Abstract
Introduction
Currently fetal nuchal translucency (NT) ≥3.5 mm is an indication for invasive testing often followed by chromosomal microarray. The aim of this study was to assess the risks for chromosomal aberrations in fetuses with an NT 3.0‐3.4 mm, to determine whether invasive prenatal testing would be relevant in these cases and to assess the residual risks in fetuses with normal non‐invasive prenatal test (NIPT) results.
Material and methods
A retrospective study and meta‐analysis of literature cases with NT between 3.0 and 3.4 mm and 2 cohorts of pregnant women referred for invasive testing and chromosomal microarray was performed: Rotterdam region (with a risk >1:200 and NT between 3.0 and 3.4 mm) tested in the period July 2012 to June 2019 and Central Denmark region (with a risk >1:300 and NT between 3.0 and 3.4 mm) tested between September 2015 and December 2018.
Results
A total of 522 fetuses were referred for invasive testing and chromosomal microarray. Meta‐analysis indicated that in 1:7.4 (13.5% [95% CI 8.2%‐21.5%]) fetuses a chromosomal aberration was diagnosed. Of these aberrant cases, 47/68 (69%) involved trisomy 21, 18, and 13 and would potentially be detected by all NIPT approaches. The residual risk for missing a (sub)microscopic chromosome aberration depends on the NIPT approach and is highest if NIPT was performed only for common trisomies–1:21 (4.8% [95% CI 3.2%‐7.3%]). However, it may be substantially lowered if a genome‐wide 10‐Mb resolution NIPT test was offered (~1:464).
Conclusions
Based on these data, we suggest that the NT cut‐off for invasive testing could be 3.0 mm (instead of 3.5 mm) because of the high risk of 1:7.4 for a chromosomal aberration. If women were offered NIPT first, there would be a significant diagnostic delay because all abnormal NIPT results need to be confirmed by diagnostic testing. If the woman had already received a normal NIPT result, the residual risk of 1:21 to 1:464 for chromosome aberrations other than common trisomies, dependent on the NIPT approach, should be raised. If a pregnant woman declines invasive testing, but still wants a test with a broader coverage of clinically significant conditions then the genome‐wide >10‐Mb resolution NIPT test, which detects most aberrations, could be proposed.
Keywords: microarray, microdeletion, non‐invasive prenatal test, nuchal translucency, prenatal diagnosis, submicroscopic chromosomal abnormalities
Abbreviations
- CI
confidence interval
- CMA
chromosomal microarray
- CNV
copy number variant
- CT
first‐trimester combined test
- MoM
multiples of the median
- NIPT
non‐invasive prenatal test
- NT
nuchal translucency
- SNP
single nucleotide polymorphism
Key message.
The risk for chromosomal aberrations in fetuses with nuchal translucency 3.0‐3.4 mm is 1:7.4, the risk after normal NIPT for common trisomies is 1:21, therefore offering an invasive test with chromosomal microarray could be considered. The 10‐Mb genome‐wide NIPT test offers the second highest detection rate.
1. INTRODUCTION
Nuchal translucency (NT) ≥3.5 mm (>p99) is a well‐recognized indication for invasive testing as it is a well‐studied ultrasound marker for common and uncommon aneuploidies as well as for a wide variety of genetic syndromes and structural anomalies. 1 , 2 , 3 , 4 , 5 , 6 Although Kagan et al have previously shown that fetuses with NT of 95th centile ≥3.4 mm have a high risk for chromosomal aberrations (1:14), 7 only a few groups performed chromosomal microarray (CMA) analysis in fetuses with NT ≥3.0 mm. 8 , 9 , 10 , 11 An enlarged (apparently isolated) NT of 3.0‐3.4 mm is diagnosed in about 0.8% of pregnant women undergoing first‐trimester combined test (CT) and in the absence of the risk assessment routinely performed after CT, it might be difficult to counsel women and advise an appropriate follow‐up test (data from 71 016 women in Central Region Denmark who had CT in 91 430 pregnancies with estimated date of delivery 2013‐2018. Annual report, Danish Fetal Medicine Database 2018; RKKP, Petersen, OB [in press]). Neither in the Netherlands nor in Denmark an apparently isolated NT of 3.0‐3.4 mm alone is an indication for invasive testing, although NT measurements are known to be a good marker for common aneuploidies. 1 , 2 , 3 Cell‐free DNA testing (so‐called non‐invasive prenatal test [NIPT]) is currently available in many countries. It can be offered as part of a contingent screening program: after a CT resulting in an increased risk for trisomy 13, 18, or 21 12 , 13 , 14 or as a first‐tier screening test to all pregnant women. 15 Currently, in some countries a substantial number of pregnant women have already had a (targeted) NIPT before a 13‐week ultrasound scan, whereas others may have a choice between NIPT and invasive testing after CT or 13‐week ultrasound scan without the risk calculation. Whereas the presence of a structural anomaly or an NT ≥3.5 mm is an internationally recognized indication for invasive testing, the decisions in pregnancies with NT slightly lower than 3.5 mm can be difficult.
The aim of this study was to assess the risks for chromosomal aberrations in fetuses with an NT 3.0‐3.4 mm, to determine whether it would be reasonable to offer invasive prenatal testing, and to assess the residual risks for (sub)microscopic chromosomal aberrations other than trisomy 13, 18, and 21 in fetuses with an NT 3.0‐3.4 mm.
2. MATERIAL AND METHODS
2.1. Literature data
To assemble a cohort that was as large as possible, a semi‐systematic literature search was performed (see Supplementary material, Appendix S1). Papers were screened for cohorts of fetuses with NT 3.0‐3.4 mm tested with CMA. Only papers presenting the total number of fetuses with NT 3.0‐3.4 mm and at least the number of abnormal cases among these fetuses were selected. Unfortunately, not all publications specified the chromosomal aberrations, and many were excluded because the total number of fetuses with NT of interest was not specified. Eventually, only 3 publications were selected, 9 , 10 , 11 which provided data on 311 fetuses (Tables 1 and 2).
TABLE 1.
Cytogenomic results in fetuses with NT 3.0‐3.4 mm and the detection possibilities by different NIPT approaches
| Study—invasively tested with microarray | Cohort selection | n | % of aberrant cases | Risk | Detectable/undetectable by targeted NIPT (+13, +18, +21) | Detectable/undetectable by targeted NIPT (+13, +18, +21, incl. X/Y) | Detectable/undetectable by genome‐wide NIPT (>20 Mb, excl. X/Y) | Detectable/undetectable by genome‐wide NIPT (>10 Mb, incl. X/Y) | Not detectable by genome‐wide NIPT (<10 Mb) |
|---|---|---|---|---|---|---|---|---|---|
| Grossman et al 2019 | NT 3.0‐3.4 mm a | 4/31 | 12.9% | 1:8 | 4 b /0 | 4/0 | 4/0 | 4/0 | 0 |
| Maya et al 2017 | NT 3.0‐3.4 mm and risk <1:380 | 11/170 | 6.5% | 1:15 | 6/5 | 7/4 | 7/4 | 8/3 | 3 (all sCNV) |
| Zhao et al 2019 | NT 3.0‐3.4 mm | 18/110 c | 16.4% | 1:6 | 11/7 | 11/7 | 14/4 | 15/3 | 3 (all sCNV) |
| Current data Aarhus (DK) | NT 3.0‐3.4 mm and risk >1/300 | 14/128 | 10.9% | 1:9 | 9/5 | 10/4 | 10/4 | 13/1 | 1 |
| Current data Rotterdam (NL) | NT 3.0‐3.4 mm and risk >1/200 | 21/83 | 25.3% | 1:4 | 17/4 | 17/4 | 18/3 | 18/3 | 3 (all sCNV) |
| Pooled estimates d [95% CI]/raw totals | 13.5% d [8.2, 21.5] | 1:7.4 d | 47/21 | 49/19 | 53/15 | 58/10 | 10 | ||
| Residual risk for other chromosomal aberrations incl. sCNV, f Pooled estimate d [95% CI] |
4.8% [3.2, 7.3] 1:21 |
4.5% [2.9, 7.0] 1:22 |
3.4% [2.1, 5.5] 1:29 |
2.6% [1.4, 4.7] 1:38 |
|||||
| Residual risk for other chromosomal aberrations excl. sCNV, f Pooled estimate d [95% CI] |
3.0% [1.7, 5.2] 1:33 |
2.8% [1.5, 5.0] 1:36 |
1.9% [0.9, 4.0] 1:53 |
0.2% e 1:464 |
Abbreviations: CNV, copy number variant; n, number of abnormal cases/total number tested; NIPT, non‐invasive prenatal test; NT, nuchal translucency; sCNV, susceptibility CNV.
Pooled estimates resulting from a random‐effects model are given in bold.
Structural abnormalities at the time of NT measurement were not excluded.
The authors did not specify aberrations and assumed that sex‐chromosome aneuploidy and triploidy would be detected by NIPT.
Only 60 tested with microarray.
Resulting from a random‐effects model in comprehensive meta‐analysis software version 2 (Biostat Inc.).
The majority of zero‐event rates in this specific calculation prevents the use of comprehensive meta‐analysis. Therefore, the raw pooled estimate is reported without 95% CI.
Total number of fetuses is corrected, trisomic/aberrant cases detectable by NIPT were excluded and the residual risk for other chromosomal aberrations is calculated in patients with normal NIPT results and not for the whole population to enable post‐test counseling on residual risks in patients with normal NIPT results.
TABLE 2.
Chromosomal aberrations found in the currently presented cohorts and in the literature
| Cohort source | n | T21 | T18 | T13 | X/Y abnormalities | Other microscopically detectable | Submicroscopic |
|---|---|---|---|---|---|---|---|
| Grossman et al 2019 | 4/31 | 4 (not specified) | 0 | ||||
| Maya et al 2017 | 11/170 | 6 | 1 – trisomy X a |
1
|
3 (all susceptibility CNV)
|
||
| Zhao et al 2019 | 18/110 | 5 | 3 | 3 | 4 (not specified) |
3 (all susceptibility CNV)
|
|
| Current data Aarhus (DK) | 14/128 | 8 | 1 | 0 |
2
|
2
|
1 syndromic
|
| Current data Rotterdam (NL) | 21/83 | 13 | 2 | 2 | 0 |
1
|
3 (all susceptibility CNV)
|
| Total | 68 | 47 | 11 | 10 | |||
Abbreviation: n, number of abnormal cases/total number tested.
Trisomy X case is not excluded, because the paper does not describe possible mosaicism in other tissues and so clinical relevancy of this finding cannot be excluded. Excluding this case would not notably change the statistical calculations.
2.2. Aarhus cohort
In all, 128 women carrying a fetus with an NT 3.0‐3.4 mm at the CT were prospectively referred for Agilent genotyping array as described before. 16 As the formal indication for invasive testing is a risk for trisomy 21 >1:300 after CT (or >1:150 for trisomy 13 and trisomy 18, or single criteria: maternal age >45 years, β human chorionic gonadotropin or pregnancy‐associated plasma protein A <0.2 multiples of the median [MoM] or β human chorionic gonadotropin > 5 MoM or NT ≥3.5 mm), not all fetuses with an NT 3.0‐3.4 mm had formal indication for invasive testing. Samples were collected between 1 September 2015 until 31 December 2018 in either of four clinics performing invasive testing in the Central Denmark Region of 1.2 million inhabitants. Samples routinely referred for CMA testing with risk <1:300 and NT between 3 and 3.4 mm were included in this cohort. All cytogenetic tests were performed in one central laboratory. To create a homogeneous cohort, we excluded cases with hydrops fetalis, hygroma colli and other co‐existing congenital anomalies evident on the dating‐ or/and the NT scan. Samples were tested with SurePrint G3 Human CGH microarray 180K (Agilent Technologies) with analysis resolution of c.50 kb as described before. 16 The data are presented in Tables 1 and 2.
2.3. Rotterdam cohort
Eighty‐three women carrying a fetus with an NT 3.0‐3.4 mm at the CT were prospectively referred for Illumina single nucleotide polymorphism (SNP) genotyping array as described before. 17 As the formal indication for invasive testing is a risk ≥1:200 based on CT, only fetuses with higher post‐test risk were offered invasive testing. Samples collected in our central location (Erasmus MC) and three collaborating hospitals between 1 July 2012 until 30 June 2019 and routinely referred for SNP array testing (0.5 Mb resolution) were included in this cohort. Only women from the Rotterdam region were routinely offered CMA if undergoing an invasive procedure for an increased CT risk and NT <3.5 mm in the Netherlands. All cytogenetic tests were performed in one central laboratory. This cohort overlaps slightly with the cohort published before. 17 To create a homogeneous cohort, we excluded cases with hydrops fetalis, hygroma colli, and other co‐existing congenital anomalies evident on the dating or the NT scan. All samples were tested with quantitative fluorescence PCR or multiplex ligation‐dependent probe amplification to detect common aneuploidies (rapid aneuploidy detection). When rapid test detected trisomy 21 or 13, such samples were karyotyped to assess the recurrence risk. Cases of triploidy or trisomy 18 were not further tested with CMA or karyotyped. All cases showing normal rapid aneuploidy detection results or sex‐chromosomal aneuploidy were tested with Illumina SNP array (Illumina) (HumanCytoSNP‐12, Infinium_CytoSNP_850K or GSA+MD‐24 v1.0 BeadChip, with analysis resolution of c.0.5 Mb) as described previously. 18 The data are presented in Tables 1 and 2.
Furthermore, we evaluated which aberrations would theoretically be missed by current NIPT approaches because of the aberration size or not being in the scope of a targeted test (NIPT tests were not performed in this cohort). Detection rates in all groups independent of aberration were assumed to be 100% for simplicity. Cytogenomic results in all cohorts were grouped into several categories depending on NIPT strategies that would potentially detect them:
Aberrations detectable by targeted NIPT: trisomy 13, 18, and 21
Aberrations detectable by targeted NIPT: trisomy 13, 18, 21, and X/Y aneuploidy
Aberrations detectable by genome‐wide NIPT (autosomal >20 Mb)—current Dutch NIPT policy: trisomy 13, trisomy 18, trisomy 21, and additional findings: large chromosomal aberrations (aberrations >20 Mb)
Aberrations detectable by genome‐wide NIPT (>10 Mb), including X/Y
Submicroscopic aberrations (<10 Mb) not detectable by routine genome‐wide NIPT strategies mentioned above.
For the purpose of this paper, we assumed that all aneuploidies would be detectable by NIPT as well as structural unbalanced aberrations larger than the resolution of the particular NIPT approach. Unfortunately, it is difficult to assess how many of these cases would be missed because of mosaicism and their absence in the cytotrophoblast. We did not correct the residual risks for common trisomies as presented before. 19 The residual risk assessment for common trisomies and the positive and negative predicted values in high‐risk pregnancies that has been reviewed by several authors 20 , 21 , 22 and therefore this issue was not within the scope of this study.
The focus of this study is the residual risk for chromosomal aberrations other than trisomy 13, 18, and 21 in fetuses with NT 3.0‐3.4 mm.
Pooled prevalence (event rates) including 95% CIs were calculated using a random‐effects model 23 in comprehensive meta‐analysis software version 2 (Biostat Inc.) that employs standard continuity corrections for zero‐events cells.
2.4. Susceptibility copy number variants for neurodevelopmental disorders
A particular group of submicroscopic aberrations are susceptibility copy number variants (CNVs) for (mainly) neurodevelopmental disorders. These are variants of extreme phenotypic heterogeneity and of variable expressivity (in contrast to syndromic disorders where [a set of] specific features are associated with a particular disease/syndrome). The expressed phenotypes of these disorders probably (partly) depend on the presence of a second‐site variant or individual genetic background. If a susceptibility CNV is found prenatally, the risk for developing the disease is still unquantified, as data on individuals with neurodevelopmental phenotypes are mostly postnatally ascertained. 24 , 25 , 26
To our knowledge, there is no study that showed any biological mechanisms for the relation between susceptibility CNVs and an enlarged NT. It is not yet known whether an enlarged NT should be recognized as a second hit in the presence of such a susceptibility CNV. 27 At this moment finding additional predisposition factors may play a role in decision‐making in pregnancy; however, it is less likely that one would choose invasive testing with a primary aim to investigate susceptibility CNVs. Because reporting susceptibility CNVs can be problematic in some clinical settings, we provided risk figures for both scenarios, depending on the decisions on reporting susceptibility CNVs. Discussing the issues of reporting susceptibility CNVs is not in the scope of the current paper.
2.5. Ethical approval
According to the Research Codes of Erasmus MC, data that cannot be traced to an individual may be used for research. Patients are informed that we may investigate/publish their medical data as long as all data remain anonymous and cannot lead to the identification of the individual. All presented data were obtained during routine diagnostic procedures. All presented data are anonymous and do not allow identification of the individual patients.
3. RESULTS
A total of 522 fetuses with NT 3.0‐3.4 mm were subjected to CMA testing as the result of an increased risk after CT/enlarged NT (Tables 1 and 2). The estimated proportions (event rates) and 95% CI of abnormal cases in the selected papers and cohorts, including the pooled estimate based on the random‐effects model, are shown in Figure 1. Meta‐analysis of the whole cohort demonstrated a risk of 1:7.4 (13.5%, 95% CI, 8.2%‐21.5%) for an abnormal result in this cohort (Table 1). Over all studies, 47 in a total of 68 aberrations (69.1%) were either trisomy 13, 18, and 21. Eleven (11/68, 16.2%) aberrations were either sex‐chromosome aberrations (both aneuploidy and structural aberrations) or chromosomal imbalances >10 Mb. In total, 58/522 (11%) cases would also be detected by karyotyping. Submicroscopic aberrations were found in 10 cases (10/68 14.7%). Most of them (9/10) were susceptibility CNVs. In 1 case (0.2%) out of 464 chromosomally normal fetuses a syndromic disorder caused by a submicroscopic aberration was found. Therefore, the prevalence of submicroscopic aberrations in karyotypically normal fetuses (464 = 522‐58) was calculated to be 2.2% (10/464): 1.9% (9/464) for susceptibility CNVs and 0.2% (1/464) for syndromic CNVs.
FIGURE 1.
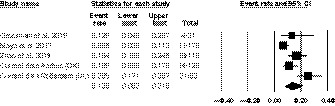
Forest plot showing event rate of aberrant cases based on cytogenomic results in fetuses with nuchal translucency 3.0‐3.4 mm in selected sources representing the risk for overall risk for chromosomal aberrations in the combined cohort (13.5%, 95% CI 8.2%‐21.5% equivalent to a risk of 1:7.4). Only the first author is given for each study. Boxes represent event rate per source and their size is proportional to their weight in the analysis, and lines represent 95% CI. Diamond represents pooled estimate and its width represents the 95% CI
The risk of missing an aberration depends on the NIPT approach used, and we have generated four hypothetical NIPT scenarios from a targeted trisomy 13, 18, and 21 alone to a genome‐wide with a resolution of 10 Mb, assuming that these NIPTs had no false‐negative results for common trisomies or segmental aberrations that were in the scope of the particular test. Not surprisingly the broader the NIPT test the fewer aberrations would be potentially missed (Table 1).
The residual risk for a chromosomal aberration other than common trisomies in a fetus with NT 3.0‐3.4 mm and with normal results for chromosomes 13, 18, and 21 was calculated to be 1:21 (all aberrations included, 4.8% [95% CI 3.2%‐7.3%]) or 1:33 (excluding susceptibility CNVs, 3.0% [95% CI 1.7%‐5.2%]).
These residual risks can theoretically be substantially lowered by genome‐wide analysis and higher resolution NIPT. When the genome‐wide NIPT with the currently available 10‐Mb genome‐wide resolution would be used, the residual risk for other syndromic chromosome aberrations might be equivalent to a population risk for a submicroscopic CNV, which was previously estimated to be 1:270 for early‐onset syndromic disorders. 28
4. DISCUSSION
Based on two patient cohorts and a literature review, we aimed to assess the risks for chromosomal aberrations in fetuses with an NT 3.0‐3.4 mm, to determine whether offering invasive prenatal testing would be reasonable. Our results showed that 13.5% (95% CI 8.2%‐21.5%) of the fetuses tested with microarray demonstrated a chromosomal aberration, suggesting a risk of 1:7.4. Because only data from invasively tested fetuses were available (please see section Study limitation), and the full characteristics of the presented cohorts were not available, we compared our pooled estimations to the previously published studies to judge to what extent our data are representative. To be able to compare the current data with the literature cohort tested with karyotyping, we took only microscopically visible aberrations into account. Strong association between chromosomal aberrations and fetal NT >3 mm was already suggested by Pandya et al. 29 When karyotypically visible aberrations are taken into account, our pooled cohort showed 11% of abnormal cases, whereas the clinical data of Kagan et al 7 showed chromosomal aberrations in 7.1% of fetuses (p95 ‐> 3.4 mm, 507/7109), Äyräs et al 30 in 9.6% (p95 ‐> 3.4 mm, 65/679), Nicolaides et al 31 in 13% (NT = 3 mm 7/52) and Bardi et al 32 in 14% (p95‐p99, 124/894). Although the incidence of chromosome aberrations presented in this paper is within the previously published range (7%‐14%), one has to be aware that the incidence based on fetal invasive testing, such as in our study, might represent the upper bound risk estimate, but on the other hand, in population‐based studies the bias could be caused by missing pediatric cases with less pronounced symptoms caused by a chromosomal aberration that is not always evident at birth or even within the first 3 years.
Our study showed that the incidence of chromosomal aberrations in fetuses with NT 3.0‐3.4 mm is higher than 1:10. According to the current updated ISUOG consensus statement on cell‐free DNA aneuploidy testing, in women at very high risk after combined screening (>1:10, with no ultrasound anomaly) cell‐free DNA testing should not replace invasive testing. 33
The secondary aim was to assess the residual risks for (sub)microscopic chromosomal aberrations other than trisomy 13, 18, and 21. There are only a few studies on microarray results in fetuses with NT >3 mm that show the relation between the specific NT thickness 3.0‐3.4 mm and the incidence of chromosomal aberrations. In the presented pooled cohort, offering NIPT for trisomy 13, 18, and 21 only will notably lower the residual risk to 1:21; however, it still remains higher than the cut‐off for offering invasive testing in the authors’ countries (1:200 to 1:300). In our pooled cohort, the prevalence of submicroscopic aberrations in karyotypically normal fetuses was 2.2% (10/464), which seems to be higher than in fetuses tested because of advanced maternal age or maternal anxiety (0.84%, 95% CI 0.55%‐1.30%) 28 suggesting that microarray testing may have an additional value in prenatal cytogenetic diagnosis not only in fetuses with NT >3.5 mm, but in fetuses with NT >3 mm as well.
Counseling for invasive testing for fetal chromosome aberrations has changed, and varies significantly between counties, 34 In some countries NIPT became a first‐tier population screening test, whereas in other countries it is a second‐tier test. In our opinion, pretest counseling of couples opting for or eligible for invasive prenatal testing needs to address both the risk of missing aberrations that are in the scope of NIPT and the residual risk for other chromosomal aberrations beyond the technical possibilities of NIPT (the scope of this paper). Such a residual risk is not only dependent on the NIPT approach providing either screening for common aneuploidies or broad screening for unbalanced chromosomal aberrations, but depends on the results of the ultrasound anomaly scan and the a priori risk determined by CT as well. The risk for common aneuploidies in a high‐risk population can be reduced by an additional screening test such as NIPT, but it might still remain high enough to offer diagnostic invasive testing.
The current study focused on the intermediate NT measurement results (3.0‐3.4 mm) that can cause a clinical challenge both in the presence or absence of a normal NIPT result. Based on the presented data, we discuss a prenatal strategy in different clinical scenarios depending on whether a pregnant woman already had a (normal) low‐risk NIPT result or faces the choice between invasive testing and NIPT. In the majority of the pregnant population, the risk of submicroscopic chromosomal aberrations is higher than the risk of Down syndrome/common trisomies. 28 , 35 In light of our results, and the increasing evidence of a very low risk of procedure‐related miscarriage after invasive procedures, 36 we believe it is time to expand the information to include the residual risk for all chromosomal aberrations, when pregnant women are offered the choice between invasive testing or NIPT in the case of NT 3.0‐3.4 mm.
4.1. Fetus with NT 3.0‐3.4 mm and no NIPT performed
Based on the current data and literature review, we suggest that not only an NT ≥3.5 mm, but also an NT ≥3.0 mm could be considered as an indication for invasive prenatal testing because the frequency of chromosome aberrations seems to be very high (in the presented cohort 1:7.4 and according to the literature at least 1:14 7 ). Our results support the previous studies of both Khalil et al and Maya et al, who suggested that invasive testing should be offered in case of a fetal NT ≥3.0 mm. 9 , 37 If NIPT is offered as the first test, then these women may experience a longer period of anxiety (while waiting for a definitive result) because every abnormal NIPT result requires subsequent confirmatory diagnostic testing. Moreover, such a delay may result in the need for late termination in affected cases. Therefore, we suggest offering invasive testing to this group to make early diagnosis of clinically important chromosomal aberrations a reproductive choice. Our conclusion is supported by previously published data, which showed that offering NIPT instead of CMA in high‐risk pregnancies (after CT) significantly decreases the diagnostic yield. 14 Pre‐test counseling is an essential part of the screening procedure because some of the women may prefer NIPT over an invasive procedure even when having a high‐risk pregnancy. Providing up‐to‐date, balanced, and accurate information early in gestation is crucial to facilitate patient‐informed decision‐making. 38 In our opinion, the present study supports offering invasive testing as an appropriate choice with a high detection rate. As always, NIPT could be an alternative to invasive testing, in which case we suggest genome‐wide NIPT with resolution of >10 Mb could be considered.
4.2. Fetus with NT 3.0‐3.4 mm and normal NIPT showing no trisomy 13, 18, and 21
For the purpose of this paper, focusing on aberrations beyond NIPT scope, we assumed that all common aneuploidies would be detectable by NIPT. However, during post‐test counseling on normal NIPT results, the negative predictive values of NIPT for trisomies 13, 18, and 21 have to be discussed. In fact, the residual risks for a chromosome aberration that is dependent on a priori risk should be taken into account at the time of pre‐test counseling in all scenarios. This study shows that even when it is assumed that NIPT did not miss trisomy 13, 18, or 21, fetuses with NT 3.0‐3.4 mm have a residual risk of 1:21 (including susceptibility CNVs)—1:33 (excluding susceptibility CNVs)—for a fetal chromosomal aberration other than trisomy 13, 18, and 21. This justifies offering invasive testing followed by CMA, regardless of the local policy on reporting susceptibility CNVs. Our results confirmed the previously published data and showed that not all chromosome aberrations can be detected by offering NIPT to women with a high risk after CT. 5 , 6 , 14 , 39 , 40 It has been previously shown that CMA is the recommended method in these women if they want to be informed of as many chromosomal aberrations as possible. 8 , 14 , 17 Our data suggest that in fetuses with NT 3.0‐3.4 mm notable numbers of abnormal cases would be missed by targeted NIPT for trisomy 13, 18, and 21 and NT measurement in pregnancies with a normal NIPT result has an additional value in assessing the residual risk for another chromosome aberration in the individual fetus.
4.3. Fetuses with NT 3.0‐3.4 mm and normal genome‐wide NIPT (with ~10 Mb resolution, including sex‐chromosome aberrations) may have a population risk for syndromic submicroscopic aberrations
The higher the NIPT resolution the fewer aberrations will be missed and the residual risk can be substantially reduced and perhaps nearly brought to population risk for submicroscopic chromosomal aberrations associated with early‐onset syndromic disorders (1:270 28 ). Our study did not show an increased frequency of early‐onset syndromic disorders in fetuses with NT 3.0‐3.4 mm as was seen in fetuses with NT >3.5 mm by Grande et al. 8 The submicroscopic aberrations that were found in this cohort were mostly susceptibility CNV, and in only one case a syndromic disorder was found (OMIM 300910). However, the overall incidence of submicroscopic chromosome aberrations was higher than in women tested because of advanced maternal age or maternal anxiety (0.84%, 95% CI 0.55%‐1.30%), 28 suggesting that microarray testing may have an additional value also in fetuses with NT 3‐3.4 mm. Larger cohorts tested with microarray are needed to assess the actual frequency of submicroscopic chromosome aberrations in this group.
4.4. Study limitations
A main limitation of the study is that it only includes CMA data from fetuses with an NT 3.0‐3.4 mm undergoing invasive testing because of an increased risk after CT and not only because of an apparently isolated NT of 3.0‐3.4 mm. Moreover, the cut‐off for invasive testing is different in different countries, so there are differences observed between the cohorts. The Rotterdam cohort selection was the most stringent (the highest cut‐off risk after CT) (Table 1), which is reflected in the highest prevalence of aberrations. On the other hand Maya et al, who were interested in submicroscopic findings, excluded fetuses with risks >1:380, clearly influencing the prevalence of aberrations in their cohort. 9 This study is based on retrospective data, and corrections for MoM of serum markers, maternal age or other demographic factors in the whole studied cohort were not possible. For the purpose of this study, this was the best group we could select, although we are aware that it is a subgroup of the general population who opted for invasive testing and most likely represents an upper‐bound risk estimate. Data on fetuses that were invasively tested should be compared with population studies; however, without CMA testing in all individuals it is difficult to assess the frequency of submicroscopic findings, as these may cause syndromes that are not always obvious at birth and may be missed in clinical follow up for years.
Finally, only one fetus showed a syndromic disorder due to a submicroscopic microarray finding, which is lower than the frequency in general population data (1:270), 28 most probably explained by the limited size of the presented combined cohort.
In our opinion, larger cohorts with enlarged NT 3.0‐3.4 mm irrespective of the risk calculation after CT should be analyzed to assess the true risks of a pathogenic submicroscopic unbalanced chromosome aberration in such cases.
The detection rates of NIPT are simplified theoretical calculations that assumed that all aneuploidies as well as structural unbalanced aberrations larger than the resolution of the particular NIPT approach would be detectable. While counseling for NIPT, the whole test characteristics need to be taken into account, especially including potential confined placental mosaicism cases.
5. CONCLUSION
As 69% of chromosome aberrations found in fetuses with NT 3.0‐3.4 mm involved trisomy 21, 18, and 13, NIPT seems to be an appropriate test in such cases at first sight. However, our study shows that the overall risk for a chromosome aberration in these fetuses seems to be very high (~1:10). As an aberrant NIPT result requires confirmatory studies, performing NIPT would delay a final diagnosis in a notable number of women. Our study showed that the residual risk for other chromosomal aberrations than common trisomies is high 1:21‐1:33. Therefore, we advise offering invasive testing independent of the NIPT results for common trisomies. Nevertheless, the decision should always be made by the patient herself and if a pregnant woman carrying a fetus with NT 3.0‐3.4 mm declines an invasive procedure, then genome‐wide NIPT with a resolution of 10 Mb can be proposed as a second‐option to assure the highest diagnostic yield.
CONFLICT OF INTEREST
None.
Supporting information
Appendix S1
ACKNOWLEDGMENTS
The authors would like to thank the Danish Fetal Medicine Database for sharing their data. We thank all clinicians for referring the patients and all laboratory personnel for their dedicated work to achieve rapid prenatal results. We thank Gerdien B. de Jonge and Wichor M. Bramer (Biomedical Information Specialists, Medical Library Erasmus MC) for their assistance in performing the systematic search and removing the duplicate papers during the review process.
Petersen OB, Smith E, Van Opstal D, et al. Nuchal translucency of 3.0‐3.4 mm an indication for NIPT or microarray? Cohort analysis and literature review. Acta Obstet Gynecol Scand. 2020;99:765–774. 10.1111/aogs.13877
Diane Van Opstal and Marike Polak contributed equally to this study.
Funding information
No specific funding was provided to support this study, but Ida Vogel was supported by the Novo Nordisk Foundation NNF16OC0018772, and Olav Bjørn Petersen was supported by the Novo Nordisk Foundation grant NNFSA170030576.
REFERENCES
- 1. Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K. Fetal nuchal translucency: ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ. 1992;304(6831):867‐869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal‐translucency thickness at 10–14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352(9125):343‐346. [DOI] [PubMed] [Google Scholar]
- 3. Souka AP, Von Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH. Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol. 2005;192(4):1005‐1021. [DOI] [PubMed] [Google Scholar]
- 4. Bilardo CM, Muller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30(1):11‐18. [DOI] [PubMed] [Google Scholar]
- 5. Lund IC, Christensen R, Petersen OB, Vogel I, Vestergaard EM. Chromosomal microarray in fetuses with increased nuchal translucency. Ultrasound Obstet Gynecol. 2015;45(1):95‐100. [DOI] [PubMed] [Google Scholar]
- 6. Srebniak MI, de Wit MC, Diderich KE, et al. Enlarged NT (>/=3.5 mm) in the first trimester—not all chromosome aberrations can be detected by NIPT. Mol Cytogenet. 2016;9(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kagan KO, Avgidou K, Molina FS, Gajewska K, Nicolaides KH. Relation between increased fetal nuchal translucency thickness and chromosomal defects. Obstet Gynecol. 2006;107(1):6‐10. [DOI] [PubMed] [Google Scholar]
- 8. Grande M, Jansen FAR, Blumenfeld YJ, et al. Genomic microarray in fetuses with increased nuchal translucency and normal karyotype: a systematic review and meta‐analysis. Ultrasound Obstet Gynecol. 2015;46(6):650‐658. [DOI] [PubMed] [Google Scholar]
- 9. Maya I, Yacobson S, Kahana S, et al. Cut‐off value of nuchal translucency as indication for chromosomal microarray analysis. Ultrasound Obstet Gynecol. 2017;50(3):332‐335. [DOI] [PubMed] [Google Scholar]
- 10. Grossman TB, Bodenlos KL, Chasen ST. Abnormal nuchal translucency: residual risk with normal cell‐free DNA screening. J Matern Fetal Neonatal Med. 2019;22:1‐6. [DOI] [PubMed] [Google Scholar]
- 11. Zhao XR, Gao L, Wu Y, Wang YL. Application of chromosomal microarray in fetuses with increased nuchal translucency. J Matern Fetal Neonatal Med. 2020;33:1749‐1754. [DOI] [PubMed] [Google Scholar]
- 12. Oepkes D, Page‐Christiaens GCL, Bax CJ, et al. Trial by Dutch laboratories for evaluation of non‐invasive prenatal testing. Part I—clinical impact. Prenat Diagn. 2016;36(12):1083‐1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Schendel RV, Page‐Christiaens GCL, Beulen L, et al. Trial by Dutch laboratories for evaluation of non‐invasive prenatal testing. Part II women's perspectives. Prenat Diagn. 2016;36:1091‐1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Srebniak MI, Knapen MFCM, Polak M, et al. The influence of SNP‐based chromosomal microarray and NIPT on the diagnostic yield in 10,000 fetuses with and without fetal ultrasound anomalies. Hum Mutat. 2017;38(7):880‐888. [DOI] [PubMed] [Google Scholar]
- 15. van der Meij KRM, Sistermans EA, Macville MVE, et al. TRIDENT‐2: National implementation of genome‐wide non‐invasive prenatal testing as a first‐tier screening test in the Netherlands. Am J Hum Genet. 2019;105(6):1091‐1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vogel I, Petersen OB, Christensen R, Hyett J, Lou S, Vestergaard EM. Chromosomal microarray as primary diagnostic genomic tool for pregnancies at increased risk within a population‐based combined first‐trimester screening program. Ultrasound Obstet Gynecol. 2018;51(4):480‐486. [DOI] [PubMed] [Google Scholar]
- 17. Van Opstal D, de Vries F, Govaerts L, et al. Benefits and burdens of using a SNP array in pregnancies at increased risk for the common aneuploidies. Hum Mutat. 2015;36(3):319‐326. [DOI] [PubMed] [Google Scholar]
- 18. Srebniak MI, Mout L, Van Opstal D, Galjaard RJ. 0.5 Mb array as a first‐line prenatal cytogenetic test in cases without ultrasound abnormalities and its implementation in clinical practice. Hum Mutat. 2013;34(9):1298‐1303. [DOI] [PubMed] [Google Scholar]
- 19. Van Opstal D, Srebniak MI, Polak J, et al. False negative NIPT results: risk figures for chromosomes 13, 18 and 21 based on chorionic villi results in 5967 cases and literature review. PLoS ONE. 2016;11(1):e0146794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mackie FL, Hemming K, Allen S, Morris RK, Kilby MD. The accuracy of cell‐free fetal DNA‐based non‐invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta‐analysis. BJOG. 2017;124(1):32‐46. [DOI] [PubMed] [Google Scholar]
- 21. Gil MM, Accurti V, Santacruz B, Plana MN, Nicolaides KH. Analysis of cell‐free DNA in maternal blood in screening for aneuploidies: updated meta‐analysis. Ultrasound Obstet Gynecol. 2017;50(3):302‐314. [DOI] [PubMed] [Google Scholar]
- 22. Hartwig TS, Ambye L, Sorensen S, Jorgensen FS. Discordant non‐invasive prenatal testing (NIPT)—a systematic review. Prenat Diagn. 2017;37:527‐539. [DOI] [PubMed] [Google Scholar]
- 23. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177‐188. [DOI] [PubMed] [Google Scholar]
- 24. Srebniak MI, Diderich KEM, Govaerts LCP, et al. Types of array findings detectable in cytogenetic diagnosis: a proposal for a generic classification. Eur J Hum Genet. 2014;22:856‐858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rosenfeld JA, Coe BP, Eichler EE, Cuckle H, Shaffer LG. Estimates of penetrance for recurrent pathogenic copy‐number variations. Genet Med. 2013;15(6):478‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Girirajan S, Rosenfeld JA, Coe BP, et al. Phenotypic heterogeneity of genomic disorders and rare copy‐number variants. N Engl J Med. 2012;367(14):1321‐1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Veltman JA, Brunner HG. Understanding variable expressivity in microdeletion syndromes. Nat Genet. 2010;42(3):192‐193. [DOI] [PubMed] [Google Scholar]
- 28. Srebniak MI, Joosten M, Knapen M, et al. Frequency of submicroscopic chromosomal aberrations in pregnancies without increased risk for structural chromosomal aberrations: systematic review and meta‐analysis. Ultrasound Obstet Gynecol. 2018;51(4):445‐452. [DOI] [PubMed] [Google Scholar]
- 29. Pandya PP, Brizot ML, Kuhn P, Snijders RJ, Nicolaides KH. First‐trimester fetal nuchal translucency thickness and risk for trisomies. Obstet Gynecol. 1994;84(3):420‐423. [PubMed] [Google Scholar]
- 30. Ayras O, Tikkanen M, Eronen M, Paavonen J, Stefanovic V. Increased nuchal translucency and pregnancy outcome: a retrospective study of 1063 consecutive singleton pregnancies in a single referral institution. Prenat Diagn. 2013;33(9):856‐862. [DOI] [PubMed] [Google Scholar]
- 31. Nicolaides KH, Brizot ML, Snijders RJ. Fetal nuchal translucency: ultrasound screening for fetal trisomy in the first trimester of pregnancy. Br J Obstet Gynaecol. 1994;101(9):782‐786. [DOI] [PubMed] [Google Scholar]
- 32. Bardi F, Bosschieter P, Verheij J, et al. Is there still a role for nuchal translucency measurement in the changing paradigm of first trimester screening? Prenat Diagn. 2020;40(2):197‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Salomon LJ, Alfirevic Z, Audibert F, et al. ISUOG updated consensus statement on the impact of cfDNA aneuploidy testing on screening policies and prenatal ultrasound practice. Ultrasound Obstet Gynecol. 2017;49(6):815‐816. [DOI] [PubMed] [Google Scholar]
- 34. Gadsbøll K, Petersen OBB, Gatinois V, et al. Current use of noninvasive prenatal testing in Europe, Australia and USA: a graphical presentation. Acta Obstet Gynecol Scand. 2020;99:722‐730. [DOI] [PubMed] [Google Scholar]
- 35. Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367(23):2175‐2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Salomon LJ, Sotiriadis A, Wulff CB, Odibo A, Akolekar R. Risk of miscarriage following amniocentesis or chorionic villus sampling: systematic review of literature and updated meta‐analysis. Ultrasound Obstet Gynecol. 2019;54(4):442‐451. [DOI] [PubMed] [Google Scholar]
- 37. Khalil A, Mahmoodian N, Kulkarni A, et al. Estimation of detection rates of aneuploidy in high‐risk pregnancy using an approach based on nuchal translucency and non‐invasive prenatal testing: a cohort study. Fetal Diagn Ther. 2015;38(4):254‐261. [DOI] [PubMed] [Google Scholar]
- 38. Gregg AR, Skotko BG, Benkendorf JL, et al. Noninvasive prenatal screening for fetal aneuploidy, 2016 update: a position statement of the American College of Medical Genetics and Genomics. Genet Med. 2016;18(10):1056‐1065. [DOI] [PubMed] [Google Scholar]
- 39. Leung TY, Vogel I, Lau TK, et al. Identification of submicroscopic chromosomal aberrations in fetuses with increased nuchal translucency and apparently normal karyotype. Ultrasound Obstet Gynecol. 2011;38(3):314‐319. [DOI] [PubMed] [Google Scholar]
- 40. Petersen OB, Vogel I, Ekelund C, et al. Potential diagnostic consequences of applying non‐invasive prenatal testing: population‐based study from a country with existing first‐trimester screening. Ultrasound Obstet Gynecol. 2014;43(3):265‐271. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


