More nuanced health advice is needed to protect populations and individuals from exposure to bushfire smoke
Bushfires have always been a feature of the natural environment in Australia, but the risk has increased over time as fire seasons start earlier, finish later, and extreme fire weather (ie, very hot, dry and windy conditions that make fires fast moving and very difficult to control) becomes more severe with climate change.1, 2, 3 The 2019–20 bushfires in Australia, particularly in New South Wales, Victoria, Queensland and the Australian Capital Territory, have caused at least 33 fatalities, extensive damage to property and destruction of flora and fauna, and have exposed millions of people to extreme levels of air pollution. Bushfire smoke, as well as smoke from prescribed burns, contains a complex mixture of particles and gases that are chemically transformed in the atmosphere and transported by the wind over long distances.4 In this context, a major public health concern is population exposure to atmospheric particulate matter (PM) with a diameter < 2.5 μm (PM2.5), which can penetrate deep into the respiratory system, inducing oxidative stress and inflammation,5 and even translocate into the bloodstream.6
Such exposure can adversely affect health outcomes. Mortality rates have been found to increase in Sydney on days with high bushfire smoke pollution.7 Hospital admissions, emergency department attendances, ambulance call‐outs and general practitioner consultations, particularly for respiratory conditions, all increase during periods of severe PM2.5 levels from bushfires.8, 9, 10, 11 The risks from air pollution are amplified when combined with high temperatures during heatwaves, with an increased effect on mortality.12
Certain population groups are at higher risk from exposure to smoke, either because they typically breathe in more air per bodyweight and their organs are still developing (young children), spend more time outdoors (outdoor workers, homeless people), or are more vulnerable to smoke due to old age or a pre‐existing health condition (asthma, chronic obstructive pulmonary disease or other respiratory condition, cardiovascular illness, or diabetes). There is evidence that exposure to bushfire smoke during pregnancy is associated with reduced birthweight in babies and a higher risk of gestational diabetes in mothers.13, 14 People in lower socio‐economic groups are potentially at higher risk, as they may have poorer housing, and lower health literacy and ability to take preventive measures.
Health protection advice and trade‐offs
Current health protection advice related to bushfire smoke mainly focuses on short term measures aimed at reducing personal exposure to pollution. This includes advice to stay indoors with windows and doors closed, and reduce strenuous physical exercise outdoors, particularly if individuals experience health symptoms or have pre‐existing respiratory or cardiovascular conditions, when PM2.5 concentrations are increased. The PM2.5 national standard of 25 μg/m3 measured as a 24‐hour mean (National Environment Protection (Ambient Air Quality) Measure: https://www.legislation.gov.au/Details/F2016C00215) is consistent with the World Health Organization's air quality guidelines.15 However, PM2.5 concentrations presented as hourly averages are more useful for planning daily activities, as these better reflect current air quality, which can change rapidly during bushfire episodes. Currently, state and territory government departments use a range of different air quality metrics (such as a composite Air Quality Index based on multiple pollutants), averaging times and thresholds to stratify health messages into colour‐coded bands (very good, good, fair, poor, very poor, hazardous). The discrepancies in the presentation of this air quality information and related health advice across jurisdictions is confusing for the public.
General advice also includes having access to regular medication, such as asthma medication, checking on older neighbours, and seeking medical attention if needed. Such advice, however, has been tailored to brief air pollution episodes that last only a few hours or days. In situations like the 2019–20 bushfire smoke events in eastern Australia, where severe smoke pollution persists over longer periods (weeks to months) and affects large population centres, there is a need for more nuanced and detailed health advice based on location‐specific air quality data and forecasts.
Reducing prolonged or heavy physical exercise outdoors may become impractical over longer periods; for example, for school children and outdoor workers. Children and adults need to carry out a range of daily activities that involve spending time outdoors. Advice to reduce strenuous physical exercise outdoors becomes problematic over longer periods, owing to the recognised health benefits from active travel (ie, walking and cycling) and regular outdoor exercise, and potential lack of access to indoor sports facilities. We believe that more nuanced advice would encourage individuals to be guided by location‐specific air quality forecasts and the pattern of hourly PM2.5 concentrations at nearby air quality monitoring locations, and to plan their daily activities in ways that minimise exposure to pollution.
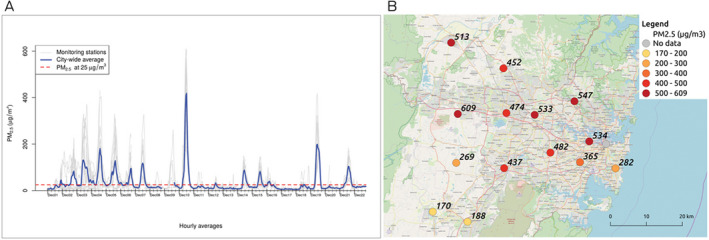
For example, PM2.5 levels were lower in most locations in Sydney in early morning hours during the December 2019 bushfire smoke episode (Box 1, A). Exercising outdoors and cycling or walking to school or work within this time window would help maintain good physical activity levels without substantially increasing exposure to smoke. Locations in the city's north were affected by much higher PM2.5 concentrations than some locations in the south at the highest peak of smoke on 10 December 2019 (Box 1, B). Real time information on the temporal and spatial variation of air pollution in all jurisdictions should be made available online and through other media to enable individuals to assess nearby air quality. Avoiding pollution from other sources (road traffic, cigarette smoking, etc) is also advisable, although widespread bushfire smoke is likely to dominate personal exposure to PM2.5 during severe smoke events.
Box 1. Hourly average PM2.5 levels, Sydney region, December 2019.
PM2.5 = atmospheric particulate matter with a diameter < 2.5 μm. A: Hourly average PM2.5 data between 1 and 22 December 2019, downloaded for 15 air quality monitoring stations in the Sydney region from the New South Wales Department of Planning, Industry and Environment database (https://www.dpie.nsw.gov.au/air-quality/search-for-and-download-air-quality-data). The straight line represents the Australian PM2.5 standard of 25 μg/m3 measured as a 24‐hour mean (National Environment Protection (Ambient Air Quality) Measure). Note that full data validation has not been completed for these records and they have only passed an initial automated validation process. B: Hourly average PM2.5 levels (μg/m3) at monitoring stations at the peak of the bushfire smoke event on 10 December 2019 at 1 pm.
Advice to stay indoors may be ineffective over longer periods. Older houses in Australia are often quite “leaky”, allowing bushfire smoke to penetrate indoors over time and creating unhealthy indoor air quality conditions. Well sealed and air conditioned indoor environments (typically, modern apartments and offices, libraries and shopping centres) can provide respite from smoke pollution, particularly if effective air filtration systems are in place. However, many urban residents exposed to bushfire smoke, such as older people and those with restricted mobility, may not have easy access to such places.
Temporary relocation to a different area or city could reduce exposure to air pollution during localised but persistent smoke episodes. However, relocation has its own risks and is impractical (particularly for older people and for those with cognitive or mobility problems), especially when larger geographical areas are affected by smoke.16 Temporary relocation to a dwelling with better indoor air quality (eg, a modern air conditioned apartment) within the same neighbourhood may be a more practical and less stressful solution for those at higher risk (eg, people with severe asthma, pregnant women, and older people).
The priority for those affected should be to create a clean air space within their home, by sealing doors and windows and using air conditioning and filtration if possible, where they can spend most of their time during prolonged periods of bushfire smoke.17 However, many people may not be able to afford air conditioning and filtration units. Homes should be ventilated during periods of cleaner outdoor air quality (eg, around midnight in Sydney in December 2019; Box 1, A), to cool down the homes and avoid build‐up of indoor pollutants.
Access to regular medication, including asthma preventers and relievers, statins or aspirin, is important for people with pre‐existing lung and heart conditions, and should be arranged in consultation with their GPs. Maintaining a healthy diet, with plenty of fruit and vegetables, and keeping well hydrated is likely to help reduce short and long term health effects. There is suggestive evidence that antioxidant and fish oil supplementation and dietary intake may have a protective effect against air pollution exposure;18, 19 however, more research is needed to support this.
Much of the media attention during periods of bushfire smoke relates to the use of facemasks. These are increasingly used by the general public in highly polluted Asian cities, particularly in China.20 Use of facemasks during brief air pollution episodes (outside occupational settings and extreme air pollution emergencies related to volcanic eruptions) is not routinely recommended by health authorities. This is because their effectiveness depends heavily on the facial fit, material and condition of the masks. Surgical masks may have reasonable filtration efficiency; however, their design generally confers poor facial fit and high inward leakage of PM2.5. 20 Professional P2 or N95 facemasks, which can provide very efficient filtration of PM2.5 if well fitted, are only designed for adults and can make breathing more difficult and increase thermal discomfort.20 More research is needed on the longer term health benefits and potential drawbacks of different types of facemasks for adults and children. Such masks do not confer protection from exposure to toxic gases in bushfire smoke (eg, carbon monoxide, nitrogen oxides and volatile organic compounds) that may be present closer to the fire front. There are a number of practical, medical and ethical considerations that should ultimately inform a decision about whether or not to recommend and distribute facemasks to the general public, outdoor workers and sensitive groups during air pollution emergencies.21, 22 Clear information about the effectiveness, benefits and drawbacks of different types of masks should be provided by health authorities to enable individuals, health professionals and employers to make informed decisions.
Risk communication
Nuanced and balanced public health communication that takes into account health risks, people's concerns and the effectiveness and practicality of protective measures is needed. Bushfire smoke alerts, real time air quality data and forecasts, and related health protection advice (Box 2) can help to reduce population exposure to hazardous air pollution, by enabling individuals, particularly those more sensitive, to plan their daily activities accordingly.
Box 2. Factsheet: bushfire smoke and health protection.
Source: Australian National University Research School of Population Health (https://rsph.anu.edu.au/news-events/news/how-protect-yourself-and-others-bushfire-smoke).

Environmental health literacy and a better understanding of the causes and effects of bushfires, and of the health consequences of air pollution more broadly, are important. There may be a misconception that smoke from burning wood or other organic fuels is “natural”, hence not harmful to health. There is no consistent scientific evidence supporting this belief. Toxicological studies have consistently demonstrated that particles derived from biomass burning can activate inflammatory, oxidative and genotoxic responses, similar to road traffic particles.23 A recent systematic review of epidemiological studies has shown higher asthma‐related effects for PM2.5 from landscape fire smoke compared with other sources.11
Comparison of pollutant concentrations with regulatory standards (eg, 24‐hour PM2.5 average of 25 μg/m3) highlights the scale of the problem and drives institutional action. However, local air quality can change very rapidly. At a personal level, real time hourly PM2.5 data and smoke forecasts are more helpful for planning daily activities to reduce exposure to air pollution. The AirRater smartphone app (https://airrater.org/) shares location‐specific hourly PM2.5 measurements from all jurisdictions. However, many locations affected by bushfire smoke do not have air quality monitoring stations. This highlights the need for increased air quality monitoring capabilities at state and territory level, including fixed monitoring sites, portable equipment and low cost sensors that can be rapidly deployed in a bushfire emergency.
It should be emphasised that there is no safe level of exposure to PM2.5 and any reduction in exposure reduces the risk of mortality and morbidity. Health professionals often compare outdoor air pollution with cigarette smoke, as both contain mixtures of toxic chemicals and have the same route of exposure (ie, inhalation) and common health outcomes (eg, lung cancer and other respiratory illnesses, heart disease, mortality risk). Although equivalence of bushfire smoke exposure with smoking a specific number of cigarettes is debatable,24 the broader comparison helps raise awareness of the long term health risks associated with outdoor air pollution, and reinforces preventive measures.
Conclusions, recommendations and evidence needs
The unprecedented bushfire smoke levels in eastern Australia have raised concerns about short and long term health consequences in the affected populations. They have also tested the existing health protection advice, which mainly focuses on shorter and more localised smoke episodes, and methods for communicating air quality information. Exposed populations increasingly seek advice on interventions (eg, facemasks, air cleaners, daily activities) that can help people self‐manage health risks from bushfire smoke. It is important that health professionals and patients, as well as healthy individuals and those at higher risk (eg, pregnant women and older people), develop a good understanding of the available health protection measures and their effectiveness and potential trade‐offs (Box 3).25, 26
Box 3. Benefits and drawbacks of personal risk reduction measures during bushfire smoke events.
| Risk reduction measure | Benefits | Drawbacks |
|---|---|---|
| Staying indoors (at home, workplace or school)17 |
|
|
| Reducing strenuous physical exercise outdoors17 |
|
|
| Using a clean air facility or public building with good indoor air quality (eg, air conditioned shopping centre, public library, community centre, sports centre)* |
|
|
| Portable air cleaners (air purifiers)17 | ||
| Face masks, including professional masks and surgical masks20, 21, 22 |
|
|
| Antioxidant supplements, fish oils (omega‐3 fatty acids), and other dietary advice18, 19 |
|
|
| Asthma medication, aspirin, statins, other medications17 |
|
|
| Smoke forecasts, near real time air quality data (PM2.5), air pollution and health alerts5 | ||
| Temporary relocation16 |
|
|
HEPA = high efficiency particulate air. PM2.5 = atmospheric particulate matter with a diameter < 2.5 μm. * Based on the authors’ expert opinion.
Public access to local, user‐friendly air quality information and reliable smoke forecasts is essential for managing personal exposure as well as clinical deterioration in sensitive individuals. We strongly recommend that all Australian jurisdictions present actual hourly PM2.5 data rather than an index. Real time, hourly averaged PM2.5 concentrations are the most appropriate metric to guide personal behaviour that minimises exposure to bushfire smoke. Health messages need to be evidence‐informed and specific for at‐risk groups and the general public. More government investment is needed in air quality monitoring, forecasting and research on public health messaging, and exposure reduction measures to protect Australians from bushfire smoke.
Consistency of air quality information and related public health advice across jurisdictions is essential. It is time for an independent national expert committee on air pollution and health protection to be established to support environmental health decision making in Australia. This new expert committee should have a clear mandate and resources to develop evidence‐based, accurate, practical and consistent advice on health protection against bushfire smoke, and air pollution more broadly, across jurisdictions.
Managing the health impacts of fire smoke should be integral to landscape fire planning and bushfire emergency response. Close collaboration between health, education, environmental, fire management and emergency response agencies is essential for achieving the best overall outcomes for population health and wellbeing. Further research is needed into the medium and longer term impacts of bushfire smoke, as well as the effectiveness and health equity implications of related health protection advice. Working towards ambitious climate change mitigation targets is an essential long term strategy for managing the underlying causes of the increasing bushfire risk in Australia and overseas.
Competing interests
Sotiris Vardoulakis has received funding support from the UK National Institute for Health Research, Medical Research Council, Natural Environment Research Council, Public Health England, EU Horizon 2020, and Dyson Ltd. Geoffrey Morgan and Ivan Hanigan receive funding support from the Australian National Health and Medical Research Council.
Provenance
Not commissioned; externally peer reviewed.
Acknowledgements
This research was undertaken with support from the Australian National University College of Health and Medicine, and the assistance of resources from the Centre for Air pollution, energy and health Research (CAR). We used the CAR Data and Analysis Technology platform (https://cardat.github.io) to analyse data.
Podcast with Sotiris Vardoulakis available at mja.com.au/podcasts
References
- 1. Harris S, Lucas C. Understanding the variability of Australian fire weather between 1973 and 2017. PLoS One 2019; 14: e0222328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Di Virgilio G, Evans JP, Blake SAP, et al. Climate change increases the potential for extreme wildfires. Geophys Res Lett 2019; 46: 8517–8526. [Google Scholar]
- 3. Beggs PJ, Zhang Y, Bambrick H, et al. The 2019 report of the MJA–Lancet Countdown on health and climate change: a turbulent year with mixed progress. Med J Aust 2019; 211: 490–491.e21. https://www.mja.com.au/journal/2019/211/11/2019-report-mja-lancet-countdown-health-and-climate-change-turbulent-year-mixed [DOI] [PubMed] [Google Scholar]
- 4. Johnston FH. Understanding and managing the health impacts of poor air quality from landscape fires. Med J Aust 2017; 207: 229–230. https://www.mja.com.au/journal/2017/207/6/understanding-and-managing-health-impacts-poor-air-quality-landscape-fires. [DOI] [PubMed] [Google Scholar]
- 5. Lodovici M, Bigagli E. Oxidative stress and air pollution exposure. J Toxicol 2011; 2011: 487074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brook RD, Rajagopalan S, Pope CA 3rd, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 2010; 121: 2331–2378. [DOI] [PubMed] [Google Scholar]
- 7. Morgan G, Sheppeard V, Khalaj B, et al. Effects of bushfire smoke on daily mortality and hospital admissions in Sydney. Australia. Epidemiology 2010; 21: 47–55. [DOI] [PubMed] [Google Scholar]
- 8. Martin KL, Hanigan IC, Morgan GG, et al. Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994‐2007. Aust. N Z J Public Health 2013; 37: 238–243. [DOI] [PubMed] [Google Scholar]
- 9. Johnston FH, Purdie S, Jalaludin B, et al. Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996‐2007: a case‐crossover analysis. Environ Health 2014; 13: 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salimi F, Henderson SB, Morgan GG, et al. Ambient particulate matter, landscape fire smoke, and emergency ambulance dispatches in Sydney. Australia. Environ Int 2017; 99: 208–212. [DOI] [PubMed] [Google Scholar]
- 11. Borchers Arriagada N, Horsley JA, Palmer AJ, et al. Association between fire smoke fine particulate matter and asthma‐related outcomes: Systematic review and meta‐analysis. Environ Res 2019; 179: 108777. [DOI] [PubMed] [Google Scholar]
- 12. Shaposhnikov BD, Revich BB, Bellander BT, et al. Mortality related to air pollution with the Moscow heat wave and wildfire of 2010. Epidemiology 2014; 25: 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holstius DM, Reid CE, Jesdale BM, et al. Birth weight following pregnancy during the 2003 Southern California wildfires. Environ Health Perspect 2012; 120: 1340–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Melody SM, Ford JB, Wills K, et al. Maternal exposure to fine particulate matter from a large coal mine fire is associated with gestational diabetes mellitus: a prospective cohort study. Environ Res 2019; 108956 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization Europe . Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Global update 2005. Copenhagen: WHO, 2006. http://www.euro.who.int/__data/assets/pdf_file/0005/78638/E90038.pdf?ua=1 (viewed Jan 2020). [Google Scholar]
- 16. Willoughby M, Kipsaina C, Ferrah N, et al. Mortality in nursing homes following emergency evacuation: a systematic review. J Am Med Dir Assoc 2017; 18: 664–670. [DOI] [PubMed] [Google Scholar]
- 17. Laumbach R, Meng Q, Kipen H. What can individuals do to reduce personal health risks from air pollution? J Thorac Dis 2015; 7: 96–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Whyand T, Hurst JR, Beckles M, et al. Pollution and respiratory disease: can diet or supplements help? A review. Respir Res 2018; 19: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lin Z, Chen R, Jiang Y, et al. Cardiovascular benefits of fish‐oil supplementation against fine particulate air pollution in China. J Am Coll Cardiol 2019; 73: 2076–2085. [DOI] [PubMed] [Google Scholar]
- 20. Cherrie JW, Apsley A, Cowie H, et al. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ Med 2018; 75: 446–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McDonald F, Horwell CJ, Wecker R, et al. Facemask use for community protection from air pollution disasters: An ethical overview and framework to guide agency decision making. Int J Disaster Risk Reduction 2020; 43: 101376. [Google Scholar]
- 22. Huang W, Morawska L. Face masks could raise pollution risks. Nature 2019; 574: 29–30. [DOI] [PubMed] [Google Scholar]
- 23. Johnston HL, Mueller W, Steinle S, et al. How harmful is particulate matter emitted from biomass burning? A Thailand perspective Curr Pollut Rep 2019; 5: 353–377. [Google Scholar]
- 24. Muller RA, Muller EA. Air pollution and cigarette equivalence. Berkeley Earth. http://berkeleyearth.org/air-pollution-and-cigarette-equivalence/ (viewed Jan 2020).
- 25. Australian National University Research School of Population Health. How to protect yourself and others from bushfire smoke. https://rsph.anu.edu.au/news-events/news/how-protect-yourself-and-others-bushfire-smoke (viewed Jan 2020).
- 26. Centre for Air pollution, energy and health Research. Bushfire smoke: what are the health impacts and what can we do to minimise exposure? 10 Dec 2019. https://www.car-cre.org.au/factsheets (viewed Jan 2020).


