyond the visible. Available at: https://hosted.bmj.com/rosaceabeyondthevisible (last accessed 3 July 2019).
- 23. Webster G, Schaller M, Tan J et al Defining treatment success in rosacea as ‘clear’ may provide multiple patient benefits: results of a pooled analysis. J Dermatolog Treat 2017; 28:469–74. [DOI] [PubMed] [Google Scholar]
- 24. Harper J, Del Rosso JQ, Ferrusi IL. Cross‐sectional survey of the burden of illness of rosacea by erythema severity. J Drugs Dermatol 2018; 17:150–8. [PubMed] [Google Scholar]
- 25. Thomas CL, Kim B, Lam J et al Objective severity does not capture the impact of rosacea, acne scarring and photoaging in patients seeking laser therapy. J Eur Acad Dermatol Venereol 2017; 31:361–6. [DOI] [PubMed] [Google Scholar]
- 26. Gallo RL, Granstein RD, Kang S et al Rosacea comorbidities and future research: the 2017 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol 2018; 78:167–70. [DOI] [PubMed] [Google Scholar]
- 27. Asai Y, Tan J, Baibergenova A et al Canadian clinical practice guidelines for rosacea. J Cutan Med Surg 2016; 20:432–45. [DOI] [PubMed] [Google Scholar]
- 28. Al‐Amry MA, Al‐Ghadeer HA. Ocular acne rosacea in tertiary eye center in Saudi Arabia. Int Ophthalmol 2016; 38:59–65. [DOI] [PubMed] [Google Scholar]
- 29. Gold LS, Papp K, Lynde C et al Treatment of rosacea with concomitant use of topical ivermectin 1% cream and brimonidine 0.33% gel: a randomized, vehicle‐controlled study. J Drugs Dermatol 2017; 16:909–16. [PubMed] [Google Scholar]
- 30. Del Rosso JQ, Johnson S, Jackson M. Combined doxycycline 40 mg modified release capsules plus ivermectin 1% cream therapy for severe papulopustular rosacea. Presented at Fall Clinical Dermatology, Las Vegas, CA, U.S.A., 18–21 October 2018.
- 31. ClinicalTrials.gov . Oracea soolantra association in patients with severe rosacea (ANSWER). Available at: https://clinicaltrials.gov/ct2/show/NCT03075891 (last accessed 3 July 2019).
- 32. Steinhoff M, Vocanson M, Voegel JJ et al Topical ivermectin 10 mg/g and oral doxycycline 40 mg modified‐release: current evidence on the complementary use of anti‐inflammatory rosacea treatments. Adv Ther 2016; 33:1481–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Armon K, Stephenson T, MacFaul R et al An evidence and consensus based guideline for acute diarrhoea management. Arch Dis Child 2001; 85:132–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995; 311:376–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fletcher AJ, Marchildon GP. Using the Delphi method for qualitative, participatory action research in health leadership. Int J Qual Methods 2014; 13:1–18. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Conflicts of interest.
Appendix S2 Literature search.
Appendix S3 Consensus statements and voting results.
Appendix S4 Rosacea tracker.
Appendix S5 ROSCO project 2019: updated treatment algorithm.
Appendix S6 Phenotype image library.
Appendix S7 Patient case studies.
Powerpoint S1 Journal Club Slide Set.
Video S1 Author video.


