Key Points
Question
What is the incidence of myopic maculopathy in a general Japanese population, and what are the associated risk factors?
Findings
In this cohort study of 2164 patients with a 5-year follow-up, 24 patients developed myopic maculopathy, ie, the 5-year incidence was 1.1%. Aging and longer axial length were associated with the development of myopic maculopathy.
Meaning
These findings indicate that the incidence of myopic maculopathy in the Japanese population is much higher than those reported for other Asian populations and strengthen the evidence that aging and axial length are risk factors for myopic maculopathy.
Abstract
Importance
Myopic maculopathy is a leading cause of irreversible visual impairment worldwide. Moreover, the burden of myopic maculopathy has been expected to increase owing to the rising prevalence of myopia globally. However, there is limited epidemiologic evidence regarding the incidence of and risk factors for myopic maculopathy. This study from Japan, with a relatively high prevalence of myopia, could provide valuable information related to these issues.
Objective
To estimate the incidence of myopic maculopathy and its risk factors in Hisayama in southwestern Japan.
Design, Setting, and Participants
A population-based prospective cohort study in a Japanese community in Hisayama, Japan. The study included a total of 2164 residents 40 years or older who had no myopic maculopathy at the baseline eye examination in 2012 and underwent follow-up eye examinations in 2017.
Main Outcomes and Measures
Incidence of myopic maculopathy. The grades of myopic maculopathy were categorized based on the criteria of the Meta-analysis of Pathologic Myopia Study Group classification system.
Results
The mean (SD) age of the study participants was 62.4 (10.9) years, and the proportion of men was 42.5% (920 participants). In the follow-up examination in 2017, 24 patients developed myopic maculopathy. The 5-year cumulative incidence of myopic maculopathy was 1.1% (95% CI, 0.6-1.5) overall, 1.4% (95% CI, 0.6-2.2) for men, and 0.9% (95% CI, 0.4-1.4) for women. Multiple logistic regression analysis showed that older age (per 1 year; odds ratio [OR], 1.06; 95% CI, 1.01-1.11) and longer axial length (per 1 mm; OR, 2.94; 95% CI, 2.19-3.95) were associated with incident myopic maculopathy.
Conclusions and Relevance
Twenty-four study participants (1%) developed myopic maculopathy during the 5-year study period, which is much higher than the rate in a previous study on a Chinese population. We also confirmed that aging and longer axial length were independent and significant risk factors for myopic maculopathy. These findings should be reviewed among various populations in other parts of the world.
This study estimates the incidence of myopic maculopathy and its risk factors in Hisayama in southwestern Japan.
Introduction
Myopic maculopathy is the leading cause of irreversible visual impairment and blindness for middle-aged and older people around the world.1,2,3 The population-based data from several countries have estimated myopic maculopathy as the first or second most frequent cause of blindness in the Asian population1 and the second to fourth most common cause of low vision/blindness in the European population2 and Latino population.3 The prevalence of myopic maculopathy has been expected to increase globally owing to the rising prevalence of myopia among the world population.4,5 Therefore, the increasing burden of myopic maculopathy is a major public health problem worldwide.
The epidemiologic findings of the incidence of myopic maculopathy and its risk factors would be useful for understanding the natural course of the disease and for planning for the prevention and management of the problem. Several cross-sectional population-based studies have provided valuable information on risk factors associated with the presence of myopic maculopathy.6,7,8,9,10,11,12,13 However, to our knowledge, there has been no population-based prospective study focused on both the incidence rate of myopic maculopathy and its risk factors. Therefore, we conducted a longitudinal study to determine the 5-year incidence of myopic maculopathy and identify the risk factors for myopic maculopathy in a population from southwest Japan.
Methods
Study Population
The Hisayama Study is an ongoing, long-term population-based study on cardiovascular disease and its risk factors in the town of Hisayama, which is adjacent to the Fukuoka metropolitan area in southwest Japan.14 As a part of the study, an epidemiologic study of eye disease among the residents 40 years or older has been under way since 1998.15
In 2012, all the residents 40 years or older at the time of April 1 in the town of Hisayama (n = 4624) were encouraged to participate in the health checkup. Among them, a total of 2948 patients (participation rate, 63.8%) consented to participate in the eye examinations. After excluding 81 patients with myopic maculopathy at baseline, 74 patients who had missing or ungradable photographs in both eyes, and 629 patients who did not participate in the follow-up eye examination in 2017, the remaining 2164 patients (920 men and 1244 women) were enrolled in this study.
Ethical Considerations
This study was approved by the Kyushu University institutional review board for clinical research and was carried out in accordance with the Declaration of Helsinki. The study participants were not offered incentives to participate. Written informed consent was obtained from all participants.
Ophthalmic Examination and Other Myopia-Related Factor Measurements
At the ophthalmic examination, measurements of the objective refraction, axial lengths, and noncontact tonometry and color fundus photography of both eyes were performed for each participant. Objective refraction was measured using an AR-660 automatic refractometer (Nidek). A spherical equivalent (SE) refraction was used to calculate refractive error. The SE refraction was defined as a sphere plus half of the cylindrical refraction. Axial length measurements were performed with noncontact partial coherence laser interferometry (IOL Master; Carl Zeiss). Each participant underwent ophthalmic examination after pupil dilatation with 1.0% tropicamide and 10% phenylephrine. Nonstereoscopic fundus photographs (45°) were taken using a digital fundus camera (TRC NW-200; Topcon Corporation). At the 5-year follow-up eye examination, fundus photographs (45°) were taken using a Topcon digital fundus camera (DRI-OCT Triton; Topcon Corporation). We photographed 1 field, centered at a point midway between the temporal edge of the optic disc and the fovea in both eyes.
Definition of Myopic Maculopathy
According to the Meta-analysis for Pathologic Myopia Study Group classification system, myopic maculopathy is graded into 3 categories: diffuse chorioretinal atrophy (category 2), patchy chorioretinal atrophy (category 3), and macular atrophy (category 4).16 In addition to this categorization, any of 3 additional features, namely, lacquer cracks, myopic choroidal neovascularization, and Fuchs spot, are defined as plus lesion. In this study, myopic maculopathy was diagnosed as the presence of any lesions of category 2, 3, 4, or any plus lesion in either eye based on the grading of the color fundus photographs. All photographs were evaluated independently by 2 experienced ophthalmologists (E.U. and S.H.). When their judgments disagreed, the photographs were reexamined by 3 retinal specialists (E.U., S.H., and M.Y.), and the final judgment was determined after discussion. Graders were blinded to the clinical data of participants in the process of the photograph evaluation. The level of agreement between the graders was moderate (κ statistic: 0.86) to substantial for most features.
Data Collection
Information on smoking habits and alcohol intake was obtained using a standard questionnaire by trained interviewers at the initial examination. Smoking habits and alcohol intake were classified as either current habitual use or not. Patients engaging in sports at least 3 times a week during their leisure time were defined as the regular exercise group. Body height and weight were measured in light clothing without shoes, and the body mass index was calculated as the weight in kilograms divided by the height in meters squared. Blood pressure was measured 3 times after the patients had rested for at least 5 minutes in the sitting position. The average of the 3 measurements was used for the analysis. Hypertension was defined as systolic blood pressure at least 140 mm Hg, diastolic blood pressure at least 90 mm Hg, or current use of antihypertensive medication. For the most participants, blood samples were collected from an antecubital vein after an overnight fast of at least 12 hours, and oral glucose tolerance test was performed with a 75-g glucose equivalent carbohydrate load (Trelan G; Shimizu Pharmaceutical Inc). Plasma glucose level was measured by the hexokinase method. Diabetes was defined as a fasting plasma glucose level at least 126.13 mg/dL (to convert to millimoles per liter, multiply by 0.0555), a 2-hour postloading or random glucose level of at least 200 mg/dL, or use of antidiabetic medication or insulin. Serum total cholesterol level was determined enzymatically using an autoanalyzer (TBA-80S; Toshiba Inc).
Statistical Analysis
Differences in the mean values and frequencies were compared by t test and χ2 test, respectively. The odds ratios (ORs) and their 95% CIs for the development of myopic maculopathy were calculated by using a logistic regression analysis. Essentially, we used data gathered from the right eye for the analysis of axial length but data from the left eye when only the left eye developed myopic maculopathy. In the multivariable-adjusted analysis, the risk factors for myopic maculopathy were selected from the following plausible risk factors for myopic maculopathy by a logistic regression analysis with a backward elimination procedure, in which the variables with P less than .10 were allowed to remain in the relevant model: age, sex, axial length, SE refraction, height, body mass index, systolic blood pressure, diastolic blood pressure, hypertension, diabetes, serum total cholesterol, smoking habits, alcohol intake, and regular exercise. Spherical equivalent refraction was not included in the multivariable-adjusted analysis as a covariate because there is a strong association between SE refraction and axial length. The SAS software package, version 9.4 (SAS Institute), was used to carry out all statistical analyses. A 2-tailed value of P less than .05 was considered statistically significant in all analyses.
Results
The baseline characteristics of the study population by sex are shown in Table 1. The mean (SD) age was 62.4 (10.9) years, and the proportion of men was 42.5% (920 participants). The frequencies of hypertension, diabetes, smoking habits, and alcohol intake, regular exercise, and the mean values of height, body mass index, systolic blood pressure, diastolic blood pressure, and axial length were higher for men than for women, whereas women had the higher mean of serum total cholesterol. There was no significant difference in mean age and SE refraction between sexes.
Table 1. Baseline Characteristics of the Study Population by Sex in the Hisayama Study, 2012-2017a.
| Variables | Mean (SD) | P value | |
|---|---|---|---|
| Men (n = 920) | Women (n = 1244) | ||
| Age, y | 62.8 (10.8) | 62.0 (10.9) | .12 |
| Height, cm | 165.4 (6.5) | 152.9 (6.4) | <.001 |
| BMI | 23.6 (2.9) | 22.8 (3.6) | <.001 |
| Systolic blood pressure, mm Hg | 132.1 (17.7) | 127.1 (18.5) | <.001 |
| Diastolic blood pressure, mm Hg | 79.9 (10.6) | 74.4 (10.8) | <.001 |
| Hypertension, No. (%) | 525 (57.0) | 579 (46.5) | <.001 |
| Diabetes, No. (%) | 207 (22.5) | 159 (12.7) | <.001 |
| Serum total cholesterol, mmol/L | 5.0 (0.7) | 5.4 (0.9) | <.001 |
| Current smoking, No. (%) | 258 (28.0) | 74 (6.0) | <.001 |
| Current drinking, No. (%) | 672 (73.0) | 435 (34.9) | <.001 |
| Regular exercise, No. (%) | 169 (18.4) | 181 (14.6) | .01 |
| Axial length, mma | 24.1 (1.4) | 23.6 (1.2) | <.001 |
| Median (IQR)a | 23.9 (23.2 to 24.7) | 23.3 (22.7 to 24.3) | NA |
| SE refraction, dioptera,b | −0.72 (1.5) | −0.71 (1.7) | .96 |
| Median (IQR)a | −0.38 (−1.38 to 0.13) | −0.43 (−1.25 to 0.13) | NA |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range; NA, not applicable; SE, spherical equivalent.
Data from right eyes.
Excludes 121 patients with history of cataract surgery or unavailable SE refraction data.
The incidence of myopic maculopathy is shown in Table 2. During the 5-year follow-up, 27 eyes of 24 participants developed myopic maculopathy, ie, the unadjusted 5-year incidence of myopic maculopathy was 1.1% (95% CI, 0.6-1.5). The mean (SD) age of participants who developed myopic maculopathy was 61.7 (11.2) years. The 5-year incidence of myopic maculopathy was slightly higher in men (13 participants; 1.4%; 95% CI, 0.6-2.2) than in women (11 participants; 0.9%; 95% CI, 0.4-1.4), although the difference did not reach the statistically significant level (P = .24). With respect to the category of myopic maculopathy, 17 participants presented with diffuse chorioretinal atrophy (category 2) and 7 participants presented with patchy chorioretinal atrophy (category 3). Bilateral involvement was present in 3 participants (12.5%) with myopic maculopathy.
Table 2. Incidence of Myopic Maculopathy in the Hisayama Study, 2012-2017.
| Variable | Mean (SD) | ||
|---|---|---|---|
| Diffuse atrophy | Patchy atrophy | Myopic maculopathy | |
| Total population, No. (%) | 17 (0.8) | 7 (0.3) | 24 (1.1) |
| Age, mean (SD), y | 63.3 (10.1) | 57.6 (13.5) | 61.7 (11.2) |
| Women, No. (%) | 6 (35.3) | 5 (71.4) | 11 (45.8) |
| Bilateral involvement, No. (%) | 0 | 3 (42.9) | 3 (12.5) |
| Axial length, mean (SD), mm | 25.6 (1.0) | 26.9 (1.5) | 26.0 (1.3) |
| SE refraction, mean (SD), dioptera | −2.1 (0.9) | −8.0 (4.2) | −4.3 (3.8) |
Abbreviation: SE, spherical equivalent.
Excludes eyes with history of cataract surgery.
Next, we investigated the risk factors for the development of myopic maculopathy (Table 3). In the age- and sex-adjusted analysis, the ORs for the development of myopic maculopathy increased with longer axial length (per 1 mm: OR, 2.94; 95% CI, 2.19-3.95; P < .001) and SE refraction (per –1 diopter: OR, 1.53; 95% CI, 1.01-2.32; P = .046). In the multivariable-adjusted analysis, older age (per 1 year: OR, 1.06; 95% CI, 1.01-1.11; P = .01) and longer axial length (per 1 mm: OR, 2.94; 95% CI, 2.19-3.95; P < .001) were associated with the development of myopic maculopathy.
Table 3. Age-Adjusted, Sex-Adjusted, and Multivariable-Adjusted ORs of Risk Factors for Myopic Maculopathy in the Hisayama Study, 2012-2017.
| Variable | Myopic maculopathy | |||
|---|---|---|---|---|
| Age- and sex-adjusteda | Multivariable-adjustedb | |||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Age per 1 y | 0.98 (0.94-1.03) | .49 | 1.06 (1.01-1.11) | .01 |
| Men vs women | 1.61 (0.72-3.62) | .24 | 1.41 (0.58-3.42) | .45 |
| Axial length per 1 mm | 2.94 (2.19-3.95) | <.001 | 2.94 (2.19-3.95) | <.001 |
| SE refraction per -1 diopterc | 1.53 (1.01-2.32) | .046 | NA | NA |
| Height per 1 cm | 0.96 (0.91-1.02) | .24 | NA | NA |
| BMI per 1 | 1.02 (0.90-1.15) | .77 | NA | NA |
| Systolic blood pressure per 1 mm Hg | 0.99 (0.97-1.01) | .37 | NA | NA |
| Diastolic blood pressure per 1 mm Hg | 0.99 (0.95-1.03) | .54 | NA | NA |
| Hypertension | 0.88 (0.42-1.86) | .73 | NA | NA |
| Diabetes | 0.47 (0.11-2.10) | .32 | NA | NA |
| Serum total cholesterol per 38.61 mg/dL | 0.91 (0.58-1.44) | .69 | NA | NA |
| Current smoking | 0.59 (0.17-2.11) | .41 | NA | NA |
| Current drinking | 0.91 (0.38-2.20) | .83 | NA | NA |
| Regular exercise | 1.36 (0.50-3.70) | .55 | NA | NA |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); OR, odds ratio; NA, not applicable; SE, spherical equivalent.
SI conversion factor: To convert cholesterol to millimoles per liter, multiply by 0.0259.
Age is sex-adjusted and sex is age-adjusted.
Multivariate regression analysis with a backward elimination procedure.
SE refraction was excluded in the model because there is a strong association between SE refraction and axial length.
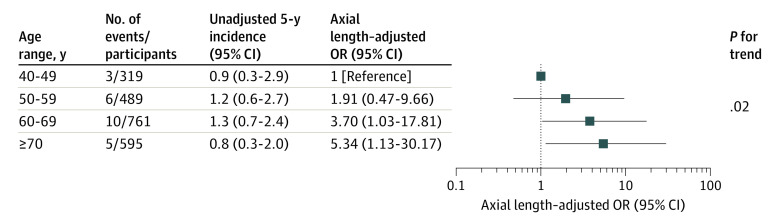
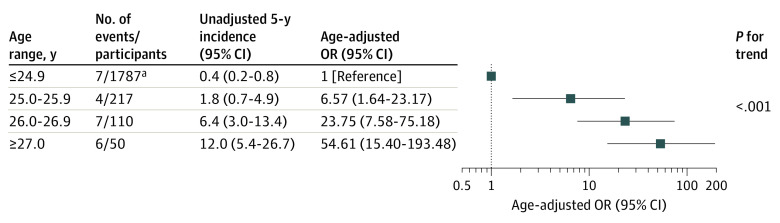
The crude 5-year incidence of myopic maculopathy increased with age and reached a peak in the 60 to 69 years age group and then decreased in the 70 years and older age group. However, the axial length–adjusted ORs for the development of myopic maculopathy increased with elevating age (40-49 years: OR, 1.00; ≥70 years: OR, 5.34; 95% CI, 1.13-30.17; P for trend <.05) (Figure 1). The crude incidence of myopic maculopathy increased with longer axial length (≤24.9 mm: 0.4%; 95% CI, 0.2-0.8; ≥27.0 mm: 12.0%; 95% CI, 5.4-26.7; P for trend <.001). This trend remained after adjustment for age (≤24.9 mm: OR, 1.00; ≥27.0 mm: OR, 54.61; 95% CI, 15.40-193.48; P for trend <.001) (Figure 2).
Figure 1. Odds Ratios (ORs) of Myopic Maculopathy According to the Age Categories.
The axial length-adjusted OR for the development of myopic maculopathy increased with elevating age (P for trend = .02).
Figure 2. Odds Ratios (ORs) of Myopic Maculopathy According to Axial Length Levels.
The age-adjusted OR for the development of myopic maculopathy increased with longer axial length (P for trend <.001).
aAxial length levels of less than 24.0 mm and 24.0 to 24.9 mm were combined because no participant with less than axial length of 24 mm developed myopic maculopathy.
Discussion
We demonstrated that the 5-year cumulative incidence of myopic maculopathy in a general Japanese population 40 years and older was 1.1%. We observed that older age and longer axial length were independently associated with risk. These findings indicated that incidence of myopic maculopathy in the Japanese population is much higher than previously reported for other Asian populations and strengthened the evidence that aging and axial length are risk factors for myopic maculopathy.
Previously, 2 population-based studies examined the incidence of myopic maculopathy in Chinese populations. The Handan Eye Study17 and the Beijing Eye Study6 reported that the 5-year incidences of myopic maculopathy were 0.08% and 0.12%, respectively. These values were much lower than ours. It has been reported that high myopia is more common among Asian populations, especially in Japan.18,19 The difference in the incidence of myopic maculopathy among these studies may be mainly attributable to myopic refractive error, especially severe error, among the Japanese participants. In our study, the prevalence of myopia and high myopia were 45.8% for SE of 0.5 diopters or less and 9.5% for SE of 5.0 diopters or less, which are much higher than the corresponding values in the Handan Eye Study (22.8% and 1.4%) and Beijing Eye Study (21.8% and 3.3%). Other possible explanations are that these findings were attributable to differences in the definition of chorioretinal atrophy across studies. The Meta-analysis for Pathologic Myopia classification, which was used in the Handan Eye Study and our study, includes patchy chorioretinal atrophy, whereas the classification by Steidl and Pruett used in the Beijing Eye Study does not include patchy chorioretinal atrophy. This may be the reason for the higher incidence of myopic maculopathy in our study. In addition, the discrepancy may have been owing to a difference in the year in which the study was conducted. Our study in 2012 used a more recent digital fundus camera (TRC NW-200) than the other studies (Beijing Eye Study in 2001: CR6-45N; Handan Eye Study in 2006: CR2), which presumably resulted in higher image quality. It is possible that myopic maculopathy, especially diffuse chorioretinal atrophy, would be more likely to be detected by the fundus camera used in our study. Further investigations on the ethnic differences in the incidence of myopic maculopathy are warranted.
We found that there was no evidence of significant risk factors associated with the unadjusted risk of myopic maculopathy, but aging was a significant risk factor for developing myopic maculopathy after adjustment for axial length. To estimate the association between age and myopic maculopathy, it is necessary to adjust for axial length as a potential confounding factor because participants born in the older age cohort have a significantly shorter axial length in this study (40-49 years: median 24.2 mm; ≥70 years: 23.2 mm; P for trend <.05) (eFigure in the Supplement). The inverse associations between axial length and age have been observed in several population-based studies20,21 and indicate that this association is probably related to the age cohort effect.22,23 Actually, we previously reported that the axial length extended significantly with time.4 Several epidemiologic studies have shown that aging is a risk factor for the onset of myopic maculopathy.6,7,9 The population-based studies in Singapore have shown that the prevalence of myopic maculopathy is low in children but increases with age.11,24 Histological studies have shown that the density of photo receptors, ganglion cells, retinal pigment epithelium, and optic nerve fibers decreases with age.25,26 Taken together, these findings support the idea that increasing age may contribute to the pathogenesis of myopic maculopathy and confirm the age-related nature of the disease.
This study provides epidemiologic evidence that longer axial length increases the risk of developing myopic maculopathy based on the prospective longitudinal data. These findings are consistent with other cross-sectional studies,7,8,10,11,13,27 which showed that longer axial length was associated with the prevalence of myopic maculopathy. In our study, all characteristics of each category of incident myopic maculopathy had diffuse chorioretinal atrophy without plus lesion. The thinning of the choroid with axial elongation has also been proposed to play an important role in the pathogenesis of diffuse chorioretinal atrophy.28,29,30 A 2019 hospital-based study31 with choroidal thickness measurements reported that choroidal thinning was associated significantly with the progression of diffuse chorioretinal atrophy. Animal experiments have revealed that obliteration of precapillary arterioles or postcapillary venules and fibrotic changes in the choroid may be the underlying cause of the marked thinning of the choroid in myopia.32,33 Therefore, our findings support the idea that axial length has a major effect on the etiology of myopic maculopathy by causing choroidal thinning.
Limitations
Several limitations of our study should also be noted. First, the determination of incidence and classification of myopic chorioretinal atrophy were performed using only fundus photographs, not optical coherence tomography or fluorescein and indocyanine green angiograms, and this could have led to an underestimation of the true incidence. However, the detection of the characteristics of myopic maculopathy, ie, diffuse chorioretinal atrophy, patchy chorioretinal atrophy, and macular atrophy, was based on the examination of the conventional fundus photographs at the baseline and follow-up examinations. Optical coherence tomography images or fluorescein and indocyanine green angiograms would have been useful for the differentiation of plus disease into a topic that was not addressed in the present investigation, ie, lacquer cracks, myopic choroidal neovascularization, and Fuchs spot. Thus, because the diagnosis of myopic maculopathy depended predominantly on the ophthalmoscopic appearance of the fundus on the fundus photographs, we consider that this limitation may not have exerted a meaningful influence on our findings of increase in the incidence of myopic maculopathy. Second, we were unable to perform separate analyses by sex because of the small number of myopic maculopathy events. Further large-scale longitudinal studies will be needed to elucidate this issue. Third, the generalizability of our findings to the entire population of Japan may be limited because this study was conducted in a single town of southwestern Japan. Nevertheless, according to the national census, the age and occupational distributions and the nutrient intake of residents in this town have been almost identical to those of Japan as a whole during the past 50 years according to the national census.14 Moreover, it may be difficult to apply our findings to other ethnicities owing to the different lifestyles and genetic backgrounds. Therefore, it is necessary to investigate the incidence of myopic maculopathy and its risk factors among various populations from other sites of Japan and other countries.
Conclusions
Our results suggest that the incidence of myopic maculopathy is much higher among Japanese individuals compared with other Asian people. We confirmed that older age and longer axial length are risk factors for myopic maculopathy. Because the prevalence of myopic maculopathy has been expected to increase owing to the rising prevalence of myopia globally, the research in not only the Japanese population but also various populations may be needed to identify health services planning in the world.
eFigure. Box and whisker plots showing the age-specific distribution of axial length
References
- 1.Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y; Tajimi Study Group . Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology. 2006;113(8):1354-1362. doi: 10.1016/j.ophtha.2006.04.022 [DOI] [PubMed] [Google Scholar]
- 2.Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol. 1998;116(5):653-658. doi: 10.1001/archopht.116.5.653 [DOI] [PubMed] [Google Scholar]
- 3.Cotter SA, Varma R, Ying-Lai M, Azen SP, Klein R; Los Angeles Latino Eye Study Group . Causes of low vision and blindness in adult Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2006;113(9):1574-1582. doi: 10.1016/j.ophtha.2006.05.002 [DOI] [PubMed] [Google Scholar]
- 4.Ueda E, Yasuda M, Fujiwara K, et al. Trends in the prevalence of myopia and myopic maculopathy in a Japanese population: the Hisayama Study. Invest Ophthalmol Vis Sci. 2019;60(8):2781-2786. doi: 10.1167/iovs.19-26580 [DOI] [PubMed] [Google Scholar]
- 5.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042. doi: 10.1016/j.ophtha.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 6.Liu HH, Xu L, Wang YX, Wang S, You QS, Jonas JB. Prevalence and progression of myopic retinopathy in Chinese adults: the Beijing Eye Study. Ophthalmology. 2010;117(9):1763-1768. doi: 10.1016/j.ophtha.2010.01.020 [DOI] [PubMed] [Google Scholar]
- 7.Asakuma T, Yasuda M, Ninomiya T, et al. Prevalence and risk factors for myopic retinopathy in a Japanese population: the Hisayama Study. Ophthalmology. 2012;119(9):1760-1765. doi: 10.1016/j.ophtha.2012.02.034 [DOI] [PubMed] [Google Scholar]
- 8.Choudhury F, Meuer SM, Klein R, et al. ; Chinese American Eye Study Group . Prevalence and characteristics of myopic degeneration in an adult Chinese American population: the Chinese American Eye study. Am J Ophthalmol. 2018;187:34-42. doi: 10.1016/j.ajo.2017.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109(4):704-711. doi: 10.1016/S0161-6420(01)01024-7 [DOI] [PubMed] [Google Scholar]
- 10.Jonas JB, Nangia V, Gupta R, Bhojwani K, Nangia P, Panda-Jonas S. Prevalence of myopic retinopathy in rural Central India. Acta Ophthalmol. 2017;95(5):e399-e404. doi: 10.1111/aos.13301 [DOI] [PubMed] [Google Scholar]
- 11.Chang L, Pan CW, Ohno-Matsui K, et al. Myopia-related fundus changes in Singapore adults with high myopia. Am J Ophthalmol. 2013;155(6):991-999.e1. doi: 10.1016/j.ajo.2013.01.016 [DOI] [PubMed] [Google Scholar]
- 12.Chen SJ, Cheng CY, Li AF, et al. Prevalence and associated risk factors of myopic maculopathy in elderly Chinese: the Shihpai eye study. Invest Ophthalmol Vis Sci. 2012;53(8):4868-4873. doi: 10.1167/iovs.12-9919 [DOI] [PubMed] [Google Scholar]
- 13.Wong YL, Sabanayagam C, Ding Y, et al. Prevalence, risk factors, and impact of myopic macular degeneration on visual impairment and functioning among adults in Singapore. Invest Ophthalmol Vis Sci. 2018;59(11):4603-4613. doi: 10.1167/iovs.18-24032 [DOI] [PubMed] [Google Scholar]
- 14.Hata J, Ninomiya T, Hirakawa Y, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the Hisayama Study (1961-2009). Circulation. 2013;128(11):1198-1205. doi: 10.1161/CIRCULATIONAHA.113.002424 [DOI] [PubMed] [Google Scholar]
- 15.Yasuda M, Kiyohara Y, Hata Y, et al. Nine-year incidence and risk factors for age-related macular degeneration in a defined Japanese population the Hisayama study. Ophthalmology. 2009;116(11):2135-2140. doi: 10.1016/j.ophtha.2009.04.017 [DOI] [PubMed] [Google Scholar]
- 16.Ohno-Matsui K, Kawasaki R, Jonas JB, et al. ; META-analysis for Pathologic Myopia (META-PM) Study Group . International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159(5):877-83.e7. doi: 10.1016/j.ajo.2015.01.022 [DOI] [PubMed] [Google Scholar]
- 17.Lin C, Li SM, Ohno-Matsui K, et al. ; Handan Eye Study Group . Five-year incidence and progression of myopic maculopathy in a rural Chinese adult population: the Handan Eye Study. Ophthalmic Physiol Opt. 2018;38(3):337-345. doi: 10.1111/opo.12456 [DOI] [PubMed] [Google Scholar]
- 18.Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T; Tajimi Study Group . Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008;115(2):363-370.e3. doi: 10.1016/j.ophtha.2007.03.075 [DOI] [PubMed] [Google Scholar]
- 19.Xu L, Li Y, Wang S, Wang Y, Wang Y, Jonas JB. Characteristics of highly myopic eyes: the Beijing Eye Study. Ophthalmology. 2007;114(1):121-126. doi: 10.1016/j.ophtha.2006.05.071 [DOI] [PubMed] [Google Scholar]
- 20.Warrier S, Wu HM, Newland HS, et al. Ocular biometry and determinants of refractive error in rural Myanmar: the Meiktila Eye Study. Br J Ophthalmol. 2008;92(12):1591-1594. doi: 10.1136/bjo.2008.144477 [DOI] [PubMed] [Google Scholar]
- 21.Fotedar R, Wang JJ, Burlutsky G, et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL Master) in an older white population. Ophthalmology. 2010;117(3):417-423. doi: 10.1016/j.ophtha.2009.07.028 [DOI] [PubMed] [Google Scholar]
- 22.Larsen JS. The sagittal growth of the eye, IV: ultrasonic measurement of the axial length of the eye from birth to puberty. Acta Ophthalmol (Copenh). 1971;49(6):873-886. doi: 10.1111/j.1755-3768.1971.tb05939.x [DOI] [PubMed] [Google Scholar]
- 23.Mutti DO, Mitchell GL, Jones LA, et al. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005;46(9):3074-3080. doi: 10.1167/iovs.04-1040 [DOI] [PubMed] [Google Scholar]
- 24.Samarawickrama C, Mitchell P, Tong L, et al. Myopia-related optic disc and retinal changes in adolescent children from singapore. Ophthalmology. 2011;118(10):2050-2057. doi: 10.1016/j.ophtha.2011.02.040 [DOI] [PubMed] [Google Scholar]
- 25.Panda-Jonas S, Jonas JB, Jakobczyk-Zmija M. Retinal photoreceptor density decreases with age. Ophthalmology. 1995;102(12):1853-1859. doi: 10.1016/S0161-6420(95)30784-1 [DOI] [PubMed] [Google Scholar]
- 26.Gao H, Hollyfield JG. Aging of the human retina: differential loss of neurons and retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 1992;33(1):1-17. doi: 10.1167/iovs.61.1.1 [DOI] [PubMed] [Google Scholar]
- 27.Hashimoto S, Yasuda M, Fujiwara K, et al. Association between axial length and myopic maculopathy: the Hisayama Study. Ophthalmol Retina. 2019;3(10):867-873. doi: 10.1016/j.oret.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 28.Ikuno Y, Tano Y. Retinal and choroidal biometry in highly myopic eyes with spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2009;50(8):3876-3880. doi: 10.1167/iovs.08-3325 [DOI] [PubMed] [Google Scholar]
- 29.Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009;148(3):445-450. doi: 10.1016/j.ajo.2009.04.029 [DOI] [PubMed] [Google Scholar]
- 30.Wang NK, Lai CC, Chu HY, et al. Classification of early dry-type myopic maculopathy with macular choroidal thickness. Am J Ophthalmol. 2012;153(4):669-677, 677.e1-677.e2. doi: 10.1016/j.ajo.2011.08.039 [DOI] [PubMed] [Google Scholar]
- 31.Fang Y, Du R, Nagaoka N, et al. OCT-based diagnostic criteria for different stages of myopic maculopathy. Ophthalmology. 2019;126(7):1018-1032. doi: 10.1016/j.ophtha.2019.01.012 [DOI] [PubMed] [Google Scholar]
- 32.Shih YF, Fitzgerald ME, Norton TT, Gamlin PD, Hodos W, Reiner A. Reduction in choroidal blood flow occurs in chicks wearing goggles that induce eye growth toward myopia. Curr Eye Res. 1993;12(3):219-227. doi: 10.3109/02713689308999467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moriyama M, Ohno-Matsui K, Futagami S, et al. Morphology and long-term changes of choroidal vascular structure in highly myopic eyes with and without posterior staphyloma. Ophthalmology. 2007;114(9):1755-1762. doi: 10.1016/j.ophtha.2006.11.034 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Box and whisker plots showing the age-specific distribution of axial length