Abstract
Objectives
To assess the frequency of maternal death (MD) due to cardiac disease in low‐ and middle‐income countries (LMIC).
Methods
Systematic review searching Medline, EMBASE, Web of Science, Cochrane Library, Emcare, LILACS, African Index Medicus, IMEMR, IndMED, WPRIM, IMSEAR up to 01/Nov/2017. Maternal mortality reports from LMIC reviewing all MD in a given geographical area were included. Hospital‐based reports or those solely based on verbal autopsies were excluded. Numbers of MD and cardiac‐related deaths were extracted. We calculated cardiac disease MMR (cMMR, cardiac‐related MD/100 000 live births) and proportion of cardiac‐related MDs among all MDs. Frequency of cardiac MD was compared with the MMR of the country.
Results
Forty‐seven reports were included, which reported on 38,486 maternal deaths in LMIC. Reported cMMR ranged from 0/100 000 live births (Moldova, Ghana) to 31.9/100 000 (Zimbabwe). The proportion of cardiac‐related MD ranged from 0% (Moldova, Ghana) to 24.8% (Sri Lanka). In countries with a higher MMR, cMMR was also higher. However, the proportion of cardiac‐related MD was higher in countries with a lower MMR.
Conclusions
The burden of cardiac‐related mortality is difficult to assess due limited availability of mortality reports. The proportion of cardiac deaths among all MD appeared to be higher in countries with a lower MMR. This is in line with what has been called ‘obstetric transition’: pre‐existing medical diseases including cardiac disease are becoming relatively more important where the MMR falls.
Keywords: cardiac disease, maternal mortality, low‐ and middle‐income countries
Abstract
Objectifs
Evaluer la fréquence des décès maternels (DM) dus à une maladie cardiaque dans les pays à revenu faible ou intermédiaire (PRFI).
Méthodes
Revue systématique en recherchant sur Medline, EMBASE, Web of Science, Cochrane Library, Emcare, LILACS, African Index Medicus, IMEMR, IndMED , WPRIM, IMSEAR jusqu'au 1er novembre 2017. Les reports de mortalité maternelle provenant des PRFI examinant tous les DM dans une zone géographique donnée ont été inclus. Les reports en milieu hospitalier ou ceux basés uniquement sur des autopsies verbales ont été exclus. Le nombre de DM et de décès liés à la maladie cardiaque a été extrait. Nous avons calculé le taux de mortalité maternelle par maladie cardiaque (TMMc, DM lié à un effet cardiaque/100.000 naissances vivantes) et la proportion de DM cardiaques parmi tous les DM. La fréquence des DM cardiaques a été comparée au TMM du pays.
Résultats
47 reports ont été inclus, faisant état de 38.486 décès maternels dans les PRFI. Le TMMc rapporté allait de 0/100.000 naissances vivantes (Moldavie, Ghana) à 31,9/100.000 (Zimbabwe). La proportion de DM d'origine cardiaque variait de 0% (Moldavie, Ghana) à 24,8% (Sri Lanka). Dans les pays avec un TMM plus élevé, le TMMc était également plus élevé. Cependant, la proportion de DM d'origine cardiaque était plus élevée dans les pays où le TMM était inférieur.
Conclusions
La charge de la mortalité liée à une maladie cardiaque est difficile à évaluer en raison de la disponibilité limitée des rapports de mortalité. La proportion de décès cardiaques parmi tous les DM semble être plus élevée dans les pays où le TMM est plus faible. Cela correspond à ce que l'on a appelé la «transition obstétricale»: les maladies médicales préexistantes, y compris les maladies cardiaques, deviennent relativement plus importantes là où le TMM chute.
Mots‐clés: maladie cardiaque, mortalité maternelle, pays à revenu faible ou intermédiaire
Introduction
It is generally assumed that cardiac disease is rare in women of reproductive age. However, in high‐income countries such as the United Kingdom, the United States of America or the Nordic countries, cardiac disease has become the commonest cause of maternal deaths (MD) [1, 2, 3]. Data regarding the number of maternal deaths due to cardiac disease in low‐ and middle‐income countries (LMIC) are scarce. Attention to cardiac disease as a cause of maternal mortality is rare compared with conditions such as hypertensive disorders, postpartum haemorrhage and HIV/AIDS, which are regarded as more important causes [4, 5]. However, the prevalence of cardiac disease is most likely underreported in LMIC due to inadequate diagnostic means and poor registration [6, 7, 8].
Global progress reports on maternal mortality have emphasised the increased importance of indirect maternal deaths due to pre‐existing medical conditions in LMICs that have managed to reduce their maternal mortality ratio (MMR) [5, 9]. It is likely that the role of cardiac disease in maternal deaths could become increasingly important where other causes, primarily direct obstetric causes, become less prevalent.
This is the first systematic review to assess the frequency of maternal deaths due to cardiac disease based on national and regional maternal mortality reports from LMIC and to compare these findings with the MMR of that country.
Methods
Search strategy and selection criteria
Maternal mortality reports from LMIC were identified by a systematic review of literature. Medline (using Pubmed), EMBASE, Web of Science, Cochrane Library, Emcare, LILACS, African Index Medicus, IMEMR, IndMED, WPRIM and IMSEAR databases were searched from January 1 2000 to November 1 2017 with the assistance of a qualified librarian at the Leiden University Medical Centre (Appendix S1). We screened the website of the Maternal Death Surveillance and Response (MDSR) Action Network and references from the maternal mortality country profiles of the WHO for eligible publications [10, 11]. If a publication mentioned a different or more recent report, this reference was searched, or, if it could not be retrieved, the first author of the referring publication was contacted to obtain the report. The systematic review was conducted following the PRISMA guidelines [12].
Regional and national maternal death reviews (MDR) performed in a low‐ or middle‐income country were eligible if the aim of the study was to review all maternal deaths (MD) in a given geographical area, preferably including out‐of‐facility deaths. However, a facility‐based approach, exclusively reviewing facility‐based MDs, is commonly used in regions with high institutional birth rates and in several mortality reports of high quality such as the confidential enquiries into maternal deaths of South Africa, Moldova and Kerala region, India [13, 14, 15, 16, 17, 18, 19]. Therefore, we considered reports documenting MDs from all health facilities of all levels within the study area, including health posts and health centres. Reports from single or non‐population‐based groups of hospitals were excluded as the data were unlikely to be representative of the study area. The World Bank rating of 2017 was used to assess whether a country was considered an LMIC [20].
Reports were included if maternal deaths met the WHO definition of ‘deaths of women while pregnant or within 42 days of termination of pregnancy from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes’, and if the total number of MD and the number of deaths specified per cause were provided [21]. To identify MD due to cardiac disease, one of the following identifiers had to be used: cardiac disease, heart disease or the specific cardiac condition such as rheumatic heart disease (RHD), any type of cardiomyopathy or congenital heart disease. Authors of reports using less specific definitions such as ‘cardiovascular disorders’ or ‘cardiac failure’ were contacted to provide the exact number of MD due to cardiac disease. If these data could not be retrieved, the report was excluded.
Studies exclusively based on verbal autopsy, sisterhood methods or household survey were excluded since these were considered insufficient to robustly identify MD due to cardiac disease. Studies with a sample size below twenty were excluded. Reports were screened for duplication. If one of the duplicate reports contained data from a larger study area or longer study period, this report was included. Full text had to be available in English, French, German, Spanish or Portuguese.
Study selection was done by two independent researchers (SH and AP). The opinion of a third researcher (TA) was sought if consensus was not reached. Data extraction was performed by one author (SH) and reviewed by a second (AP).
Data analysis
To assess the quality of the included reports, we evaluated the methods used for identification of MD in the study area, and those for establishing cause of death, as well as the level of expertise available for case review. For each item, the best available method is listed at the top in Table 1. First, we evaluated robustness of MD identification in the study area and whether out‐of‐facility deaths were included. We considered MD identification of the highest quality if there was a system in place to trace maternal deaths in an enhanced manner, including identifying out‐of‐facility deaths, for example through a Reproductive Age Mortality Survey (RAMOS), involvement of communities and/or analysis of information from mortuaries. Secondly, the method used to establish the cause of maternal deaths was assessed. At facility level, establishment of the cause of death could range from a MD notification form, filled in by the attending healthcare worker, up to a facility‐based audit. At central level, for example regional or national level, review of the cause of death could range from analysing information of the MD notification forms up to a complete review of medical records. Finally, level of expertise for case review was based on the presence of an obstetrician and additional medical specialists such as anaesthetists, physicians, pathologists or paediatricians.
Table 1.
Quality assessment of mortality reports
| Identification of MD | Review at facility level | Review at central level | Cause of death established by |
|---|---|---|---|
| OFD included, systematically traced | Facility‐based audit | Audit of complete file | Panel with O&G and non‐O&G specialists |
| OFD included, but not systematically traced | MD notification form | Review of MD notification form | Panel with O&G specialist |
| Excluded women who died outside a facility | None | Staff at facility | |
| Other |
Presented are the different methods used to identify maternal deaths in the study area, to review cases at facility and central level and which level of expertise was available to establish cause of death. The best available method is listed at the top of each section. MD, maternal death; OFD, out‐of‐facility death; O&G, obstetrics and gynaecology.
We did not produce a summary quality measure since we considered the robustness of MD identification of equal importance to the methods and level of expertise used to establish cause of death. For some reports, a high level of expertise was available at central level to review all cases, but identification of MD and quality of data collection at facility level was poor. On the contrary, some reports used a well‐functioning MD notification system but had limited expertise available for case review. The total number of MD, deaths from cardiac disease and the study period were extracted from each report. The proportion of cardiac MDs among all MDs (%cMD) was calculated by dividing the number of reported cardiac MD by the total number of MD and is presented as a percentage. The MMR was calculated as the number of reported MD per 100 000 live births and cardiac disease MMR (cMMR) as the number of reported cardiac‐related MD per 100 000 live births. For population‐based studies, the MMR was extracted from the report. Reports were defined as population‐based when the aim of the study was to review all MD that occurred during the study period in the study area, including women who died outside a health facility. For facility‐based reports or if the report did not provide data to calculate an MMR, the national MMR estimated by the WHO for the closest corresponding year of the study period was extracted from the ‘Maternal mortality country profiles’ [11]. Reports mentioning zero cardiac deaths were assessed for possible missed cardiac deaths. If the report included deaths due to unknown causes or unclear diagnoses, for example death due to anaemia, sudden death or out‐of‐facility death and no autopsy was performed, this meant that MDs due to cardiac disease were possibly missed. In such cases, the number of cardiac deaths was reported as ‘missing’, and the report excluded from data analysis. The level of income of a country was categorised as either upper MIC, lower MIC or LIC based on the World Bank rating at the time of data collection of each country [20].
For all reports, the relation of the frequency of cardiac‐related MD with the MMR of its country was assessed using plots. For countries with multiple reports of different study periods, but reporting data of the same geographical area, progress over time was explored using detailed plots. Data regarding the total number of cardiac MD were plotted in a world map. When multiple reports were available for one country, the most recent report, covering the largest geographical area and/or of highest quality, was used for comparison. Selection process is detailed further in Appendix S2.
Considering the low number and heterogeneity of the included reports, frequency of cardiac MD in relation to the MMR or time was not compared statistically. Data were analysed using SPSS version 22 (IBM Corp., Armonk, NY). Plots were drafted with Prism version 8.1 (GraphPad Software). The review was registered with PROSPERO (CRD42018089452). All results are presented in the tables and figures and therefore not published in a separate online database.
Results
Forty‐seven maternal mortality reports were included, reporting on a total of 38,486 maternal deaths in LMIC [13, 14, 15, 16, 17, 18, 19, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61]. Study selection is summarised in Figure 1. Titles and abstracts of 2064 identified records were screened, which resulted in 132 eligible records. Full‐text articles of these records were evaluated and 85 reports excluded. In 11 of 132 reports, it was unclear whether the definition used comprised maternal deaths due to cardiac disease alone. In four reports, the quality of the methods section was insufficient to assess the methods used to identify MD and establish the cause of death. Three hospital‐based reports reviewed MD for one or multiple hospitals only but were not population‐based. Two regional reports from South Africa were excluded as national reports were available for the same study period.
Figure 1.
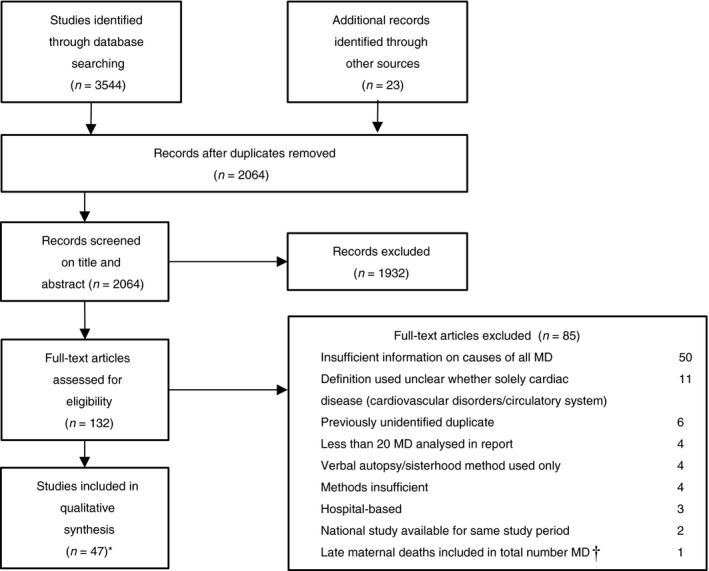
Flowchart showing selection of studies included in review. *The corresponding author of a report from Rwanda confirmed that MDs described as ‘due to cardiac failure’ were all MD due to cardiac disease. The report from Moldova for 2006–2008 only mentioned the total number of indirect deaths. The author of this report confirmed none of these deaths were caused by cardiac disease. The same author provided us with the mortality data of the review of 2009–2013, of which the report in English is not yet available. †Late maternal death is a death of a woman from direct or indirect causes more than 42 days but less than one year after termination of pregnancy. MD, Maternal death.
The 47 included reports included maternal mortality data from 29 countries. Characteristics of these reports are presented in Table 2. The included reports presented data from eight LIC, thirteen lower MIC and eight upper MIC. Twenty reports presented regional maternal mortality data, and twenty‐seven reported national data. The study period was clearly defined in all studies and ranged from 1992 until 2015. Twenty‐seven studies were population‐based [23, 26, 27, 28, 31, 33, 34, 37, 38, 40, 41, 43, 44, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 57, 59, 60, 61]. Fourteen reports were facility‐based [13, 14, 15, 16, 17, 18, 19, 22, 32, 35, 42, 45, 56, 58]. The proportion of reviewed deaths outside facilities ranged from 1.8% (Botswana, 2010) to nearly half of the reviewed deaths in Zimbabwe (49.3%), Pakistan (50.0%), Bangladesh (51.6%) and Nepal (53.8%) [48, 50, 53, 57]. In 21 out of 27 population‐based reports, an MMR was extracted directly from the report [23, 26, 27, 31, 33, 34, 37, 38, 40, 41, 43, 46, 47, 48, 49, 50, 54, 55, 57, 59, 60]. Five reports stated zero cardiac deaths of which data were reported as missing of the reports from Tanzania, Malawi and Sudan as possible deaths due to cardiac disease were missed (Appendix S2) [14, 25, 36, 45, 51]. In these reports, cause of death was not known (330/1433 deaths in the report from Malawi), or unclear (75/898 deaths due to anaemia in the report from Sudan, 213/1433 deaths due to anaemia in the report from Malawi, 1/45 death due to anaemia and one sudden death in the report from Tanzania and in all three reports no autopsies were performed).
Table 2.
Overview of 47 included maternal mortality reports
| Country | LIC/l‐MIC/u‐MIC | MMR | Period | Cardiac MD/total MD | Proportion cardiac MD (%) | cMMR | OFD included | Review at facility level | Review central level | Case review by |
|---|---|---|---|---|---|---|---|---|---|---|
| Bangladesh | LIC | 479† | 1996–1997 | 291/7086 | 4.1% | 19.7 | Yes | Research team | None | Recent medical graduates |
| Ethiopia | LIC | 523† | 2008 | 14/633 | 2.2% | 11.6 | Yes | MD notification form | None | Staff at facility |
| Ghana, Upper West reg. | LIC | 325† | 2009 | 0/47 | 0.0% | 0.0 | if reported | MD notification form | Audit of complete file | Panel, expertise unclear |
| Ghana, Accra reg* | LIC | 467† | 2002 | 3/178 | 1.7% | 7.9 | Yes | None | Audit of complete file | Panel with O&G specialist |
| Malawi | LIC | 629† | 2008–2012 | **/1433 | N/A | N/A | No | Facility audit | CEMD, audit of complete file | Panel with O&G specialist |
| Malawi, Central reg.* | LIC | 648† | 2007 | 1/43 | 2.3% | 15.1 | No | Facility audit | None | Staff at facility |
| Nepal, 8 reg. | LIC | 229‡ | 2008–2009 | 11/160 | 6.9% | 15.7 | Yes | Facility audit | None | Staff at facility |
| Rwanda | LIC | 381† | 2009–2013 | 23/987 | 2.3% | 8.9 | No | Facility audit | None | Staff at facility |
| Tanzania, Arusha reg. | LIC | 961† | 1995–1996 | **/45 | /A | N/A | Yes | None | Audit of complete file | Panel with O&G specialist |
| Zimbabwe | LIC | 725‡ | 2006 | 16/364 | 4.4% | 31.9 | Yes | MD notification form | Review of MD notification forms | Staff at facility |
| Egypt, Dakahlia reg. | l‐MIC | 71‡ | 2004–2005 | 15/171 | 8.8% | 6.3 | Yes | MD notification form | Audit of complete file | Panel, expertise unclear |
| Egypt* | l‐MIC | 84‡ | 2000 | 45/580 | 7.8% | 6.5 | Yes | None | Audit of complete file | Panel with O&G and non‐O&G specialists |
| El Salvador | l‐MIC | 50‡ | 2011 | 4/64 | 6.3% | 3.2 | Yes | MD notification form | Audit of complete file | Panel, expertise unclear |
| Guatemala, ‘dep. of Guatemala’ | l‐MIC | 156‡ | 1993–1996 | 2/435 | 0.5% | 0.7 | Yes | None | Audit of complete file | Data clerk |
| India, Kerala reg. | l‐MIC | 29¶ | 2004–2009 | 32/501 | 6.4% | 1.9 | No | MD notification form | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Jamaica* | l‐MIC | 95‡ | 1998–2003 | 12/232 | 5.2% | 4.9 | Yes | None | Audit of complete file | Panel, expertise unclear |
| Jamaica | l‐MIC | 96‡ | 1993–1995 | 3/141 | 2.1% | 2.1 | Yes | None | Audit of complete file | Panel, expertise unclear |
| Jordan | l‐MIC | 19‡ | 2007–2008 | 8/76 | 10.5% | 2.0 | Yes | None | Audit of complete file | Panel, expertise unclear |
| Moldova* | l‐MIC | 34† | 2009–2013 | 2/49 | 4.1% | 1.4 | No | MD notification form | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Moldova | l‐MIC | 39† | 2006–2008 | 0/29 | 0.0% | 0.0 | No | MD notification form | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Morocco, 6 priority reg. | l‐MIC | 121‡ | 2015 | 7/152 | 4.6% | 5.6 | Yes | MD notification form | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Morocco* | l‐MIC | 153† | 2009 | 16/303 | 5.3% | 8.1 | If reported | MD notification form | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Pakistan, Sindh reg. | l‐MIC | 279‡ | 2006–2008 | 3/72 | 4.2% | 11.6 | Yes | MD notification form | None | Staff at facility |
| Russia, St. Petersburg | l‐MIC | 43‡ | 1992–2003 | 12/179 | 6.7% | 2.9 | Yes | Facility audit | None | Research team with O&G specialist |
| Sri Lanka* | l‐MIC | 34‡ | 2015 | 28/113 | 24.8% | 8.4 | Yes | District audit | Audit of complete file | Panel with O&G and non‐O&G specialists |
| Sri Lanka | l‐MIC | 32‡ | 2014 | 16/112 | 14.3% | 4.6 | Yes | District audit | Audit of complete file | Panel with O&G and non‐O&G specialists |
| Sudan | l‐MIC | 349† | 2010 | **/898 | N/A | N/A | If reported | MD notification form | Review of MD notification forms | Panel, expertise unclear |
| Swaziland | l‐MIC | 586† | 2000–2001 | 2/43 | 4.7% | 27.3 | No | None | Audit of complete file | Panel, expertise unclear |
| Botswana | u‐MIC | 129† | 2015 | 2/73 | 2.7% | 3.5 | Unknown | Unclear | National statistics | Unknown |
| Botswana* | u‐MIC | 169† | 2010 | 7/55 | 12.7% | 21.5 | Yes | MD notification form | Audit of complete file | Panel, expertise unclear |
| China, Wuhan reg. | u‐MIC | 14,5‡ | 2001–2012 | 8/91 | 8.8% | 1.3 | Yes | MD notification form | Audit of complete file | Panel, expertise unclear |
| China, Henan reg. | u‐MIC | 45,5‡ | 1996–2009 | 90/1129 | 8.0% | 3.6 | Yes | MD notification form | Audit of complete file | Panel with O&G specialist |
| China, Shanghai reg. | u‐MIC | 20,5‡ | 2000–2009 | 24/262 | 9.2% | 1.9 | Yes | MD notification form | Audit of complete file | Panel with O&G specialist |
| China, Zhejiang reg. | u‐MIC | 58† | 1995–2008 | 95/901 | 10.5% | 6.1 | Yes | MD notification form | Audit of complete file | Panel, expertise unclear |
| China combined§ | u‐MIC | 35§ | 1995–2012 | 217/2383 | 9.1% | 3.2 | ||||
| Fiji | u‐MIC | 34† | 2008–2012 | 5/37 | 13.5% | 4.6 | If reported | MD notification form | None | Staff at facility |
| Irak | u‐MIC | 27‡ | 2010–2012 | 79/1039 | 7.6% | 2.1 | Yes | MD notification form | Audit of complete file | Panel with O&G specialist |
| Iran, Yazd reg. | u‐MIC | 34† | 2002–2011 | 8/40 | 20.0% | 6.8 | Unknown | MD notification form | Unclear | Unclear |
| Malaysia* | u‐MIC | 28,7‡ | 2009–2011 | 65/430 | 15.1% | 4.3 | Yes | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Malaysia | u‐MIC | 27‡ | 2006–2008 | 49/396 | 12.4% | 3.4 | Yes | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa* | u‐MIC | 138† | 2014 | 49/1238 | 4.0% | 5.5 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 154† | 2011–2013 | 169/4333 | 3.9% | 6.0 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 154† | 2008–2010 | 157/4867 | 3.2% | 5.0 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 112† | 2005–2007 | 97/3959 | 2.5% | 2.7 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 112† | 2002–2004 | 85/3296 | 2.6% | 2.9 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 85† | 1999 | 23/584 | 3.9% | 3.3 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| South Africa | u‐MIC | 85† | 1998 | 28/565 | 5.0% | 4.2 | No | Facility audit | CEMD, audit of complete file | Panel with O&G and non‐O&G specialists |
| Surinam | u‐MIC | 130‡ | 2010–2014 | 2/65 | 3.1% | 4.0 | Yes | MD notification form | Audit of complete file | Panel with O&G and non‐O&G specialists |
CEMD, Confidential enquiry into maternal deaths; LIC, low‐income country; l‐MIC, lower middle‐income country; u‐MIC, upper middle‐income countries; MD, maternal death; MMR, maternal mortality ratio/100 000 live births; cMMR, cardiac‐related maternal mortality ratio/100 000 live births; N/A, not available; OFD, out‐of‐facility deaths; O&G, obstetrics and gynaecology.
Data report used for figure 3, as most representative data for country.
MMR estimation of WHO, population‐based study but no MMR available in report or not population‐based study.
MMR from report, population‐based study.
MMR based on average of 4 reports from China.
MMR from report used even though facility‐based report. The region is known for a consistently lower MMR than the national MMR due to better health indicators, more details available in supplement 2.
Missing data.
Reported cMMR ranged from 0/100 000 live births in reports from Ghana and Moldova to 31.9/100 000 live births in Zimbabwe [14, 36, 48]. The proportion of reported cardiac‐related MD among all MD ranged from 0% in reports from Ghana and Moldova to 24.8% in Sri Lanka [14, 36, 38]. Figure 2 shows the relation of the frequency of cardiac MD with the MMR of its country. Level of economy of the countries is indicated by colour. Reports from countries with a lower MMR appear to have a higher proportion of cardiac MD (Figure 2a), but the cardiac MMR is higher in countries with a higher MMR (Figure 2b). In reports from LIC, the proportion of cardiac MDs appeared to be lower compared with MIC; however, the cMMR is higher in LIC. For six countries, multiple reports of the same study area were available, and trends over time were plotted in Figure 2c. For five countries, the same methods were used to collect data over time, whereas two different methods were used for the two reports from Botswana.
Figure 2.
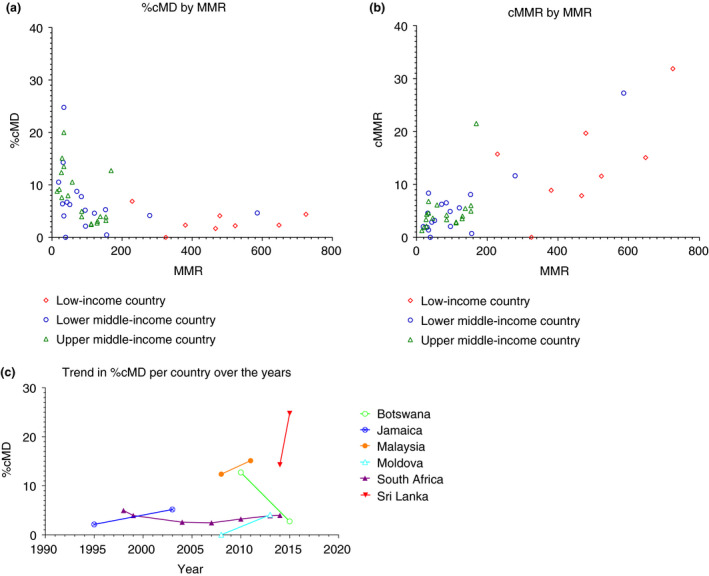
Three plots showing the trends of maternal deaths due to cardiac disease in relation to the MMR of its country and over time. (a) The relation of the proportion of cardiac‐related maternal deaths with the MMR of its country. All included studies are plotted. (b) The relation of cMMR with the MMR of its country. All included studies are plotted. (c) For the available studies with multiple reports, the proportion of cardiac‐related maternal deaths over time is plotted. cMD, cardiac‐related maternal death; MMR, maternal mortality ratio/100 000 live births; cMMR, cardiac‐related maternal mortality ratio/100 000 live births.
Figure 3 shows the cardiac MMR for each country. For this figure, the national or most recent study was selected if multiple reports were available for these countries, Table 2. For Botswana, Ghana and Malawi, a regional or less recent report was considered to have more representative data and selected for country comparison (Appendix S2). For China, four regional reports with similar methods were available. The findings of these four reports were combined for country comparison in Figure 3.
Figure 3.
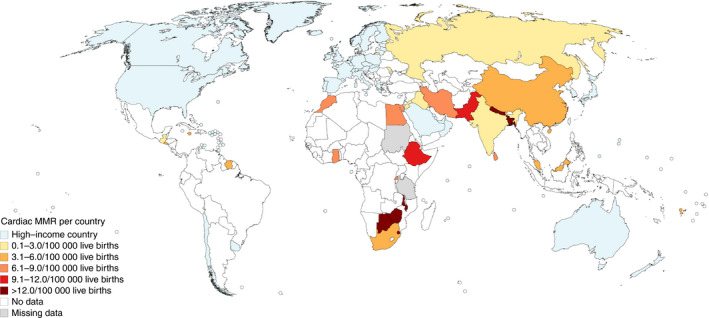
World map showing incidence of maternal deaths due to cardiac disease per country. MMR, maternal mortality ratio.
The included reports used different methods to establish the cause of maternal deaths. In six reports, information regarding the cause of death was only based on maternal death notification forms, filled in at facility level (Table 2) [25, 28, 30, 39, 48, 50]. The report from Botswana in 2015 was a national statistics mortality report. In this report, it was unclear whether the cause of death was based on information from death certificates, maternal death notification forms or audits [29]. Four reports were based on information from audits at facility level only [34, 42, 56, 57]. For the 36 remaining reports, review of medical records was performed at regional or national level. Table 2 indicates the level of expertise available to establish cause of death. In the reports from Guatemala and Botswana (2015), the actual number of deaths due to cardiac disease may have been higher, but the definitions applied were unclear, thus we have reported the minimum number. In both reports, two maternal deaths due to cardiomyopathy were presented. In the report from Botswana, another eight MD due to ‘diseases of the circulatory system’ were documented and for Guatemala four maternal deaths due to ‘cardiovascular problems’. We were unable to contact the authors, so we report the number of cardiac MD as two for both reports [29, 40].
Discussion
This review shows a substantial incidence of maternal deaths due to cardiac disease in LMIC. In the included reports, cardiac‐related MMR was highest in countries with a high MMR, but the proportion of cardiac deaths among all maternal deaths appeared to be higher in countries with a lower MMR. Probably, we identified only ‘the tip of the iceberg’, and the number of MD due to cardiac disease is likely to be even be higher.
Health facilities are insufficiently equipped to identify cardiac deaths and cardiac MD might have been missed. In many LMIC, women do not have access to health facilities equipped with the diagnostic means or clinicians to diagnose cardiac disorders and it is not uncommon that a cardiac disorder is only identified during pregnancy when a woman presents in extremis with heart failure [6, 7, 8]. This might explain the finding of a lower proportion of cardiac deaths in countries with a lower level of income. A study undertaken in Eritrea identified rheumatic heart disease (RHD) in 2.3% of asymptomatic pregnant women during antenatal visits [62]. The Sudanese report included in our review suggested that there were no cardiac deaths although the country has a high prevalence of RHD among young women [7, 63, 64]. Underdiagnosis of cardiac disease in LMIC may explain the wide range of maternal mortality from 0 to 34% that has been reported among pregnant women with cardiac disease [6, 8, 65, 66, 67, 68, 69]. It is likely that only the most severe cases are identified in settings with limited access to facilities where cardiac disease can be diagnosed. Lastly, many maternal deaths due to medical conditions including cardiac disease happen between six weeks and one year after the end of pregnancy and are therefore not included in the WHO definition of MD [4, 66].
Quality of the included reports varied and might have influenced the incidence figures as well. For three reports, we had to report missing data due to the high likelihood of missed cardiac MD. The national report from Malawi noted a high level of missing data and although MD is notifiable by law, zero MDs were reported at central level [45]. The report from Ethiopia had information on only 6% of the expected number of MD [28]. No medical doctor was involved to confirm the cause of death for two reports [40, 53]. Some reports used unclear definitions like cardiovascular disorder, which includes for example stroke. These were excluded since we could not establish the number of deaths due to cardiac disease. In four reports, half of the cases were out‐of‐facility deaths and no autopsies were performed [48, 50, 53, 57]. Possible cardiac MDs were missed in these reports. Autopsy can assist in establishing the underlying cause of the MD, and several cardiac‐related MDs were identified by autopsy in LMIC [70, 71].
Cardiac‐related MMR was highest in countries with a high MMR, but the proportion of cardiac deaths among all maternal deaths appeared to be larger in countries with a lower MMR. This is an important finding since this is in line with what has been titled the ‘obstetric transition model’, a common pathway that has been identified among countries that were able to reduce their maternal mortality [5]. As the MMR falls, MDs from direct causes are of relative decreasing importance, while the opposite is true for maternal deaths due to pre‐existing medical diseases. Since most LMIC are achieving progress in reducing maternal mortality, focus needs to shift from the prevention of deaths from the traditional ‘big killers’ such as hypertensive disorders, postpartum haemorrhage and HIV/AIDS to pre‐existing medical diseases in these countries. Deaths from direct causes can be prevented by improving obstetric care. Different interventions will be needed to prevent deaths from cardiac disease. A multidisciplinary approach available for preconception counselling and during pregnancy, birth, and the postpartum period has been shown to improve maternal outcome, but remains unattainable in most LMIC [16, 19, 54, 72, 73].
In LMIC, women of reproductive age with cardiac disease are facing challenges far different from those that women in high‐income countries (HIC) face. Most management guidelines are based on research performed in HIC and not applicable or implementable in LMIC. Besides the differences in availability of resources, the most prevalent cardiac disorder among pregnant women in HIC is congenital heart disease, which needs a different approach than RHD, which is the most common cardiac condition among pregnant women in LMIC [8, 74]. A global study on RHD, a cardiac condition preventable with timely administration of antibiotics, found that RHD patients were predominately young women of reproductive age. These women have limited access to family planning as is shown by the alarmingly low coverage of contraceptive use of 3·6%. [64] Surgical intervention for RHD patients with placement of mechanical valves is increasingly available for young girls and women in LMIC and has increased survival in this group [63, 64, 75, 76]. At the same time, these women might consider becoming pregnant in the future. With the need for lifelong anticoagulation therapy, the risks of maternal morbidity and mortality and foetal complications are high, based on findings mainly from HIC [77, 78]. As previously mentioned, the limited available data from LMIC show a wide range of maternal mortality among cardiac patients. There is an adapted WHO risk classification available that classifies risk of maternal complications based on various cardiac conditions [79]. However, a global study showed that this risk classification does not perform as well in LMICs as compared with HICs [74]. Given all these limitations in LMIC, it is highly problematic to provide adequate risk assessment and treatment for a young woman with a cardiac condition, who is considering a pregnancy.
Despite the extensive search in several databases, we could only identify reports from 29 LMIC countries. It is possible that mortality reports from other countries have been missed. MDRs may not have been published in our searched databases or in any other online database. We attempted to overcome this by searching the publications of the MDSR Action Network website and references of the maternal mortality country profiles of the WHO, since both of these organisations are well‐informed regarding the presence of MDRs globally [9, 10]. An additional 23 reports were identified for possible inclusion using this strategy. Nevertheless, only for six countries multiple reports were available to assess the progress over time, for which one even used different methods for data collection. Even though Figure 2c indicates that for most of these countries, the impact of cardiac MD appears to increase over time, more data are needed to adequately assess this development.
Conclusion
To our knowledge, this is the first review assessing the frequency of maternal deaths due to cardiac disease in LMIC. Due to the limited availability of mortality reports from LMIC and the varying quality of the reports, it is hard to assess the real burden of maternal death due to cardiac disease. However, in the available reports a high incidence of cardiac‐related maternal deaths was identified, which may in reality be even higher due to the likely presence of underreporting. Our findings are in line with the obstetric transition model: indirect deaths including cardiac deaths are becoming relatively more important in several countries as obstetric care improves and obstetric deaths are reduced. Since most LMIC are achieving progress in reducing maternal mortality, more attention is needed for pre‐existing medical disease like cardiac disease as a cause of maternal mortality. Prospective studies on prevalence, pregnancy outcome and interventions are needed to assess the real burden or cardiac‐related maternal mortality in LMIC and establish feasible and relevant guidelines.
Supporting information
Appendix S1. Database search strategy.
Appendix S2. Quality assessment for reports mentioning zero cardiac deaths and when multiple reports per country were available.
Acknowledgement
We thank J.W. Schoones from the Leiden University Medical Center for help with the literature search.
Sustainable Development Goals (SDGs):SDG 3 (good health and well‐being), SDG 17 (partnerships for the goals)
References
- 1. Knight M, Nair M, Tuffnell D, Shakespeare J, Kenyon S, Kurinczuk JJ (Eds.) on behalf of MBRRACE‐UK. Saving Lives, Improving Mothers' Care – Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2013–15. National Perinatal Epidemiology Unit, University of Oxford: Oxford, 2017. [Google Scholar]
- 2. Vangen S, Bodker B, Ellingsen L et al Maternal deaths in the Nordic countries. Acta Obstet Gynecol Scand 2017: 96: 1112–1119. [DOI] [PubMed] [Google Scholar]
- 3. Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy‐related mortality in the United States, 2011–2013. Obstet Gynecol 2017: 130: 366–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nair M, Nelson‐Piercy C, Knight M. Indirect maternal deaths: UK and global perspectives. Obstet Med 2017: 10: 10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Souza JP, Tuncalp O, Vogel JP et al Obstetric transition: the pathway towards ending preventable maternal deaths. BJOG 2014: 121(Suppl 1): 1–4. [DOI] [PubMed] [Google Scholar]
- 6. Bhatla N, Lal S, Behera G et al Cardiac disease in pregnancy. Int J Gynaecol Obstet 2003: 82: 153–159. [DOI] [PubMed] [Google Scholar]
- 7. Zuhlke L, Mirabel M, Marijon E. Congenital heart disease and rheumatic heart disease in Africa: recent advances and current priorities. Heart 2013: 99: 1554–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Watkins DA, Sebitloane M, Engel ME, Mayosi BM. The burden of antenatal heart disease in South Africa: a systematic review. BMC Cardiovasc Disord 2012: 12: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Say L, Chou D, Gemmill A et al Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health 2014: 2: e323–e333. [DOI] [PubMed] [Google Scholar]
- 10. Maternal Death Surveillance and Response (MDSR) Action Network. (Available from: http://mdsr‐action.net/) [01 Nov 2017].
- 11. World Health Organization . Maternal mortality country profiles. (Available from: http://www.who.int/gho/maternal_health/countries/en/#E) [15 Jan 2018].
- 12. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009: 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hodorogea S. Confidential Enquiry into Maternal Deaths Moldava 2009–2013. N. Testemitanu State Medical and Pharmaceutical University, Chisinau, Republic of Moldova. Personal communication.
- 14. Hodorogea S, Friptu V. The Moldovan experience of maternal death reviews. BJOG 2014: 121(Suppl 4): 81–85. [DOI] [PubMed] [Google Scholar]
- 15. National Committee for Confidential Enquiry into Maternal Deaths . Saving Mothers 2008–2010: Fifth report on the Confidential Enquiries into Maternal Deaths in South Africa, comprehensive report. Department Health, Republic of South Africa: Pretoria, 2012. [Google Scholar]
- 16. National Committee for Confidential Enquiry into Maternal Deaths . Saving Mothers 2011–2013: Sixth report on the Confidential Enquiries into Maternal Deaths in South Africa, short report. Department Health, Republic of South Africa: Pretoria, 2015. [Google Scholar]
- 17. National Committee for Confidential Enquiry into Maternal Deaths . Saving Mothers 2014, Annual report and detailed analysis of maternal deaths due to non‐pregnancy related infections. Department Health, Republic of South Africa: Pretoria, 2015. [Google Scholar]
- 18. National Committee for Confidential Enquiry into Maternal Deaths . Saving Mothers 2005–2007: Fourth Report on Confidential Enquiries into Maternal Deaths in South Africa. Department Health, Republic of South Africa: Pretoria, 2011. [Google Scholar]
- 19. Paily VP, Ambujam K, Rajasekharan Nair V, Thomas B. Confidential Review of Maternal Deaths in Kerala: a country case study. BJOG 2014: 121(Suppl 4): 61–6. [DOI] [PubMed] [Google Scholar]
- 20. World Bank Data . Country classification by level of income; 2017. (Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519‐world‐bank‐country‐and‐lending‐groups) [15 June 2017].
- 21. World Health Organization . The WHO Application of ICD‐10 to deaths during pregnancy, childbirth and the puerperium: ICD‐MM. World Health Organization: Geneva, 2012. [Google Scholar]
- 22. National Committee for Confidential Enquiry into Maternal Deaths . A review of maternal deaths in South Africa during 1998. S Afr Med J 2000: 90: 367–373. [PubMed] [Google Scholar]
- 23. el Abdel‐Hady S, Mashaly AM, Sherief LS et al Why do mothers die in Dakahlia, Egypt? J Obstet Gynaecol Res 2007: 33: 283–287. [DOI] [PubMed] [Google Scholar]
- 24. Abouchadi S, Alaoui AB, Meski FZ, Bezad R, De Brouwere V. Preventable maternal mortality in Morocco: the role of hospitals. Trop Med Int Health 2013: 18: 444–450. [DOI] [PubMed] [Google Scholar]
- 25. Ahmed U, Eltigani L, Eltahir S, Mirghani S, Abd Alillah K, Abraha K. Maternal death review for maternal mortality reduction in Sudan 2010. Sudan Med J 2012: 48: 13–23. [Google Scholar]
- 26. Amarin Z, Khader Y, Okour A, Jaddou H, Al‐Qutob R. National maternal mortality ratio for Jordan, 2007–2008. Int J Gynaecol Obstet 2010: 111: 152–156. [DOI] [PubMed] [Google Scholar]
- 27. Sandoval De Baños PM. Case Study on Maternal Death Surveillance and Response, Country: El Salvador. Grupo de Trabajo Regional para la Reducción de la mortalidad materna: San Salvador, 2014. [Google Scholar]
- 28. Bekele A, Hassen A, Abebe S et al Second Ethiopian national Maternal Death Surveillance and Response (MDSR) report EFY 2008. Ethiopian Public Health Institute: Addis Abeba, 2017. [Google Scholar]
- 29. Statistics Botswana and Ministry of Health & Wellness . Botswana – Maternal Mortality Ratio (MMR) 2011–2015. Statistics Botswana: Gaberone, 2017. [Google Scholar]
- 30. Byhell M, Nand D, Fong J, Vuadreu R. Maternal Mortality in Fiji 2008–2012. Fiji J Public Health 2014: 3: 32–37. [Google Scholar]
- 31. Campbell O, Gipson R, Issa AH et al National maternal mortality ratio in Egypt halved between 1992–93 and 2000. Bull World Health Organ 2005: 83: 462–471. [PMC free article] [PubMed] [Google Scholar]
- 32. National Committee for Confidential Enquiry into Maternal Deaths . Saving Mothers 2002–2004: Third Report on Confidential Enquiries into Maternal Deaths in South Africa. Department Health, Republic of South Africa: Pretoria, 2006. [Google Scholar]
- 33. Du L, Qin M, Zhang L, Xu H. Zhu L. Trends in maternal mortality in resident vs. migrant women in Shanghai, China, 2000–2009: a register‐based analysis. Reprod Health Matters 2012: 20: 73–80. [DOI] [PubMed] [Google Scholar]
- 34. Gurina NA, Vangen S, Forsen L, Sundby J. Maternal mortality in St. Petersburg, Russian Federation. Bull World Health Organ 2006: 84: 283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. National Committee for Confidential Enquiry into Maternal Deaths . Second Interim Report on Confidential Enquiries into Maternal Deaths in South Africa, Maternal Deaths for 1999. Department Health, Republic of South Africa: Pretoria, 2000. [Google Scholar]
- 36. Issah K, Nang‐Beifubah A, Opoku CF. Maternal and neonatal survival and mortality in the Upper West Region of Ghana. Int J Gynaecol Obstet 2011: 113: 208–210. [DOI] [PubMed] [Google Scholar]
- 37. Jayaratne K. Maternal Death Surveillance and Response (MDSR) – Outcomes of 2014. Family Health Bureau, Ministry of Health Sri Lanka: Colombo, 2015. [Google Scholar]
- 38. Maternal & Child Morbidity Surveillance Unit . Maternal Death Surveillance and Response System: Dissmenation of 2015 Data. Family Health Bureau, Ministry of Health Sri Lanka: Colombo, 2016. [Google Scholar]
- 39. Karimi‐Zarchi M, Ghane‐Ezabadi M, Vafaienasab M et al Maternal mortality in Yazd Province, Iran. Electron Physician 2016: 8: 1949–1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kestler E, Ramirez L. Pregnancy‐related mortality in Guatemala, 1993–1996. Rev Panam Salud Publica 2000: 7: 41–45. [DOI] [PubMed] [Google Scholar]
- 41. Kodan LR, Verschueren KJC, van Roosmalen J, Kanhai HHH, Bloemenkamp KWM. Maternal mortality audit in Suriname between 2010 and 2014, a reproductive age mortality survey. BMC Pregnancy Childbirth 2017: 17: 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kongnyuy EJ, Mlava G, van den Broek N. Facility‐based maternal death review in three districts in the central region of Malawi: an analysis of causes and characteristics of maternal deaths. Womens Health Issues 2009: 19: 14–20. [DOI] [PubMed] [Google Scholar]
- 43. Krishnan M, on behalf of National Technical Committee for the CEMD . Report on the confidential enquiries into maternal deaths in Malaysia 2006–2008. Family Health Development Division, Ministry of Health, Malaysia: Kuala Lumpur, 2012. [Google Scholar]
- 44. Madzimbamuto FD, Ray SC, Mogobe KD et al A root‐cause analysis of maternal deaths in Botswana: towards developing a culture of patient safety and quality improvement. BMC Pregnancy Childbirth 2014: 14: 231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mataya R, on behalf of Malawi National Confidential Committee on Enquiry into Maternal Death . Report on the Confidential Enquiry into Maternal Deaths in Malawi (2008–2012). Ministry of Health, Republic of Malawi: Lilongwe,2014. [Google Scholar]
- 46. McCaw‐Binns A, Lindo JL, Lewis‐Bell KN, Ashley DE. Maternal mortality surveillance in Jamaica. Int J Gynaecol Obstet 2008: 100: 31–36. [DOI] [PubMed] [Google Scholar]
- 47. McCaw‐Binns A, Standard‐Goldson A, Ashley D, Walker G, MacGillivray I. Access to care and maternal mortality in Jamaican hospitals: 1993–1995. Int J Epidemiol 2001: 30: 796–801. [DOI] [PubMed] [Google Scholar]
- 48. Munjanja SP, Nystrom L, Nyandoro M, Magwali T. Zimbabwe Maternal and Perinatal Mortality Study 2007. Ministry of Health and Child Welfare: Harare, 2009. [Google Scholar]
- 49. Namiq E, Jabar M, Hasson Alsenaid E, Ali Galib B. Maternal Death Surveillance and Response (MDSR) Iraq 2010–2012. Ministry of Health: Bagdad. [Google Scholar]
- 50. Nisar N, Sohoo NA. Maternal mortality in rural community: a challenge for achieving millennium development goal. J Pak Med Assoc 2010: 60: 20–24. [PubMed] [Google Scholar]
- 51. Olsen BE, Hinderaker SG, Bergsjo P et al Causes and characteristics of maternal deaths in rural northern Tanzania. Acta Obstet Gynecol Scand 2002: 81: 1101–1109. [PubMed] [Google Scholar]
- 52. Qiu L, Lin J, Ma Y et al Improving the maternal mortality ratio in Zhejiang Province, China, 1988–2008. Midwifery 2010: 26: 544–548. [DOI] [PubMed] [Google Scholar]
- 53. Rahman MH, Akhter HH, Khan Chowdhury ME, Yusuf HR, Rochat RW. Obstetric deaths in Bangladesh, 1996–1997. Int J Gynaecol Obstet 2002: 77: 161–169. [DOI] [PubMed] [Google Scholar]
- 54. National Technical Committee of the Confidential Enquiries into Maternal Deaths . Report on the confidential enquiries into maternal deaths in Malaysia 2009 – 2011. Family Health Development Division, Ministry of Health Malaysia: Kuala Lumpur, 2012. [Google Scholar]
- 55. Sahel A, De Brouwere V, Essobli A, Elmanjra C, Zakour N. Enquête confidentielle sur les décès maternels de 2015 dans les six régions prioritaires au Maroc. Ministrère de la Santé: Marrakech, 2017. [Google Scholar]
- 56. Sayinzoga F, Bijlmakers L, van Dillen J, Mivumbi V, Ngabo F, van der Velden K. Maternal death audit in Rwanda 2009–2013: a nationwide facility‐based retrospective cohort study. BMJ Open 2016: 6: e009734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Suvedi Krishna B, Pradhan A, Barnett S, Puri M, Rai Chitrakar S et al Nepal Maternal Mortality and Morbidity Study 2008/2009: Summary of Preliminary Findings. Family Health Division, Department of Health Services: Kathmandu, 2009. [Google Scholar]
- 58. Ndavi PM, Dlamini D, Khumalo P. Report on maternal mortality review in the Kingdom of Swaziland 2001. Ministry of Health and Social Welfare: Mbabane, 2001. [Google Scholar]
- 59. Yang S, Zhang B, Zhao J et al Progress on the maternal mortality ratio reduction in Wuhan, China in 2001–2012. PloS One 2014: 9: e89510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. You F, Huo K, Wang R et al Maternal mortality in Henan Province, China: changes between 1996 and 2009. PloS One 2012: 7: e47153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zakariah AY, Alexander S, van Roosmalen J, Buekens P, Kwawukume EY, Frimpong P. Reproductive age mortality survey (RAMOS) in Accra, Ghana. Reproductive Health 2009: 6: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Otto H, Saether SG, Banteyrga L, Haugen BO, Skjaerpe T. High prevalence of subclinical rheumatic heart disease in pregnant women in a developing country: an echocardiographic study. Echocardiography 2011: 28: 1049–1053. [DOI] [PubMed] [Google Scholar]
- 63. ElSayed A, Elnur EE. The rebirth of cardiac surgery in Sudan. Cardiovasc Diagn Ther 2016: 6: S20–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zuhlke L, Engel ME, Karthikeyan G et al Characteristics, complications, and gaps in evidence‐based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J 2015: 36: 1115–1122a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Diao M, Kane A, Ndiaye MB et al Pregnancy in women with heart disease in sub‐Saharan Africa. Arch Cardiovasc Dis 2011: 104: 370–374. [DOI] [PubMed] [Google Scholar]
- 66. Sliwa K, Libhaber E, Elliott C et al Spectrum of cardiac disease in maternity in a low‐resource cohort in South Africa. Heart 2014: 100: 1967–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rezk M, Elkilani O, Shaheen A, Gamal A, Badr H. Maternal hemodynamic changes and predictors of poor obstetric outcome in women with rheumatic heart disease: a five‐year observational study. J Matern Fetal Neonatal Med 2017: 31: 1542–1547. [DOI] [PubMed] [Google Scholar]
- 68. Campanharo FF, Cecatti JG, Haddad SM et al The impact of cardiac diseases during pregnancy on severe maternal morbidity and mortality in Brazil. PloS One 2015: 10: e0144385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Avila WS, Rossi EG, Ramires JA et al Pregnancy in patients with heart disease: experience with 1,000 cases. Clin Cardiol 2003: 26: 135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Castillo P, Hurtado JC, Martinez MJ et al Validity of a minimally invasive autopsy for cause of death determination in maternal deaths in Mozambique: An observational study. PLoS Med 2017: 14: e1002431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Faduyile FA, Soyemi SS, Emiogun FE, Obafunwa JO. A 10 years autopsy‐based study of maternal mortality in Lagos State University Teaching Hospital, Lagos, Nigeria. Niger J Clin Pract 2017: 20: 131. [DOI] [PubMed] [Google Scholar]
- 72. Knight M, Nair M, Tuffnell D et al Saving Lives, Improving Mothers’ Care Surveillance of maternal deaths in the UK 2012–14 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009–14. National Perinatal Epidemiology Unit, University of Oxford: Oxford, 2015. [Google Scholar]
- 73. European Society of Gynecology, Association for European Paediatric Cardiology, German Society for Gender Medicine et al ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011: 32: 3147–3197. [DOI] [PubMed] [Google Scholar]
- 74. van Hagen IM, Boersma E, Johnson MR et al Global cardiac risk assessment in the Registry Of Pregnancy And Cardiac disease: results of a registry from the European Society of Cardiology. Eur J Heart Fail 2016: 18: 523–533. [DOI] [PubMed] [Google Scholar]
- 75. Guteta S, Yadeta D, Azazh A, Mekonnen D. Cardiac surgery for valvular heart disease at a referral hospital in Ethiopia: a review of cases operated in the last 30 years. Ethiop Med J 2016: 54: 49–55. [PubMed] [Google Scholar]
- 76. Barbosa PJ, Lopes AA, Feitosa GS et al Prognostic factors of rheumatic mitral stenosis during pregnancy and puerperium. Arq Bras Cardiol 2000: 75: 215–224. [DOI] [PubMed] [Google Scholar]
- 77. Elkayam U, Singh H, Irani A, Akhter MW. Anticoagulation in pregnant women with prosthetic heart valves. J Cardiovasc Pharmacol Ther 2004: 9: 107–115. [DOI] [PubMed] [Google Scholar]
- 78. van Hagen IM, Roos‐Hesselink JW, Ruys TP et al Pregnancy in women with a mechanical heart valve: data of the European society of cardiology registry of pregnancy and cardiac disease (ROPAC). Circulation 2015: 132: 132–142. [DOI] [PubMed] [Google Scholar]
- 79. Thorne S, MacGregor A, Nelson‐Piercy C. Risks of contraception and pregnancy in heart disease. Heart 2006: 92: 1520–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Database search strategy.
Appendix S2. Quality assessment for reports mentioning zero cardiac deaths and when multiple reports per country were available.


