Abstract
Background and aims
The associations between traumatic events, substance use and perceived discrimination have been rarely studied among migrants in host countries. We examined whether pre‐migration potentially traumatic experiences (PTEs) or perceived discrimination (PD) are associated with substance use among migrants with voluntary (Russians) and forced (Kurds) migration backgrounds.
Design
Cross‐sectional interview and health examination data from the Finnish Migrant Health and Wellbeing Study were used. The target sample (n = 1000 for each group) was drawn from the national population register using stratified random sampling by participants’ country of birth and native language.
Setting
Population‐based data were collected from six cities in Finland during 2010–12.
Participants
The participation rates were 68% (Russians) and 59% (Kurds). The analytical sample size varied (Russians n = 442–687, Kurds n = 459–613), as some participants completed only interview, health examination or short interview. The majority of Kurds had a refugee background (75%) while Russians had mainly migrated for other reasons (99%).
Measurements
The three main outcomes were self‐reported binge drinking, daily smoking and life‐time cannabis use. PTEs and PD were self‐reported in the interview. Socio‐demographic background, migration‐related factors and current affective symptoms were adjusted for.
Findings
Among Kurds, PTEs were associated with binge drinking [adjusted odds ratio (aOR) = 2.65, 95% confidence interval (CI) = 1.30–5.42] and PD was associated with life‐time cannabis use (aOR = 3.89, 95% CI = 1.38–10.97) after adjusting for contextual factors. Among Russians, PTEs were associated with life‐time cannabis use adjusting for contextual factors (aOR = 2.17, 95% CI = 1.12–4.18).
Conclusions
In Finland, pre‐migration traumatic experiences appear to be associated with life‐time cannabis use among the Russian migrant population (voluntary migration) and binge drinking among the Kurdish migrant population (forced migration). Perceived discrimination in Finland appears to be associated with life‐time cannabis use among Kurdish migrants.
Keywords: Alcohol, binge drinking, cannabis, daily smoking, discrimination, forced migration, migrant, substance use, tobacco, traumatic experiences
Introduction
Knowledge concerning substance use and associating risk factors among forced migrant populations remains limited 1, 2, 3, 4, despite the increasing number of people on the move globally 5. The prevalence of substance use depends on the migrant population under study and measures of substance use employed 6, 7, 8, 9, 10, 11, 12, 13, 14, 15. Variations in cultures, social acceptability of substance use, availability of substances and gender may contribute to migrants’ substance use habits, which may change over time in new host countries 14, 16, 17, 18, 19. For example, alcohol use is widely prohibited in the Middle East and North Africa 20, 21, 22, 23, 24, while in eastern Europe and Nordic countries, including Finland, a high number of drinks consumed per drinking occasion is common 25, 26 and intoxication by alcohol is relatively accepted as a drinking habit 27.
Research on conflict‐affected populations, i.e. general populations and internal migrants, has indicated associations between traumatic experiences and alcohol use disorder (AUD) 28, 29, 30, nicotine dependence 31, cannabis use disorder 32 and other illicit drug abuse 31, 33. Among migrants, substance use may be influenced by pre‐migration traumatic experiences, duration of displacement, hardship and discrimination in new host countries 14, 34, 35. Among forced migrants, traumatic experiences may also have a negative impact on health and mental health 36, 37, 38. However, knowledge concerning substance use and traumatic experiences among migrant populations is scarce 2, 4, 39, and we found no previous studies on the association between traumatic pre‐migration experiences and substance use among migrants in their new host countries.
A growing body of literature demonstrates the harmful effects of discrimination on the mental health of migrant and general populations 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51. Previous studies, mostly conducted among general populations in North America, have shown associations between perceived discrimination and alcohol use 52, 53, 54, 55, 56, 57, 58, 59, smoking 53, 54, 59, 60, 61, 62 and illicit substance use 54, 57, 58, 63. So far, only Visser et al. 64 from the Netherlands have studied substance use and perceived discrimination among migrants in Europe. They reported that perceived discrimination was associated with substance use among Ghanaian and African Surinamese but not among South Asian Surinamese, Turkish or Moroccan participants. Nevertheless, information on substance use and discrimination among migrants, particularly in the European context, remains very limited.
Aim
We aim to study associations between substance use (binge drinking, daily smoking and life‐time cannabis use) and (i) exposure to pre‐migration potentially traumatic experiences (PTEs) and (ii) perceived discrimination (PD) in the host country (Finland). Socio‐demographic factors, migration‐related factors and current affective symptoms are considered confounding variables.
Data from a population‐based study 65 are analysed separately for two migrant populations: the Russians and the Kurds. These groups have dissimilar reasons for migration: Russians have migrated voluntarily, whereas Kurds are mainly a forced migrant population group 65. These groups also have divergent substance use habits in the new host country 66. For example, in our previous study 11% of Russian men and 51% of Kurdish men reported abstaining from alcohol use 66. Furthermore, we have indicated that comorbid affective symptoms are more common among substance using Kurds in particular 67. This study will expand previous knowledge on pre‐migration traumatic experiences, post‐migration perceived discrimination and substance use 50, 68.
Methods
Design
The data originate from a comprehensive cross‐sectional survey, the Finnish Migrant Health and Wellbeing Study (Maamu) 65, carried out by the Finnish National Institute for Health and Welfare (THL) during 2010–12 among Russian, Somali and Kurdish origin populations. A detailed description of the Maamu Study has been reported elsewhere 65, 69 . As the prevalence of substance use among Somali participants was very low 66, further analyses of the present study could not be performed among them (binge drinking prevalence 1%, n = 2; daily smoking prevalence 5%, n = 30; life‐time cannabis use 0%, n = 0).
The Maamu Study consisted of a health examination and a structured face‐to‐face interview, conducted by trained bilingual field staff in the participants’ native language or in Finnish. A short interview including the most essential items of the interview and health examination was offered to those who were unable to participate in the interview and health examination, and it was conducted face‐to‐face, by telephone or mail. Ethical approval was granted by the Coordinating Ethics Committee of the Hospital District of Helsinki and Uusimaa. Each participant gave their written informed consent prior to participation.
Participants
The Maamu Study sample is a stratified random sample consisting of 3000 migrants (1 thousand from each of the defined groups) aged 18–64 years from six cities in Finland. The sample was drawn from the National Population Register. The sample did not include individuals resident in Finland for less than 1 year, living in reception centres or still seeking for asylum. Russian origin was defined by the native language being Russian or Finnish and the country of birth being Russia or the Former Soviet Union. Kurdish origin was defined by the native language being Kurdish and the country of birth being Iraq or Iran. Russian and Kurdish populations were selected based on being among the largest migrant groups in Finland and their prominence in the international context of migration 65. The participation rate was 68 % for the Russian and 59 % for the Kurdish migrants. The majority of the Russian participants (99%) had migrated due to personal reasons (e.g. work, family ties) representing voluntary migration, whereas the majority of the Kurdish participants had arrived as asylum seekers or quota refugees representing forced migration (75%).
Measures
Outcome variables
Binge drinking, daily smoking and life‐time cannabis use were defined as primary outcome variables.
Binge drinking, i.e. having six or more alcohol units on one occasion, was selected to indicate a risky drinking occasion and a hazardous pattern of alcohol use 70, 71, 72. Binge drinking was measured with the third question from the Alcohol Use Disorder Identification Test for Consumption (AUDIT‐C) 73, 74, 75, 76: ‘How often do you have six or more alcohol units on one occasion?’, with response categories ‘never’, ‘less than monthly’, ‘monthly’, ‘weekly’ and ‘daily or almost daily’. The variable was dichotomized: ‘no binge drinking’/‘yes’, i.e. binge drinking less than monthly or more often. AUDIT‐C screens for risky drinking with three items 73, 74, 75. The total score was used as a continuous variable and as an outcome measure in post‐hoc analyses.
Daily smoking was asked as: ‘Do you smoke currently (cigarettes, cigars, pipe)?’, with response categories ‘yes, daily’, ‘yes, occasionally’ and ‘not at all’. The variable was dichotomized: ‘no’ included ‘not at all’ and ‘yes, occasionally’; ‘yes’ included ‘yes, daily’. Daily smoking indicates a frequent and more hazardous smoking pattern. The answer ‘yes, occasionally’ was pooled with ‘not at all’, as detailed information on frequency or quantity of occasional smoking was not available.
Life‐time cannabis use was asked as: ‘Have you ever used cannabis?’, with responses ‘no’/‘yes’.
Explanatory variables
Pre‐migration potentially traumatic experiences (PTEs) were measured with items: ‘Have you experienced the following unpleasant events in your former home country? (1) Experienced a combat situation in war? (2) Been the victim of a natural disaster, e.g. earthquake, flood or fire? (3) Witnessed violent death or serious injury? (4) Experienced sexual violence? (5) Been a target of a serious physical attack or harm? (6) Been detained or kidnapped? (7) Been tortured? (8) Experienced some other form of horrible violence?’, with answer options ‘yes’/‘no’ 68. These items were selected from the Harvard Trauma Questionnaire (HTQ), a validated instrument for measuring exposure to severe traumatic events 68, 77, 78, 79, 80, 81. A dichotomous combination variable was formed: ‘yes’ included answer ‘yes’ to any of the eight items 68.
Perceived discrimination (PD) was measured with four items from the Everyday Discrimination Scale (EDS) 82. The selected items were: (1) ‘You are not treated as politely as other people’; (2) ‘You are not treated as respectfully as other people’; (3) ‘You have been called names or insulted verbally’; and (4) ‘You have been threatened or harassed’. The answer categories were ‘yes’/‘no’. A dichotomous combination variable was formed: ‘yes’ included response ‘yes’ to any of the four items 51.
Confounding variables
Affective symptoms are defined here as a mixture of depressive and anxiety symptoms, and measured with the validated and widely used Hopkins Symptoms Checklist‐25 (HSCL‐25) 79, 83, 84, 85, 86, 87. It includes 25 items on depressive and anxiety symptoms during the preceding week, rated on a scale from 1, ‘not at all bothered’ to 4, ‘extremely bothered’. Mean scores for the HSCL‐25 were calculated, and a cut‐off point of 1.75 was applied to create a dichotomized variable for clinically significant symptoms (no/yes), as previously used 50, 67, 79, 88, 89, 90.
Socio‐demographic factors examined were gender, age (as a continuous variable), marital status (married or cohabitating versus other), level of basic education (secondary school or less versus higher), employment status (employed versus other) and a subjective evaluation of one's economic situation (satisfactory versus unsatisfactory).
Migration‐related variables included were age at migration to Finland (as a continuous variable), self‐reported language proficiency in one of the official languages of Finland (good versus fair or less) and refugee background (arrival to Finland as a quota refugee or an asylum seeker versus other reasons for migration).
Analyses
The associations of potentially traumatic experiences (PTEs) and perceived discrimination (PD) and substance use were examined separately for both subpopulations using multivariate logistic regression analysis. The analyses were not pre‐registered. Confounding variables were added to the multivariate models stepwise in blocks. The variables were selected to the multivariate models based on association with substance use in cross‐tabulation (P < 0.1), previous results 66 and identified from literature 50, 51, 68. Logistic regression was used in all analyses and the sampling design was taken into account. Finite population correction was applied because of the inclusion of a significant proportion of the total population in the sample 91. Predictive margins were used in calculation of the age‐ and gender‐adjusted prevalence rates of descriptive statistics 92. The odds ratios (OR), adjusted odds ratios (aOR), beta coefficients (β) and 95% confidence intervals (CI) are reported as age‐adjusted figures. A p‐value < 0.05 was considered statistically significant.
Post‐hoc analyses, suggested by reviewers, were performed using the AUDIT‐C score as a continuous outcome variable in regression analyses, using pooled data including both the Kurds and the Russians with age and gender as covariates. Interactions between migrant group and PTEs/PD and gender and PTEs/PD were analysed.
All analyses included complete cases in each model, and missing data were not included in the analytical sample. The analytical sample size varied from analysis to analysis (Russians n = 442–687, Kurds n = 459–613), as some participants completed only the interview, the health examination or the short interview. Inverse probability weights 93 determined by main predictive factors of non‐response (migrant group, gender, age, municipality and marital status) were used to reduce the effects of missing data (Russian 30%, Kurdish 37%). Separate analyses weights were calculated and used for items included in the short interview, the interview and the health examination.
The linearity of continuous independent variables (age and age at migration) were examined with fractional polynomials 94. The effects were linear, except for the association of cannabis use and age among Russians, where the power of 2 was found significant. Thus, a cubic transformation of age was used in the cannabis use models of Russians.
Statistical significance was assessed with the Satterthwaite‐adjusted F‐statistic. The statistical analyses were performed with SAS version 9.3, SUDAAN version 11.0.1 and Stata version 15 software versions.
Results
Descriptive statistics highlighting the divergent backgrounds of the study populations are reported in Table 1. The analyses were not pre‐registered and the results should be considered exploratory.
Table 1.
Descriptive statistics on the study population.
| Russian % (95% CI) | n | Kurdish % (95% CI) | n | P‐valuea | |
|---|---|---|---|---|---|
| Gender: men | 37 (33.0–40.9) | 687 | 56 (52.2–59.4) | 613 | < 0.001 |
| Mean ageb | 39 (38.4–40.5) | 687 | 35 (34.1–35.7) | 613 | < 0.001 |
| Mean age at migrationb | 27 (26.2–28.4) | 687 | 24 (23.2–24.7) | 613 | < 0.001 |
| Migration background: refugee | 1 (0.3–3.1) | 519 | 75 (71.1–78.2) | 508 | < 0.001 |
| Marital status: married or cohabiting | 61 (56.5–64.6) | 687 | 66 (62.0–69.1) | 612 | 0.066 |
| Education: high school graduate | 77 (73.5–80.4) | 670 | 43 (39.4–46.6) | 606 | < 0.001 |
| Employment: employed | 55 (50.5–56.8) | 686 | 40 (36.4–43.5) | 610 | < 0.001 |
| Economic situation: unsatisfactory | 48 (43.4–52.9) | 527 | 66 (62.1–69.9) | 500 | < 0.001 |
| Language proficiency: fair or less | 42 (37.9–47.2) | 528 | 51 (47.5–55.7) | 507 | 0.004 |
| Potentially traumatic experiences (PTEs)c | 24 (19.9–27.9) | 529 | 77 (73.0–80.0) | 507 | < 0.001 |
| Perceived discrimination (PD)d | 41 (36.7–44.8) | 685 | 39 (35.1–42.2) | 613 | 0.424 |
| Binge drinkingc | 42 (37.0–46.6) | 526 | 18 (15.1–21.5) | 508 | < 0.001 |
| Daily smokingd | 16 (13.2–19.2) | 687 | 19 (16.2–22.0) | 613 | 0.173 |
| Life‐time cannabis usec | 17 (13.7–21.2) | 528 | 4 (2.6–6.2) | 507 | < 0.001 |
| Affective symptomsa | 18 (14.7–22.5) | 459 | 35 (30.9–38.7) | 496 | < 0.001 |
Comparison between Russian and Kurdish migrants.
Age presented as mean, not percentage.
Collected in the interview.
Collected in the interview and short interview.
Collected in health examination primarily as self‐administered questionnaire or by interview with the small number of illiterate participants. CI = confidence interval.
The comparison between potentially traumatic experiences (PTEs) versus no PTEs in relation to prevalence of substance use is illustrated in Fig. 1. The associations between PTEs and substance use are reported in Table 2. Among Kurds, PTEs were associated with binge drinking, and the association remained significant after adjusting for contextual factors (aOR = 2.65, 95% CI = 1.30–5.42) and affective symptoms (aOR = 2.35, 95% CI = 1.17–4.73). A similar association was observed when alcohol use was measured using AUDIT‐C score as a continuous variable (β = 0.51, 95% CI = 0.13–0.89). Among Russians, PTEs increased the odds for daily smoking (OR = 1.88, 95% CI = 1.06–3.33) and life‐time cannabis use (OR = 2.08, 95% CI = 1.11–3.92), but only the findings on life‐time cannabis use remained significant after adjusting for contextual factors (aOR = 2.17, 95% CI = 1.12–4.18).
Figure 1.
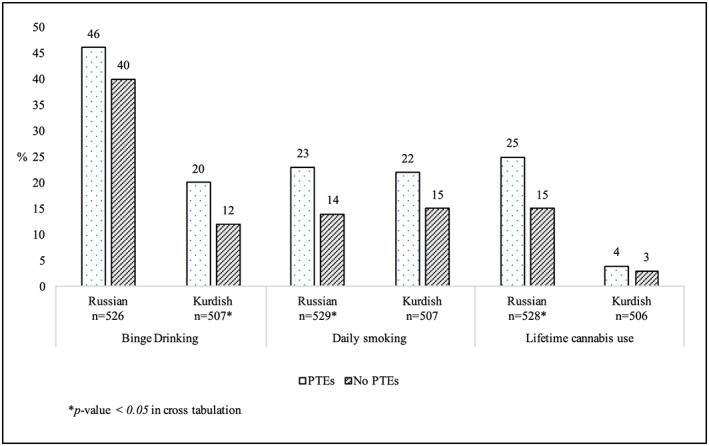
Prevalence of substance use among participants with pre‐migration potentially traumatic experiences (PTEs) versus no PTEs [Colour figure can be viewed at wileyonlinelibrary.com]
Table 2.
The associations between potentially traumatic experiences (PTEs) and substance use.
| Russian | Kurdish | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P‐value | n | OR | 95% CI | P‐value | n | ||
| Binge drinking | |||||||||
| Model 1 | 1.30 | 0.78–2.17 | 0.315 | 526 | 2.05 | 1.08–3.89 | 0.029 | 507 | |
| Model 2 | 1.28 | 0.76–2.14 | 0.352 | 523 | 2.37 | 1.24–4.56 | 0.009 | 496 | |
| Model 3 | 1.25 | 0.75–2.08 | 0.397 | 523 | 2.65 | 1.30–5.42 | 0.008 | 496 | |
| Model 4 | 1.02 | 0.59–1.78 | 0.993 | 443 | 2.35 | 1.17–4.73 | 0.016 | 460 | |
| AUDIT‐C scorea | b | b | |||||||
| Model 1 | 0.44 | −0.015‐0.89 | 0.058 | 521 | 0.53 | 0.14–0.93 | 0.008 | 495 | |
| Model 2 | 0.44 | −0.018‐0.89 | 0.060 | 521 | 0.52 | 0.14–0.89 | 0.007 | 495 | |
| Model 3 | 0.44 | −0.020‐0.90 | 0.061 | 521 | 0.51 | 0.13–0.89 | 0.009 | 495 | |
| Model 4 | 0.25 | −0.27‐0.77 | 0.348 | 442 | 0.45 | 0.056–0.84 | 0.025 | 459 | |
| Daily smoking | |||||||||
| Model 1 | 1.88 | 1.06–3.33 | 0.030 | 529 | 1.73 | 0.91–3.29 | 0.097 | 507 | |
| Model 2 | 1.70 | 0.96–3.01 | 0.071 | 526 | 1.56 | 0.81–2.99 | 0.185 | 496 | |
| Model 3 | 1.64 | 0.93–2.89 | 0.088 | 526 | 1.73 | 0.90–3.35 | 0.103 | 496 | |
| Model 4 | 1.55 | 0.84–2.88 | 0.163 | 449 | 1.46 | 0.73–2.92 | 0.278 | 496 | |
| Life‐time cannabis use | |||||||||
| Model 1 | 2.08 | 1.11–3.92 | 0.023 | 528 | 1.41 | 0.47–4.19 | 0.540 | 506 | |
| Model 2 | 2.17 | 1.13–4.16 | 0.020 | 525 | 1.26 | 0.43–3.71 | 0.679 | 495 | |
| Model 3 | 2.17 | 1.12–4.18 | 0.021 | 525 | 1.40 | 0.39–4.97 | 0.604 | 495 | |
| Model 4 | 1.81 | 0.90–3.61 | 0.094 | 445 | 0.85 | 0.28–2.54 | 0.769 | 459 | |
Statistically significant findings (P < 0.05) shown in bold type.
Model 1: univariate logistic regression, adjusted for age and gender.
Model 2: adjusted for age, gender, socio‐demographic background (marital status, education, employment, economic situation).
Model 3: adjusted for age, gender, socio‐demographic background (marital status, education, employment, economic situation) and migration related variables (refugee status (for Kurdish), age at migration, language proficiency).
Model 4: adjusted for age, gender, current affective symptoms (HSCL‐25 > 1.75)
AUDIT‐C total score as a continuous variable;
beta coefficient (β) instead of OR. OR =odds ratio; CI = confidence interval; HSCL = Hopkins Symptoms Checklist.
The comparison between perceived discrimination (PD) versus no PD in relation to prevalence of substance use is illustrated in Fig. 2, and the associations between PD and substance use are reported in Table 3. Among Kurds, PD was associated with life‐time cannabis use (OR = 3.74, 95% CI = 1.28–10.91), remaining significant when both contextual factors and affective symptoms were adjusted for (aOR = 3.52, 95% CI = 1.16–10.71). PD also correlated with higher AUDIT‐C score among Kurds (β = 0.46, 95% CI = 0.12–0.79). Among Russians, PD increased the odds for daily smoking (OR = 1.60, 95% CI = 1.01–2.54), but adjusting for contextual factors and affective symptoms reduced the association to non‐significant.
Figure 2.
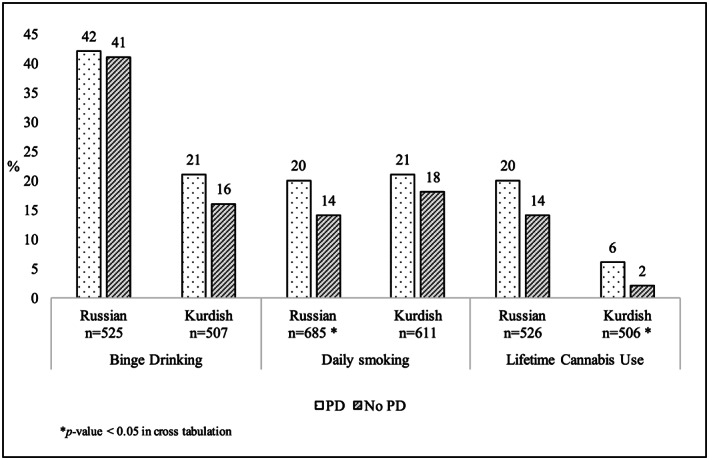
Prevalence of substance use among participants with post‐migration perceived discrimination (PD) versus no PD
Table 3.
The associations between perceived discrimination (PD) and substance use.
| Russian | Kurdish | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P‐value | n | OR | 95% CI | P‐value | n | ||
| Binge drinking | |||||||||
| Model 1 | 1.07 | 0.69–1.66 | 0.775 | 525 | 1.53 | 0.96–2.44 | 0.073 | 507 | |
| Model 2 | 0.96 | 0.61–1.51 | 0.864 | 522 | 1.59 | 0.96–2.64 | 0.073 | 496 | |
| Model 3 | 0.92 | 0.59–1.45 | 0.731 | 522 | 1.63 | 0.98–2.70 | 0.059 | 496 | |
| Model 4 | 1.15 | 0.72–1.84 | 0.557 | 442 | 1.45 | 0.89–2.35 | 0.137 | 460 | |
| AUDIT‐C scorea | b | b | |||||||
| Model 1 | −0.17 | −0.55‐0.22 | 0.399 | 520 | 0.42 | 0.088–0.75 | 0.013 | 495 | |
| Model 2 | −0.17 | −0.56‐0.22 | 0.388 | 520 | 0.41 | 0.085–0.74 | 0.014 | 495 | |
| Model 3 | −0.20 | −0.60‐0.20 | 0.325 | 520 | 0.46 | 0.12–0.79 | 0.007 | 495 | |
| Model 4 | −0.15 | −0.57‐0.28 | 0.493 | 442 | 0.36 | 0.020–0.70 | 0.038 | 470 | |
| Daily smoking | |||||||||
| Model 1 | 1.60 | 1.01–2.54 | 0.046 | 685 | 1.27 | 0.85–1.91 | 0.247 | 611 | |
| Model 2 | 1.31 | 0.75–2.27 | 0.339 | 524 | 1.32 | 0.83–2.08 | 0.241 | 496 | |
| Model 3 | 1.23 | 0.71–2.12 | 0.462 | 524 | 1.36 | 0.86–2.14 | 0.190 | 496 | |
| Model 4 | 1.63 | 0.91–2.93 | 0.100 | 450 | 1.20 | 0.75–1.91 | 0.454 | 460 | |
| Life‐time cannabis use | |||||||||
| Model 1 | 1.66 | 0.94–2.96 | 0.083 | 526 | 3.74 | 1.28–10.91 | 0.016 | 506 | |
| Model 2 | 1.68 | 0.94–3.00 | 0.079 | 523 | 3.90 | 1.37–11.12 | 0.011 | 495 | |
| Model 3 | 1.59 | 0.89–2.84 | 0.121 | 523 | 3.89 | 1.38–10.97 | 0.010 | 495 | |
| Model 4 | 1.60 | 0.85–3.01 | 0.142 | 443 | 3.52 | 1.16–10.71 | 0.026 | 459 | |
Statistically significant findings (P < 0.05) shown in bold type.
Model 1: univariate logistic regression, adjusted for age and gender.
Model 2: adjusted for age, gender, socio‐demographic background (marital status, education, employment, economic situation).
Model 3: adjusted for age, gender, socio‐demographic background (marital status, education, employment, economic situation) and migration related variables (refugee status (for Kurdish), age at migration, language proficiency).
Model 4: adjusted for age, gender, current affective symptoms (HSCL‐25 > 1.75).
AUDIT‐C total score as a continuous variable;
beta coefficient (β) instead of OR. OR =odds ratio; CI = confidence interval; HSCL = Hopkins Symptoms Checklist.
In post‐hoc analyses comparing the study populations and genders, no statistically significant differences between the Kurds and the Russians or between men and women were detected (see Supporting information, Tables S1, S2). Some differences between the groups might remain undetected due to the lack of statistical power.
Discussion
To our knowledge, this is the first European population‐based migrant study examining the associations between substance use and both pre‐ and post‐migration severe psychosocial stressors. In this population‐based study of Russian and Kurdish migrants, we found that pre‐migration potentially traumatic experiences (PTEs) as well as perceived discrimination (PD) in the new host country were associated with substance use, but the associations did not occur consistently between these populations and with regard to the substances examined.
Among Kurds, a predominantly forced migrant population, binge drinking, i.e. having more than six drinks on one occasion, and AUDIT‐C total score were associated with pre‐migration PTEs. This is mainly in line with previous studies including forced migrants 28, 29, 30, but contradictory results have also been reported 95, 96. The previous studies have examined alcohol use disorder (AUD) among internally displaced people, e.g. in Uganda 29, Georgia 30 and Croatia 28, and AUD 96 or hazardous drinking 95 among conflict‐affected general populations. We found no previous comparable research concerning forced migrants in their new host countries. It is possible that previous results among general populations or internally displaced people may not be comparable to international migrants facing specific challenges in new host countries 50, 51. Our study makes a relevant contribution to the existing literature demonstrating an association between a hazardous pattern of alcohol use and traumatic experiences among Kurds, a forced migrant population.
A possible explanation for the association between PTEs and alcohol use among Kurds could be the ‘self‐medication theory’, according to which an individual may engage in alcohol use to eliminate the uncomfortable symptoms and displeasing sensations (e.g. insomnia, flashbacks, hypervigilance) related to traumatic experiences 31, 97, 98, 99. Alternatively, explanations could include the differences in cultural norms and social acceptability of alcohol use between region of origin and the new host country. Alcohol use is widely prohibited in the Middle East 20, 21, 22, whereas it is socially acceptable in Finnish society. Therefore, our results may also reflect a change in alcohol use habits over time spent in the new host country, especially among traumatized individuals 14, 17, 18, 19, 34, 66. Previous results from this sample have shown that the most severe PTEs (e.g. torture) were more common among Kurds compared with other migrant groups 68. Thus, the severity of traumatization could be another explanation for associations particularly among Kurds. In the future, it would be important to evaluate the change of substance use habits before and after migration, and the effects of severity of traumatic experiences or cumulative traumatization on individuals with migrant backgrounds.
In line with previous findings among general populations 31, 97, 98, daily smoking and life‐time cannabis use were associated with PTEs only among the Russians in the unadjusted analyses. This could be explained by the limitations of cross‐sectional study design or the differences in prevalence rates. However, it is also possible that the patterns of associations among Russian migrants in Finland (mainly voluntary migrants) might be more similar and comparable to the general population than the associations among Kurds (mainly forced migrants).
Perceived discrimination (PD) was associated with life‐time cannabis use and AUDIT‐C score, but not with binge drinking among Kurds, and only with daily smoking in the unadjusted analyses among Russians. Our findings are in line with previous findings among general populations mainly in North America 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 100, 101, 102, 103. In the European context, Visser et al. 64 have reported associations between PD, alcohol use and smoking among African Surinamese and Ghanaians but not among Turkish and Moroccan participants. Illicit substance use was not examined. It is possible that PD affects other aspects of self‐rated health 50 rather than exacerbating drinking behaviour among certain migrant groups 101. Our contradicting results concerning alcohol use and perceived discrimination indicate a need for more detailed research on this topic.
There are theories about psychological distress being the mediating factor between perceived discrimination and substance use 82, and about substance use being a response or coping mechanism to the negative emotional states caused by discrimination and other post‐migration stressors 34, 53, 55, 82. Our results of the association between life‐time cannabis use, alcohol use and PD among the Kurds, after adjusting for markers of distress caused by poorer socio‐economic situation and current affective symptoms, could be interpreted as highlighting the importance of discrimination as a separate risk factor for substance use independent of other post‐migration stressors. This is in line with previous results demonstrating the impacts of discrimination on health of migrants 50. Discrimination could be a considerable risk factor among Kurds, a stateless group who have also been frequently discriminated against in their regions of origin 104. Our findings on PTEs, PD and substance use among Kurds highlight the impacts of cumulative adversities and that this population could be in a particularly vulnerable situation. From a public health perspective, our results highlight the need to assess and identify protective factors and resilience in future research.
Strengths and limitations
This study is based on population‐based migrant data that are collected from several cities in Finland and has a relatively high response rate. Despite the satisfying overall response rate, non‐response may have caused selection bias, especially concerning people with problematic substance use. Analysis weights were used to address this, but the effects of under‐reporting and attrition are difficult to estimate. The effects of under‐reporting or misreporting need to be considered concerning, e.g. the possible negative cultural connotations of substance use among Muslim participants 105, 106.
The strengths of this study include the use of population‐based data with two divergent migrant groups and bilingual field personnel who conducted the interviews either in participants’ native language or in Finnish. Using population‐based data reduces observation biases as, e.g. cultural variation between the populations can be recognized, in comparison with studies where migrants are analysed as a single population 107. Cross‐sectional data do not allow for deducing causality, and information on the substance use in the country of origin or change of substance use habits after migration, were not available.
Dichotomization of the selected outcome variables (binge drinking, daily smoking, life‐time cannabis use) is a limitation. This was, however, approached by post‐hoc analyses using AUDIT‐C as a continuous variable. In addition, life‐time cannabis use could be considered a weak measure, and disorder‐level substance use could not be evaluated with this study design and methodology. Exploring the use of other substances, such as khat, might have also provided the possibility to investigate these associations among the Somali participants. Another important limitation was that we were not able to perform the analyses separately for both genders due to the low prevalence of substance use among Kurdish women 66. This limitation was approached by adjusting for gender in the analyses, but it is likely that this does not account for the gendered nature of substance use, especially among Kurdish migrants 66. Regardless, our study adds to the very limited body of population‐based research on substance use among migrants and its association with severe pre‐ and post‐migration psychosocial stressors. Information on the substance use of Kurds is especially scant, and this study aims to reduce these gaps.
Other limitations include the adaptation of HTQ and EDS from their original versions. However, the measures have been used in several previous studies examining Russian and Kurdish origin populations 50, 51, 68. Additionally, the cut‐off point of the HSCL‐25 scale has not been validated among the populations under study, despite its good cross‐cultural reliability and validity 85, 87, 108, 109. Nevertheless, one of the strengths of our study is that current affective symptoms were considered when assessing the associations between PTEs, PD and substance use. To our knowledge, this approach has not been taken before.
Conclusion
Pre‐migration traumatic experiences and perceived discrimination in the new country of residence are associated with substance use among a forced and a voluntary migrant population. However, the associations did not occur consistently among these populations and with regard to the substances examined. In clinical practice, psychosocial risk factors, including substance use, traumatic experiences and perceived discrimination, should be screened for individuals with various migration backgrounds. Ultimately, our results demonstrate the negative health effects of discrimination and highlight that zero tolerance of discrimination is needed to reduce health disparities.
Declaration of interests
S.N. (lecture fee: Shire, travel fee: Sunovion) and A.E.C. (lecture and writing fees: Statistics Finland, Eli Lilly Finland, Duodecim, Talentum, stakeholder in clinical practice: Studio Soleil Ltd). The other authors declare no competing interests.
Supporting information
Table S1 Comparison between the study populations (post‐hoc analyses).
Table S2 Comparison between the genders (post‐hoc analyses).
Acknowledgements
This work was supported by The Finnish Foundation for Alcohol Studies, Juho Vainio Foundation (Juho Vainion Säätiö) (ES) and Finnish Cultural Foundation (Suomen kulttuurirahasto) (AEC).
Salama, E. S. , Castaneda, A. E. , Lilja, E. , Suvisaari, J. , Rask, S. , Laatikainen, T. , and Niemelä, S. (2020) Pre‐migration traumatic experiences, post‐migration perceived discrimination and substance use among Russian and Kurdish migrants—a population‐based study. Addiction, 115: 1160–1171. 10.1111/add.14904.
References
- 1. Close C., Kouvonen A., Bosqui T., Patel K., O'Reilly D., Donnelly M. The mental health and wellbeing of first generation migrants: a systematic‐narrative review of reviews. Globalizat Health 2016; 12: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ezard N. Substance use among populations displaced by conflict: a literature review. Disasters 2011; 36: 533–557. [DOI] [PubMed] [Google Scholar]
- 3. Horyniak D., Horyniak D., Melo J. S., Melo J. S., Farrell R. M., Farrell R. M., et al Epidemiology of substance use among forced migrants: a global systematic review. PLOS ONE 2016; 11: e0159134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lo J., Patel P., Shultz J. M., Ezard N., Roberts B. A systematic review on harmful alcohol use among civilian populations affected by armed conflict in low‐ and middle‐income countries. Subst Use Misuse 2017; 52: 1494–1510. [DOI] [PubMed] [Google Scholar]
- 5. International Organization for Migration . World Migration Report 2018. McAuliffe M, Ruhs M, editors. Grand‐Saconnex, Switzerland: International Organization for Migration; 2017, pp. 1–364.
- 6. Abebe D. S., Hafstad G. S., Brunborg G. S., Kumar B. N., Lien L. Binge drinking, cannabis and tobacco use among ethnic Norwegian and ethnic minority adolescents in Oslo, Norway. J Immigr Minor Health 2015; 17: 1–10. [DOI] [PubMed] [Google Scholar]
- 7. Acartürk C. Z., Nierkens V., Agyemang C., Stronks K. Depressive symptoms and smoking among young Turkish and Moroccan ethnic minority groups in the Netherlands: a cross‐sectional study. Subst Abuse Treat Prev Policy 2011; 6: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Amundsen E. J. Low level of alcohol drinking among two generations of non‐Western immigrants in Oslo: a multi‐ethnic comparison. BMC Public Health 2012; 12: 535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carrasco‐Garrido P., De Miguel A. G., Barrera V. H., Jimenez‐Garcia R. Health profiles, lifestyles and use of health resources by the immigrant population resident in Spain. Eur J Public Health 2007; 17: 503–507. [DOI] [PubMed] [Google Scholar]
- 10. Delforterie M. J., Creemers H. E., Huizink A. C. Recent cannabis use among adolescent and young adult immigrants in the Netherlands—the roles of acculturation strategy and linguistic acculturation. Drug Alcohol Depend 2014; 136: 79–84. [DOI] [PubMed] [Google Scholar]
- 11. Hjern A., Allebeck P. Alcohol‐related disorders in first‐ and second‐generation immigrants in Sweden: a national cohort study. Addiction 2004; 99: 229–236. [DOI] [PubMed] [Google Scholar]
- 12. Lindstrom M., Sundquist J. Ethnic differences in daily smoking in Malmo, Sweden. Varying influence of psychosocial and economic factors. Eur J Public Health 2002; 12: 287–294. [DOI] [PubMed] [Google Scholar]
- 13. Svensson M., Hagquist C. Adolescent alcohol and illicit drug use among first‐ and second‐generation immigrants in Sweden. Scand J Public Health 2010; 38: 184–191. [DOI] [PubMed] [Google Scholar]
- 14. Salas‐Wright C. P., Vaughn M. G. A ‘refugee paradox’ for substance use disorders? Drug Alcohol Depend 2014; 142: 345–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Markkula N., Lehti V., Gissler M., Suvisaari J. Incidence and prevalence of mental disorders among immigrants and native Finns: a register‐based study. Soc Psychiatry Psychiatr Epidemiol 2017; 52: 1523–1540. [DOI] [PubMed] [Google Scholar]
- 16. Wanigaratne S, Strang J. Substance misuse. In: Bhugra D, Bhugra D, Bhui K, Bhui K, editors. Textbook of Cultural Psychiatry. 2nd edn Cambridge, UK: Cambridge University Press; 2018, pp. 244–255. [Google Scholar]
- 17. Westermeyer J., Mellman L., Alarcon R. Cultural competence in addiction psychiatry. Addict Disord Treat 2006; 5: 1–13. [Google Scholar]
- 18. Westermeyer J. Cultural aspects of substance abuse and alcoholism. Psychiatric Clin North Am 1995; 18: 589–605. [PubMed] [Google Scholar]
- 19. Room R. Multicultural contexts and alcohol and drug use as symbolic behaviour. Addict Res Theory 2004; 13: 321–331. [Google Scholar]
- 20. AlMarri T. S. K., Oei T. P. S. Alcohol and substance use in the Arabian Gulf region: a review. Int J Psycho 2009; 44: 222–233. [DOI] [PubMed] [Google Scholar]
- 21. Baasher T. The use of drugs in the Islamic World. Br J Addict 1981; 76: 233–243. [DOI] [PubMed] [Google Scholar]
- 22. Hafeiz H. B. Socio‐demographic correlates and pattern of drug abuse in eastern Saudi Arabia. Drug Alcohol Depend 1995; 38: 255–259. [DOI] [PubMed] [Google Scholar]
- 23. Rossow I., Clausen T. The collectivity of drinking cultures: is the theory applicable to African settings? Addiction 2013; 108: 1612–1617. [DOI] [PubMed] [Google Scholar]
- 24. Clausen T., Rossow I., Naidoo N., Kowal P. Diverse alcohol drinking patterns in 20 African countries. Addiction 2009; 104: 1147–1154. [DOI] [PubMed] [Google Scholar]
- 25. Griswold M. G., Fullman N., Hawley C., Arian N., Zimsen S. R. M., Tymeson H. D., et al Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet 2018; 392: 1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Horvat P., Stefler D., Murphy M., King L., McKee M., Bobak M. Alcohol, pattern of drinking and all‐cause mortality in Russia, Belarus and Hungary: a retrospective indirect cohort study based on mortality of relatives. Addiction 2018; 113: 1252–1263. [DOI] [PubMed] [Google Scholar]
- 27. Room R., Mäkelä K. Typologies of the cultural position of drinking. J Stud Alcohol 2000; 61: 475–483. [DOI] [PubMed] [Google Scholar]
- 28. Kozaric‐Kovacic D., Ljubin T., Grappe M. Comorbidity of posttraumatic stress disorder and alcohol dependence in displaced persons. Croat Med J 2000; 41: 173–178. [PubMed] [Google Scholar]
- 29. Roberts B., Ocaka K. F., Browne J., Oyok T., Sondorp E. Alcohol disorder amongst forcibly displaced persons in northern Uganda. Addict Behav 2011; 36: 870–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Roberts B, Murphy A, Chikovani I, Makhashvili N, Patel V, McKee M. Individual and community level risk‐factors for alcohol use disorder among conflict‐affected persons in Georgia. Schmidt U, editor. PLOS ONE 2014;9:e98299–e98211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Breslau N., Davis G. C., Schultz L. R. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry 2003; 60: 289–294. [DOI] [PubMed] [Google Scholar]
- 32. Metrik J., Jackson K., Bassett S. S., Zvolensky M. J., Seal K., Borsari B. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychol Addict Behav 2016; 30: 743–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Odenwald M., Hinkel H., Schauer E., Schauer M., Elbert T., Neuner F., et al Use of khat and posttraumatic stress disorder as risk factors for psychotic symptoms: a study of Somali combatants. Soc Sci Med 2009; 69: 1040–1048. [DOI] [PubMed] [Google Scholar]
- 34. Horyniak D., Higgs P., Cogger S., Dietze P., Bofu T. Heavy alcohol consumption among marginalised African refugee young people in Melbourne, Australia: motivations for drinking, experiences of alcohol‐related problems and strategies for managing drinking. Ethn Health 2015; 21: 284–299. [DOI] [PubMed] [Google Scholar]
- 35. Dupont H. J. B. H. M., Kaplan C. D., Verbraeck H. T., Braam R. V., van de Wijngaart G. F. Killing time: drug and alcohol problems among asylum seekers in the Netherlands. Int J Drug Policy 2005; 16: 27–36. [Google Scholar]
- 36. Steel Z., Chey T., Silove D., Marnane C., Bryant R. A., van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta‐analysis. JAMA 2009; 302: 537–549. [DOI] [PubMed] [Google Scholar]
- 37. de Jong J. T. V. M., Komproe I. H. Lifetime events and posttraumatic stress disorder in 4 postconflict settings. JAMA 2001; 286: 555–562. [DOI] [PubMed] [Google Scholar]
- 38. de Jong J. T., Komproe I. H., van Ommeren M. Common mental disorders in postconflict settings. Lancet 2003; 361: 2128–2130. [DOI] [PubMed] [Google Scholar]
- 39. Weaver H., Roberts B. Drinking and displacement: a systematic review of the influence of forced displacement on harmful alcohol use. Subst Use Misuse 2010; 45: 2340–2355. [DOI] [PubMed] [Google Scholar]
- 40. Galea S., Nandi A., Vlahov D. The social epidemiology of substance use. Epidemiol Rev 2004; 26: 36–52. [DOI] [PubMed] [Google Scholar]
- 41. Aichberger M. C., Bromand Z., Rapp M. A., Yesil R., Montesinos A. H., Temur‐Erman S., et al Perceived ethnic discrimination, acculturation, and psychological distress in women of Turkish origin in Germany. Soc Psychiatry Psychiatr Epidemiol 2015; 50: 1691–1700. [DOI] [PubMed] [Google Scholar]
- 42. Noh S., Kaspar V., Wickrama K. A. S. Overt and subtle racial discrimination and mental health: preliminary findings for Korean immigrants. Am J Public Health 2007; 97: 1269–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Williams D. R., Yu Y., Jackson J. S., Anderson N. B. Racial differences in physical and mental health: socio‐economic status, stress and discrimination. J Health Psychol 1997; 2: 335–351. [DOI] [PubMed] [Google Scholar]
- 44. Priest N., Paradies Y., Trenerry B., Truong M., Karlsen S., Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med 2013; 95: 115–127. [DOI] [PubMed] [Google Scholar]
- 45. Ikram U. Z., Snijder M. B., Fassaert T. J. L., Schene A. H., Kunst A. E., Stronks K. The contribution of perceived ethnic discrimination to the prevalence of depression. Eur J Public Health 2014; 25: 243–248. [DOI] [PubMed] [Google Scholar]
- 46. Bhui K., Stansfeld S. A., McKenzie K., Karlsen S., Nazroo J. Y., Weich S. Racial/ethnic discrimination and common mental disorders among workers: findings from the EMPIRIC study of ethnic minority groups in the United Kingdom. Am J Public Health 2005; 95: 496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Taylor J., Turner R. J. Perceived discrimination, social stress, and depression in the transition to adulthood: racial contrasts. Soc Psychol Q 2002; 65: 213–225. [Google Scholar]
- 48. Noh S., Beiser M., Kaspar V., Hou F., Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. J Health Soc Behav 1999; 40: 193–207. [PubMed] [Google Scholar]
- 49. Pascoe E. A., Richman L. S. Perceived discrimination and health: a meta‐analytic review. Psychol Bull 2009; 135: 531–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rask S., Elo I. T., Koskinen S., Lilja E., Koponen P., Castaneda A. E. The association between discrimination and health: findings on Russian. Somali and Kurdish origin populations in Finland. Eur J Public Health 2018; 29: 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Castaneda A. E., Rask S., Koponen P., Suvisaari J., Koskinen S., Härkänen T., et al The association between discrimination and psychological and social well‐being: a population‐based study of Russian, Somali and Kurdish migrants in Finland. Psychol Devel Soc 2015; 27: 270–292. [Google Scholar]
- 52. Martin J. K., Tuch S. A., Roman P. M. Problem drinking patterns among African Americans: the impacts of reports of discrimination, perceptions of prejudice, and ‘risky’ coping strategies. J Health Soc Behav 2003; 44: 408–425. [PubMed] [Google Scholar]
- 53. Borrell L. N., Roux A. V. D., Jacobs D. R. Jr., Shea S., Jackson S. A., Shrager S., et al Perceived racial/ethnic discrimination, smoking and alcohol consumption in the multi‐ethnic study of atherosclerosis (MESA). Prev Med 2010; 51: 307–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Borrell L. N., Jacobs D. R., Williams D. R., Pletcher M. J., Houston T. K., Kiefe C. I. Self‐reported racial discrimination and substance use in the coronary artery risk development in adults study. Am J Epidemiol 2007; 166: 1068–1079. [DOI] [PubMed] [Google Scholar]
- 55. Zemore S. E., Karriker‐Jaffe K. J., Keithly S., Mulia N. Racial prejudice and unfair treatment: interactive effects with poverty and foreign nativity on problem drinking. J Stud Alcohol Drugs 2011; 72: 361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chae D. H., Takeuchi D. T., Barbeau E. M., Bennett G. G., Lindsey J. C., Stoddard A. M., et al Alcohol disorders among Asian Americans: associations with unfair treatment, racial/ethnic discrimination, and ethnic identification (the national Latino and Asian Americans study, 2002–2003). J Epidemiol Community Health 2008; 62: 973–979. [DOI] [PubMed] [Google Scholar]
- 57. Otiniano Verissimo A. D., Gee G. C., Ford C. L., Iguchi M. Y. Racial discrimination, gender discrimination, and substance abuse among Latina/os nationwide. Cultur Divers Ethnic Minor Psychol 2014; 20: 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ramos Z., Fortuna L. R., Porche M. V., Wang Y., Shrout P. E., Loder S., et al Posttraumatic stress symptoms and their relationship to drug and alcohol use in an international sample of Latino immigrants. J Immigr Minor Health 2016; 19: 552–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tran A. G. T. T., Lee R. M., Burgess D. J. Perceived discrimination and substance use in Hispanic/Latino, African‐born black, and southeast Asian immigrants. Cultur Divers Ethnic Minor Psychol 2010; 16: 226–236. [DOI] [PubMed] [Google Scholar]
- 60. Bennett G. G., Wolin K. Y., Robinson E. L., Fowler S., Edwards C. L. Perceived racial/ethnic harassment and tobacco use among African American young adults. Am J Public Health 2005; 95: 238–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Guthrie B. J., Young A. M., Williams D. R., Boyd C. J., Kintner E. K. African American girls’ smoking habits and day‐to‐day experiences with racial discrimination. Nurs Res 2002; 51: 183–190. [DOI] [PubMed] [Google Scholar]
- 62. Siddiqi A., Shahidi F. V., Ramraj C., Williams D. R. Associations between race, discrimination and risk for chronic disease in a population‐based sample from Canada. Soc Sci Med 2017; 194: 135–141. [DOI] [PubMed] [Google Scholar]
- 63. Gee G. C., Delva J., Takeuchi D. T. Relationships between self‐reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. Am J Public Health 2007; 97: 933–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Visser M. J., Ikram U. Z., Derks E. M., Snijder M. B., Kunst A. E. Perceived ethnic discrimination in relation to smoking and alcohol consumption in ethnic minority groups in the Netherlands: the HELIUS study. Int J Public Health 2017; 62: 879–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Castaneda A.E., Rask S, Koponen P, Mölsä M, Koskinen S. Maahanmuuttajien terveys ja hyvinvointi. Tutkimus venäläis‐, somalialais‐ ja kurditaustaisista Suomessa [Migrant Health and Wellbeing. A study on persons of Russian, Somali and Kurdish origin in Finland] (in Finnish, English abstract). Report 61/2012. Helsinki: National Institute for Health and Welfare (THL); 2012, p. 397.
- 66. Salama E., Niemelä S., Suvisaari J., Laatikainen T., Koponen P., Castaneda A. E. The prevalence of substance use among Russian, Somali and Kurdish migrants in Finland: a population‐based study. BMC Public Health 2018; 18: 651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Salama E., Castaneda A. E., Suvisaari J., Rask S., Laatikainen T., Niemelä S. Substance use, affective symptoms and suicidal ideation among Russian, Somali and Kurdish migrants in Finland. Accepted in Transcult Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Castaneda A. E., Junna L., Lilja E., Skogberg N., Kuusio H., Mäki‐Opas J., et al The prevalence of potentially traumatic pre‐migration experiences: a population‐ based study of Russian, Somali and Kurdish origin migrants in Finland. J Trauma Stress Disor Treat 2017; 06: 1–7. [Google Scholar]
- 69. Castaneda A.E., Rask S, Härkänen T, Juntunen T, Skogberg N, Mölsä M, et al. Enhancing survey participation among foreign‐born populations: experiences from the Finnish migrant health and wellbeing study (Maamu). Finn Yearb Popul Res 2019; 53: 89–110. [Google Scholar]
- 70. Gmel G., Kuntsche E., Rehm J. Risky single‐occasion drinking: bingeing is not bingeing. Addiction 2010; 106: 1037–1045. [DOI] [PubMed] [Google Scholar]
- 71. Gual A. Risky single drinking occasions or acute alcohol intoxications? Addiction 2011; 106: 1048–1049. [DOI] [PubMed] [Google Scholar]
- 72. Herring R., Berridge V., Thom B. Binge drinking: an exploration of a confused concept. J Epidemiol Community Health 2008; 62: 476–479. [DOI] [PubMed] [Google Scholar]
- 73. Bush K., Kivlahan D. R., McDonell M. B., Fihn S. D., Bradley K. A. The AUDIT alcohol consumption questions (AUDIT‐C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med 1998; 158: 1789–1795. [DOI] [PubMed] [Google Scholar]
- 74. Dawson D. A., Dawson D. A., Grant B. F., Grant B. F., Stinson F. S., Stinson F. S., et al Effectiveness of the derived alcohol use disorders identification test (AUDIT‐C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res 2005; 29: 844–854. [DOI] [PubMed] [Google Scholar]
- 75. Frank D., DeBenedetti A. F., Volk R. J., Williams E. C., Kivlahan D. R., Bradley K. A. Effectiveness of the AUDIT‐C as a screening test for alcohol misuse in three race/ethnic groups. J Gen Intern Med 2008; 23: 781–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kaarne T., Aalto M., Kuokkanen M., Seppä K. AUDIT‐C, AUDIT‐3 and AUDIT‐QF in screening risky drinking among Finnish occupational health‐care patients. Drug Alcohol Rev 2010; 29: 563–567. [DOI] [PubMed] [Google Scholar]
- 77. Ayazi T., Lien L., Eide A. H., Ruom M. M., Hauff E., Hauff E. What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war‐affected population? A cross‐sectional community study in South Sudan. BMC Psychiatry 2012; 12: 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ayazi T., Swartz L., Eide A. H., Lien L., Hauff E. Psychotic‐like experiences in a conflict‐affected population: a cross‐sectional study in South Sudan. Soc Psychiatry Psychiatr Epidemiol 2016; 51: 971–979. [DOI] [PubMed] [Google Scholar]
- 79. Gerritsen A. A. M., Bramsen I., Devillé W., van Willigen L. H. M., Hovens J. E., van der Ploeg H. M. Physical and mental health of afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 2006; 41: 18–26. [DOI] [PubMed] [Google Scholar]
- 80. Roberts B., Odong V. N., Browne J., Ocaka K. F., Geissler W., Sondorp E. An exploration of social determinants of health amongst internally displaced persons in northern Uganda. Confl Health 2009; 3: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Munjiza J., Britvic D., Radman M., Crawford M. J. Severe war‐related trauma and personality pathology: a case–control study. BMC Psychiatry 2017; 17: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Williams D. R., Mohammed S. A. Discrimination and racial disparities in health: evidence and needed research. J Behav Med 2008; 32: 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Derogatis L. R., Lipman R. S., Rickels K. R., Uhlenhuth E. H., Covi L. The Hopkins symptom checklist (HSCL): a self‐reported symptom inventory. Behav Sci 1974; 19: 1–15. [DOI] [PubMed] [Google Scholar]
- 84. Sandanger I., Moum T., Ingebrigtsen G., Dalgard O. S., Sørensen T., Bruusgaard D. Concordance between symptom screening and diagnostic procedure: the Hopkins symptom Checklist‐25 and the composite international diagnostic interview I. Soc Psychiatry Psychiatr Epidemiol 1998; 33: 345–354. [DOI] [PubMed] [Google Scholar]
- 85. Tinghög P., Carstensen J. Cross‐cultural equivalence of HSCL‐25 and WHO (ten) wellbeing index: findings from a population‐based survey of immigrants and non‐immigrants in Sweden. Community Ment Health J 2009; 46: 65–76. [DOI] [PubMed] [Google Scholar]
- 86. Haroz E. E., Bolton P., Gross A., Chan K. S., Michalopoulos L., Bass J. Depression symptoms across cultures: an IRT analysis of standard depression symptoms using data from eight countries. Soc Psychiatry Psychiatr Epidemiol 2016; 51: 981–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hollifield M., Warner T. D., Lian N., Krakow B., Jenkins J. H., Kesler J., et al Measuring trauma and health status in refugees: a critical review. JAMA 2002; 288: 611–621. [DOI] [PubMed] [Google Scholar]
- 88. Rask S., Suvisaari J., Koskinen S., Koponen P., Mölsä M., Lehtisalo R., et al The ethnic gap in mental health: a population‐based study of Russian, Somali and Kurdish origin migrants in Finland. Scand J Public Health 2015; 44: 1–10. [DOI] [PubMed] [Google Scholar]
- 89. Gerritsen A. A., Bramsen I., Devillé W., van Willigen L. H., Hovens J. E., van der Ploeg H. M. Health and health care utilisation among asylum seekers and refugees in the Netherlands: design of a study. BMC Public Health 2004; 4: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Tinghög P., Al‐Saffar S., Carstensen J., Nordenfelt L. The association of immigrant‐ and non‐immigrant‐specific factors with mental ill health among immigrants in Sweden. Int J Soc Psychiatry 2010; 56: 74–93. [DOI] [PubMed] [Google Scholar]
- 91. Lehtonen R., Pahkinen E. Practical Methods for Design and Analysis of Complex Surveys, 2nd edn; 2003, p. 360 Chichester, UK: Wiley. [Google Scholar]
- 92. Graubard B. I., Korn E. L. Predictive margins with survey data. Biometrics 1999; 55: 652–659. [DOI] [PubMed] [Google Scholar]
- 93. Robins J. M., Andrea R., Ping Z. L. Estimation of regression coefficients when some regressors are not always observed. J Am Statist Assoc 1994; 89: 845–866. [Google Scholar]
- 94. Ambler G., Royston P. Fractional polynomial model selection procedures: investigation of type i error rate. J Stat Comput Simul 2001; 69: 89–108. [Google Scholar]
- 95. Lien L., Hauff E., Martinez P., Eide A. H., Swartz L., Ayazi T. Alcohol use in South Sudan in relation to social factors, mental distress and traumatic events. BMC Public Health 2016; 16: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Priebe S., Bogic M., Ajdukovic D., Franciskovic T., Galeazzi G. M., Kucukalic A., et al Mental disorders following war in the Balkans. Arch Gen Psychiatry 2010; 67: 518–528. [DOI] [PubMed] [Google Scholar]
- 97. Bonn‐Miller M. O., Vujanovic A. A., Boden M. T., Gross J. J. Posttraumatic stress, difficulties in emotion regulation, and coping‐oriented marijuana use. Cogn Behav Ther 2011; 40: 34–44. [DOI] [PubMed] [Google Scholar]
- 98. Bonn‐Miller M. O., Vujanovic A. A., Feldner M. T., Bernstein A., Zvolensky M. J. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event‐exposed marijuana users. J Traum Stress 2007; 20: 577–586. [DOI] [PubMed] [Google Scholar]
- 99. Brady K. T., Killeen T. K., Brewerton T., Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry 2006; 61: 22–32. [PubMed] [Google Scholar]
- 100. Choi Y., Harachi T. W., Gillmore M. R., Catalano R. F. Are multiracial adolescents at greater risk? Comparisons of rates, patterns, and correlates of substance use and violence between monoracial and multiracial adolescents. Am J Orthopsychiatry 2006; 76: 86–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Yen I. H., Ragland D. R., Greiner B. A., Fisher J. M. Racial discrimination and alcohol‐related behavior in urban transit operators: findings from the San Francisco muni health and safety study. Public Health Rep 1999; 114: 448–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gilbert P. A., Zemore S. E. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016; 161: 178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Tse W. S., Wong K. K. F. Comparing of the mediation and the moderation role of coping motive in the relationship between perceived discrimination and hazardous drinking. J Subst Abuse 2014; 20: 439–446. [Google Scholar]
- 104. Sulaiman Hill C. M. R., Thompson S. C. Afghan and Kurdish refugees, 8–20 years after resettlement, still experience psychological distress and challenges to well being. Aust NZ J Public Health 2012; 36: 126–134. [DOI] [PubMed] [Google Scholar]
- 105. Bhopal R., Vettini A., Hunt S., Wiebe S., Hanna L., Amos A. Review of prevalence data in, and evaluation of methods for cross cultural adaptation of, UK surveys on tobacco and alcohol in ethnic minority groups. BMJ 2004; 328: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Westermeyer J. Methodological issues in the epidemiological study of alcohol–drug problems: sources of confusion and misunderstanding. Am J Drug Alcohol Abuse 1990; 16: 47–55. [DOI] [PubMed] [Google Scholar]
- 107. Bhopal R. S. Migration, Ethnicity, Race, and Health in Multicultural Societies. Introduction: the concepts of ethnicity and race in health and their implications in the context of international migration, 2nd edn. Oxford, UK: Oxford University Press; 2014. 1–94. [Google Scholar]
- 108. Bean T., Derluyn I., Eurelings‐Bontekoe E., Broekaert E., Spinhoven P. Validation of the multiple language versions of the Hopkins symptom Checklist‐37 for refugee adolescents. Adolescence 2007; 42: 51–71. [PubMed] [Google Scholar]
- 109. Davidson G. R., Murray K. E., Schweitzer R. D. Review of refugee mental health assessment: best practices and recommendations. J Pac Rim Psychol 2010; 4: 72–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Comparison between the study populations (post‐hoc analyses).
Table S2 Comparison between the genders (post‐hoc analyses).


