Abstract
Objective
Enhanced cognitive behavior therapy (CBT‐E) is a transdiagnostic treatment suitable for the full range of eating disorders (EDs). Although the effectiveness of CBT(‐E) is clear, it is not being used as widely in clinical practice as guidelines recommend. The aim of the present study was to compare the effectiveness of CBT‐E with treatment as usual (TAU), which was largely based on CBT principles.
Method
We conducted a randomized controlled trial on a total of 143 adult patients with an ED who received either CBT‐E or TAU. The primary outcome was recovery from the ED. Secondary outcome measures were levels of ED psychopathology, anxiety, and depressive symptoms. Self‐esteem, perfectionism, and interpersonal problems were repeatedly measured to examine possible moderating effects. We explored differences in duration and intensity between conditions.
Results
After 80 weeks, there were no differences between conditions in decrease in ED psychopathology, or symptoms of anxiety and depression. However, in the first six weeks of treatment there was a larger decrease in ED psychopathology in the CBT‐E condition. Moreover, when the internationally most widely used definition of recovery was applied, the recovery rate at 20 weeks of CBT‐E was significantly higher (57.7%) than of TAU (36.0%). At 80 weeks, this difference was no longer significant (CBT‐E 60.9%; TAU 43.6%). Furthermore, CBT‐E was more effective in improving self‐esteem and was also the less intensive and shorter treatment.
Discussion
With broader use of CBT‐E, the efficiency, accessibility and effectivity (on self‐esteem) of treatment for EDs could be improved.
Keywords: CBT‐E, cognitive behavior therapy, eating disorders, RCT, transdiagnostic, treatment outcome
1. INTRODUCTION
Prevailing guidelines for the treatment of eating disorders (ED) endorse cognitive behavior therapy (CBT) as psychological treatment of first choice, especially for bulimia nervosa (BN) and binge‐eating disorder (BED) (Hay et al., 2014; Hilbert, Hoek, & Schmidt, 2017; National Institute for Health and Care Excellence (NICE), 2017; Yager et al., 2014). The effectiveness of CBT for anorexia nervosa (AN) is less pronounced, however this should be understood in the context of similar, somewhat disappointing, outcomes of other therapies for AN (van den Berg et al., 2019; Waller, 2016). CBT‐Enhanced (CBT‐E) is a specific form of CBT suitable for the full range of eating disorder diagnoses (Fairburn, 2008). It is based on a transdiagnostic theory of the maintaining mechanisms involved in the persistence of ED, which assumes that most mechanisms are common to all EDs, rather than being specific for one diagnostic category. According to this theory, a dysfunctional evaluation of self‐worth, overly based on shape and weight, is central to all eating disorders (Fairburn, Cooper, & Shafran, 2003). The focused version of CBT‐E (CBT‐Ef) consists of interventions to modify this overevaluation of shape and weight. The treatment protocol can be adjusted when additional maintaining mechanisms are expected to obstruct change (low self‐esteem, clinical perfectionism, and interpersonal problems). This extended protocol is known as the “broad” version of CBT‐E (CBT‐Eb). For both versions of CBT‐E, two variants of intensity have been developed involving either 20 sessions in 20 weeks for patients who are not significantly underweight (body mass index (BMI) >17.5), or 40 sessions in 40 weeks for patients who are significantly underweight (BMI <17.5). On account of its transdiagnostic reach, CBT‐E has an advantage over other CBT protocols for the otherwise specified feeding and eating disorder (OSFED). A systematic review in 2018 showed robust evidence for the effectiveness of CBT‐E in adult patients with an ED, especially those with BN, BED, and OSFED (de Jong, Schoorl, & Hoek, 2018).
Although there is clear evidence of the effectiveness of CBT(‐E) for EDs, it is not being used as widely in clinical practice as guidelines recommend (Tobin, Banker, Weisberg, & Bowers, 2007; von Ranson & Robinson, 2006). In a 2018 Dutch study among 139 clinicians who delivered CBT for eating disorders, the use of specific CBT techniques was below the level one would expect if following treatment manuals (Mulkens, de Vos, de Graaff, & Waller, 2018). Moreover, there are no empirical data about the content, effectiveness and efficiency of treatments as usual (TAU). Independent ED experts in Belgium and the Netherlands have estimated that TAU for EDs is probably more intensive, longer‐term and less effective than CBT‐E (de Jong et al., 2016). If time‐limited CBT‐E is indeed at least as effective as TAU for a broad range of ED patients, then the effectiveness, efficiency and accessibility of an evidence‐based treatment for patients with an ED could be improved.
Therefore, the primary objective of this study was to assess whether the focused version of CBT‐E for patients with an ED and a BMI >17.5 was more optimal in terms of a higher percentage of recovery compared to TAU. The secondary objectives were to assess whether CBT‐E was more effective in reducing important aspects of ED psychopathology, and comorbid symptoms of anxiety and depression. Although the effect of the focused version of CBT‐E was assessed, according to the rationale of the broad version of CBT‐E, participants with more self‐esteem problems, perfectionism and interpersonal problems at baseline were expected to respond less on the focused version of CBT‐E. Consequently, these variables were examined as possible moderating variables. Finally, to test the hypothesis that CBT‐E is a less intensive and shorter treatment than TAU, possible differences in the duration and intensity between CBT‐E and TAU were explored.
2. METHOD
2.1. Design
A multicenter randomized controlled trial (RCT) was conducted at three specialized eating disorder treatment centers in three different regions in the Netherlands. Participants were randomized into two groups (CBT‐E vs. TAU), stratified by type of ED (AN, BN, BED, OSFED), gender (male/female), BMI range (17.5–20, 20–25, 25–30, 30–40), and psychotropic medication (yes/no). They were all assessed pretreatment (T0) and at 6 weeks (T1), 20 weeks (T2), 40 weeks (T3), and 80 weeks (T4), resulting in a 2 (treatment) × 5 (time) repeated measures factorial design. Given the nature of the psychological treatment, neither the therapists nor participants were blinded for the treatment given. Ethical approval was obtained from the Institutional Review Board of Leiden University Medical Centre (NL39205.058.12). The trial was also registered in the Netherlands Trial Register (NTR4485). For details of the rationale, design, methods, and procedure, we refer to de Jong et al. (2016).
2.2. Recruitment
The patient sample (N = 143) was recruited at three specialized departments for eating disorders: PsyQ/Parnassia Psychiatric Institute in The Hague, PsyQ/Lentis Psychiatric Institute in Groningen, and Rintveld/Altrecht Mental Health Institute in Zeist. Figure 1 shows the CONSORT flow diagram. The inclusion criteria were: having an ED that required treatment (determined using SCID‐I) (First, Spitzer, Gibbon, & Williams, 1996; van Groenestijn, Akkerhuis, Kupka, Schneider, & Nolen, 1998); aged 18 years or older; a BMI >17.5 and <40 (because of possible medical complications); and giving written informed consent after receiving a detailed description of the study. The exclusion criteria were: prior CBT‐E or very similar treatment (N = 2); a coexisting general psychiatric disorder that precluded eating disorder‐focused treatment (N = 9); medical instability or pregnancy (N = 5); intellectual disability (N = 0); insufficient command of the Dutch language to fill in the research questionnaires (N = 3); ongoing psychiatric treatment (except for antidepressant or attention deficit hyperactivity disorder medications) (N = 4) or not being able to attend the scheduled therapy sessions (N = 24).
Figure 1.
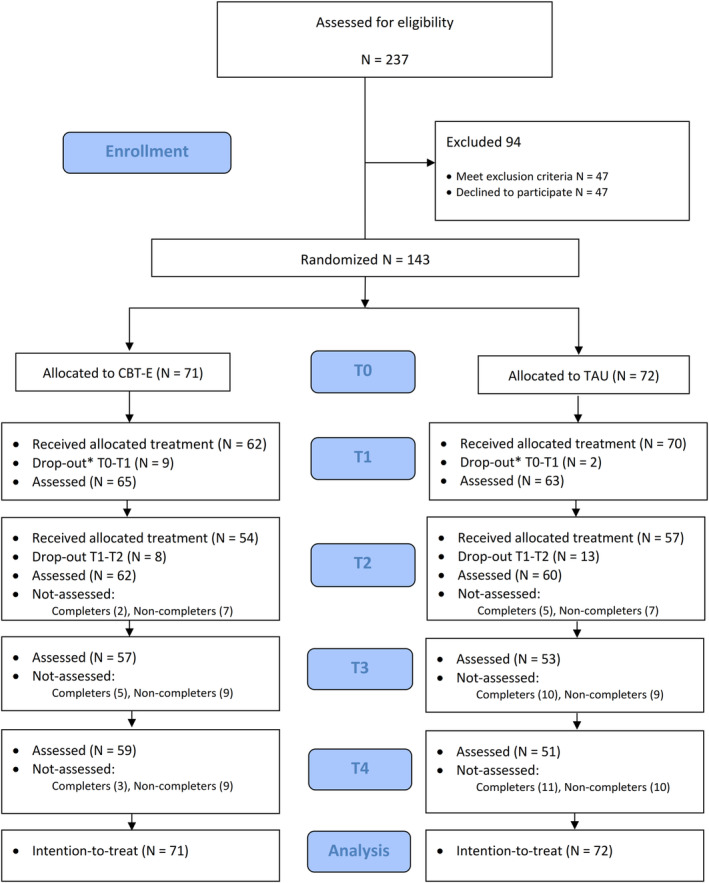
CONSORT flow diagram. *Operationalization of “treated as intended” differs between conditions [Color figure can be viewed at wileyonlinelibrary.com]
2.3. Treatments
2.3.1. Enhanced cognitive behavior therapy (CBT‐E)
CBT‐E is psychological treatment of 20 sessions, preceded by one preparatory session and followed by one review session 20 weeks after treatment. The sessions were held twice a week for the first 4 weeks, weekly for the next 10 weeks, and then biweekly in the last 6 weeks. CBT‐E is personalized to match the eating disorder psychopathology of the individual patient. In this study the focused version was used for patients with a BMI >17.5. Up to three additional sessions with significant others could be planned. A detailed manual in Dutch was developed based on the CBT‐E protocol (Fairburn, 2008) and was used by the participating therapists.
2.3.2. Treatment as usual
Because there are no empirical data about TAU in the Netherlands, clinician teams were asked about the content, intensity and duration of their TAU. The usual treatment given at the participating locations was based on CBT principles, given individually or in a group and containing elements of existing CBT treatment protocols (Dingemans, 2005; Vanderlinden, Pieters, Probst, & Norré, 2011). Depending on the center's treatment policy, this varied from low‐intensity care (weekly sessions) to high‐intensity care, which consisted of several group sessions a day for 2–4 days per week, and sometimes supplemented with individual sessions for coexisting psychopathology. The duration of the treatment was variable. Quite often more than one discipline (psychologist, dietitian, and psychiatrist) was involved in providing treatment. The type of treatment provided was registered.
2.4. Therapists and treatment integrity
All the CBT‐E therapists were psychologists, psychiatrists, registered nurses or social workers. They had at least 2 years of experience as a therapist in the field of EDs and had worked for at least 2 years according to CBT principles. CBT‐E therapists in the participating centers were trained by the founder of CBT‐E, Professor Christopher Fairburn, and had 20 supervision sessions via videoconferencing from his co‐worker, Professor Zafra Cooper. All the CBT‐E therapists treated at least three ED patients with CBT‐E under supervision before entering the trial. All the TAU therapists were psychologists/psychiatrists or registered nurses/social workers who had at least 2 years of experience as therapists in the field of EDs. TAU therapists had regular (mostly weekly), standard, local collegial consultation led by experienced eating disorder clinicians.
The quality of delivery of CBT‐E was assessed by independent raters (after an online CBT‐E training) who listened to the recorded sessions. In general, two recorded sessions for every CBT‐E patient were randomly selected (from, respectively, stages 1/2 and stages 3/4). The use of specific interventions according to the treatment manual was scored on several 3‐point Likert scales reflecting phase‐specific interventions and the use of interventions outside the scope of CBT‐E. This resulted in a total score for treatment adherence (0–25%, 25–50%, 50–75%, 75–100%). Of 121 recorded sessions, 52 were double‐rated to assess interrater reliability. For interrater reliability, Gwet's agreement coefficient (Gwet, 2008) with linear weights was calculated as an alternative to Cohen's Kappa for ordinal data (which is known to lead to paradoxical results when there is high agreement among raters) (Feinstein & Cicchetti, 1990; Warrens, 2010). There were five raters, one of whom was part of the rating pair on all occasions. This led to four rating pairs.
2.5. Assessment
Data were obtained via online questionnaires (using SurveyMonkey), with the exception of the SCID‐I ED section, which was conducted by telephone.
2.5.1. Screening and primary treatment outcome
Structured clinical interview for DSM axis‐I disorders (SCID‐I)
SCID‐I (First et al., 1996; van Groenestijn et al., 1998) is a structured interview used to assess the presence of an ED. Because SCID‐I only covers DSM‐IV AN, BN and EDNOS‐BED, skip rules were changed or omitted, and parts of the Eating Disorder Examination (EDE) (Fairburn, Cooper, & O'Connor, 2008) were added in order to diagnose DSM‐5 AN, BN, BED and OSFED (Smink, van Hoeken, Oldehinkel, & Hoek, 2014).
Web Screening Questionnaire for common mental disorders (WSQ)
The WSQ (Donker, van Straten, Marks, & Cuijpers, 2009) was used to screen for Axis‐I disorders.
2.5.2. Secondary study parameters
The Eating Disorder Examination‐Questionnaire (EDE‐Q)
The EDE‐Q (van Furth, 2000) is a self‐reported measure of ED psychopathology. Three outcome variables were created from the EDE‐Q: (a) severity of ED features as measured by the mean EDE‐Q item score (continuous), (b) a recovery rate defined as a global EDE‐Q score <1 standard deviation (SD) above community mean (categorical) (an internationally often used measure (Dalle Grave, Calugi, Sartirana, & Fairburn, 2015; Wade, Byrne, & Allen, 2017)), i.e., ≤2.77 (Mond, Hay, Rodgers, & Owen, 2006), (c) a global EDE‐Q score ≤2.77 + the reliable change index using Jacobson and Truax's method (Jacobson & Truax, 1991) assuming a test‐retest correlation of .76 (Reas, Grilo, & Masheb, 2006). A change greater than 1.41 was considered as reliable change.
Mood and Anxiety Symptom Questionnaire (MASQ)
The MASQ (de Beurs, van Hemert, & Goekoop, 1991) was used to assess the severity of symptoms of anxiety and depression.
Treatment duration
To measure treatment intensity and duration, treatment minutes (registered by the therapists) of every participant were collected between T0‐T1, T1‐T2 and T2‐T3.
2.5.3. Moderating variables
The Rosenberg Self‐Esteem Scale (RSE) (Rosenberg, 1965) is a widely‐used instrument used to assess global self‐esteem. A higher score refers to a better self‐esteem; the Frost Multidimensional Perfectionism Scale (FMPS) (Frost, Heimberg, Holt, Mattia, & Neubauer, 1993) was used to assess perfectionism, and the Inventory of Interpersonal Problems (IIP‐32) (Barkham, Hardy, & Startup, 1996) was used to measure interpersonal problems.
2.6. Power and sample size
In order to detect an absolute difference in recovery rates from ED of 25% (CBT‐E: 50% vs. TAU: 25%), a sample size of 66 patients per treatment condition was required to provide 80% power at two‐sided p <.05 (intention‐to‐treat analysis). This means that at least 132 patients were needed for this study.
2.7. Randomization
Randomization took place after screening of the inclusion/exclusion criteria and signing of the informed consent. Stratified randomization was achieved by generating a separate block for each combination of covariates (i.e., type of ED, gender, BMI range, and use of psychotropic medication) and assigning participants to the appropriate block of covariates. After the research assistant has allocated a participant to one of the strata, participants were assigned to CBT‐E or TAU using a permuted block randomization list, based on a computer generated outcome, blinded to the research assistant until the allocation to one of the strata.
2.8. Statistical methods
Pretreatment differences between conditions and between participants who completed the intended treatment and those who did not, were analyzed using t tests and Pearson's chi‐squared tests or Fisher's exact tests (if necessary).
2.8.1. Intention‐to‐treat analysis
Primarily, generalized estimating equations (GEE) were used to analyze the repeated measurement data for the presence of an eating disorder (SCID‐I) at T0, T2, and T4. The model consisted of main effects for time and type of treatment, as well as their interaction. Linear mixed models were used to analyze the repeated measurement data for eating disorder psychopathology (EDE‐Q), interpersonal problems (IIP‐32), perfectionism (FMPS), self‐esteem (RSE), lack of positive affect, somatic arousal, and negative affect at all five time points. The fixed part of each model consisted of main effects for treatment and time, as well as their interaction. Time was included in the analyses as a categorical variable, with the baseline measurement as reference category. The random part of each model contained a random intercept and a random slope for time, which were assumed to be correlated. For SCID‐I and EDE‐Q, it was investigated whether there was any difference in time effect between the three treatment locations, by incorporating a fixed effect for location and an interaction between location and time. Restricted maximum likelihood estimation was used in all mixed models. When an overall F test indicated the presence of a significant time x treatment interaction, fixed effects were reported for all parameters.
Mixed models were used to investigate the possible moderation of RSE, FMPS, and IIP‐32 baseline scores on the time × treatment interaction in the analysis concerning EDE‐Q, by including an interaction between the already present time × treatment interaction and RSE, FMPS, and IIP‐32, respectively.
2.8.2. Per protocol analysis
In an ITT analysis, the effect of being assigned to a specific treatment is estimated, irrespective of whether or not participants started or completed the treatment. To estimate the true effect of the experimental condition taking into account effects of nonadherence, a per‐protocol (PP) analysis was conducted (Oncioiu, Franchetti‐Pardo, Virtanen, Faggiano, & Galanti, 2017). For the PP analysis, not receiving CBT‐E as intended was defined as premature termination of treatment (i.e., patient had received less than 70% of the allocated treatment, <14 of the 20 sessions), or when additional treatment for the ED or comorbid psychopathology was provided. As there was no manualized protocol for TAU as control group, not receiving TAU as intended was defined as termination of the indicated treatment before T2, either against the therapist's advice or when participants were transferred to another department before T2 for another treatment as originally intended. GEE and mixed models were repeated for participants who completed the intended treatment and only findings that deviated from previous findings in the intention‐to‐treat analyses will be reported. Subsequently, group differences in recovery rates (based on SCID‐I diagnosis, EDE‐Q ≤2.77 and EDE‐Q ≤2.77 + reliable change index; Jacobson & Truax, 1991) were analyzed at 20 and 80 weeks using Pearson's chi‐squared tests. Analyses regarding recovery (based on the EDE‐Q) were repeated, after omitting participants with scores below the cut‐off at baseline (EDE‐Q ≤2.77). Differences between conditions in treatment intensity (T0‐T1, T1‐T2, T2‐T3, and T0‐T3) were analyzed using Mann–Whitney U test.
3. RESULTS
3.1. Patient sample
A total of 143 participants were enrolled from three Dutch mental health centers between 2013 and 2016 (89 from PsyQ/Parnassia Psychiatric Institute in The Hague, 34 from PsyQ/Lentis Psychiatric Institute in Groningen, and 20 from Rintveld/Altrecht Mental Health Institute in Zeist). Their diagnoses were as followed: 13 AN; BMI range 17.1–19.0 (9.1%), 50 BN; BMI range 18.8–39.3 (35%), 38 BED; BMI range 20.1–41.2 (26.6%) and 42 OSFED; BMI range 18.4–38.7 (29.4%). 71 were randomized to CBT‐E and 72 to TAU. Except for age (t(133.83) = −2.11, p = .04, d = 0.35), there were no significant differences in relevant baseline variables between the two treatment conditions and between the three locations. The demographic characteristics of the sample are summarized in Table 1. Given the recovery cut‐off for the EDE‐Q (Mond et al., 2006), there were nine participants with scores below the cut‐off at baseline in the total sample of the TAU group, and seven in the CBT‐E group.
Table 1.
Baseline characteristics of the patient sample
| CBT‐E | TAU | |||
|---|---|---|---|---|
| (N = 71) | (N = 72) | |||
| M | SD | M | SD | |
| Age (years) | 28.9 | 8.6 | 26.2 | 6.9 |
| Duration of eating disorder in years (N = 123) | 9.2 | 8.5 | 7.7 | 6.3 |
| BMI | 26.3 | 7.0 | 25.6 | 6.7 |
| EDE‐Q global score | 4.1 | 1.0 | 4.0 | 1.1 |
| FMPS | 86.5 | 22.2 | 83.1 | 22.2 |
| IIP‐32 | 1.5 | 0.6 | 1.3 | 0.6 |
| RSES | 22.3 | 5.1 | 23.6 | 5.2 |
| MASQ‐PA | 2.4 | 0.7 | 2.3 | 0.7 |
| MASQ‐SA | 1.8 | 0.6 | 1.9 | 0.7 |
| MASQ‐NA | 2.7 | 0.8 | 2.8 | 0.8 |
| WSQ | 3.8 | 2.2 | 3.4 | 2.1 |
| N | % | N | % | |
|---|---|---|---|---|
| Female | 69 | 97.2 | 68 | 94.4 |
| Currently in a relationship | 32 | 45.1 | 31 | 43.1 |
| Children | 16 | 22.5 | 11 | 15.3 |
| Live with parents | 11 | 15.5 | 10 | 13.9 |
| Anorexia nervosa | 5 | 7.0 | 8 | 11.1 |
| Bulimia nervosa | 27 | 38.0 | 23 | 31.9 |
| Binge‐eating disorder | 18 | 25.4 | 20 | 27.8 |
| Other specified feeding and eating disorders | 21 | 29.6 | 21 | 29.2 |
| Binges (during the past 28 days) | 51 | 71.8 | 53 | 73.6 |
| Purging (during the past 28 days) | 30 | 42.2 | 28 | 38.9 |
Abbreviations: CBT‐E, cognitive behavior therapy enhanced; EDE‐Q, Eating Disorder Examination‐Questionnaire; F‐MPS, Frost Multidimensional Perfectionism Scale; IIP‐32, Inventory of Interpersonal Problems; MASQ, Mood and Anxiety Questionnaire; NA, negative affect; PA, positive affect; RSE, Rosenberg Self‐Esteem Scale; SA, somatic anxiety; TAU, treatment as usual; WSQ, Web Screening Questionnaire for common mental disorders.
3.2. Treatment integrity
Due to a malfunctioning voice recorder, 8% of the recorded interview sessions were missing. According to the nomenclature proposed by Landis and Koch (1977), the interrater reliability was fair for the first couple (AC2 = .36), and almost perfect for the second and third couples (AC2 = .83 respectively .86). For the fourth couple, there was an absolute agreement on all ratings, which meant we could not calculate Gwet's AC (theoretically, however, this AC was 1.00). Ninety‐three percentage of the recorded sessions were scored in the highest rating range (75–100%), indicating there was good delivery of CBT‐E.
3.3. Characteristics of TAU
The type of treatment provided in TAU was registered (see Table 2). All treatments were based on CBT principles (i.e., registrations, cognitive techniques and behavioral experiments). However, there was a great variety in interventions, intensity, duration, setting and treatment of comorbidity.
Table 2.
Characteristics of treatment as usual (TAU) groups
| Location (N) | CBT | Group therapy | Individual therapy | Combination therapya | ≥2 disciplines involvedb | With treatment for comorbidityc |
|---|---|---|---|---|---|---|
| The Hague (43) | 43 | 8 | 24 | 11 | 40 | 14 |
| Groningen (19) | 19 | 5 | 5 | 9 | 11 | 5 |
| Zeist (10) | 10 | 2 | 4 | 4 | 10 | 2 |
| Total | 72 (100%) | 15 (21%) | 33 (46%) | 24 (33%) | 61 (85%) | 21 (29%) |
Combination of group and individual therapies.
For example, dietician, psychologist, psychiatrist, psychomotor therapist.
Including ADHD, depression, personality disorder, PTSS.
TAU differed from CBT‐E in two specific ways: (a) the content of the group treatments in TAU was based on CBT principles for specific diagnoses (for example; BN group or BED group) as opposed to CBTE that is a (individual) transdiagnostic treatment. (b) The content of individual treatments in TAU is best described as more freely applied CBT compared to manual based CBT‐E.
In addition to CBT for eating disorder psychopathology, a variety of additional interventions were integrated in TAU, including; nutritional interventions and psychomotor therapy (i.e., body awareness, emotion regulation). Furthermore, 29 % of the treatments in TAU included interventions for comorbid psychopathology (i.e., EMDR for posttraumatic stress disorder, CBT for depression and schema therapy for personality disorder). In most treatments (85%), more than one discipline was involved.
3.4. Differences between participants treated as intended versus not treated as intended
In the CBT‐E group, 17 participants (24%) did not complete treatment as intended; in the TAU group, this involved 15 participants (21%). The 32 participants who were not treated as intended did not differ from the 111 patients who completed treatment in their baseline measurements on the EDE‐Q, RSE, FMPS, and IIP‐32, their SCID diagnosis, treatment location or treatment condition (results available on request).
3.5. Intention‐to‐treat analysis
There was no significant interaction between group and time regarding recovery from SCID diagnosis (OR = 1.01, 95% CI [0.81, 1.26]). However, there was a main effect for time (OR = 2.33, 95% CI [1.98, 2.74]). Treatment locations did not differ in the overall presence of SCID diagnoses, nor was there an interaction with the time variable. Estimates and confidence intervals for this analysis are presented in Table S1 in the supplementary material.
For EDE‐Q, there was a significant main effect for time (F(4, 441) = 51.66, p <.001) and a significant interaction between group and time (F(4, 441) = 2.85, p = .02). The fixed effects in Table 3 show that this effect is particularly significant between T0 and T1. There was no main effect for location (F(2, 139) = 0.98, p = .38), nor an interaction effect between time and location (F(8, 433) = 1.06, p = .39). The left panel of Figure 2 shows the development of EDE‐Q scores over time for both groups. Parameter estimates for fixed effects can be found in Table 3.
Table 3.
Fixed effects for mixed models with EDE‐Q and RSE
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| EDE‐Q | |||||
| Intercept | 4.07 | 0.12 | 441 | 33.23 | <.001 |
| Time | |||||
| 6 weeks | −0.49 | 0.10 | 441 | −5.00 | <.001 |
| 20 weeks | −1.20 | 0.18 | 441 | −6.68 | <.001 |
| 40 weeks | −1.28 | 0.17 | 441 | −7.49 | <.001 |
| 80 weeks | −1.76 | 0.19 | 441 | −9.24 | <.001 |
| Condition1 | 0.06 | 0.17 | 141 | 0.36 | .72 |
| Condition × time | |||||
| 6 weeks | −0.31 | 0.14 | 441 | −2.22 | .03 |
| 20 weeks | −0.29 | 0.25 | 441 | −1.18 | .24 |
| 40 weeks | −0.42 | 0.24 | 441 | −1.77 | .08 |
| 80 weeks | 0.11 | 0.26 | 441 | 0.43 | .67 |
| RSE | |||||
| Intercept | 23.57 | 0.61 | 452 | 38.64 | <.001 |
| Time | |||||
| 6 weeks | 0.41 | 0.47 | 452 | 0.88 | .38 |
| 20 weeks | 1.70 | 0.61 | 452 | 2.79 | .01 |
| 40 weeks | 2.37 | 0.80 | 452 | 2.94 | <.001 |
| 80 weeks | 3.73 | 0.84 | 452 | 4.43 | <.001 |
| Condition1 | −1.27 | 0.87 | 141 | −1.47 | .14 |
| Condition × time | |||||
| 6 weeks | 1.64 | 0.66 | 452 | 2.48 | .01 |
| 20 weeks | 2.30 | 0.86 | 452 | 2.69 | .01 |
| 40 weeks | 2.36 | 1.12 | 452 | 2.10 | .04 |
| 80 weeks | 2.29 | 1.15 | 452 | 1.99 | .048 |
Abbreviations: EDE‐Q, Eating Disorder Examination Questionnaire; Condition, RSE, Rosenberg Self‐Esteem Scale.
1Condition = CBT‐E (cognitive behavior therapy enhanced).
Figure 2.
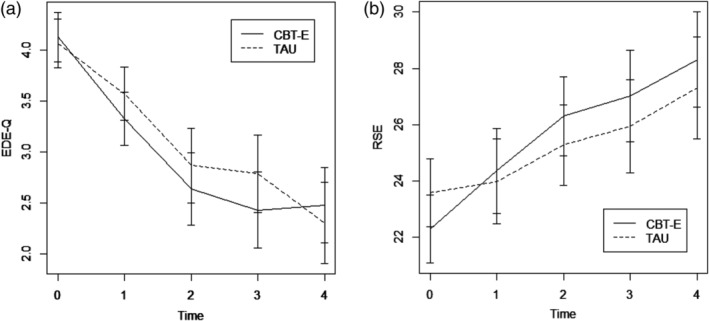
EDE‐Q and RSE scores for the CBT‐E and TAU groups. Abbreviations: CBT‐E, cognitive behavior therapy enhanced; EDE‐Q, Eating Disorder Examination Questionnaire; RSE, Rosenberg Self‐Esteem Scale; TAU, treatment as usual
For RSE, a main effect was present for time (F(4, 452) = 20.14, p <.001) as well as a group x time interaction (F(4, 452) = 2.49, p = .04). Fixed effects are presented in Table 3. In general, RSE showed a positive trend over time, and CBT‐E showed it had an extra time effect on self‐esteem. The development of RSE scores over time for both groups is depicted in the right panel of Figure 2, and parameter estimates are reported in Table 3.
For FMPS, only a significant main effect for time was found (F(4, 446) = 5.03, p <.001), but no significant group × time interaction (F(4, 446) = 1.71, p = .15).
For IIP‐32, significant main effects were found for time (F(4, 445) = 13.17, p < .001) and group (F(1, 141) = 4.19, p = .04), but no group × time interaction (F(4, 445) =1.73, p = .14).
For the MASQ, there was a main effect for time regarding negative affect (F(4, 456) = 17.57, p <.001), positive affect (F(4, 456) = 13.30, p <.001) and anxiety (F(4, 456) = 11.84, p < .001), but no group × time interactions were found for negative affect (F(4, 456) = 0.34, p = .85), positive affect (F(4, 456) = 0.62, p = .65) or anxiety (F(4, 456) = 0.67, p =.61). For all seven outcome measures, test statistics from the overall F tests are presented in Table S2 in the supplementary material.
3.6. Per protocol analysis
The recovery rates at 20 weeks (end of CBT‐E) and 80 weeks, as measured with the SCID were comparable for both treatment conditions (see Table 4). When using the international EDE‐Q recovery norm (global sore ≤1 SD above community mean; i.e., ≤2.77, and EDE‐Q ≤2.77 + RCI), the posttreatment recovery rates for CBT‐E at 20 weeks (57.7% and 46.2%) were significantly higher than that for TAU (36.0% and 26.0%). However, at 80 weeks this difference was no longer significant.
Table 4.
Participants treated as intended; rates at 20 and 80 weeks for CBT‐E and TAU using three different definitions of recovery
| At 20 weeks | At 80 weeks | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT‐E | TAU | Test statistics | CBT‐E | TAU | Test statistics | |||||||
| N | % | N | % | χ 2(1) | p | N | % | N | % | χ 2(1) | p | |
| Including participants with scores below the cut‐off at baseline | ||||||||||||
| Remitted (SCID) | 22 | 42.3 | 17 | 32.7 | 1.03 | 0.31 | 32 | 64.0 | 23 | 50.0 | 1.92 | 0.17 |
| EDE‐Q ≤2.77 | 30 | 57.7 | 18 | 36.0 | 4.81 | 0.03 | 32 | 62.7 | 22 | 50.0 | 1.56 | 0.21 |
| EDE‐Q ≤2.77 and RCI | 24 | 46.2 | 13 | 26.0 | 4.48 | 0.03 | 30 | 58.8 | 18 | 40.9 | 3.03 | 0.08 |
| Excluding participants with scores below the cut‐off at baseline | ||||||||||||
| Remitted (SCID) | 22 | 42.3 | 17 | 32.7 | 1.03 | 0.31 | 32 | 64.0 | 23 | 50.0 | 1.92 | 0.17 |
| EDE‐Q ≤2.77 | 26 | 55.3 | 14 | 31.8 | 5.09 | 0.03 | 28 | 60.9 | 17 | 43.6 | 2.53 | 0.11 |
| EDE‐Q ≤2.77 and RCI | 23 | 48.9 | 12 | 27.3 | 4.51 | 0.03 | 26 | 56.5 | 17 | 43.6 | 1.41 | 0.23 |
Abbreviations: CBT‐E, cognitive behavior therapy enhanced; TAU, treatment as usual.
RCI (Reliable Change Index) was based on a test–retest correlation of .76 and baseline pooled SD of 1.037 for both groups. Bold face values are significant.
For IIP, the main effect for treatment was nonsignificant (F(1, 109) = 1.69, p = .20), but the time x treatment effect became significant (F(4, 381) = 3.29, p = .01). CBT‐E shows an extra decline at 20 and 40 weeks compared to TAU. The overall F test statistics and fixed effects for IIP in the per protocol analysis are presented in the supplementary material, respectively in Tables S3 and S4.
3.7. Moderators
The time × treatment interaction for EDE‐Q global was moderated by the RSE baseline score (F(4, 433) = 2.56, p = .04). Between baseline and 6 weeks, participants receiving CBT‐E reported an additional decrease in EDE‐Q scores, when the RSE baseline score was higher. Overall F test statistics and fixed effects for this moderator analysis are presented in Tables S5 and S6 in the supplementary material.
3.8. Treatment intensity
Significant differences in treatment intensity between T0–T1 and T2–T3 were found. Between T0 and T1, CBT‐E was more intensive (Mann–Whitney: p <.001), while between T2–T3 TAU consisted of more treatment minutes (Mann–Whitney: p <.001). Overall, between T0–T3, CBT‐E appeared a significantly less intensive treatment than TAU (Mann–Whitney: p = .01) (see Table 5 and Figure S1 in the supplementary material).
Table 5.
Treatment intensity of participants treated as intended
| CBT‐E | TAU | |||
|---|---|---|---|---|
| Mdn | IQR | Mdn | IQR | |
| T0–T1a | ||||
| Treatment intensity (min) | 560 | 148 | 270 | 255 |
| T1–T2 | ||||
| Treatment intensity (min) | 587 | 143 | 630 | 822 |
| T2–T3a | ||||
| Treatment intensity (min) | 87 | 125 | 570 | 1,100 |
| Total (T0–T3)a | ||||
| Treatment intensity (min) | 1,272 | 249 | 1,860 | 2,280 |
Abbreviations: CBT‐E, cognitive behavior therapy enhanced; IQR, interquartile range; Mdn, median; TAU, treatment as usual.
Significant Mann–Whitney U test.
4. DISCUSSION
The first two aims in this study were to compare the focused version of CBT‐E with TAU for patients with an ED (BMI >17.5) in terms of differences in recovery from the ED, and reduction of important aspects of ED psychopathology and comorbid symptoms of anxiety and depression. Systematic registration of TAU showed that all these treatments were based on CBT principles, however with a great variation in interventions, setting, treatment intensity, number of involved disciplines, and treatment of comorbidity. After 80 weeks, there were no differences between conditions in recovery from the ED, or in decrease in global ED psychopathology and comorbid symptoms of anxiety and depression. However, significant differences in effect were found in the first six weeks of treatment, with the CBT‐E condition showing a larger decrease in ED psychopathology. Moreover, when the internationally most widely used definition of recovery was applied, the recovery rate at 20 weeks of CBT‐E was significantly higher (57.7%) than of TAU (36.0%). At 80 weeks (60 weeks follow‐up for the CBT‐E condition), this difference was no longer significant (CBT‐E 60.9%; TAU 43.6%). Compared to other RCTs examining CBT‐E with similar transdiagnostic samples (Fairburn et al., 2009; Fairburn et al., 2015) these recovery results are slightly lower, although the differences are small and direct comparisons are complicated by differences in study characteristics, instruments and data analysis. Furthermore, 24% of the participants in the present study did not complete CBT‐E as intended which is comparable to the Fairburn et al. study (2009) with a drop‐out rate of 22.1%. CBT‐E for nonunderweight patients with an ED is known to be more efficacious than interpersonal psychotherapy (Fairburn et al., 2015) and psychoanalytic therapy (Poulsen et al., 2014) in terms of a faster treatment response. This is the first study showing that CBT‐E also reaches these results faster than a less formal protocol of CBT (i.e., TAU). Although in this study therapists' considerations and exact treatment interventions (in the TAU group) were not registered, earlier studies have shown that in clinical practice, the integrity of applying CBT techniques (even in CBT eating disorder therapies) is below the level one would expect if treatment manuals were followed (Mulkens et al., 2018; Waller, Stringer, & Meyer, 2012). Together with the clear focus of CBT‐E on early behavioral change, it is likely that offering twice‐weekly sessions at the start could explain the faster response to CBT‐E in the first phase of treatment.
The third aim was to examine the possible moderating effects of self‐esteem, perfectionism and interpersonal problems. No differences between conditions were found on reduction of perfectionism or interpersonal problems, but CBT‐E proved more effective in improving self‐esteem than TAU. While it is often thought that amelioration of psychopathology symptoms during psychotherapy is associated with the enhancement of self‐esteem (Fennell & Jenkins, 2004), the precise mechanisms underpinning these effects are not known (Linardon, Kothe, & Fuller‐Tyszkiewicz, 2019). However, some potential explanations for the overall superior effect of CBT‐E on self‐esteem can be hypothesized. The main focus of CBT‐E is to modify the over‐evaluation of shape and weight by establishing self‐worth based on other aspects (friends, work, hobbies, etc.). It is assumed that by enhancing attention to other domains of self‐worth, self‐esteem can be improved (Fairburn, 2008). Interestingly, the difference in effect on self‐esteem was found to be largest in the first six weeks of treatment, which were not explicitly focused on modifying the over‐evaluation of shape and weight. However, this first phase is intensive (twice‐weekly sessions) and focuses mainly on understanding the processes that maintain the eating problems and on early behavioral change. This approach could also have secondary effects. For example, creating hope that change is possible, can enhance self‐confidence and self‐esteem (Fairburn, 2008).
Moreover, in the CBT‐E condition, changes in ED psychopathology during the first six weeks of treatment, were moderated by self‐esteem. When, at baseline, self‐esteem problems were less severe, there was an additional effect of CBT‐E on decreasing ED psychopathology in this first phase. This enhancing effect of self‐esteem disappears from week 20 onwards. Changes in ED psychopathology were not moderated by the degree of perfectionism or interpersonal problems. This means that, in this study, we found no support for the hypothesis that more severe self‐esteem problems, higher levels of perfectionism, or more interpersonal problems (the supposed additional maintaining mechanisms of ED) would obstruct long‐term improvement and would therefore need extra attention in an extended protocol.
The last aim of this study was to explore possible differences in the duration and intensity of CBT‐E and TAU. Although for nonunderweight ED patients, the current standard is to administer around 20 sessions of CBT in 20 weeks, there are no studies that have mapped the duration and intensity of TAU. In general, CBT‐E was completed in 20 weeks and was significantly more intensive for the first six weeks of treatment, whereas TAU was significantly more intensive between 20 and 40 weeks of treatment. Overall, (between start and 40 weeks of treatment) CBT‐E was significantly less intensive, which can have a major effect on health care costs.
This study has several limitations. The SCID was conducted by the research assistant. She was not blind for condition or previous SCID outcome because the outcome of the SCID was necessary for randomization and there was only one research assistant available. However, the EDE‐Q could be administered by Survey Monkey which had the benefit of unbiased data collection. Although the content of TAU was registered, there was no detailed description. For example, the way self‐esteem was addressed in TAU was unclear, which complicates interpretation of the differences in effect on self‐esteem between the two conditions. Furthermore, therapists and patients may be more interested in the effect of an intervention delivered as intended rather than in the effect of the assigned intervention. The results of our PP analysis closely replicated the results of our ITT analysis. However, as there is no univocal definition of TAU, and therefore no manualized protocol for the control group, TAU as intended had to be defined somewhat different from CBT‐E as intended with at least 14 sessions as a minimal requirement for attendance. Consequently, results have to be interpreted with caution. Moreover, because of the nature of the RCT, TAU was not limited in its duration. Therefore, we cannot draw any conclusions on the follow‐up results of TAU. Lastly, this study was restricted to participants with a BMI >17.5. Although it included a small percentage of participants with AN, we cannot generalize these findings to patients with AN.
A recommendation can be made for future research: although this study strengthens the evidence on the effectiveness of CBT‐E, little is known about the working mechanisms. Studies on these mechanisms in CBT‐E could strengthen its theoretical foundations.
5. CONCLUSION
After 80 weeks CBT‐E and TAU both have comparable effects on patients' recovery from an ED and show a decrease of ED psychopathology, however, we found CBT‐E reaches these results faster and is superior in enhancing self‐esteem with significantly fewer sessions and within a shorter time. With a broader implementation of CBT‐E in clinical practice, the efficiency, accessibility and effectivity (on self‐esteem) of treatment for patients with an ED could be improved.
Supporting information
Figure S1 Box plots for treatment intensity in minutes for both conditions, between subsequent timepoints.
Table S1. Estimates for Generalized Estimating Equations regarding SCID I diagnosis
Table S2. Overall F test statistics for model parameters in mixed models.
Table S3. Overall F test statistics for model parameters in mixed model for IIP‐32 in per protocol analyses.
Table S4. Fixed effects for mixed model with IIP‐32 in per protocol analysis
Table S5. Overall F test statistics for model parameters in mixed model for EDEQ with baseline RSE as a moderator. Baseline RSE score was standardized.
Table S6. Fixed effects in mixed model for EDEQ with baseline RSE as a moderator. Baseline RSE score was standardized.
de Jong M, Spinhoven P, Korrelboom K, et al. Effectiveness of enhanced cognitive behavior therapy for eating disorders: A randomized controlled trial. Int J Eat Disord. 2020;53:717–727. 10.1002/eat.23239
Associate Editor: Tracey Wade
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are vailable from the corresponding author upon reasonable request.
REFERENCES
- Barkham, M. , Hardy, G. E. , & Startup, M. (1996). The IIP‐32: A short version of the inventory of interpersonal problems. British Journal of Clinical Psychology, 35(1), 21–35. 10.1111/j.2044-8260.1996.tb01159.x [DOI] [PubMed] [Google Scholar]
- Dalle Grave, R. , Calugi, S. , Sartirana, M. , & Fairburn, C. G. (2015). Transdiagnostic cognitive behaviour therapy for adolescents with an eating disorder who are not underweight. Behaviour Research and Therapy, 73, 79–82. 10.1016/j.brat.2015.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beurs, E. , van Hemert, A. M. , & Goekoop, J. G. (1991). Mood and Anxiety Symptom Questionnaire (MASQ). [Dutch translation of MASQ]. Leiden: LUMC; (Based on: Watson, D. B., & Clark, L. A. (1991). Mood and Anxiety Symptom Questionnaire (MASQ). Iowa City, USA: Department of Psychology, University of Iowa). [Google Scholar]
- de Jong, M. , Korrelboom, K. , van der Meer, I. , Deen, M. , Hoek, H. W. , & Spinhoven, P. (2016). Effectiveness of enhanced cognitive behavioral therapy (CBT‐E) for eating disorders: Study protocol for a randomized controlled trial. Trials, 17(1), 573 10.1186/s13063-016-1716-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong, M. , Schoorl, M. , & Hoek, H. W. (2018). Enhanced cognitive behavioural therapy for patients with eating disorders: A systematic review. Current Opinion in Psychiatry, 31(6), 436–444. 10.1097/YCO.0000000000000452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingemans, A. E. (2005). Werkboek eetstoornis cognitieve gedragstherapie. Leidschendam: Kenniscentrum Eetstoornissen. [Google Scholar]
- Donker, T. , van Straten, A. , Marks, I. , & Cuijpers, P. (2009). A brief web‐based screening questionnaire for common mental disorders: Development and validation. Journal of Medical Internet Research, 11(3), e19 10.2196/jmir.1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. (2008). Cognitive behavior therapy and eating disorders. New York: Guilford Press. [Google Scholar]
- Fairburn, C. G. , Bailey‐Straebler, S. , Basden, S. , Doll, H. A. , Jones, R. , Murphy, R. , … Cooper, Z. (2015). A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT‐E) and interpersonal psychotherapy in the treatment of eating disorders. Behaviour Research and Therapy, 70, 64–71. 10.1016/j.brat.2015.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , Doll, H. A. , O'Connor, M. E. , Bohn, K. , Hawker, D. M. , … Palmer, R. L. (2009). Transdiagnostic cognitive‐behavioral therapy for patients with eating disorders: A two‐site trial with 60‐week follow‐up. The American Journal of Psychiatry, 166(3), 311–319. 10.1176/appi.ajp.2008.08040608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , & O'Connor, M. E. (2008). The eating disorder examination In Fairburn C. G. (Ed.), Cognitive behaviour therapy and eating disorders. New York: Guilford Press. [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A "transdiagnostic" theory and treatment. Behaviour Research and Therapy, 41(5), 509–528 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12711261 [DOI] [PubMed] [Google Scholar]
- Feinstein, A. R. , & Cicchetti, D. V. (1990). High agreement but low kappa: I. The problems of two paradoxes. Journal of Clinical Epidemiology, 43(6), 543–549. 10.1016/0895-4356(90)90158-L [DOI] [PubMed] [Google Scholar]
- Fennell, M. J. V. , & Jenkins, H. (2004). Low self‐esteem In Bennett‐Levy J., Butler G., Fennell M., Hackmann A., Mueller M., & Westbrook D. (Eds.), Oxford guide to behavioural experiments in cognitive therapy. Oxford, UK: Oxford University Press. [Google Scholar]
- First, M. B. , Spitzer, R. L. , Gibbon, M. , & Williams, J. B. W. (1996). Structured clinical interview for DSM‐IV axis I disorders. Patient Edition (SCID‐I/P, Version 2.0). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Frost, R. O. , Heimberg, R. G. , Holt, C. S. , Mattia, J. I. , & Neubauer, A. L. (1993). A comparison of two measures of perfectionism. Personality and Individual Differences, 14, 119–126. [Google Scholar]
- Gwet, K. L. (2008). Computing inter‐rater reliability and its variance in the presence of high agreement. The British Journal of Mathematical and Statistical Psychology, 61(Pt 1), 29–48. 10.1348/000711006X126600 [DOI] [PubMed] [Google Scholar]
- Hay, P. , Chinn, D. , Forbes, D. , Madden, S. , Newton, R. , Sugenor, L. , … Ward, W. (2014). Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Australian & New Zealand Journal of Psychiatry, 48(11), 977–1008. 10.1177/0004867414555814 [DOI] [PubMed] [Google Scholar]
- Hilbert, A. , Hoek, H. W. , & Schmidt, R. (2017). Evidence‐based clinical guidelines for eating disorders: International comparison. Current Opinion in Psychiatry, 30(6), 423–437. 10.1097/YCO.0000000000000360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson, N. S. , & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- Landis, J. R. , & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. [PubMed] [Google Scholar]
- Linardon, J. , Kothe, E. J. , & Fuller‐Tyszkiewicz, M. (2019). Efficacy of psychotherapy for bulimia nervosa and binge‐eating disorder on self‐esteem improvement: Meta‐analysis. European Eating Disorders Review, 27(2), 109–123. 10.1002/erv.2662 [DOI] [PubMed] [Google Scholar]
- Mond, J. M. , Hay, P. J. , Rodgers, B. , & Owen, C. (2006). Eating Disorder Examination Questionnaire (EDEQ): Norms for young adult women. Behaviour Research and Therapy, 44(1), 53–62. 10.1016/j.brat.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Mulkens, S. , de Vos, C. , de Graaff, A. , & Waller, G. (2018). To deliver or not to deliver cognitive behavioral therapy for eating disorders: Replication and extension of our understanding of why therapists fail to do what they should do. Behaviour Research and Therapy, 106, 57–63. 10.1016/j.brat.2018.05.004 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) . (2017). Eating disorders: Recognition and treatment. NICE guideline [NG69] (p. 41). London, UK: NICE. [PubMed] [Google Scholar]
- Oncioiu, S. I. , Franchetti‐Pardo, L. , Virtanen, S. E. , Faggiano, F. , & Galanti, M. R. (2017). Beyond intention‐to‐treat: The effect of brief counseling for tobacco cessation in secondary analyses of a cluster randomized controlled trial in Swedish dental clinics. Contemporary Clinical Trials Communications, 5, 92–99. 10.1016/j.conctc.2017.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulsen, S. , Lunn, S. , Daniel, S. I. , Folke, S. , Mathiesen, B. B. , Katznelson, H. , & Fairburn, C. G. (2014). A randomized controlled trial of psychoanalytic psychotherapy or cognitive‐behavioral therapy for bulimia nervosa. The American Journal of Psychiatry, 171(1), 109–116. 10.1176/appi.ajp.2013.12121511 [DOI] [PubMed] [Google Scholar]
- Reas, D. L. , Grilo, C. M. , & Masheb, R. M. (2006). Reliability of the Eating Disorder Examination‐Questionnaire in patients with binge eating disorder. Behaviour Research and Therapy, 44(1), 43–51. 10.1016/j.brat.2005.01.004 [DOI] [PubMed] [Google Scholar]
- Rosenberg, M. (1965). Society and the Adolescent Self‐Image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Smink, F. R. , van Hoeken, D. , Oldehinkel, A. J. , & Hoek, H. W. (2014). Prevalence and severity of DSM‐5 eating disorders in a community cohort of adolescents. International Journal of Eating Disorders, 47(6), 610–619. 10.1002/eat.22316 [DOI] [PubMed] [Google Scholar]
- Tobin, D. L. , Banker, J. D. , Weisberg, L. , & Bowers, W. (2007). I know what you did last summer (and it was not CBT): A factor analytic model of international psychotherapeutic practice in the eating disorders. International Journal of Eating Disorders, 40(8), 754–757. 10.1002/eat.20426 [DOI] [PubMed] [Google Scholar]
- van den Berg, E. , Houtzager, L. , de Vos, J. , Daemen, I. , Katsaragaki, G. , Karyotaki, E. , … Dekker, J. (2019). Meta‐analysis on the efficacy of psychological treatments for anorexia nervosa. European Eating Disorders Review, 27(4), 331–351. 10.1002/erv.2683 [DOI] [PubMed] [Google Scholar]
- van Furth, E. F. (2000). Vragenlijst Eetproblemen (EDEQ). [Dutch translation]. Based on: Fairburn, C.G. & Beglin, S.J. (1994). Assessment of eating disorders: Interview or self‐report questionnaire? International Journal of Eating Disorders, 16, 363–370 Retrieved from https://www.tijdschriftvoorpsychiatrie.nl/assets/measuringinstruments/EDE-Q_NL.pdf [PubMed] [Google Scholar]
- van Groenestijn, M. A. C. , Akkerhuis, G. W. , Kupka, R. W. , Schneider, N. , & Nolen, W. A. (1998). SCID‐I: gestructureerd klinisch interview voor de vaststelling van DSM‐IV As I Stoornissen. (Dutch translation of the SCID‐I). Amsterdam: Pearson Assessment and Information. [Google Scholar]
- Vanderlinden, J. , Pieters, G. , Probst, M. , & Norré, J. (2011). Protocollaire behandeling van patiënten met boulimia nervosa In Keijsers G., van Minnen A., & Hoogduin K. (Eds.), Protocollaire behandelingen voor volwassenen met psychische klachten (Deel 1). Amsterdam: Boom. [Google Scholar]
- von Ranson, K. M. , & Robinson, K. E. (2006). Who is providing what type of psychotherapy to eating disorder clients? A survey. International Journal of Eating Disorders, 39(1), 27–34. 10.1002/eat.20201 [DOI] [PubMed] [Google Scholar]
- Wade, S. , Byrne, S. , & Allen, K. (2017). Enhanced cognitive behavioral therapy for eating disorders adapted for a group setting. International Journal of Eating Disorders, 50(8), 863–872. 10.1002/eat.22723 [DOI] [PubMed] [Google Scholar]
- Waller, G. (2016). Recent advances in psychological therapies for eating disorders [version 1; peer review: 2 approved]. F1000Research, 5(F1000 Faculty Rev):702. 10.12688/f1000research.7618.1 [DOI] [PMC free article] [PubMed]
- Waller, G. , Stringer, H. , & Meyer, C. (2012). What cognitive behavioral techniques do therapists report using when delivering cognitive behavioral therapy for the eating disorders? Journal of Consulting and Clinical Psychology, 80(1), 171–175. 10.1037/a0026559 [DOI] [PubMed] [Google Scholar]
- Warrens, M. (2010). A formal proof of a paradox associated with Cohen's kappa. Journal of Classification, 27, 322–332. [Google Scholar]
- Yager, J. , Devlin, M. J. , Halmi, K. A. , Herzog, D. B. , Mitchell, J. E., III , Powers, P. , & Zerbe, K. (2014). Guideline watch (August 2012): Practice guideline for the treatment of patients with eating disorders. Focus, 12(4), 416–431. 10.1176/appi.focus.120404 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Box plots for treatment intensity in minutes for both conditions, between subsequent timepoints.
Table S1. Estimates for Generalized Estimating Equations regarding SCID I diagnosis
Table S2. Overall F test statistics for model parameters in mixed models.
Table S3. Overall F test statistics for model parameters in mixed model for IIP‐32 in per protocol analyses.
Table S4. Fixed effects for mixed model with IIP‐32 in per protocol analysis
Table S5. Overall F test statistics for model parameters in mixed model for EDEQ with baseline RSE as a moderator. Baseline RSE score was standardized.
Table S6. Fixed effects in mixed model for EDEQ with baseline RSE as a moderator. Baseline RSE score was standardized.
Data Availability Statement
The data that support the findings of this study are vailable from the corresponding author upon reasonable request.


