Abstract
Objective
People with diabetes show great variability in weight gain and duration of obesity at the time of diagnosis. BMI trajectories and other cardiometabolic risk factors prior to type 2 diabetes were investigated.
Methods
A total of 6,223 participants from the Rotterdam Study cohort were included. BMI patterns before diagnosis of diabetes were identified through latent class trajectories.
Results
During a mean follow‐up of 13.7 years, 565 participants developed type 2 diabetes. Three distinct trajectories of BMI were identified, including the “progressive overweight” group (n = 481, 85.1%), “progressive weight loss” group (n = 59, 10.4%), and “persistently high BMI” group (n = 25, 4.4%). The majority, the progressive overweight group, was characterized by a steady increase of BMI in the overweight range 10 years before diabetes diagnosis. The progressive weight loss group had fluctuations of glucose and marked beta cell function loss. The persistently high BMI group was characterized by a slight increase in insulin levels and sharp increase of insulin resistance accompanied by a rapid decrease of beta cell function.
Conclusions
Heterogeneity of BMI changes prior to type 2 diabetes was found in a middle‐aged and elderly white population. Prevention strategies should be tailored rather than focusing only on high‐risk individuals.
Study Importance.
What is already known?
-
►
Type 2 diabetes continues to be a public health threat worldwide, partly fueled by the increasing burden of obesity.
-
►
People with diabetes show great variability in terms of BMI, weight gain, and duration of obesity at the time of diagnosis.
What does this study add?
-
►
Using latent class trajectory analysis to model the patterns of BMI in the years before people developed diabetes, three different trajectories of BMI patterns were identified.
-
►
The majority of people (85.1%) were characterized by small weight gains within the overweight range before diabetes diagnosis, followed by people who lost weight during the study (10.4%). Unlike commonly expected, people with high BMI were the smallest group (4.4%). Our findings show that the majority of people might be missed from the screening efforts despite being at high risk. Prediction in these groups is difficult.
-
►
The results emphasize the complexity of diabetes pathophysiology in the population and the need to stimulate debate for precision prevention strategies.
Introduction
Observational studies have extensively shown BMI to be associated with risk for type 2 diabetes (1). Notably, the number of people with diabetes is expected to increase dramatically in the forthcoming years given the parallel increase in obesity rates worldwide (2, 3). However, patients with diabetes show great variability in terms of weight, weight gain, and duration of obesity at the time of diagnosis (4, 5, 6). Consequently, understanding the complex pathophysiological mechanism regarding patterns of change in BMI might provide new insights into precision prevention strategies to confront the new epidemiological challenges of obesity and diabetes.
Former population studies investigating BMI changes in association with chronic diseases such as cardiovascular disease (CVD) and diabetes have shown heterogeneous signatures of disease development across BMI trajectories. Previously, we identified three distinct patterns of BMI prior to CVD development, and the majority of participants who developed the disease were characterized with a stable BMI over time, highlighting a heterogeneous nature of CVD not entirely attributed to BMI (7). Similarly, another study among 6,705 British participants showed three BMI patterns accompanied with distinctive cardiometabolic risk profiles, with the majority of individuals showing modest weight gain prior to diabetes diagnosis (8). This finding goes against the common assumption that people who experienced recent substantial weight gain are more likely to be diagnosed with diabetes. Before drawing firm conclusions on the process of diabetes development, it is important to test whether similar trends are observed in other cohorts. Therefore, we aimed to identify and characterize BMI patterns in a European population of middle‐aged and elderly individuals before diabetes development. Additionally, trajectories of cardiometabolic risk factors, including glycemic traits, lipids, blood pressure, and waist circumference, within each BMI pattern were further examined.
Methods
Study population
The study was performed among participants of the prospective population‐based Rotterdam Study. In 1989, all residents aged 55 years or older in Ommoord, a suburb of Rotterdam, the Netherlands, were invited to participate in the study. Seventy‐eight percent of the invitees agreed to participate (n = 7,983). There were no eligibility criteria to enter the Rotterdam Study cohorts except the minimum age and residential area based on postal codes. The participants of the Rotterdam Study have been followed up for more than 22 years for a variety of diseases, and clinical data have been collected across five subsequent phases every 3 to 4 years. A more detailed description of the Rotterdam Study can be found elsewhere (9). The Rotterdam Study has been approved by the medical ethics committee according to the Population Screening Act: Rotterdam Study, executed by the Ministry of Health, Welfare and Sports of the Netherlands. All participants in the present analysis provided written informed consent to participate and to obtain information from their treating physicians.
For this study, we used visits of the first cohort. From 7,983 participants at baseline, we excluded 225 without informed consent, 916 with prevalent diabetes, 743 without BMI measurement throughout phases 1 to 5, and 1 with missing information of diabetes follow‐up. The final sample included 6,098 individuals (Figure 1).
Figure 1.
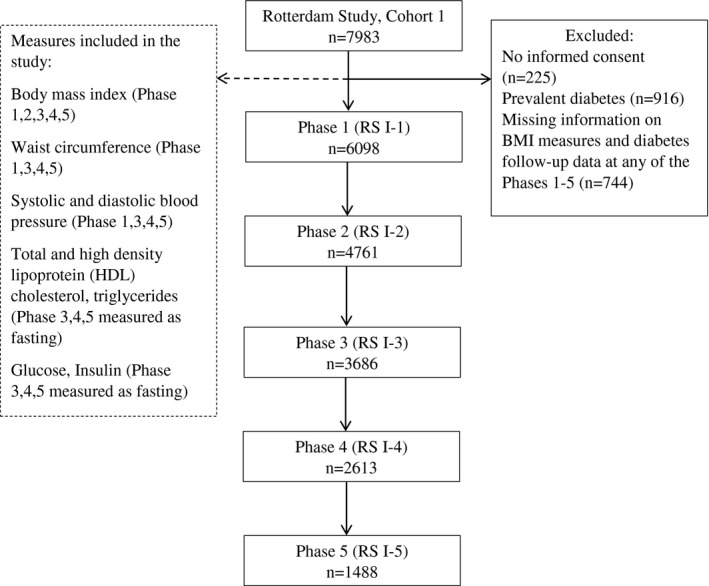
Flow diagram of the study participants for each phase.
Assessment of BMI and other cardiometabolic risk factors
Height and weight were measured with the participants standing without shoes or heavy outer garments. BMI was calculated as weight divided by height squared (kilograms per meter squared). Waist circumference was measured at the level midway between the lower rib margin and the iliac crest with participants in standing position without heavy outer garments and with emptied pockets, breathing out gently. Information on cardiometabolic risk factors was obtained through home interviews or measured at the study center, as previously described (10, 11). Height and weight were measured in all five phases, whereas systolic and diastolic blood pressure and waist circumference were measured in phases 1, 3, 4, and 5, and fasting total cholesterol, high‐density lipoprotein (HDL), cholesterol, and fasting plasma glucose were measured in phases 3, 4, and 5 (Figure 1). Serum total cholesterol, HDL cholesterol, and glucose were measured using standard laboratory techniques. Blood pressure was measured at the right brachial artery with a random‐zero sphygmomanometer with the participant in sitting position, and the mean of two consecutive measurements was used. Smoking status was classified as current smoking or others (former and never) in all phases. We assessed medication use for hypertension, hyperlipidemia, and diabetes through interview data.
Clinical outcome
The participants were followed from the date of baseline center visit onward. At baseline and during follow ‐up, cases of type 2 diabetes were ascertained by use of general practitioners’ records (including laboratory glucose measurements), hospital discharge letters, and serum glucose measurements from Rotterdam Study visits, which take place roughly every 4 years. According to the World Health Organization guidelines, type 2 diabetes was defined as a fasting blood glucose > 7.0 mmol/L or the use of blood glucose–lowering medication (12). Information regarding the use of blood glucose–lowering medication was derived from both structured home interviews and linkage to pharmacy records. At baseline, more than 95% of the Rotterdam Study population was covered by the pharmacies in the study area. All potential events of prediabetes and type 2 diabetes were independently adjudicated by two study physicians. In case of disagreement, consensus was sought with a specialist. Follow‐up data were completed until January 1, 2012 (13 ).
Statistical analysis
We used χ2 tests for categorical variables and t tests for continuous data when comparing the general characteristics between groups. Latent class trajectory analysis was performed to identify groups of participants with similar trajectories of BMI change during follow‐up until the occurrence of diabetes, as previously described ( 7,14). Regarding BMI trajectories, the groups are different from each other but not different within the class. This method does not allow for within‐class variation (as opposed to, for example, growth mixture modeling). Next, within each identified BMI group, the trajectories of change in other cardiometabolic risk factors during the time before diabetes diagnosis were developed (7).
The analysis was conducted by taking into account information from the population retrospectively from the date of diabetes diagnosis. The model used for latent class trajectories is a linear mixed‐effects model with BMI as the dependent variable and time before diagnosis (time 0), age, sex, and phase of study as independent variables. The variable “time before diabetes diagnosis” describes the shape of the trajectories of BMI and it was entered in the model as a covariate in a cubic specification. To assign the number of classes in the analysis, the Bayesian information criterion was used. The latent class trajectory model calculates a posterior probability of membership in each latent class for each participant, who is later assigned to the class for which his/her posterior probability is the highest. In order to ensure statistical and clinical meaningfulness, the following two conditions were imposed in the formation of latent classes: (1) they should contain at least 5% of participants, and (2) the mean posterior probability of each class should be higher than 75%.
Because the trajectories of change in BMI could differ between individuals who die during follow‐up and among individuals who do not die or develop diabetes during follow‐up (15), we divided the rest of the population into the following two subgroups: (1) diabetes‐free and alive until end of follow‐up and (2) nondiabetes mortality. For each identified BMI group (among individuals diagnosed with diabetes) and the two other groups (diabetes‐free and nondiabetes mortality), we examined the trajectories of other cardiometabolic risk factors, including waist circumference, systolic and diastolic blood pressure, fasting total cholesterol, low‐density lipoprotein (LDL) cholesterol, HDL cholesterol, fasting plasma glucose, and fasting plasma insulin. The homeostatic model assessment was used to estimate insulin resistance (HOMA‐IR) and beta cell function (HOMA ‐%B) (16). The absolute 8‐year risk of developing type 2 diabetes was calculated in all participants using the Framingham diabetes risk score (17), and the Framingham CVD risk score was used to estimate the 10‐year absolute risk of developing CVD (18). In our study, cardiovascular disease is composed of coronary heart disease (including fatal and nonfatal myocardial infarction and other coronary heart disease mortality) and stroke (fatal and nonfatal stroke), as previously described (10, 19, 20).
Because the aggregated effect of combined risk factors on diabetes might differ from each risk factor alone, we examined the trajectories of 8‐year diabetes risk and 10‐year diabetes risk in each BMI group. The predicted 10‐year CVD risk was calculated using the American College of Cardiology/American Heart Association Pooled Cohort Equation coefficients, which include age, sex, total cholesterol, HDL cholesterol, systolic blood pressure, blood pressure–lowering medication use, diabetes status, and smoking status in the prediction model (15). These trajectories of cardiometabolic risk factors were estimated using linear mixed‐effects models controlling for follow‐up time, age, sex, and study phase. Analyses of lipids were further adjusted for lipid‐ lowering treatment, analyses of blood pressure were further adjusted for antihypertensive treatment, and analyses of glucose were additionally adjusted for diabetes treatment. Quadratic and cubic terms for follow‐up time were included in the BMI groups (latent classes) when significant (P < 0.05). For individuals not developing diabetes during follow‐ up (diabetes‐free and nondiabetes mortality groups), year 0 is merely a time point in a normal life course, and we therefore fitted the trajectories by using linear models. Pairwise differences in growth curves between BMI groups were tested using F tests for each cardiometabolic risk factor. A χ2 test (for categorical variables) was used to compare participant characteristics between the groups. To account for multiple testing because of comparing three pairs of BMI groups, we used a Bonferroni‐adjusted significance level of 0.05/3 = 0.0167 for the F tests for each cardiometabolic risk factor. All other statistical tests used a significance level of 0.05, and all statistical tests were two sided. Analyses were conducted using R statistical software, version 3.0.1 (R Foundation for Statistical Computing, Vienna, Austria), with the package ‘‘lcmm’’ (10).
Results
Baseline characteristics of the study population are presented in Table 1. Overall, 6,223 participants with a mean age of 68.8 years, mostly women ( n = 3,681, 59.2%) and overweight (mean BMI = 26.24), were included in the study. The mean (SD) follow‐up time was 13.7 (6.5) years, during which 565 participants developed diabetes. Among individuals who did not develop diabetes, 1,891 (30%) remained alive until the end of follow‐up and 3,767 (60.5%) died from nondiabetes causes. The baseline characteristics of these subgroups are presented in Supporting Information Table S1. Table 2 shows characteristics of the participants at the time of diabetes diagnosis for all trajectories ’ groups or at the last examination for participants without diabetes.
Table 1.
Characteristics of study participants at first clinical visit
| N | 6,223 |
| Age (y) | 68.82 (8.85) |
| Gender (% women) | 3,681 (59.2) |
| Time before diagnosis/last visit (y) | 13.75 (6.55) |
| BMI (kg/m2) | 26.24 (3.70) |
| Waist circumference (cm) | 90.15 (11.10) |
| Systolic blood pressure (mm Hg) | 138.54 (22.00) |
| Diastolic blood pressure (mm Hg) | 73.82 (11.44) |
| Total cholesterol (mmol/L) | 5.83 (0.99) |
| LDL cholesterol (mmol/L) | 3.76 (0.91) |
| Triglycerides (mmol/L) | 1.49 (0.71) |
| HDL cholesterol (mmol/L) | 1.41 (0.40) |
| Glucose (mmol/L) | 5.68 (0.93) |
| Insulin (pmol/L) | 78.68 (61.44) |
| HOMA‐IR (units) | 123.54 (119.42) |
| HOMA ‐%B (units) | 1,642.76 (1,111.59) |
| Antihypertensive treatment (%) | 894 (17.0) |
| Lipid‐lowering medication (%) | 474 (13.6) |
| Current smoker (%) | 1,393 (23.1) |
Data are n (%) or mean (SD).
Fasting measurements of lipids and glycemic indices were available at third, fourth, and fifth visits of original Rotterdam Study cohort.
HDL, high‐density lipoprotein; HOMA‐%B, homeostatic model assessment‐beta cell function; HOMA‐IR, homeostatic model assessment‐insulin resistance; LDL, low‐density lipoprotein.
Table 2.
Characteristics of study participants at diagnosis for three groups with diabetes or at last visit for groups without diabetes
| Individuals developing diabetes during follow‐up (n = 565) | Individuals free of diabetes during follow‐up (n = 5,658) | ||||
|---|---|---|---|---|---|
| Weight loss, | Progressive weight gainers, | Persistently high BMI, | Diabetes‐free, | Nondiabetes mortality, | |
| n = 59 | n = 481 | n = 25 | n = 1,891 | n = 3,767 | |
| Age at diagnosis/last contact (y) | 67.2 (7.2) | 66.4 (7.0) | 64.5 (5.2) | 62.2 (5.0) | 72.4 (8.5) |
| Women (%) | 30 (50.8) | 282 (58.6) | 20 (80.0) | 1230 (65.0) | 2,119 (56.3) |
| BMI (kg/m2) | 24.9 (2.9) | 28.9 (3.3) | 39.0 (3.8) | 27.3 (4.1) | 26.2 (3.9) |
| Waist circumference (cm) | 90.5 (9.9) | 98.3 (10.3) | 117.7 (20.8) | 91.3 (11.9) | 92.6 (11.5) |
| Antihypertensive treatment (%) | 23 (39.7) | 200 (42.8) | 20 (83.3) | 883 (47.6) | 1021 (29.3) |
| Lipid‐lowering medication (%) | 11 (22.9) | 62 (23.9) | 5 (29.4) | 420 (26.6) | 255 (16.2) |
| Current smoker (%) | 22 (43.1) | 113 (32.7) | 6 (30.0) | 325 (18.4) | 866 (32.2) |
Data are n (%) or mean (SD).
Patterns of BMI change over time
Among 565 participants who developed diabetes, we identified three distinct trajectories of change in BMI levels (Figure 2). The first group (n = 481, 85.1%) representing the majority of individuals who developed diabetes, entered the study with a mean BMI of 28.0 and experienced an increase in BMI within the overweight range. This group was named “progressive overweight.” Thereafter, the second group (n = 59, 10.4%), who initially started with an average BMI of 26.6, continued to experience a decrease in BMI during the entire follow‐up. We named this group ‘‘progressive weight loss.’’ The third group comprised 25 (4.4%) individuals who entered the study with an average BMI of 35.4 and maintained their obesity status with fluctuating BMI values within the obesity range during the entire follow‐up until diagnosis of diabetes. Therefore, we named this group “persistently high BMI.”
Figure 2.
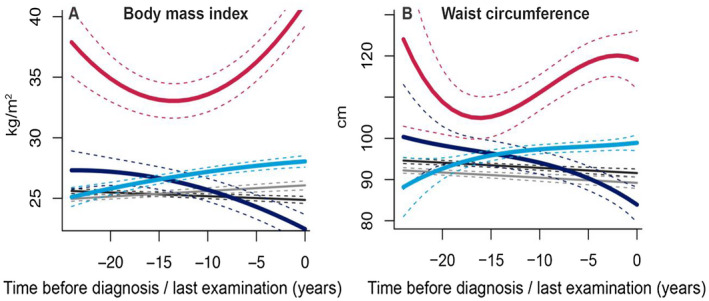
Trajectories of BMI and waist circumference during 22 years of follow‐up until diagnosis of type 2 diabetes, death, or censoring from the study. The figures represent a hypothetical man of 65 years old. Light blue, “progressive overweight” (including 85.1% of diabetes patients); red, “persistently high BMI” (4.4% of diabetes patients); dark blue, “progressive weight loss ” (10.4% of diabetes patients); gray, “diabetes‐free"; black, “nondiabetes mortality.” [Color figure can be viewed at wileyonlinelibrary.com]
Among 1,891 participants who did not develop diabetes and who were alive until the end of follow‐ up, the “diabetes‐free” group, the average BMI remained relatively stable (ranging from 25.9 to 27.3 during follow‐up). Among 3,767 who died of other causes during follow‐up, the “nondiabetes mortality” group, the average BMI at the start of the follow‐up was in the overweight range (average BMI = 26.4) and it reached the normal range just before the end of follow‐up. The analysis was performed in the total population, but in order to plot the trajectories of change in BMI and other cardiometabolic risk factors, we assumed a hypothetical individual to be a male of 65 years of age. Similar trajectories for a hypothetical woman of 65 years of age are shown in Supporting Information Figures S1‐S4.
Trajectories of waist circumference
Trajectories of waist circumferences differed significantly between the three groups (P < 0.001 for all pairwise comparisons) (Figure 2). The trajectories for the progressive overweight, persistently high BMI, and progressive weight loss groups broadly resembled the trajectories of BMI in these groups. The mean waist circumference in the diabetes‐free and nondiabetes mortality groups decreased slightly during follow ‐up.
Trajectories of glycemic indexes (glucose, insulin, and HOMA‐IR measurements)
Trajectories between fasting glucose levels differed between progressive overweight and persistently high BMI when compared with the progressive weight loss group (Figure 3). The mean glucose levels of the latter were fluctuating for the whole follow‐up time. For the progressive overweight and persistently high BMI groups, we observed an increase in mean levels of fasting glucose from 4.9 mmol/L to 9.4 mmol/L during follow‐up.
Figure 3.
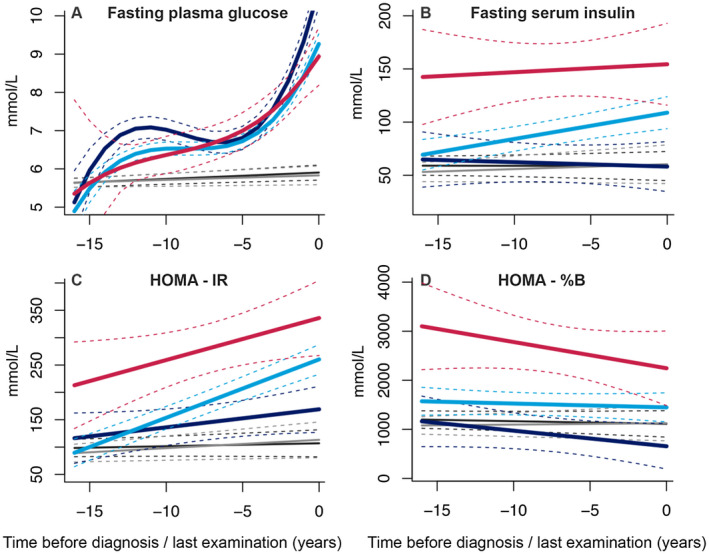
Trajectories of fasting plasma glucose, insulin, and homeostatic model assessment‐insulin resistance (HOMA‐IR) and homeostatic model assessment‐ beta cell function (HOMA‐%B) during 14 years of follow‐up until diagnosis of type 2 diabetes, death, or censoring from the study. The figures represent a hypothetical man of 65 years old. Light blue, “progressive overweight” (including 85.1% of diabetes patients); red, “persistently high BMI” (4.4% of diabetes patients); dark blue, “progressive weight loss” (10.4% of diabetes patients); gray, “diabetes‐free”; black, “non‐ diabetes mortality.” [Color figure can be viewed at wileyonlinelibrary.com]
All three groups showed significantly different trajectories for fasting insulin. The progressive overweight group experienced an increase in mean insulin levels (from 67 mmol/L to 109 mmol/L) during follow‐up. A slight increase was observed for the persistently high BMI group, which exhibited high insulin levels throughout the period, whereas modest decreases in insulin levels were observed for the progressive weight loss group.
Trajectories of HOMA‐IR differed between all three groups (P < 0.01 for all pairwise comparisons), demonstrating an incremental trend. The biggest increase was observed for the progressive overweight group (from 67 mmol/L to 258 mmol/L), followed by the persistently high BMI group, which was characterized by the highest average HOMA‐IR, and lastly, the progressive weight loss group. On the contrary, a decreasing trend was observed for HOMA‐%B for all the trajectories. The persistently high BMI group exhibited the highest average levels of HOMA‐%B accompanied by a steep decrease during follow ‐up. The progressive overweight group showed a stable trend with an average of 1,500 mmol/L, whereas the progressive weight loss group experienced lowered HOMA‐%B levels from 1,200 mmol/L to 700 mmol/L (Figure 3).
Trajectories of lipid profile and blood pressure
We found no differences in fasting total cholesterol levels, HDL, LDL, and triglycerides between the three groups of individuals who developed diabetes during follow‐up (Figure 4). For total cholesterol, we evidenced a marked increase in the persistently high BMI group starting from 4.5 mmol/L. The other two groups kept a lowering trend throughout the study, with all groups having an average total cholesterol level within the reference range (< 5.5 mmol/L). On the contrary, decreasing levels of HDL were observed for both the progressive overweight and persistently high BMI groups, while the average levels of the progressive weight loss group remained stable throughout the follow‐up. For LDL and triglyceride levels, the persistently high BMI group exhibited an increasing trend before the diabetes event. The average levels of LDL cholesterol demonstrated a modest decrease in the progressive overweight and progressive weight loss groups; meanwhile, the trend was reversed in both groups for triglyceride levels during follow‐up.
Figure 4.
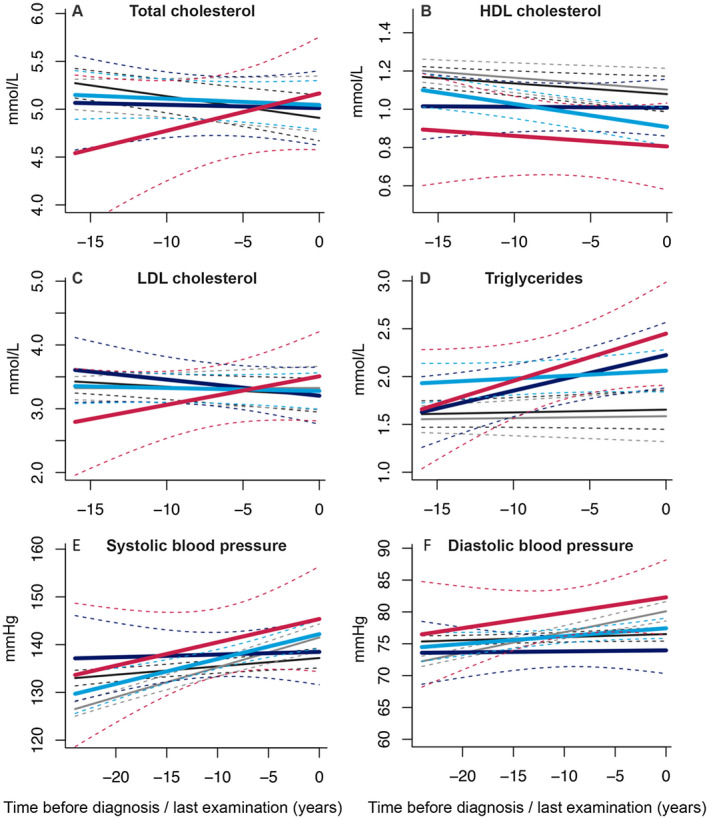
Trajectories of total cholesterol, high‐density lipoprotein (HDL) cholesterol, low‐density lipoprotein (LDL) cholesterol, triglycerides, systolic blood pressure, and diastolic blood pressure. The figures represent a hypothetical man of 65 years old. Light blue, “progressive overweight” (including 85.1% of diabetes patients); red, “persistently high BMI” (4.4% of diabetes patients); dark blue, “progressive weight loss” (10.4% of diabetes patients); gray, “diabetes‐free” ; black, “nondiabetes mortality.” [Color figure can be viewed at wileyonlinelibrary.com]
Trajectories of systolic and diastolic blood pressure differed significantly between all BMI groups. Both the progressive overweight and persistently high BMI groups showed an increasing trend before diagnosis of diabetes in both systolic and diastolic blood pressure levels, whereas the progressive weight loss group was relatively stable during follow‐ up (Figure 4).
Trajectories of estimated 8‐year type 2 diabetes risk
Framingham 8‐ year diabetes risk followed nearly the same stable trend for the progressive weight loss, diabetes‐free, and nondiabetes mortality groups (Supporting Information Figure S4A). The persistently high BMI group demonstrated an increase of 8‐year diabetes risk from 6% to 19% before diabetes diagnosis. A decreasing trend was shown for the progressive overweight group with a difference of nearly 4% to 5%.
Discussion
We examined BMI trajectories in a middle‐aged and elderly population ‐based study with more than 20 years of follow‐up using latent class trajectory analysis and identified the following three distinct groups of BMI changes: a “progressive overweight” group, a “persistently high BMI ” group, and a group with “progressive weight loss.” Within the BMI groups that developed diabetes, trajectories of obesity, visceral fat as measured with waist circumference, glucose, insulin, HOMA‐IR, and HOMA‐%B showed distinct patterns throughout the follow‐up of the study. This study shed further insights into the timing and the extent of pathophysiological changes before diabetes diagnosis in a middle‐aged and elderly European population, highlighting the heterogeneous nature of diabetes diagnosis depending on the level of obesity.
The majority of individuals in our study diagnosed with diabetes were progressively gaining weight within the overweight range. Development of diabetes was not preceded by a recent weight gain, as commonly believed, but rather by a continuous weight gain over the years. Similarly, in the study from Vistisen et al. ( 8), most of the individuals were found to have overweight when they entered the study and changed very little during follow‐up until diabetes diagnosis. While there was relatively stable HOMA beta cell function, they exhibited progressively increasing trends of insulin levels and HOMA‐IR starting from the beginning of the follow‐up, whereas glucose levels increased substantially approximately 5 years before the diagnosis. The persistently high BMI group showed prominent trajectories of glucose metabolism parameters as compared with the progressive overweight group. These results are in line with a previous study investigating BMI trajectories in relation to glucose and insulin metabolism; individuals with similar persistently high BMI were characterized by a high level of beta cell function (an adaptive response of the pancreas to obesity), which decreased over time. Similar trends were followed by high plasma insulin levels and insulin resistance ( 21).
As expected, Framingham 8‐year diabetes risk was predicting well for the persistently high BMI group. In the progressive overweight group, we observed a decreasing trend of the predicted risk for diabetes throughout the period of follow‐up, whereas the progressive weight loss group did not change substantially. These results might suggest that the diagnosis of diabetes might be biased toward enhanced screening efforts reserved to individuals with obesity rather than overweight. Similar findings were reported in an investigation of obesity trajectories prior to diabetes development in a UK study (8). The “stable overweight” group was less often diagnosed with diabetes by general practitioners than the “persistently high BMI” group. This indicates an inclination of physicians to more effectively screen individuals with obesity in comparison to individuals with overweight.
We found that 10.4% of participants (second largest group) experienced progressive weight loss before diagnosis of diabetes, a pattern not observed in the UK investigation (8). In an Austrian study of older adults, three trajectories of BMI before diabetes diagnosis were discovered, two of which were characterized by a plateau or increase followed by a decrease of BMI (22). These groups had increased overall and diabetes mortality. Among the elderly, the relation between body weight, body composition, and health behaviors is different from younger adults (23, 24). Weight loss has often been associated with a high risk for mortality (15, 22, 25, 26), while its association with CVD still remains inconclusive (26, 27). In this group, waist circumference trajectories followed the same decreasing trend as BMI, while fluctuations of fasting glucose levels with a sharp increase 5 years before diabetes diagnosis were observed. However, these changes did not correspond to an increase of insulin levels, while HOMA‐%B levels were the lowest among the three groups, decreasing constantly. Despite the weight loss progression prior to diabetes diagnosis, the inability to respond adequately to high glucose levels, together with the impaired beta cell compensation from the pancreas, appears to be involved in the disease development regardless of obesity levels. Individuals in this group might benefit from strategies focusing on prevention of further loss of beta cell function rather than tackling peripheral insulin sensitivity. This concept is supported by previous work (28, 29) and by our recent observation in a family study (30).
Despite the differences in BMI trajectories, most of the other cardiometabolic risk factors, including blood pressure and lipid profile, developed without substantial changes in the three groups. Moreover, we were able to assess medication data for all BMI subgroups, and we found that antihypertensive medication and lipid‐lowering drugs were more frequently used among the persistently high BMI individuals followed by progressive overweight and progressive weight loss groups. This data showed that, most likely, individuals with overweight and those losing weight over time are less likely to receive medication. Notably, the progressive overweight group and progressive weight loss group constituted more than 95% of the middle‐ aged and elderly population developing diabetes events. Therefore, adequate treatment for these categories of patients could have a substantial impact on decreasing the overall burden of diabetes and associated comorbidities in the total population.
In recent years, many statistical methods have been developed to explore trajectories of BMI, including population‐level growth curves, hierarchical clustering, mixed‐effects models, etc. ( 21-22,31). Although they might contribute to our understanding of pathophysiological mechanisms, they offer a simplified scenario of the complexity and heterogeneity of disease. In our quest for precision medicine, identification of homogeneous groups in terms of risk patterns may facilitate stratification for targeted interventions. In this regard, latent class trajectory analysis allows for the identification of classes of people who are very similar toward the development of a particular factor over time, but at the same time, they are different when compared with other groups.
Strengths of our study include the prospective design with availability of repeated measurements for BMI and other cardiometabolic risk factors, including medication use data, over a long follow ‐up time, which altogether allowed performing latent class trajectory analysis. Previous literature has used BMI in predefined categories, which might introduce some misclassification bias, whereas our analysis allows full exploration of heterogeneous patterns of BMI changes that might influence diabetes risk. Nevertheless, one of the drawbacks of this method is the assigned not‐ balanced sample size pertaining to the groups, which makes comparisons of the result difficult in the light of statistical power. In addition, generalizability of the study may be limited because of the specific population analyzed. The majority of individuals were middle‐aged and elderly, with a mean age of 68.8 years old.
In conclusion, we identified three distinct patterns of BMI changes prior to diagnosis of type 2 diabetes. These population patterns contribute to our understanding of the complex etiology and pathophysiology of type 2 diabetes and the challenges that arise when implementing weight‐loss–intervention programs for diabetes management. In the realm of precision medicine, we were able to identify groups with similar BMI trajectories by employing latent class trajectory analysis that might facilitate stratification for targeted interventions in the future. It has always been expected that individuals who are more prone to develop diabetes are those with obesity or those who gained substantial weight recently. However, we found the majority of individuals were characterized by small weight gain (within the overweight range) during follow‐up before diabetes diagnosis. In line with previous research, we showed that many individuals with overweight or normal weight might be missed from screening efforts (as measured, for example, with Framingham risk score), although they are at high risk. Therefore, prediction in these groups is difficult. Future studies should establish how to better target these subgroups and develop precision management strategies to prevent diabetes.
Disclosure
The authors declared no conflict of interest.
Author contributions
JN and KDh contributed to the conception and design of the study and researched the data. All authors contributed to the acquisition and/or interpretation of the data. JN and KDh wrote the manuscript. All authors critically read the manuscript, suggested revisions, and approved the final version of the manuscript. OHF is the guarantor for the work as a whole, including study design, access to data, and the decision to submit and publish the manuscript.
Supporting information
Supplementary Material
References
- 1. Dhana K, Nano J, Ligthart S, et al. Obesity and life expectancy with and without diabetes in adults aged 55 years and older in the Netherlands: a prospective cohort study. PLoS Med 2016;13:e1002086. doi: 10.1371/journal.pmed.1002086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NCD Risk Factor Collaboration . Trends in adult body‐mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population‐based measurement studies with 19.2 million participants. Lancet 2016;387:1377‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NCD Risk Factor Collaboration . Worldwide trends in diabetes since 1980: a pooled analysis of 751 population‐based studies with 4.4 million participants. Lancet 2016;387:1513‐1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brancati FL, Wang NY, Mead LA, Liang KY, Klag MJ. Body weight patterns from 20 to 49 years of age and subsequent risk for diabetes mellitus: the Johns Hopkins Precursors Study. Arch Intern Med 1999;159:957‐963. [DOI] [PubMed] [Google Scholar]
- 5. Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol 1997;146:214‐222. [DOI] [PubMed] [Google Scholar]
- 6. Hanson RL, Narayan KM, McCance DR, et al. Rate of weight gain, weight fluctuation, and incidence of NIDDM. Diabetes 1995;44:261‐266. [DOI] [PubMed] [Google Scholar]
- 7. Dhana K, van Rosmalen J, Vistisen D, et al. Trajectories of body mass index before the diagnosis of cardiovascular disease: a latent class trajectory analysis. Eur J Epidemiol 2016;31:583‐592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vistisen D, Witte DR, Tabak AG, et al. Patterns of obesity development before the diagnosis of type 2 diabetes: the Whitehall II cohort study. PLoS Med 2014;11:e1001602. doi: 10.1371/journal.pmed.1001602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hofman A, Brusselle GG, Darwish Murad S, et al. The Rotterdam Study: 2016 objectives and design update. Eur J Epidemiol 2015;30:661‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Koller MT, Leening MJ, Wolbers M, et al. Development and validation of a coronary risk prediction model for older U.S. and European persons in the Cardiovascular Health Study and the Rotterdam Study. Ann Intern Med 2012;157:389‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kavousi M, Elias‐Smale S, Rutten JH, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med 2012;156:438‐444. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization . Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation. Geneva: World Health Organization; 2006. [Google Scholar]
- 13. Leening MJG, Kavousi M, Heeringa J, et al. Methods of data collection and definitions of cardiac outcomes in the Rotterdam Study. Eur J Epidemiol 2012;27:173‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Proust‐Lima C, Letenneur L, Jacqmin‐Gadda H. A nonlinear latent class model for joint analysis of multivariate longitudinal data and a binary outcome. Stat Med 2007;26:2229‐2245. [DOI] [PubMed] [Google Scholar]
- 15. Zajacova A, Ailshire J. Body mass trajectories and mortality among older adults: a joint growth mixture‐discrete‐time survival analysis. Gerontologist 2014;54:221‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta‐cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412‐419. [DOI] [PubMed] [Google Scholar]
- 17. Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D'Agostino RB Sr. Prediction of incident diabetes mellitus in middle‐aged adults: the Framingham Offspring Study. Arch Intern Med 2007;167:1068‐1074. [DOI] [PubMed] [Google Scholar]
- 18. D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743‐753. [DOI] [PubMed] [Google Scholar]
- 19. Goff DC Jr, Lloyd‐Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63(25 Pt B):2935‐2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bos MJ, Koudstaal PJ, Hofman A, Ikram MA. Modifiable etiological factors and the burden of stroke from the Rotterdam study: a population‐based cohort study. PLoS Med 2014;11:e1001634. doi: 10.1371/journal.pmed.1001634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walsh EI, Shaw J, Cherbuin N. Trajectories of BMI change impact glucose and insulin metabolism. Nutr Metab Cardiovasc Dis 2018;28:243‐251. [DOI] [PubMed] [Google Scholar]
- 22. Peter RS, Keller F, Klenk J, Concin H, Nagel G. Body mass trajectories, diabetes mellitus, and mortality in a large cohort of Austrian adults. Medicine (Baltimore) 2016;95:e5608. doi: 10.1097/MD.0000000000005608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Villareal DT, Apovian CM, Kushner RF, Klein S; American Society for Nutrition, NAASO, The Obesity Society . Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res 2005;13:1849‐1863. [DOI] [PubMed] [Google Scholar]
- 24. Gaddey HL. Unintentional weight loss in older adults. Am Fam Physician 2014;89:781‐782. [PubMed] [Google Scholar]
- 25. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861‐1867. [DOI] [PubMed] [Google Scholar]
- 26. Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: comparison of laboratory‐based versus non‐laboratory‐based model. Heart 2015;101:377‐383. [DOI] [PubMed] [Google Scholar]
- 27. Rimm EB, Stampfer MJ, Giovannucci E, et al. Body size and fat distribution as predictors of coronary heart disease among middle‐aged and older US men. Am J Epidemiol 1995;141:1117‐1127. [DOI] [PubMed] [Google Scholar]
- 28. Engberg S, Glumer C, Witte DR, Jorgensen T, Borch‐Johnsen K. Differential relationship between physical activity and progression to diabetes by glucose tolerance status: the Inter99 Study. Diabetologia 2010;53:70‐78. [DOI] [PubMed] [Google Scholar]
- 29. Saito T, Watanabe M, Nishida J, et al. Zensharen Study for Prevention of Lifestyle Diseases G. Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Arch Intern Med 2011;171:1352‐1360. [DOI] [PubMed] [Google Scholar]
- 30. Jainandunsing S, Koole HR, van Miert JNI, et al. Transcription factor 7‐like 2 gene links increased in vivo insulin synthesis to type 2 diabetes. EBioMedicine 2018;30:295‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zajacova A, Huzurbazar S, Greenwood M, Nguyen H. Long‐term BMI trajectories and health in older adults: hierarchical clustering of functional curves. J Aging Health 2015;27:1443‐1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


