Abstract
Background
There is growing evidence that technology-based interventions (TBIs) are effective for the treatment of depression. As TBIs are gaining acceptance, a question arises whether good therapeutic alliance, considered a key aspect of psychotherapy, can be established without or with minimal face-to-face contact or rather changes if blended concepts are applied. While therapeutic alliance has been studied extensively in the context of face-to-face therapy, only few studies have reviewed evidence on alliance ratings in TBIs.
Objective
The purpose of this study was to examine therapeutic alliance in technology-based psychological interventions for the treatment of depression.
Methods
We searched Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, PsycINFO, PSYNDEX, CINAHL, clinical trial registers, and sources of grey literature for randomized controlled trials on TBIs in the treatment of adults with unipolar depression. All publications were selected according to prespecified criteria. Data were extracted by two independent reviewers.
Results
A total of eight out of 98 studies (9.5%) included in the review on TBIs for depression considered therapeutic alliance as part of their evaluation. The available data covered eight different treatment conditions, including four stand-alone treatments (face-to-face psychotherapy, email, telephone, and internet program) and four combined treatments (face-to-face psychotherapy plus a smartphone app and an internet program combined with face-to-face psychotherapy, treatment as usual, or email/telephone). On average, patients rated the alliance positively across all groups. Importantly, no relevant group differences regarding therapeutic alliance sum scores were found in any of the studies. Five studies investigated the relationship between patients’ alliance ratings and treatment outcome, revealing mixed results.
Conclusions
Our results suggest that it is possible to establish a positive therapeutic alliance across a variety of different TBIs for depression, but this is based on a small number of studies. Future research needs to determine on what basis therapeutic alliance is formed in settings that do not allow for additional nonverbal cues, perhaps with adapted instruments to measure therapeutic alliance.
Trial Registration
PROSPERO International Prospective Register of Systematic Reviews CRD42016050413; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42016050413)
International Registered Report Identifier (IRRID)
RR2-10.1136/bmjopen-2018-028042
Keywords: therapeutic alliance, depression, technology-based intervention, treatment
Introduction
Background
Globally, over 300 million people (point prevalence in 2015) are estimated to have depression, accounting for 4.4% of the world population [1]. Depression is the greatest contributor for both disability and suicide [1] and is associated with greatly increased health care costs [2]. Treatment of depression with face-to-face psychotherapy has been shown to be effective over the last decades [3]. There is growing evidence that technology-based interventions (TBIs) are also effective for the treatment of depression, with great clinical improvement and recovery after treatment [4-9].
TBIs differ according to various aspects, including the type of technology (eg, computer and smartphone), therapeutic rationale (eg, cognitive behavior therapy and behavioral activation), the clinical phase of depression management (waiting period, acute treatment, and aftercare), and the amount of human support [10]. The degree of support as well as the delivery mode can range from a stand-alone self-administered treatment with no therapist contact at all to a blended treatment with active involvement of a therapist and regular face-to-face meetings.
Besides lowering the threshold to access treatment (eg, providing geographic and time-related flexibility) [11], TBIs, such as online therapy, provide an opportunity to reach people who refuse to seek traditional services, especially those who wish to remain anonymous [11,12].
Considering these aspects as well as the increasing interest in TBIs, a question arises whether adequate therapeutic alliance, considered a key aspect of psychotherapy, can be established without or with minimal face-to-face contact or rather changes when blended concepts are applied.
Therapeutic alliance can be viewed as the “quality of partnership and mutual collaboration between a therapist and client” [13], albeit a generally valid definition of the construct does not exist. According to Bordin [14], good therapeutic alliance is characterized by an agreement between the therapist and patient on the goals of the therapy, the tasks to be performed, and their emotional bond (eg, if the patient feels respected and appreciated by the therapist). Depending on the type of technology, the communication between the therapist and patient can be synchronous (telephone or video conference) or asynchronous (email or web-based program). Moreover, different technologies provide different cues about the therapist, such as visual (video conference) and auditory (telephone) cues, which may influence the emotional bond. This complexity needs to be incorporated when describing findings concerning therapeutic alliance, as pointed out in a recent review by Berger [15].
There are different instruments to assess therapeutic alliance, and the most frequently used instrument is the Working Alliance Inventory (WAI) [16,17], which includes the three aspects of goal, task, and bond. These instruments can be administered at different time points and are based on the patient’s, the therapist’s, or an observer’s point of view.
Positive alliance ratings are good predictors of treatment success in traditional face-to-face psychotherapy, even when controlling for other possible confounders, such as prior symptom change [13,18,19].
While therapeutic alliance has been studied extensively in the context of face-to-face therapy [13], only few studies have reviewed the evidence on alliance ratings in TBIs [17,20]. In a meta-analysis of 295 studies, Flückiger et al [17] recently showed that alliance ratings in internet-based programs are similar to those in face-to-face settings. They further revealed that the effect size of the relationship between alliance and treatment outcome is comparable in TBIs and face-to-face settings. The authors reported that most of the studies investigating alliance in internet-based interventions relied on the WAI. However, this review focused on internet-based interventions only and did not refer specifically to people diagnosed with depression. There are randomized controlled trials (RCTs) addressing therapeutic alliance in TBIs for people with depression [21,22]. However, there is no published systematic review on this topic.
Aim
The purpose of this study was to examine therapeutic alliance in TBIs for the treatment of depression in a systematic review, considering the following research questions: (1) How many of the studies included in the review consider therapeutic alliance in their evaluation? (2) How is therapeutic alliance assessed? (3) How is the quality of therapeutic alliance rated across different interventions? (4) Is there a relationship between therapeutic alliance and treatment outcome?
Methods
Design
This study is part of a preregistered systematic review (PROSPERO registration number: CRD42016050413) on the comparative effectiveness of Technology-based Interventions in different steps of Depression Care (TIDECA). The corresponding protocol has been published [23] and includes more detailed descriptions. This review is in accordance with the standards of the Cochrane Collaboration [24] and is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [25].
Search Strategy
We searched the following key databases: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, PsycINFO, PSYNDEX, and CINAHL. The search was not limited by date, language, or publication status. Supplementary material of the study protocol [23] includes applied search strategies of key databases. We further searched clinical trial registers (ClinicalTrials.gov, International Clinical Trial Registry Platform, and German Clinical Trial Register) and sources of grey literature (Open Grey, Trip Database, ProQuest Dissertations & Theses Abstract and Indexing, and specialized registers of Institute for Scientific Information Web of Science). Additionally, all first authors of the included publications were contacted for supplementary information on further published and unpublished trials and specific study information or the status of on-going studies, which were identified as published study protocols or preregistered trials.
Inclusion and Exclusion Criteria
We applied PICOS categories (Population; Intervention; Comparator; Outcome; Study design) [24,26] to define the inclusion and exclusion criteria for our study. All abstracts were screened according to prespecified criteria. We included studies only if (1) they were cluster RCTs, (2) participants were 18 years or older, (3) participants had a diagnosis of unipolar depression based on a formal classification system, (4) mental or somatic comorbidities were not the main focus of the intervention or study, and (5) the active intervention included a TBI based on an explicit psychotherapeutic theory and aimed to improve depressive symptoms. For more details, refer to the study protocol [23].
Selection Procedure
The selection process is presented in Figure 1. The search yielded at total of 13,077 records after duplicates were removed. Two authors (MK and SL) independently screened the first 100 records for inclusion. Since the interrater reliability for this sample was high (98%), one author (MK) screened the remaining records in the course of the title/abstract screening and the second author (SL) assessed publications labelled as “unclear.” Selected full-text publications (n=802) were subsequently screened for inclusion by two independent reviewers (MK and MD). Discrepancies were resolved by discussion with a third reviewer (SL). A total of 98 publications fulfilled all inclusion criteria for the TIDECA study and were finally screened to determine whether they included data on the therapeutic working alliance relationship. Eight publications were included in this review.
Figure 1.
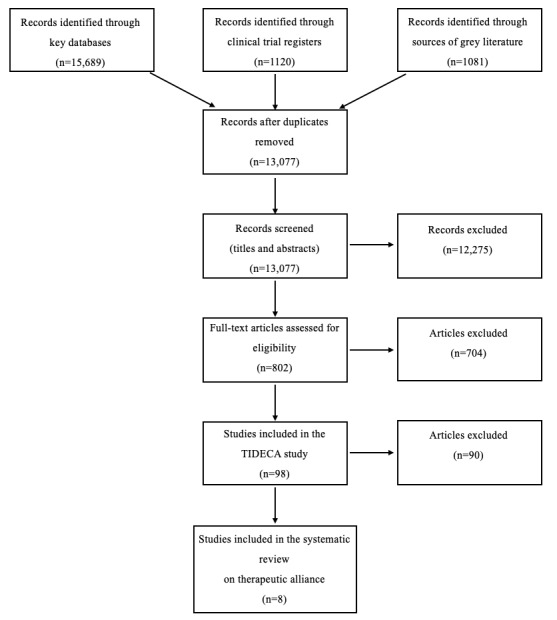
PRISMA flow diagram. TIDECA: Technology-based Interventions in different steps of Depression Care.
Data Extraction
We developed a standardized data collection sheet, which was piloted on three studies. The sheet collected the following data: (1) general data (eg, year of publication), (2) methodological information (including risk of bias assessment), (3) demographic and clinical sample characteristics, (4) classification of the clinical phase of depression management (waiting period, acute treatment, and aftercare), (5) delivery mode (eg, blended treatment), (6) treatment characteristics, (7) sample size and study flow, (8) primary and secondary outcome data, and (9) data on therapeutic alliance, including measuring instrument, rating of therapeutic alliance for all included groups (means, standard deviations, and P values for available group differences), and data on the relationship between therapeutic alliance and treatment outcomes (P values). Data were extracted by two independent reviewers (EW and MK), and inconsistencies were resolved by discussion or by involving a third reviewer (SL).
Data Analysis
Given the heterogeneity of the studies included, qualitative (respectively descriptive) synthesis of the evidence was performed, rather than a meta-analysis.
Descriptive statistics were used to present means, standard deviations, and percentage scores. Standard deviations were derived from standard errors, if not provided otherwise. We decided to focus on alliance ratings after the treatment had started (instead of pretreatment ratings) in order to detect possible group differences based on the different interventions. If several time points after the start of treatment were reported in the studies, we selected the earliest alliance ratings, in line with previous findings showing that therapeutic alliance is established at an early stage of therapy [27]. Given that only a small number of studies provided the therapists’ ratings of therapeutic alliance and all studies provided the patients’ ratings, the results focused on the patients’ ratings.
Quality Appraisal
The risk of bias assessment was evaluated by two independent reviewers (EW and MK) for the included studies according to the Risk of Bias Tool of the Cochrane Handbook for Systematic Reviews [24] (including the domains random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias). In line with a previous operationalization [28], we specified the domain “other bias” using the following three additional categories: insufficient treatment adherence, allegiance bias, and attention bias. Interrater reliability was calculated to be 77%. Discrepancies were resolved by discussions between the reviewers (EW and MK) or by involving a third reviewer (SL).
Protocol Changes
Since the applied literature search was very comprehensive, we did not perform an additional systematic forward and backward reference search.
Results
Study Characteristics
Among the selected studies in the TIDECA review, 9.5% (8/98) considered therapeutic alliance as part of their evaluation. As displayed in Table 1, studies examining therapeutic alliance were published within the last decade and were mainly located in Europe, except for one study from the United States [29-36]. The sample size of these studies ranged from 38 to 325 participants. The technological delivery modes in the intervention groups included email, web-based programs, telephone, and a smartphone app. Waitlists, face-to-face psychotherapy, treatment as usual (TAU) combined with a waitlist, and an active control group with TAU were used as controls. Among the studies, four used a TBI as a stand-alone intervention, three implemented a blended treatment (ie, combining TBIs with face-to-face therapy), and one conducted enhanced stand-alone interventions (ie, combining TBIs with TAU without following a specific concept). The therapeutic rationale of applied TBIs was based on behavioral psychotherapy in all studies. The length of the treatment ranged from 8 to 18 weeks. The qualifications of the therapists varied from MSc students of clinical psychology and licensed psychotherapists to PhD-level psychologists.
Table 1.
Study characteristics.
| Study, authors (publication year) | Study location | Na | Study arms | Delivery mode |
Therapeutic rational of TBIb | Length (weeks) | Qualification of the therapists |
Degree of guidancec |
| Andersson et al (2012) [29] | Sweden | 88 | Email support vs internet program vs waitlist | Stand-alone intervention | CBTd | 8 | MSc students of clinical psychology | Predominantly therapist administered (email) and predominantly self-help (internet) |
| Berger et al (2018) [30] | Germany | 98 | Internet program + F2Fe vs F2F | Blended treatment | CBT | 12 | Licensed psychotherapists | Predominantly therapist administered |
| Lindner et al (2014) [31] | Sweden | 38 | internet program + telephone support vs internet program + email support | Stand-alone intervention | BAf + ACTg | 8 | MSc students of clinical psychology | Predominantly self-help |
| Ly et al (2015) [32] | Sweden | 93 | Smartphone + F2F vs F2F | Blended treatment | BA | 9 (blended) and 10 (control) | MSc students of clinical psychology | Predominantly self-help |
| Meyer et al (2015) [33] | Germany | 163 | Internet program + TAUh vs TAU + waitlist | Enhanced stand-alone intervention | CBT | 13.05 | No therapists involved | Self-administered |
| Steinmann et al (2019) [34] | Germany | 59 | Telephone + F2F + letters vs telephone + F2F | Stand-alone intervention | CBT | 9-13 | Licensed psychotherapists | Predominantly therapist administered |
| Stiles-Shields et al (2014) [35] | USA | 325 | Telephone vs F2F | Stand-alone intervention | CBT | 18 | PhD-level psychologists | Predominantly therapist administered |
| Zwerenz et al (2017) [36] | Germany | 229 | Internet program + TAU vs active control + TAU | Blended treatment | CBT | 12 | No therapists involved | Self-administered |
aN: number of participants randomized.
bTBI: technology-based intervention.
cBased on the study by Newman et al [37].
dCBT: cognitive behavioral therapy.
eF2F: regular face-to-face psychotherapy.
fBA: behavioral activation.
gACT: acceptance and commitment therapy.
hTAU: treatment as usual.
Notable differences were observed with regard to the degree of therapist guidance. Therapists in predominantly self-help interventions focused on providing feedback, validation, reinforcement, and encouragement to continue with the program. In predominantly therapist-administered interventions, the therapy was delivered by therapists, whereas interventions based on self-help did not involve any therapists.
Risk of Bias Assessment
Overall, the risk of bias assessment showed a low risk of bias for selection bias, detection bias, and attrition bias (Figure 2). Given the nature of the studies, blinding of participants and personnel was not possible, thus creating a high risk for performance bias. Selective reporting (reporting bias) was unclear or high in all but one study, mainly due to unexplained or unjustified discrepancies between the protocol or the trial registration and the reported measures. Other sources of bias were unclear or high in all but two studies.
Figure 2.
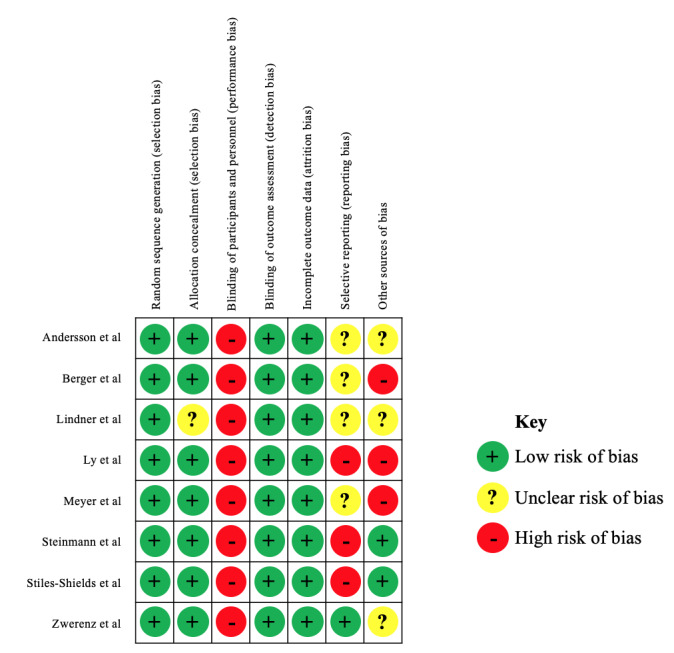
Risk of bias assessment. Other sources involved insufficient treatment adherence, allegiance bias or conflict of interest, and attention bias.
Sample Characteristics
Table 2 provides an overview of the sociodemographic characteristics of the sample. The sample is rather typical for psychotherapeutic studies, with a mean participant age of 43.9 (SD 13.9) years and the majority of participants being female (769/1,093, 70.4%), being employed (554/941, 58.9%), and having a high level of education (672/1034, 65.0%). All studies included only participants who had a clinical diagnosis of depression, except for the study by Meyer et al [33], which had a sample with 84% (137/163) of patients having depression.
Table 2.
Sample sociodemographic characteristics.
| Characteristic | Valuea (N=1093b) | ||
| Age (years) | 43.9 (13.9) | ||
| Sex (females) | 769 (70.4%) | ||
| Occupation |
|
||
|
|
Employed (full and part time) | 554 (58.9%) | |
|
|
Unemployed (including retired and disabled) | 303 (29.3%) | |
|
|
Undergoing training (students and trainees) | 41 (9.0%) | |
| Education |
|
||
|
|
Low educational level (<9 years) | 42 (4.1%) | |
|
|
Middle educational level (9-11 years) | 297 (28.7%) | |
|
|
High educational level (≥12 years) | 672 (65.0%) | |
| Marital status |
|
||
|
|
Married/with partner | 480 (46.4%) | |
|
|
Single/without partner (including divorced and widowed) | 329 (46.4%) | |
aData are presented as mean (SD) or n (%).
bValues refer to the available data. Some studies did not report in line with our subcategories (missing data: occupation, four studies; education, one study; marital status, two studies).
Assessment of Therapeutic Alliance
Table 3 summarizes how therapeutic alliance was assessed in the included studies. Five studies [29-32,35] relied on the WAI in its original format of 36 items (7-point Likert scale) [16], the short form version (WAI-S) with 12 items (7-point Likert scale) [38], or the short form-revised version (WAI-SR) with only positively worded items (5-point Likert scale) [39]. All five studies reported the total score, and three studies [29,30,35] further reported the subscores of the WAI (task, goal, and bond).
Table 3.
Assessment of therapeutic alliance.
| Study, authors (publication year) | Assessment tool | Measures reported | Rater | Time of assessment | Total treatment length |
| Andersson et al (2012) [29] | WAIa | Total score + 3 subscores (task, goal, and bond) | Client | After 3 weeks | 8 weeks |
| Berger et al (2018) [30] | WAI-Short Revised | Total score + 3 subscores (task, goal, and bond) | Client + therapist | After 6/12 weeks | 12 weeks |
| Lindner et al (2014) [31] | WAI-Short Form | Total score | Client | After 2/8/12 weeks | 8 weeks |
| Ly et al (2015) [32] | WAI-Short Form | Total score | Client | Pre-treatment/after 3 weeks | 9 weeks (10 weeks control) |
| Meyer et al (2015) [33] | HAQ-11b | Total score | Client | After 3 weeks | 13.05 weeksc |
| Steinmann et al (2019) [34] | HAQd | Subscore (collaboration or bonding) | Client | Study intake | 9-13 weeks |
| Stiles-Shields et al (2014) [35] | WAI-Short Revised | Total score + 3 subscores (task, goal, and bond) | Client + therapist | At 4/14 weeks | 18 weeks |
| Zwerenz et al (2017) [36] | HAQ | Total score | Client + therapist | Study intake/end of TAUe | 12 weeks |
aWAI: Working Alliance Inventory.
bHAQ-11: 11-item Helping Alliance Questionnaire.
cA period of 3 months was converted to weeks with a factor of 4.35 weeks per month for comparability.
dHAQ: Helping Alliance Questionnaire.
eTAU: treatment as usual.
Two studies relied on the original Helping Alliance Questionnaire [40]; one reported the total score [36], whereas the other reported the subscore for collaboration or bond [34]. One study [33] assessed therapeutic alliance using the 11-item Helping Alliance Questionnaire (HAQ-11) [41], with a 6-point response score. The mean total score of the HAQ-11 was converted to a percentage score that indicated how many participants viewed the alliance as positive.
All studies used the client-rated version of the assessment tools, and three studies [30,35,36] also utilized therapist ratings. While all studies scheduled an early or mid-treatment assessment of the alliance, ranging from 2 to 6 weeks of treatment, some studies included pretreatment and follow-up evaluations as well. Notably, Steinmann et al [34] reported alliance ratings at study intake only, and Zwerenz et al [36] administered the HAQ to measure therapeutic alliance in the TAU arm but not in the TBI arm. Therefore, these data were not considered in the subsequent results.
Ratings of Therapeutic Alliance
The patients’ ratings of therapeutic alliance (between week 2 and 6) are displayed in Table 4. The available data cover eight different treatment conditions, including four stand-alone treatments (face-to-face psychotherapy, email, telephone, and internet program) and four combined treatments (face-to-face psychotherapy plus a smartphone app and an internet program combined with face-to-face psychotherapy, treatment as usual, or email/telephone).
Table 4.
Patients’ ratings for therapeutic alliance.
| Study, authors (publication year) and subscale | Alliance ratingsa, mean (SD) | Group differencesd |
|||||||||
|
|
|
F2Fb | F2F + smartphone | Internet program |
Internet program + F2F | Internet program + TAUc | Internet program + email/phone | Telephone |
|
|
|
| Andersson et al (2012) [29] | |||||||||||
|
|
Total | N/Ae | N/A | 5.25 (0.82) | N/A | N/A | 5.58 (0.82) | N/A | N/A | >.05 | |
|
|
Task | N/A | N/A | 5.19 (0.84) | N/A | N/A | 5.23 (0.83) | N/A | N/A | >.05 | |
|
|
Bond | N/A | N/A | 5.47 (0.97) | N/A | N/A | 5.86 (0.91) | N/A | N/A | >.05 | |
|
|
Goal | N/A | N/A | 5.08 (0.92) | N/A | N/A | 5.63 (0.86) | N/A | N/A | .04f | |
| Berger et al (2018) [30] | |||||||||||
|
|
Total | 3.48 (0.88) | N/A | N/A | 3.64 (0.59) | N/A | N/A | N/A | N/A | >.03g | |
|
|
Task | 3.27 (0.89) | N/A | N/A | 3.42 (0.63) | N/A | N/A | N/A | N/A | >.03g | |
|
|
Bond | 3.60 (1.00) | N/A | N/A | 3.98 (0.64) | N/A | N/A | N/A | N/A | >.03g | |
|
|
Goal | 3.55 (0.99) | N/A | N/A | 3.52 (0.74) | N/A | N/A | N/A | N/A | >.03g | |
| Lindner et al (2014) [31] | |||||||||||
|
|
Total | N/A | N/A | N/A | N/A | N/A | N/A | 58.37 (10.55) | N/A | .6 | |
| Ly et al (2015) [32] | |||||||||||
|
|
Total | 65.7 (11.3) | 63.5 (9.6) | N/A | N/A | N/A | N/A | N/A | N/A | .75-.37 | |
| Meyer et al (2015) [33] | N/A |
|
|||||||||
|
|
Total | N/A | N/A | N/A | N/A | 71.0% | N/A | N/A | N/A | N/A | |
| Stiles-Shields et al (2014) [35] | |||||||||||
|
|
Total | 49.9 (7.57) | N/A | N/A | N/A | N/A | N/A | N/A | 49.7 (7.45) | .78 | |
|
|
Task | 23.3 (4.26) | N/A | N/A | N/A | N/A | N/A | N/A | 23.4 (4.15) | .86 | |
|
|
Bond | 21.9 (5.21) | N/A | N/A | N/A | N/A | N/A | N/A | 22.0 (5.13) | .76 | |
|
|
Goal | 16.5 (2.48) | N/A | N/A | N/A | N/A | N/A | N/A | 15.9 (2.44) | .053 | |
aMeans and standard deviations are displayed, except for the study by Meyer et al, where the percentage of participants rating the alliance as positive is displayed.
bF2F: regular face-to-face psychotherapy.
cTAU: treatment as usual.
dP values based on t tests (Andersson et al and Ly et al), Mann-Whitney U tests (Berger et al), repeated measures analysis of variance (Lindner et al), and least square estimated means (Stiles-Shields et al).
eN/A: not applicable.
fStatistically significant.
gNot statistically significant after Bonferroni correction.
On average, patients rated the alliance positively across all groups. Importantly, no relevant group differences regarding therapeutic alliance sum scores were found in any of the studies. Andersson et al [29] found a significant difference (P=.04) between email-based therapy and the use of a self-help internet program when comparing the subscore goal, with higher scores in the email condition. However, no relevant group differences regarding the other subscores where found.
Berger et al [30] and Stiles-Shields et al [35] further analyzed therapists’ alliance ratings and found no statistically significant group differences between face-to-face psychotherapy and face-to-face psychotherapy combined with an internet program (P>.09) or between face-to-face psychotherapy and telephone treatment (P>.05).
Relationship Between Therapeutic Alliance and Treatment Outcome
Five studies [29,30,32,33,35] investigated the relationship between patients’ alliance ratings and treatment outcome (Table 5).
Table 5.
Relationship between patients’ therapeutic alliance ratings and treatment outcome.
| Study, authors (publication year) | F2Fa | F2F + smartphone | Internet program | Internet program + F2F | Internet program + TAUb | Internet program + email/phone | Telephone | |
| Andersson et al (2012) [29] | N/Ac | N/A | 0d | N/A | N/A | N/A | N/A | N/A |
| Berger et al (2018) [30] | +e | N/A | N/A | 0 | N/A | N/A | N/A | N/A |
| Ly et al (2015) [32] | 0 | + | N/A | N/A | N/A | N/A | N/A | N/A |
| Meyer et al (2015) [33] | N/A | N/A | N/A | N/A | + | N/A | N/A | N/A |
| Stiles-Shields et al (2014) [35] | 0 | N/A | N/A | N/A | N/A | N/A | N/A | 0 |
aF2F: regular face-to-face psychotherapy.
bTAU: treatment as usual.
cN/A: not applicable.
dNo significant relationship between therapeutic alliance and treatment outcome.
eStatistically significant positive relationship between therapeutic alliance and treatment outcome. Significance based on Spearman correlation (Berger et al, P<.01) and mixed effects models (Ly et al, P=.00-.05; Meyer et al, P<.01).
Berger et al [30] found a statistically significant positive association between patients’ alliance ratings at 6 weeks and treatment outcome in the face-to-face psychotherapy group (P<.05) but not in the combined treatment group. They further showed that residual gain scores of depression were predicted by the patients’ alliance rating at 12 weeks in both the regular face-to-face therapy group (P<.05) and combined group (P<.01). The therapists’ ratings at 6 weeks showed no significant association with treatment outcome for either the regular (P=.61) or combined treatment (P=.08). The therapists’ ratings at 12 weeks were significantly associated with treatment outcome in the combined group (P<.05) but not in the regular face-to-face therapy group (P=.60).
Ly et al [32] reported a significant positive association between patients’ working alliance scores and changes in treatment outcome for the blended treatment (P<.05) but not for the regular face-to-face psychotherapy.
Meyer et al [33] found a positive correlation between the patients’ HAQ-11 scores after 3 weeks of treatment with the internet program plus treatment as usual and symptom reduction. This correlation remained significant (P<.02) when controlling for early symptom change.
Anderson et al [29] and Stiles-Shields et al [35] found no relevant relationship between patients’ alliance ratings and treatment outcome.
Discussion
Principal Findings
This study investigated if and how therapeutic alliance ratings were considered in RCTs on different technology-based psychological interventions for depression. Out of the 98 studies included in the TIDECA review, 8 (9.5%) investigated therapeutic alliance. A previous review on e-therapy for different mental health diagnoses found that 1.3% of the included studies considered measures of therapeutic alliance [20]. Notably, the studies included in that review were published between 2002 and 2010, whereas the studies in our review were published between 2012 and 2019. This result may suggest an increased interest in the subject matter; however, it is difficult to directly compare the numbers, since the inclusion criteria of both studies were not identical. Our results showed that the assessment of therapeutic alliance was based on either the WAI or HAQ and that all studies used the patients’ ratings, whereas only three studies reported the therapists’ ratings as well. Furthermore, this study analyzed therapeutic alliance ratings across different interventions considering factors (eg, the degree of therapeutic guidance) that may affect therapeutic alliance, as well as the relationship between therapeutic alliance and treatment outcome.
It was shown that in a face-to-face psychotherapy setting, the therapeutic relationship was not rated differently when adding an internet-based program as an adjunctive treatment tool. Further, a setting with reduced (four instead of 10) face-to-face sessions and a supportive smartphone app also showed no relevant differences compared with a control setting (10 face-to-face sessions and no smartphone app) regarding therapeutic alliance. Replacing all face-to-face sessions with telephone therapy revealed no relevant difference in alliance ratings. This is especially notable as telephone communication eliminates all visual cues.
In guided internet-based programs, no difference regarding therapeutic alliance was found between guidance via email and guidance via telephone. Thus, in this specific setting, vocal cues and synchronous communication, as provided by the telephone, did not result in other therapeutic alliance ratings compared with asynchronous communication and missing vocal cues. Further, guided internet programs showed alliance ratings similar to those for individualized email therapy.
Overall, therapeutic alliance was rated positively, regardless of the type of technology applied. Notably, this also applied to a setting with no therapist contact at all [33], although it is unclear what exactly is reflected by alliance measures between a person and a program.
Our results are based on one study for each treatment comparison; thus, conclusions need to be considered with caution. Further, therapeutic alliance was assessed at different time points, ranging from 2 to 6 weeks after baseline, which adds heterogeneity to the sample. Thus, different alliance ratings may relate to how the relationship was perceived at a specific time point during the treatment, rather than reflecting differences between the interventions themselves. With this in mind, our results suggest that in the context of TBIs for depression, visual and vocal cues, synchronous communication, and physical presence of the therapist are not requirements for developing good therapeutic alliance. This finding is especially interesting in light of the idea that nonverbal behavior is a key factor of relationship formation between patients and therapists [42]. Possibly, there are other factors that compensate for the lack of nonverbal cues, such as more flexibility when accessing therapeutic modules in web-based programs or smartphone apps. Additionally, there are limited studies about the influence of nonverbal cues on the therapeutic relationship [43]; thus, the relevance of these cues for building an adequate alliance is unclear.
We found mixed results concerning the relationship between therapeutic alliance and treatment outcome (eg, alliance ratings in face-to-face therapy were closely related to the treatment outcome in one study but not in another). It has been argued that alliance ratings are not directly related to treatment outcome, but rather represent a third variable, such as early improvement and treatment motivation [44]. This notion was not confirmed by the results of the study by Meyer et al [33], which showed that early alliance ratings predicted treatment outcome, even when controlling for early symptom change.
Strengths and Limitations
Our review was conducted in line with the Cochrane guidelines, and studies were selected according to prespecified criteria, which were previously published in the study protocol, reflecting high methodological standards. The strict application of inclusion and exclusion criteria reduced the overall number of studies considered in this review. All studies were conducted in Western countries, mainly Europe (Sweden and Germany), and one study was conducted in the United States. These countries share similar communication patterns (eg, relying highly on semantic meaning rather than contextual and nonverbal cues) [45]. Thus, it is unclear whether our results can be extended to non-Western countries, especially in the context of TBIs, where visual and vocal cues are eliminated (eg, email and web-based programs).
There are some additional considerations when interpreting our results. First, the majority of the studies relied upon the WAI for the assessment of therapeutic alliance. As recently pointed out [46], this instrument has not been developed and tested for use in technology-based interventions and may need some adaptions to identify setting-specific influences. This may apply to the specific wording of the instrument (eg, program instead of therapist), as well as the content of the questions (eg, the goals of the treatment are usually not discussed in a self-help program). Thus, it is possible that future studies utilizing a tool that is specifically developed and validated in this context may show divergent results.
Second, not all studies specifically reported whether any additional contact between therapists and patients occurred outside of the treatment setting. For example, if a patient is assigned to an email therapy group but meets the therapist during the recruitment or initial assessment process, additional exposure to visual and vocal cues could influence the formation of a therapeutic bond. Thus, we encourage future studies to take this point into consideration by reporting all contacts between therapists and patients.
Third, most patients were recruited via advertisements. Previous research has shown that patients recruited from nonclinical settings have a more positive attitude toward internet interventions for the treatment of depression than patients recruited from clinical settings [47]. Further, therapists that agreed to participate in the studies may have been subject to a similar selection bias. Thus, the results may not be transferrable to clinical practice, where more skeptical individuals (concerning TBIs) are present.
Fourth, only three out of eight studies took the therapists’ perception of therapeutic alliance into consideration. Previous studies have shown that therapists and patients may judge the alliance differently [13]; thus, it would be favorable to include both measures in future studies.
Implications for Clinical Practice and Future Research
As the field may continue to expand and more therapists may consider technology-based treatment options, it is important to further investigate on what basis the alliance is formed in settings that do not allow for additional cues, such as facial expression and tone. For example, in an RCT with several arms, each eliminating a different component of face-to-face communication (eg, visual or auditory cues), researchers could investigate if and how therapeutic alliance is affected. Importantly, these studies should include both the therapists’ and patients’ perspectives. Further, it will be important to replicate the finding that early alliance ratings may predict treatment outcome independently from early symptom change. Such studies will require more frequent measurements of therapeutic alliance, symptom change, and alternative factors that could relate to treatment outcome, such as pretreatment motivation, in order to establish the relation of these aspects. Moreover, research needs to address how personal preferences and attitudes toward TBIs may interact with the formation of a therapeutic alliance, both from the patient’s and therapist’s perspective. Finally, it remains unclear what exactly is measured in settings without any therapist contact at all. Possibly, the alliance between a person and a technology-based program reflects less of the emotional aspect of therapeutic alliance and is more related to how the program matches an individual’s goals and expectations of the tasks required.
Conclusion
This review shows that studies on therapeutic alliance in TBIs for the treatment of depression are still limited, especially regarding therapists’ alliance ratings. Taking into account different degrees of therapeutic guidance, qualifications of therapists, modes of delivery, and types of technologies, the results of this review suggest that a positive therapeutic alliance can be established in TBIs for people with depression.
Acknowledgments
The Federal Ministry of Education and Research (in German: Bundesministerium für Bildung und Forschung; BMBF) funded the systematic review on the comparative effectiveness of Technology-based Interventions in different steps of Depression Care (TIDECA; funding code: 01KG1705, funding period: August 2017 to October 2019). The funding institution had no role in the design of this study and no role during its execution, the analysis and interpretation of data, or the decision to submit the results. The review on therapeutic alliance was conducted as part of a doctoral degree (medicine) and did not receive any additional funding. We thank Mareike Dreier (MD) for her assistance in screening the full-text publications for inclusion.
Abbreviations
- HAQ
Helping Alliance Questionnaire
- HAQ-11
11-item Helping Alliance Questionnaire
- RCT
randomized controlled trial
- TAU
treatment as usual
- TBI
technology-based intervention
- TIDECA
Technology-based Interventions in different steps of Depression Care
- WAI
Working Alliance Inventory
- WAI-S
Working Alliance Inventory short form version
- WAI-SR
Working Alliance Inventory short form-revised version
Footnotes
Conflicts of Interest: None declared.
References
- 1.World Health Organization World Health Organization. 2017. [2019-08-29]. Depression and Other Common Mental Disorders: Global Health Estimates https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/
- 2.Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, Dodel R, Ekman M, Faravelli C, Fratiglioni L, Gannon B, Jones DH, Jennum P, Jordanova A, Jönsson L, Karampampa K, Knapp M, Kobelt G, Kurth T, Lieb R, Linde M, Ljungcrantz C, Maercker A, Melin B, Moscarelli M, Musayev A, Norwood F, Preisig M, Pugliatti M, Rehm J, Salvador-Carulla L, Schlehofer B, Simon R, Steinhausen H, Stovner LJ, Vallat J, Van den Bergh P, den Bergh PV, van Os J, Vos P, Xu W, Wittchen HU, Jönsson B, Olesen J, CDBE2010 Study Group Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011 Oct;21(10):718–79. doi: 10.1016/j.euroneuro.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Cuijpers P, Van Straten A, Warmerdam L, Smits N. Characteristics of effective psychological treatments of depression: a metaregression analysis. Psychother Res. 2008 Mar;18(2):225–36. doi: 10.1080/10503300701442027. [DOI] [PubMed] [Google Scholar]
- 4.Andrews G, Basu A, Cuijpers P, Craske M, McEvoy P, English C, Newby J. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: An updated meta-analysis. J Anxiety Disord. 2018 Apr;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. https://linkinghub.elsevier.com/retrieve/pii/S0887-6185(17)30447-4. [DOI] [PubMed] [Google Scholar]
- 5.Josephine K, Josefine L, Philipp D, David E, Harald B. Internet- and mobile-based depression interventions for people with diagnosed depression: A systematic review and meta-analysis. J Affect Disord. 2017 Dec 01;223:28–40. doi: 10.1016/j.jad.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jun;32(4):329–42. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther. 2009;38(4):196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- 8.Mohr DC, Vella L, Hart S, Heckman T, Simon G. The Effect of Telephone-Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta-Analysis. Clin Psychol (New York) 2008;15(3):243–253. doi: 10.1111/j.1468-2850.2008.00134.x. http://europepmc.org/abstract/MED/21369344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Twomey C, O'Reilly G, Meyer B. Effectiveness of an individually-tailored computerised CBT programme (Deprexis) for depression: A meta-analysis. Psychiatry Res. 2017 Oct;256:371–377. doi: 10.1016/j.psychres.2017.06.081. [DOI] [PubMed] [Google Scholar]
- 10.Ebert DD, Van Daele T, Nordgreen T, Karekla M, Compare A, Zarbo C, Brugnera A, Øverland S, Trebbi G, Jensen KL, Kaehlke F, Baumeister H. Internet- and Mobile-Based Psychological Interventions: Applications, Efficacy, and Potential for Improving Mental Health. European Psychologist. 2018 May;23(2):167–187. doi: 10.1027/1016-9040/a000318. [DOI] [Google Scholar]
- 11.Musiat P, Tarrier N. Collateral outcomes in e-mental health: a systematic review of the evidence for added benefits of computerized cognitive behavior therapy interventions for mental health. Psychological Medicine. 2014 Nov;44(15):3137–3150. doi: 10.1017/s0033291714000245. [DOI] [PubMed] [Google Scholar]
- 12.Townsend L, Gearing RE, Polyanskaya O. Influence of health beliefs and stigma on choosing internet support groups over formal mental health services. Psychiatr Serv. 2012 Apr;63(4):370–6. doi: 10.1176/appi.ps.201100196. [DOI] [PubMed] [Google Scholar]
- 13.Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy (Chic) 2011 Mar;48(1):9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- 14.Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;16(3):252–260. doi: 10.1037/h0085885. [DOI] [Google Scholar]
- 15.Berger T. The therapeutic alliance in internet interventions: A narrative review and suggestions for future research. Psychother Res. 2017 Sep;27(5):511–524. doi: 10.1080/10503307.2015.1119908. [DOI] [PubMed] [Google Scholar]
- 16.Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989 Apr;36(2):223–233. doi: 10.1037/0022-0167.36.2.223. [DOI] [Google Scholar]
- 17.Flückiger C, Del Re AC, Wampold BE, Horvath AO. The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy (Chic) 2018 Dec;55(4):316–340. doi: 10.1037/pst0000172. [DOI] [PubMed] [Google Scholar]
- 18.Falkenström F, Ekeblad A, Holmqvist R. Improvement of the working alliance in one treatment session predicts improvement of depressive symptoms by the next session. J Consult Clin Psychol. 2016 Aug;84(8):738–51. doi: 10.1037/ccp0000119. [DOI] [PubMed] [Google Scholar]
- 19.Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol. 2000 Jun;68(3):438–50. [PubMed] [Google Scholar]
- 20.Sucala M, Schnur JB, Constantino MJ, Miller SJ, Brackman EH, Montgomery GH. The therapeutic relationship in e-therapy for mental health: a systematic review. J Med Internet Res. 2012 Aug 02;14(4):e110. doi: 10.2196/jmir.2084. https://www.jmir.org/2012/4/e110/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Preschl B, Maercker A, Wagner B. The working alliance in a randomized controlled trial comparing online with face-to-face cognitive-behavioral therapy for depression. BMC Psychiatry. 2011 Dec 6;11(1):1–10. doi: 10.1186/1471-244x-11-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beckner V, Vella L, Howard I, Mohr DC. Alliance in two telephone-administered treatments: relationship with depression and health outcomes. J Consult Clin Psychol. 2007 Jun;75(3):508–12. doi: 10.1037/0022-006X.75.3.508. [DOI] [PubMed] [Google Scholar]
- 23.Köhnen M, Kriston L, Härter M, Dirmaier J, Liebherz S. Rationale and design of a systematic review: effectiveness and acceptance of technology-based psychological interventions in different clinical phases of depression management. BMJ Open. 2019 Mar 27;9(3):e028042. doi: 10.1136/bmjopen-2018-028042. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=30918040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JP, Green S. Cochrane Training. 2011. [2019-08-29]. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] https://training.cochrane.org/handbook/archive/v5.1/
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009 Aug 18;151(4):264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 26.Counsell C. Formulating questions and locating primary studies for inclusion in systematic reviews. Ann Intern Med. 1997 Sep 01;127(5):380–7. doi: 10.7326/0003-4819-127-5-199709010-00008. [DOI] [PubMed] [Google Scholar]
- 27.Eaton TT, Abeles N, Gutfreund MJ. Therapeutic alliance and outcome: Impact of treatment length and pretreatment symptomatology. Psychotherapy: Theory, Research, Practice, Training. 1988;25(4):536–542. doi: 10.1037/h0085379. [DOI] [Google Scholar]
- 28.Machmutow K, Meister R, Jansen A, Kriston L, Watzke B, Härter MC, Liebherz S. Comparative effectiveness of continuation and maintenance treatments for persistent depressive disorder in adults. Cochrane Database Syst Rev. 2019 May 20;5:CD012855. doi: 10.1002/14651858.CD012855.pub2. http://europepmc.org/abstract/MED/31106850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andersson G, Paxling B, Wiwe M, Vernmark K, Felix CB, Lundborg L, Furmark T, Cuijpers P, Carlbring P. Therapeutic alliance in guided internet-delivered cognitive behavioural treatment of depression, generalized anxiety disorder and social anxiety disorder. Behav Res Ther. 2012 Sep;50(9):544–50. doi: 10.1016/j.brat.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Berger T, Krieger T, Sude K, Meyer B, Maercker A. Evaluating an e-mental health program ("deprexis") as adjunctive treatment tool in psychotherapy for depression: Results of a pragmatic randomized controlled trial. J Affect Disord. 2018 Feb;227:455–462. doi: 10.1016/j.jad.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 31.Lindner P, Olsson EL, Johnsson A, Dahlin M, Andersson G, Carlbring P. The impact of telephone versus e-mail therapist guidance on treatment outcomes, therapeutic alliance and treatment engagement in Internet-delivered CBT for depression: A randomised pilot trial. Internet Interventions. 2014 Oct;1(4):182–187. doi: 10.1016/j.invent.2014.09.001. [DOI] [Google Scholar]
- 32.Ly KH, Topooco N, Cederlund H, Wallin A, Bergström J, Molander O, Carlbring P, Andersson G. Smartphone-Supported versus Full Behavioural Activation for Depression: A Randomised Controlled Trial. PLoS One. 2015;10(5):e0126559. doi: 10.1371/journal.pone.0126559. http://dx.plos.org/10.1371/journal.pone.0126559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meyer B, Bierbrodt J, Schröder J, Berger T, Beevers CG, Weiss M, Jacob G, Späth C, Andersson G, Lutz W, Hautzinger M, Löwe B, Rose M, Hohagen F, Caspar F, Greiner W, Moritz S, Klein JP. Effects of an Internet intervention (Deprexis) on severe depression symptoms: Randomized controlled trial. Internet Interventions. 2015 Mar;2(1):48–59. doi: 10.1016/j.invent.2014.12.003. [DOI] [Google Scholar]
- 34.Steinmann M, Heddaeus D, Liebherz S, Daubmann A, Härter M, Watzke B. Effectiveness of Telephone-Administered Cognitive-Behavioral Psychotherapy for Depression With Versus Without Additional Letters: A Randomized Controlled Trial. Telemed J E Health. 2020 Mar;26(3):347–353. doi: 10.1089/tmj.2018.0311. [DOI] [PubMed] [Google Scholar]
- 35.Stiles-Shields C, Kwasny MJ, Cai X, Mohr DC. Therapeutic alliance in face-to-face and telephone-administered cognitive behavioral therapy. J Consult Clin Psychol. 2014 Apr;82(2):349–54. doi: 10.1037/a0035554. http://europepmc.org/abstract/MED/24447003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zwerenz R, Becker J, Knickenberg RJ, Siepmann M, Hagen K, Beutel ME. Online Self-Help as an Add-On to Inpatient Psychotherapy: Efficacy of a New Blended Treatment Approach. Psychother Psychosom. 2017;86(6):341–350. doi: 10.1159/000481177. [DOI] [PubMed] [Google Scholar]
- 37.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011 Feb;31(1):89–103. doi: 10.1016/j.cpr.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 38.Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989 Sep;1(3):207–210. doi: 10.1037/1040-3590.1.3.207. [DOI] [Google Scholar]
- 39.Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research. 2006 Jan;16(1):12–25. doi: 10.1080/10503300500352500. [DOI] [Google Scholar]
- 40.Bassler M, Potratz B, Krauthauser H. Der Helping Alliance Questionnaire (HAQ) von Luborsky. Psychotherapeut. 1995;40:23–32. doi: 10.1037/t16583-000. [DOI] [Google Scholar]
- 41.Alexander LB, Luborsky L. The Penn Helping Alliance Scales. In: Greenberg LS, Pinsof WM, editors. Guilford clinical psychology and psychotherapy series. The psychotherapeutic process: A research handbook. New York: Guilford Press; 1986. pp. 325–366. [Google Scholar]
- 42.Hall JA, Harrigan JA, Rosenthal R. Nonverbal behavior in clinician—patient interaction. Applied and Preventive Psychology. 1995 Dec;4(1):21–37. doi: 10.1016/s0962-1849(05)80049-6. [DOI] [Google Scholar]
- 43.Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol. 2011 Jun;79(3):284–95. doi: 10.1037/a0023419. [DOI] [PubMed] [Google Scholar]
- 44.Strunk DR, Cooper AA, Ryan ET, DeRubeis RJ, Hollon SD. The process of change in cognitive therapy for depression when combined with antidepressant medication: Predictors of early intersession symptom gains. J Consult Clin Psychol. 2012 Oct;80(5):730–8. doi: 10.1037/a0029281. http://europepmc.org/abstract/MED/22774791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Qureshi A, Collazos F. The intercultural and interracial therapeutic relationship: challenges and recommendations. Int Rev Psychiatry. 2011;23(1):10–9. doi: 10.3109/09540261.2010.544643. [DOI] [PubMed] [Google Scholar]
- 46.Gómez Penedo JM, Berger T, Grosse Holtforth M, Krieger T, Schröder J, Hohagen F, Meyer B, Moritz S, Klein JP. The Working Alliance Inventory for guided Internet interventions (WAI-I) J Clin Psychol. 2019 Jun 25;:1–32. doi: 10.1002/jclp.22823. [DOI] [PubMed] [Google Scholar]
- 47.Schröder J, Berger T, Meyer B, Lutz W, Hautzinger M, Späth C, Eichenberg C, Klein JP, Moritz S. Attitudes Towards Internet Interventions Among Psychotherapists and Individuals with Mild to Moderate Depression Symptoms. Cogn Ther Res. 2017 Apr 22;41(5):745–756. doi: 10.1007/s10608-017-9850-0. [DOI] [Google Scholar]


